w w w . r b o . o r g . b r
Original
Article
Results
of
open
reduction
and
internal
fixation
of
severe
fractures
of
the
proximal
humerus
in
elderly
patients
夽
,
夽夽
Alberto
Naoki
Miyazaki,
Marcelo
Fregoneze,
Pedro
Doneux
Santos,
Luciana
Andrade
da
Silva
∗,
Guilherme
do
Val
Sella,
João
Manoel
Fonseca
Filho,
Marco
Tonding
Ferreira,
Paulo
Roberto
Davanso
Filho,
Sergio
Luiz
Checchia
DepartmentofOrthopaedicsandTraumatology,FaculdadedeCiênciasMédicas,SantaCasadeSãoPaulo,SãoPaulo,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received22March2013 Accepted20May2013
Keywords:
Humeralfractures Elderly
Fracturefixation,internal Avascularnecrosis
a
b
s
t
r
a
c
t
Objective:Toevaluate clinicalandradiologicalresults withopen reductionandinternal fixationofseverefracturesoftheproximalhumerusinthepatientsovertheageof60years.
Methods:BetweenJune1992andFebruary2011,21patientswithFGEPUovertheageof60 yearsweretreatedbyopenreductionandinternalfixationattheGroupofShoulderand ElbowDepartmentofOrthopaedicsandTraumatologyofSantaCasadeSãoPauloMedical School.18patientswerereviewed.
Results:Twopatientshadexcellentresults,12good,threeregularandonebad.Therefore,we findthat77.7%ofthesehadgoodandexcellentresults.Allpatientsweresatisfiedwiththe treatmentandonlythreepatientsdidnotreturntopreviousactivities.Meanpostoperative mobilitieswere122◦elevation(90–150◦),39lateralrotation(20–60◦)andmedialrotationof T11(T5tosacroiliacjoint).
Conclusion: OpenreductionandinternalfixationofFGEPUmayalsobeindicatedforelderly patientsandobtained77.7%ofgoodandexcellentresults.Statistically(p<0.05),the anatom-icalreductionofthefracturewasfoundtobeimportantforobtaininggoodresults.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
Avaliac¸ão
dos
resultados
da
reduc¸ão
aberta
e
da
fixac¸ão
interna
das
fraturas
graves
da
extremidade
proximal
do
úmero
em
idosos
Palavras-chave:
Fraturasdohumero Idoso
Fixac¸ãointernadefraturas Necroseavascular
r
e
s
u
m
o
Objetivo:avaliarclinicaeradiologicamenteosresultadosobtidoscomareduc¸ãoabertaea fixac¸ãointernadasfraturasgravesdaextremidadeproximaldoúmero(FGEPU)napopulac¸ão comidadeigualousuperiora60anos.
Métodos:entrejunhode1992efevereirode2011,oGrupodeOmbroeCotovelodo Depar-tamentodeOrtopediaeTraumatologiadaFaculdadedeCiênciasMédicasdaSantaCasade
夽Pleasecitethisarticleas:MiyazakiAN,etal.Avaliac¸ãodosresultadosdareduc¸ãoabertaedafixac¸ãointernadasfraturasgravesda
extremidadeproximaldoúmeroemidosos.RevBrasOrtop.2014;49:25–30.
夽夽
StudyconductedatGroupofShoulderandElbow,DepartmentofOrthopaedicsandTraumatologyofSantaCasadeSãoPauloMedical School,SantaCasadeSãoPaulo,SãoPaulo,SP,Brazil.
∗ Correspondingauthor.
E-mail:lucalu01@me.com(L.A.daSilva).
2255-4971/$–seefrontmatter©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditoraLtda.Allrightsreserved.
SãoPaulotratou,comreduc¸ãoabertaefixac¸ãointerna,21pacientescomFGEPUecomidade superiora60anos.Desses,18foramreavaliados.
Resultados:doispacientesevoluíramcomresultadosexcelentes,12bons,trêsregulareseum ruim.Portanto,verificamosque77,7%evoluíramcombonseexcelentesresultados.Todosos pacientesestavamsatisfeitoscomotratamentoeapenastrêsnãoretornaramàsatividades prévias.Asmédiasdemobilidadepós-operatóriaforamde122◦deelevac¸ão(90◦–150◦),39◦ derotac¸ãolateral(20◦–60◦)eT11derotac¸ãomedial(T5aGlúteo).
Conclusão: areduc¸ãoabertaeafixac¸ãointernadasFGEPUpodemserindicadastambém parapacientesidososeobtivemos77,7%debonseexcelentesresultados.Estatisticamente (p<0,05),areduc¸ãoanatômicadafraturamostrou-seimportanteparaaobtenc¸ãodebons resultados.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Todososdireitosreservados.
Introduction
Fracturesoftheproximalendofthehumerusinfourparts andfracture-dislocationsinthreepartsarecharacterizedby lossofjointcongruityandsevereimpairmentofvascularity ofhumeralhead.1,2 Theepiphysealfractures,that compro-misetheheadofhumerus,are infrequent,beingcausedby animpactagainsttheglenoidcavity;theselesionsare associ-atedwithinjurytothehumeralheadbloodsupplyortheir fragmentsand, therefore,are difficult totreatand its evo-lutionisaccompaniedbyhigh complicationrates.2,3 Those aforementioned injuries (excluding fractures in four parts impactedinvalgus)arecalledseverefracturesoftheproximal humerus(SFPU).Thefour-partfractures impactedinvalgus wereexcluded because,accordingtoJakobetal.4 andlater Reschet al.,5 preserve intactthe medialperiosteumofthe anatomicalneck,andthisisessentialformaintainingthe vas-cularizationofthehumeralhead,whichwould explainthe lowerrateofosteonecrosis.5,6
Somestudies haveattemptedtodemonstrate the bene-fitsanddisadvantagesofthetreatmentoptionsoffour-part fracturesand fracture-dislocationsinthreeparts, but what is the best way to treat? This remains challenging and controversial.7–9Intheliterature,therearedescriptionsof sev-eralmethodsoftreatment,includingconservativeones,and differenttypesofsurgicaltechniques,suchaspercutaneous fixation, open reductionand internal fixation withvarious typesofsynthesis,andthereplacementofhumeralhead.10–12 Thenaturalhistoryofthetreatmentofthesefractures sug-geststhattheycanevolvetononunion,pseudoartrosisand/or avascularnecrosis,13 leading to unsatisfactory results. The occurrenceofpersistentpainandstiffness,regardlessof treat-mentchosen,iscommon.8,9,11,14
HelmyandHinterman15claimthat,intheliterature,there isnounanimityofopinionastothebest methodof treat-mentofthesefractures.Theonlyapparentconsensusisabout theimportanceofananatomicalreductionand ofastable osteosynthesis.12,16
Intheelderlypopulation,thetreatmentoftheselesions remainsevenmorecontroversial.Internalfixation ofthese fractures,especiallyinpatientswithosteopeniaandinthose with comminuted fractures, resulted in high complication rates.10,16–18Forthesepatients,hemiarthroplastyremainsthe treatmentofchoice,becauseoftheanatomicalandtechnical
difficultiesinitsmaintenance1,4,5,10,19and ofthehigh com-plicationrates,suchaspost-traumaticosteonecrosisofthe humeralhead.17,20 However,itisknownthatthefunctional outcomeofhemiarthroplastiesforthetreatmentoffractures is unsatisfactory,as comparedwiththe initialdescriptions of Neer.5,6 Usually, patients develop loss of lift force and decreased range of motion, despite the low incidence of pain.5,10
It is important to remember that sometimes the osteonecrosis of the humeral head will not evolve with unfavourableclinicalandfunctionaloutcomes,especiallyin thecaseofananatomicalreconstructionofthefractureand intheabsenceofacompletecollapseofthesubchondralbone duetoosteonecrosis.13
The objective of this study is to evaluateclinically and radiographicallytheresultsobtainedwithopenreductionand internalfixationofSFPUinapopulationagedover60years.
Patients
and
methods
BetweenJune1992andFebruary2011,21patientsolderthan 60 years withSFPU were treated withopen reduction and internalfixationattheGroupofShoulderandElbow, Depart-mentofOrthopaedicsandTraumatology,FacultyofMedical Sciences,SantaCasadeSãoPaulo.Ofthese,twodiedandone isbedridden,so18werereassessed.Patientswithfractures intwo parts, inthreepartswithout associateddislocation, infour-partimpacted invalgusandthose notclassifiedby Neerwereexcluded.20Alsoexcludedwerethosepatientswho were less than 60 yearsof age and who underwent hemi-arthroplastywithpostoperativefollow-up<12months.Eight patientsweremale(44%)andtenfemales(56%),withamean ageof68years(range60–78).Thedominantlimbwasaffected inninecases(50%)(Table1).
Themechanismsofinjurywere:fallsfromaheightinthree cases(17%)andfallstothegroundinfifteen(83%).
All patients underwent radiographs of the shoulder (traumaseries),fordiagnosisandclassificationoffractures; computedtomographywasusedintencasestocomplement thestudy.
ThefractureswereclassifiedaccordingtoNeer,20asshown inTable2.
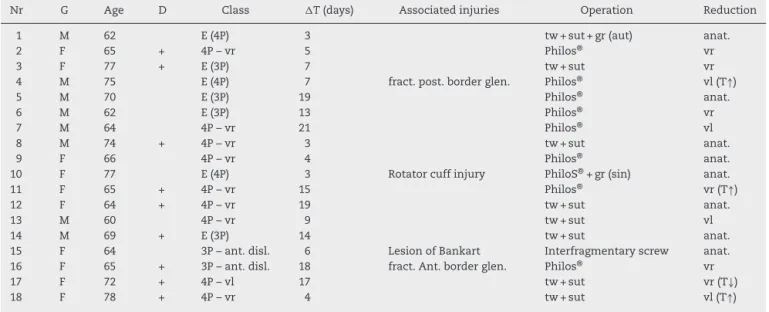
Table1–Demographicdataofpatients,classificationoffractures,associatedinjuries,fracturereductionandfixation type.
Nr G Age D Class T(days) Associatedinjuries Operation Reduction
1 M 62 E(4P) 3 tw+sut+gr(aut) anat.
2 F 65 + 4P–vr 5 Philos® vr
3 F 77 + E(3P) 7 tw+sut vr
4 M 75 E(4P) 7 fract.post.borderglen. Philos® vl(T↑)
5 M 70 E(3P) 19 Philos® anat.
6 M 62 E(3P) 13 Philos® vr
7 M 64 4P–vr 21 Philos® vl
8 M 74 + 4P–vr 3 tw+sut anat.
9 F 66 4P–vr 4 Philos® anat.
10 F 77 E(4P) 3 Rotatorcuffinjury PhiloS®+gr(sin) anat.
11 F 65 + 4P–vr 15 Philos® vr(T↑)
12 F 64 + 4P–vr 19 tw+sut anat.
13 M 60 4P–vr 9 tw+sut vl
14 M 69 + E(3P) 14 tw+sut anat.
15 F 64 3P–ant.disl. 6 LesionofBankart Interfragmentaryscrew anat.
16 F 65 + 3P–ant.disl. 18 fract.Ant.borderglen. Philos® vr
17 F 72 + 4P–vl 17 tw+sut vr(T↓)
18 F 78 + 4P–vr 4 tw+sut vl(T↑)
G,gender,Age,age,D,dominance,class,classificationofNeer;T,timeintervalbetweentraumaandsurgery,M,male;F,female;E,epiphyseal fractureassociated;3P,fractureintothreeparts;4P,fractureintofourparts;anat.,anatomicreduction;vr,varusdeviation,vl,valgusdeviation; ant.disl.,anteriordislocationassociated;fract.,fracture;.Glen.,glenoid;.post.,posterior;ant.,anterior;tw,threadedwires,gr(sin),synthetic graft;gr(aut),autograft;sut,suturewithtransosseouspointsofgreater/lessertuberosity,T,reductionofgreatertuberosity(↓-low;↑-high). Source:HospitalMedicalFile.
posteriorborderoftheglenoid cavity(case4);lesionofthe anterior–inferiorlipoftheglenoidcavity,diagnosed intraop-eratively(case15);androtatorcuffinjury(case10)(Table1).
Themeantimeintervalbetweentraumaandsurgerywas 10days(range3–21)(Table1).
Thesurgical methodofchoice was open reductionand internalfixation by deltopectoral approach, withthe most atraumaticsurgicaltechniquepossible.Thefixationmethods variedaccordingtothetypeoffracture:threadedwires asso-ciatedwithnonabsorbentsuturebandnr.5(Ethibond®)(eight
cases),lockedplate(Philos®)(ninecases)and
interfragmen-taryscrews(onecase).Autologouscancellousbonegraftfrom theiliaccrestwasusedinonecase(case1)(Table1).
Inthepostoperativeperiod,Velpeauslingimmobilization wasapplied,withpermissiontoexerciseonlyforelbowand wristforsixtoeightweeks,dependingontheradiographic
Table2–DistributionoffracturesaccordingtoNeer classification.
Neerclassification Total
Fract.disl.anterior3P w/fract.tub> 2 w/fract.tub< –
Fract.4P vldeviationofhead 1
vrdeviationofhead 8 Epifisary fract.3Pepifisarytrait 4 fract.4Pepifisarytrait 3
Total 18
Fract.disl,fracture-dislocation;3P,threeparts,w/,with;fract. frac-ture;tub.,tuberosity(<-less;>-larger);4P,fourparts;vl,valgus;vr, varus;head,humeralhead.
Source:HospitalMedicalFile.
fractureunion.Afterevidenceofconsolidation,thepatients beganpassiveexercisestogainrangeofmotion(ROM),andat 12weeksactiveexercisestogainmusclestrength.
Theresultswereevaluatedbyascoresystemdefinedby UniversityofCaliforniaatLosAngeles(UCLA)21andROMwas measured according toAmerican Academy ofOrthopaedic Surgeons(AAOS)criteria.22
TheclassificationofFicatetal.andEnnekingetal., modi-fiedbyNeeretal.,wasusedforevaluationofosteonecrosisof thehumeralhead,whenpresent.23
StatisticalanalysiswasperformedusingtheFisherexact test. Thefollowingvariables were calculated:end resultof UCLAbytypeoffracture,age,typeofreduction,forpresence orabsenceofosteonecrosis,andforpresenceorabsenceof arthrosis.Alsothefollowingwerestatisticallyanalyzed:age, dependingonthetypeoffractureandpresenceorabsenceof osteonecrosis,aswellasthevariables“reductiondepending onthe typeoffractureand offixation”,and “osteonecrosis accordingtothetypeoffixationandreduction”.Theanalyses wereperformedwiththeaidofstatisticalsoftwareMinitab®
version16.Asignificancelevelof5%foralltestsof hypothe-siswasadopted;therefore,thehypotheseswithasignificance level(pvalue)<0.05wererejected.
Results
Table3–Results.
Nr T(months) E,LR,MR Complications Othersurgeries UCLA(total)
1 45 140,45,T10 RSM 34
2 28 130,45,T12 29
3 17 90,30,GL RSM 26
4 28 100,20,L2 NecrosisII 28
5 29 120,30,T7 29
6 29 80,20,T8 Arthrosis(ecc.)+NecrosisIV RSM 19
7 36 130,30,T12 29
8 12 150,45,T7 RSM 30
9 12 140,60,T8 29
10 17 150,60,T12 33
11 29 110,30,GL Arthrosis(cent.)+NecrosisIII 24
12 188 150,45,T8 RSM 35
13 183 150,30,T5 RSM 33
14 109 130,60,T7 RSM 33
15 107 110,50,L2 NecrosisII 26
16 29 90,30,GL 30
17 18 120,45,L3 RSM 31
18 45 110,30,L4 RSM 30
T,follow-uptime;E,elevationindegrees;LR,lateralrotationindegrees;MR,medialrotationaccordingtovertebrallevel;T,thoracicvertebra; GL,gluteus;cent.,centric;ecc.,eccentric,RSM,removalofsynthesismaterial.
Source:HospitalMedicalFile.
Mean postoperative mobility was 122◦ of elevation
(90–150◦),39◦ oflateral rotation(20–60◦)and T11ofmedial
rotation(T5-gluteus)(Table3).
Aftertheanalysisofpostoperativeradiographs,theresults offracturereductionobtainedduringsurgerywere: anatom-icalreductionineight(44%),varusinsix(33%)andvalgusin four(23%).Thegreatertuberosityremainedhighinthreecases (cases4,11and18)andlowinone(case 17).Consolidation occurredinallfractures.
Theobservedcomplicationswere:twocasesoftransient neuropraxiaofthe axillarynerve(11%, cases5and 6),two superficialinfections(11%,cases17and18),onewith impinge-ment syndrome associated with malunion of the greater tuberosity(5%,case18),twowithosteoarthritisofthe shoul-derinassociationwithosteonecrosis(11%,cases6and11),
sixvarusconsolidationsasaresultofunsatisfactory reduc-tion(39%,cases2,3,6,11,16and17),apoorplacementofthe implant(5%,case6),fourwithosteonecrosisofthehumeral head:twooftypeII(cases4and15),oneoftypeIII(case11) andoneoftypeIV(case6),whichamountedto22%ofpatients (Table3).
The mean UCLAscoreof thetwo shouldersthat devel-opedarthrosiswas21(19–24)points,withmeanelevationof 95◦.Inthefourcaseswhichdevelopedosteonecrosisofthe
humeralhead,themeanscorewas24(19–29)pointsandthe meanelevationwas105◦.Inthe12caseswhichdidnotdevelop
osteoarthritisand/ornecrosis,themeanscorewas30(28–35) points,withameanelevationof130◦.Inpatientsinwhomwe
obtainedanatomicalreductionofthefracture,theUCLAmean scorewas31(28–35)points,withmeanelevationof138◦,and
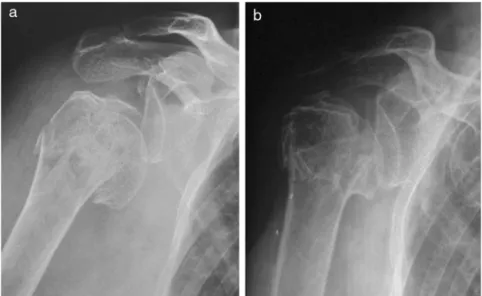
Fig.2–Case3:Radiographsoftherightshoulder(frontalview),showingathree-partfracturewithepiphysealtrait;(a) preoperative,(b)postoperative,17months.
inthosewithoutanatomicreduction,themeanscorewas27 (18–33)points,withameanelevationof111◦.
Discussion
Inliteraturethereisnoconsensusregardingthetreatmentof SFPU.12In1970,Neeretal.publishedtheirexperiencewiththe treatmentofSFPUwithuseofhemiarthroplasty;theseauthors obtainedgoodandexcellentresultsin90%oftheirpatients.11 Theseresultswerenotreproducedlaterbyotherauthors,and highratesofcomplicationsandunsatisfactoryresultswere observed.24–26
Inrecentdecades,studieshaveshownthatopen reduc-tionandinternalfixationofSFPUledtosatisfactoryresults inmostpatients.Age,typeoffracture,achieving(ornot)the reduction,reductiontechnique,qualityoffixation,evolution withorwithoutosteonecrosisofthehumeralhead,and evo-lutionwithorwithoutarthritisintheshoulderjointarethe mainprognosticfactorsintreatment.12,13,27,28
Theadvancedageofpatientswhounderwentopen reduc-tionandinternalfixationofSFPU(mostlyosteoporoticpeople) isquotedbyGerberetal.12 asanegativeprognosticfactor. However,inourstudy,nostatisticallysignificantcorrelation betweenageandworseoutcomesbyUCLAscore(p=0.23)was noted,whichagreeswiththefindingsofMoonotetal.29
Thetypeoffracture,asdescribedintheliterature, influ-ences the worst results, especially in the higher rates of complicationsrelatedtomoreseverecases.27However,inour studywecouldnotcorrelatestatisticallyfractureseveritywith worseoutcomes(p=0.33).
Studiesdescribetheimportanceofanatomicreductionof thefractureduringsurgery;andthebestresultswereobtained incasesinwhichthisobjectivewasachievedandmaintained untilconsolidation5,13,27(Fig.1).However,theachievementof thisobjectiveisdependentonfactorssuchastypeoffracture andtypeoffixation.12 Inourstudy,non-anatomical reduc-tionoccurredin11cases.Thisfactorinfluencedstatistically
intheworstresults,whencomparedwiththecasesinwhich anatomicreductionwasachieved(p=0.03).
Inrecentyears,studieshavedemonstratedthatthequality offixationisofutmostimportanceinthetreatmentofSFPU, mainlytomaintainthereductionachievedduringthesurgery alsointhepostoperativeperiod.12,16 However,inourstudy, whenfixationmethods(threadedwiresassociatedwithsuture bandorPhilos®plate)werecompared,therewasno
statisti-callysignificantdifferencewithrespecttotheresultsbyUCLA score(p=0.33).
Osteonecrosisofhumeralheadoccurredinfourpatients (22%), a result slightly below the value reported in the literature.12,17,20Thesefourpatientshadtheworstfunctional results(p=0.006).ThreecaseswerefixedwithPhilos®plate
andonecasewiththreadedwiresassociatedwithsutureband. Inthreecases,anatomicreductionwasnotobtained(Fig.2). However,with regardtothe presenceofosteonecrosis, the variables“typeoffixation”and“fracturereduction”showed nostatisticallysignificantdifference(p=0.37andp=1.0);this isconsistentwiththefindingsofSüdkampetal.16
Inourstudy,ageand typeoffracturewerealsonot cor-related with osteonecrosis (p=0.67 and p=0.26), which is consistentwiththe findingsofGerberet al.12 Ourlowrate ofosteonecrosisofthehumeralheadcanbeexplainedbythe group’sexperienceinthetreatmentofSFPUandbytheuse ofthemoreatraumatictechniquepossible.Another explana-tionwouldbethedifficultytocorrectlyclassifythefractures accordingtoNeeretal.classification,20andthiscouldcause aincorrectlygreater numberofSFPU.Theinterpretationof imagesoftheproximalhumerusfractureand,thus,its classi-fication,arequitecontroversial.12
24pointsinthefinalevaluation.Sofar,noneofthesepatients requiredarthroplastictreatment.
Conclusion
Open reductionand internalfixation ofSFPU may also be indicatedforelderlypatients.Weobtained77.7%ofgoodand excellentresults.
Statistically(p=0.03),ananatomicreductionofthefracture wasfoundtobeimportantforobtaininggoodresults.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. NaranjaRJ,IannottiJP.Displacedthree-andfour-part proximalhumerusfractures:evaluationandmanagement.J AmAcadOrthopSurg.2000;8(6):373–82.
2. NeerCS.Four-segmentclassificationofproximalhumeral fractures:purposeandreliableuse.JShoulderElbowSurg. 2002;11(4):389–400.
3. ChesserTJS,LangdonIJ,OgilvieC,SarangiPP,ClarkeAM. Fracturesinvolvingsplittingofthehumeralhead.JBoneJoint SurgBr.2001;83(3):423–6.
4. JakobRP,MiniaciA,AnsonPS,JabergH,OsterwalderA,Ganz R.Fourpartvalgusimpactedfracturesoftheproximal humerus.JBoneJointSurgBr.1991;73(2):295–8. 5. ReschH,BeckE,BayleyI.Reconstructionofthe
valgus-impactedhumeralheadfracture.JShoulderElbow Surg.1995;4(2):73–80.
6. ReschH,HübnerC,SchwaigerR.Minimallyinvasive reductionandosteosynthesisofarticularfracturesofthe humeralhead.Injury.2001;32(1):25–32.
7. ZytoK,WallaceWA,FrostickSP,PrestonBJ.Outcomeafter hemiarthroplastyforthree-andfour-partfracturesofthe proximalhumerus.JShoulderElbowSurg.1998;7(2):85–9. 8. KristiansenB,ChristensenSW.Platefixationofproximal
humeralfractures.ActaOrthopScand.1986;57:320–3. 9. PaavolainenP,BjorkenheimJM,SlatisP,PaukkuP.Operative
treatmentofsevereproximalhumeralfractures.ActaOrthop Scand.1983;54(3):374–9.
10.ReschH,PovaczP,FröhlichR,WambacherM.Percutaneous fixationofthree-andfour-partfracturesoftheproximal humerus.JBoneJointSurgBr.1997;79(2):295–300.
11.NeerCS.DisplacedproximalhumeralfracturesII.Treatment ofthree-partandfour-partdisplacement.JBoneJointSurg Am.1970;52(6):1090–103.
12.GerberC,WernerCML,VienneP.Internalfixationofcomplex fracturesoftheproximalhumerus.JBoneJointSurgBr. 2004;86:848–55.
13.GerberC,HerscheO,BerberatC.Theclinicalrelevanceof posttraumaticavascularnecrosisofthehumeralhead.J ShoulderElbowSurg.1998;7(6):586–90.
14.RobinsonCM,PageRS.Severelyimpactedvalgusproximal humeralfractures.Resultsofoperativetreatment.JBone JointSurgAm.2003;85(9):1647–55.
15.HelmyN,HintermannB.Newtrendsinthetreatmentof proximalhumerusfractures.ClinOrthopRelatRes. 2006;(442):100–8.
16.SüdkampN,BayerJ,HeppP,VoigtC,OesternH,KääbM,etal. Openreductionandinternalfixationofproximalhumeral fractureswithuseofthelockingproximalhumerusplate. Resultsofaprospective,multicenter,observationalstudy.J BoneJointSurgAm.2009;91(6):1320–8.
17.RobinsonCM,PageRS,HillRM,SandersDL,Court-BrownCM, WakefieldAE.Primaryhemiarthroplastyfortreatmentof proximalhumeralfractures.JBoneJointSurgAm. 2003;85(7):1215–23.
18.MittlmeierTW,StedtfeldHW,EwertA,BeckM,FroschB,Gradl G.Stabilizationofproximalhumeralfractureswithan angularandslidingstableantegradelockingnail(TargonPH). JBoneJointSurgAm.2003;85Suppl.4:136–46.
19.JakobRP,KristiansenT,MayoK,GanzR,MüllerME. Classificationandaspectsoftreatmentoffracturesofthe proximalhumerus.In:BatemanJE,WelshRP,editors.Surgery oftheshoulder.Philadelphia:B.C.Decker;1984.p.
330–43.
20.Neer2ndCS.Displacedproximalhumeralfractures.I. Classificationandevaluation.JBoneJointSurgAm. 1970;52(6):1077–89.
21.EllmanH,KaySP.Arthroscopicsubacromialdecompression forchronicimpingement.Two-tofive-yearresults.JBone JointSurgBr.1991;73(3):395–8.
22.AmericanAcademyofOrthopaedicSurgeons(AAOS).Joint motion:methodofmeasuringandrecording.Chicago: AmericanAcademyofOrthopaedics;1965.
23.NeerCS.Glenohumeralarthroplastyinshoulder reconstruction.Philadelphia:Saunders;1990.p.143–272. 24.BiglianiLU,FlatowEL.Failedprosteticreplacementfor
displacedproximalhumeralfractures.OrthopTrans. 1991;15:747–8.
25.TannerMW,CofieldRH.Prostheticarthroplastyforfractures andfracture-dislocationsoftheproximalhumerus.Clin OrthopRelatRes.1983;(179):116–28.
26.ChecchiaSL,DoneauxP,MiyasakiAN,FregoneseM,SilvaLA, FariaFN,etal.Tratamentodasfraturasdoterc¸oproximaldo úmerocomapróteseparcialEccentra®.RevBrasOrtop. 2005;40(3):130–40.
27.KoJY,YamamotoR.Surgicaltreatmentofcomplexfractureof theproximalhumerus.ClinOrthopRelatRes.
1996;(327):225–37.
28.BoileauP,TrojaniC,WalchG,KrishnanSG,RomeoA, SinnertonR.Shoulderarthroplastyforthetreatmentofthe sequelaeoffracturesoftheproximalhumerus.JShoulder ElbowSurg.2001;10(4):299–308.
29.MoonotP,AshwoodN,HamletM.Earlyresultsfortreatment ofthree-andfour-partfracturesoftheproximalhumerus usingthePhilosplatesystem.JBoneJointSurgBr. 2007;89(9):1206–9.