w w w . r b h h . o r g
Revista
Brasileira
de
Hematologia
e
Hemoterapia
Brazilian
Journal
of
Hematology
and
Hemotherapy
Original
article
Lack
of
association
between
Kidd
blood
group
system
and
chronic
kidney
disease
Tiago
Verri
Capriolli,
Jeane
Eliete
Laguila
Visentainer,
Ana
Maria
Sell
∗UniversidadeEstadualdeMaringá(UEM),Maringá,PR,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received27March2017 Accepted30May2017 Availableonline28June2017
Keywords:
Kiddbloodgroupsystem Chronickidneyfailure Serotyping
Bloodureanitrogen Ureatransporter
a
b
s
t
r
a
c
t
Background:TheKiddbloodgroupsystemhasthreeantigens,Jka,JkbandJk3,foundonred
bloodcellsandonendothelialcellsoftheinnerliningofbloodvesselsintherenalmedulla. Theseare knownasureatransporter B(UT-B).Researchershavefoundthatindividuals carryingtheJk(a−b−)orJk-null(UT-Bnull)phenotypeshavealowerurine-concentrating capabilityandriskofsevererenalimpairment.Thisstudyevaluatedthedistributionofthe KiddphenotypesinpatientswithchronickidneydiseaseandapossibleassociationofKidd antigenswiththedevelopmentofrenaldisease.
Methods:JkaandJkbantigenswerephenotypedusingthegelcolumnagglutinationtest
(ID-cardsBio-RAD)in197patientswithchronickidneydiseaseand444blooddonors,asthe controlgroup.Thephenotypeandantigenfrequenciesbetweenpatientsandcontrolswere evaluatedusingtheChi-squaremethodwithYatescorrectionandlogisticregressionafter adjustmentsforgenderandage.
Results:NodifferenceswereobservedbetweentheKiddphenotypesfrequencydistribution betweenpatientswithchronickidneydiseaseandblooddonors[Jk(a−b+)=22.3%and27.2%; Jk(a+b−)=30.5%and24.3%;Jk(a+b+)=47.25%and48.4%,respectively].
Conclusion: ThedistributionofKiddphenotypesfoundinthestudiedpopulationisexpected forCaucasians;JkaandJkbantigensandphenotypeswerenotfoundtoberelatedto
sus-ceptibilityforchronickidneydisease.
©2017Associac¸ ˜aoBrasileiradeHematologia,HemoterapiaeTerapiaCelular.Published byElsevierEditoraLtda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Theredbloodcell(RBC)membranecontainsmanyanchored surfaceproteinsandproteinsthatcrossthelipidbilayer car-ryingdifferentbloodgroupantigens.Currently,36systems1of
RBCgroupshavebeendescribedaccordingtotheInternational
∗ Correspondingauthorat:UniversidadeEstadualdeMaringá(UEM),Av.Colombo,5790,blocoT20,87020-900Maringá,PR,Brazil.
E-mails:anamsell@gmail.com,amsell@uem.br(A.M.Sell).
SocietyofBloodTransfusion(ISBT)(http://www.isbtweb.org). Amongthem,theKiddbloodgroupsystem(JK;ISBT009)has beenrecognizedasclinicallyimportantsinceitsidentification in1951.2
AntigensoftheKiddbloodgroupsystemareexpressedon type3glycoproteins, alsoknownas theurea transporterB
http://dx.doi.org/10.1016/j.bjhh.2017.05.007
(UT-B).Thisproteincontains389aminoacidsandpassesten timesthroughthelipidbilayerwithboththeNterminusandC terminusbeingintracellular.Threeantigenshavebeenfound (Jka,JkbandJk3)ontheneighboringfourthextracellular loop-ingandthreephenotypes,Jk(a+b−),Jk(a−b+),andJk(a+b+), arecommonamongdifferentpopulations.TheJk(a−b−) phe-notypeis rarein mostpopulations. Itwas first foundin a FilipinaofSpanish andChineseancestrywiththe antibod-iesusuallybeingdetectedaftertransfusionsorpregnancies. Afterimmunization,anti-Jk3canbefoundinpatientswith theJk(a−b−)recessivephenotype,causingacuteanddelayed hemolytictransfusionreactions.3,4
TheJkglycoproteiniscodedbytheSolutecarrierfamily14, memberA1(SLC14A1)gene,amemberoftheurea-transporter genefamily,locatedonchromosome18q12-q21andorganized into11exons.Thetwomajorcodominantallelesofthegene, JK*AandJK*B,havesimilar frequenciesinCaucasian popu-lations(0.51and0.49,respectively)anddefinetheJkaandJkb antigens,respectively.TheJka/Jkbpolymorphismisdefinedby 838A>Ginexon9(Asp280Asnsubstitution),theothertwo sin-glenucleotidepolymorphisms(SNPs)causenochangestothe aminoacidsequence.5
The Kidd antigens or UT-B are expressed on RBCs and theendotheliumofthevasarectaandepithelialsurfacesof therenalinnermedulla,aswellasinnon-renaltissuesand endothelialcells.6–8 TheKiddproteinisamajortransporter
of urea across the RBC membrane and this rapid process helps maintainthe osmoticstability of the cell. Null phe-notypeindividuals lackthis transporter.WithintheKidney, theureatransporterenablestherenalmedullatomaintaina highconcentrationofbothureaandurine,aswellasconserve water.IndividualswiththeJk(a−b−)phenotypehavelower urine-concentratingability.9–11 InUT-B-nullmice,long-term
UTBdeficiencywasassociatedtosevererenaldysfunctionand structuraldamage.12UT-Bisoformsarealsoimportantin
sev-eralcellularfunctions,includingureanitrogensalvageinthe colon,nitricoxidepathwaymodulationinthehippocampus, andnormalizationofthecardiacconductionsystem.13
Chronic kidney disease (CKD) is a major public health problem,definedasabnormalitiesofkidneystructureand/or function,presentforatleastthreemonthswithimplications on health.14 The adverse outcomes of the disease include
lossofkidneyfunction,cardiovasculardiseaseandpremature death.Besidesenvironmentalfactors,geneticabnormalities arealsoinvolved15includingvariationsintheMYH9(encoding
non-muscle myosin IIAheavy chain),16 APOL1
(apolipopro-teinL1),17–19NPHS1(nephrin),20andSHROOM3(shroomfamily
member3)21genes.
TherelationshipbetweentheKiddantigensand chronic kidneydiseaseremainsunknown.Therefore,theaimofthis studywastoinvestigatethedistributionofKiddphenotypes inpatientswith thechronic kidney disease anda possible associationofKiddantigenswiththedevelopmentofrenal disease.
Methods
Theethicaland methodological aspectsofthis study were approved by the Research Ethics Committee on Human
Beings from the Maringa State University (COPEP-UEM # 1.141.385/2014,CAAE43117115.0.0000.0104,accordingtothe ResolutionoftheBrazilianCouncilonHealth-CNS466/12.
Subjects
Thisretrospectivecase–controlstudyenrolled197unrelated patients with chronic kidney disease (CKD group) and 444 unrelated blood donors as a control group, living in the same geographical area as the patients. The individuals were attended and immunophenotypedbetween 2013 and 2015attheRegional BloodBank ofPatoBranco,southwest regionofParana(locatedinthesouthernregionofBrazilat 26◦13′46′′–09′′Sand52◦40′16′′–09′′W).
Serologictests
RedbloodcellphenotypingforKiddbloodgroupsystemswas performedonagelcard (ID-PerfilII–k-Kpa-Kpb-Jka-Jkb-ctl) usingmonoclonalantibodiesaccordingtothemanufacturer’s instructions (Diamed ID-Cards, DiaMed® AG, Switzerland). RBCsweresuspendedinBromelinsolution(BioRadID-Diluent 1)atafinalconcentrationof1:21or5%.
Statisticalanalysis
Theantigenandphenotypefrequencieswereestimatedand the data was tested for their fit to the Hardy–Weinberg equilibrium22 by calculating the expected frequencies of
the genotypes and comparing them with the observed values. The Student’s t-test was used to compare differ-encesbetweengroups.Statisticalcomparisonsbetweenthese groups were performedand the estimatedrisk of develop-ing CKD in individuals who have genetic polymorphisms was calculated by determining the Odds Ratio (OD) with a 95% of confidence interval (CI) adjusted for gender and age. Association tests were carried out to identify the codominant, dominant, recessive, overdominant and log-additive geneticinheritance models. p-Values≤0.05 by the Chi-square test with Yates correction and logistic regres-sion were considered statisticallysignificant. All statistical analyses were performed using the software OpenEpi pro-gramVersion2.3.1(http://www.openepi.com)andSNPStats23
(http://bioinfo.iconcologia.net/index.php).
Results
The Kidd phenotype frequency distribution in the stud-ied populations was in Hardy–Weinberg equilibrium (p -value=0.48:CKDandp-value=0.51:controls).
Table1–CharacteristicsoftheCKDpatientandcontrolindividuals.
Patients(n=197) Controls(n=444)
Total(>45yearsold) Total <45yearsold >45yearsold
n=197 n=444 n=349 n=94
n(%) n(%) n(%) n(%)
Gendera
Male 110(55.8) 219(49.3) 163(46.7) 56(59.6)
Female 87(44.2) 225(50.7) 186(53.3) 38(40.4)
Age(years)
Mean 62.8± 13.9 30.6 ± 11.1b 31.1± 7.2b 52.5± 5.4b
Ethnicgroup
Caucasian 104(100) 437(98.4) 342(98.0) 94(100)
Black 0 6(1.3) 6(1.7) 0
Mulatto 0 1(0.3) 1(0.28) 0
a p-Value>0.05(between-groupcomparisonby2test).
b p-Value<0.0001(betweenpatientsandcontrols.Student’st-test).
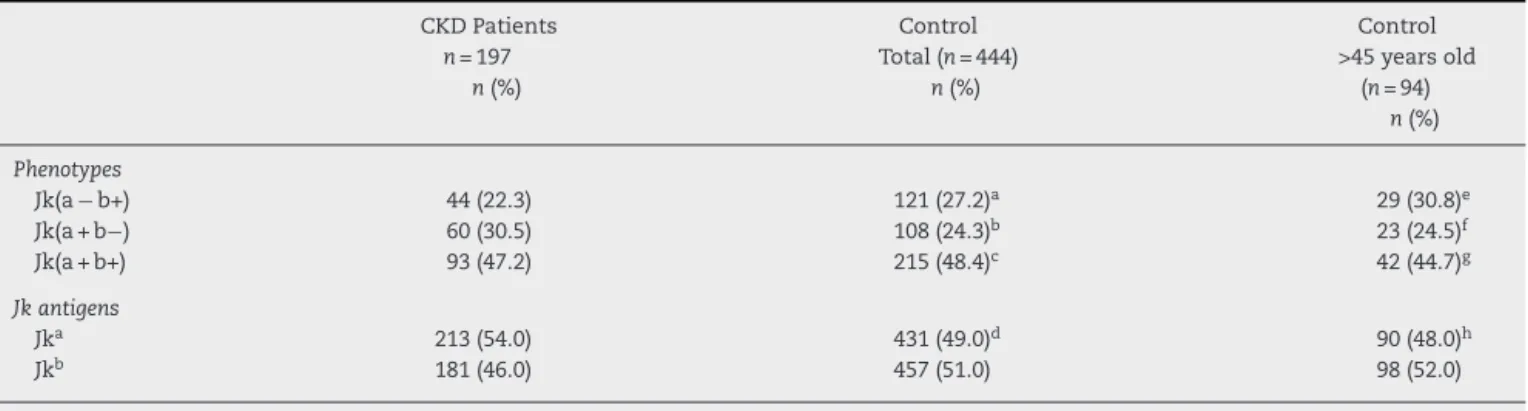
Table2–DistributionofJkantigenandphenotypefrequenciesinCKDpatientsandcontrols(totaland>45yearsold).
CKDPatients
n=197
n(%)
Control Total(n=444)
n(%)
Control >45yearsold
(n=94)
n(%)
Phenotypes
Jk(a−b+) 44(22.3) 121(27.2)a 29(30.8)e
Jk(a+b−) 60(30.5) 108(24.3)b 23(24.5)f
Jk(a+b+) 93(47.2) 215(48.4)c 42(44.7)g
Jkantigens
Jka 213(54.0) 431(49.0)d 90(48.0)h
Jkb 181(46.0) 457(51.0) 98(52.0)
ap-Value=0.32;bp-Value=0.55;cp-Value=1;dp-Value=0.16(CKDpatientsvs.controls−totalofsamples).
ep-Value=0.55;fp-Value=0.18;gp-Value=1;hp-Value=0.16(CKDpatientsvs.controls>45yearsold).
(n=94)foranalyses,consideringtheminimumagereported bypatients.Inthisgroup,themeanagewas52.54±5.36years (p-value<0.0001),and58.9%were malesand 41.1%females withallofthembeingself-declaredCaucasians.
Thedistributionsofantigenandphenotypefrequenciesfor theKiddbloodgroupsystemsinCKDpatientsandcontrols (totalgroupandgroup>45 yearsold)areshowninTable2. ThephenotypefrequenciesfortheKiddbloodgroupsystem inCKDpatientswere22.3%forJk(a−b+),30.5%forJk(a+b−) and47.2%forJk(a+b+).Forcontrols(totaland>45yearsold, respectively)thephenotypefrequencieswere27.2%and30.8% forJk(a−b+), 24.3%and 24.5%forJk(a+b−),and 48.4%and 44.7%forJk(a+b+).Thenullphenotypewasnotobservedin anyofthegroups.
DifferencesindistributionsoftheJkaandJkbantigenand phenotypefrequencieswerenotobservedwhencaseand con-trolgroupswerecomparedaccordingtoinheritancemodelsor afterlogisticregressionstratifiedbyage.
Discussion
Inthisassociation study,patientswithCKDon hemodialy-siswereanalyzedinordertoinvestigatethedistributionof JKphenotypesinpatientswithCKDandapossibleinfluence
ofJka andJkbantigensandphenotypesinthedevelopment ofrenaldisease.However,differencesbetweenJkaorJkb anti-genandphenotypefrequencieswerenotobservedbetween patientsandcontrols.
controlgroupwithanageofunder45arepossiblecandidates fordevelopingrenaldysfunctioninthefuture.Ontheother hand,incase–controlstudies,ideallythereshouldbeatleast onecontrolpercase,24 andthecontrolgroupofindividuals
olderthan45yearshadfewerpatientsthantheCKDGroup. However,theJka orJkb antigenand phenotypefrequencies inboth control groupsof this study were similar tothose frequenciesfoundinanotherBrazilianpopulation,25thereby
validatingtheresultsinthisstudy.
Theurea transporter in the kidney enables its medulla to maintain a high concentration of both urea and urine, as well as conserve water. Individuals with the Jk(a−b−) phenotypehad lowerurine-concentratingability.Inanimal models,long-termUTBdeficiencywasassociatedwithsevere renaldysfunctionandstructuraldamage.Ontheotherhand, geneticvariationsoftheSLC14A1genewereassociatedwith bladder cancer and,some genotypes were associated with highermorbidity,26–29 andrejectionafterrenaltransplant.30
However,wedidnotfindanynullallelesinCKDpatientsor controlsthatcouldbeidentifiedasariskfactorforthedisease. Inthis study,morethan 50% ofthe CKDpatients were homozygous carrying either Jk(a+b−) or Jk(a−b+) pheno-types,inagreementwiththeresultsreportedintheliterature forCaucasians.25Furthermore,nodifferenceswereobserved
betweenpatientsandcontrolsregardingthedistributionofJka orJkbantigenandphenotypefrequencies.Thus,Kidd pheno-typeswerenotassociatedtoCKD.
Conclusion
ThedistributionofKiddphenotypesfoundinthestudied pop-ulationwasasexpectedforCaucasiansandtherefore,Jkaand Jkbantigensandphenotypeswerenotfoundtobeassociated tothedevelopmentofCKD.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
Theauthorsappreciatetheparticipationandcooperationof allvolunteers(patientsandcontrols),aswellasoftheRegional BloodBankofPatoBrancoandHEMEPAR-Centrode Hematolo-giaeHemoterapiadoParaná,andImmunogeneticsLaboratory (LIG-UEM).
r
e
f
e
r
e
n
c
e
s
1. MöllerM,JöudM,StorryJR,OlssonML.Erythrogene:a databaseforin-depthanalysisoftheextensivevariationin36 bloodgroupsystemsinthe1000GenomesProject.BloodAdv. 2016;1(3):240–9.
2. AllenF,DiamondL,NiedzielaB.Anewbloodgroupantigen. Nature.1951;167:482.
3. DanielsG.Otherbloodgroups.In:RobackJD,CombsMR, GrossmanBJ,HillyerCD,editors.Technicalmanual.16thed.
Bethesda,MD:AmericanAssociationofBloodBanks;2008.p. 411–36.
4.OnoderaT,SasakiK,TsuneyamaH,IsaK,OgasawaraK, SatakeM,etal.JKnullallelesidentifiedfromJapanese individualswithJk(a−b−)phenotype.VoxSang. 2014;106(4):382–4.
5.HamiltonJR.Kiddbloodgroupsystem:areview. Immunohematology.2015;31(1):29–35.
6.SandsJM,GargusJJ,FröhlichO,GunnRB,KokkoJP.Urinary concentratingabilityinpatientswithJk(a− b−)bloodtype wholackcarrier-mediatedureatransport.JAmSocNephrol. 1992;2(12):1689–96.
7.InoueH,JacksonSD,VikulinaT,KleinJD,TomitaK,Bagnasco SM.IdentificationandcharacterizationofaKidd
antigen/UT-Bureatransporterexpressedinhumancolon.Am JPhysiolCellPhysiol.2004;287(1):C30–5.
8.StewartG.TheemergingphysiologicalrolesoftheSLC14A familyofureatransporters.BrJPharmacol.
2011;164(7):1780–92.
9.SandsJM.Molecularmechanismsofureatransport.JMembr Biol.2003;191(3):149–63.
10.TimmerRT,KleinJD,BagnascoSM,DoranJJ,VerlanderJW, GunnRB,etal.LocalizationoftheureatransporterUT-B proteininhumanandraterythrocytesandtissues.AmJ PhysiolCellPhysiol.2001;281(4):C1318–25.
11.LucienN,Sidoux-WalterF,RoudierN,RipocheP,HuetM, Trinh-Trang-TanMM,etal.Antigenicandfunctional propertiesofthehumanredbloodcellureatransporter hUT-B1.JBiolChem.2002;277(37):34101–8.
12.ZhouL,MengY,LeiT,ZhaoD,SuJ,ZhaoX,etal.
UT-B-deficientmicedeveloprenaldysfunctionandstructural damage.BMCNephrol.2012;13:6.
13.ShayakulC,Clémenc¸onB,HedigerMA.Theureatransporter family(SCL14):physiological,pathologicalandstructural aspects.MolAspectsMed.2013;34(2–3):313–22.
14.Chapter1:DefinitionandclassificationofCKD.KidneyInt Suppl(2011).2013;3(1):19–62.
15.PattaroC,TeumerA,GorskiM,ChuAY,LiM,MijatovicV,etal. Geneticassociationsat53locihighlightcelltypesand biologicalpathwaysrelevantforkidneyfunction.Nat Commun.2016;7:10023.
16.NelsonGW,FreedmanBI,BowdenDW,LangefeldCD,AnP, HicksPJ,etal.DensemappingofMYH9localizesthe strongestkidneydiseaseassociationstotheregionofintrons 13to15.HumMolGenet.2010;19(9):1805–15.
17.FreedmanBI,MureaM.TargetorgandamageinAfrican Americanhypertension:roleofAPOL1.CurrHypertensRep. 2012;14(1):21–8.
18.ParsaA,KaoWH,XieD,AstorBC,LiM,HsuCY,etal.APOL1 riskvariants,race,andprogressionofchronickidneydisease. NEnglJMed.2013;369(23):2183–96.
19.ChenTK,EstrellaMM,ParekhRS.Theevolvingscienceof apolipoprotein-L1andkidneydisease.CurrOpinNephrol Hypertens.2016;25(3):217–25.
20.BonomoJA,NgMC,PalmerND,KeatonJM,LarsenCP,HicksPJ, etal.Codingvariantsinnephrin(NPHS1)andsusceptibilityto nephropathyinAfricanAmericans.ClinJAmSocNephrol. 2014;9(8):1434–40.
21.KhaliliH,SullA,SarinS,BoivinFJ,HalabiR,SvajgerB,etal. DevelopmentaloriginsforkidneydiseaseduetoShroom3 deficiency.JAmSocNephrol.2016;27(10):
2965–73.
22.GuoSW,ThompsonEA.Performingtheexacttestof Hardy–Weinbergproportionformultiplealleles.Biometrics. 1992;48(2):361–72.
24.DorakTM.Basicpopulationgenetics.Availablefrom:
http://www.dorak.info/genetics/popgen.html[cited21.02.17]. 25.GuelsinGA,SellAM,CastilhoL,MasakiVL,deMeloFC,
HashimotoMN,etal.GeneticpolymorphismsofRh,Kell, DuffyandKiddsystemsinapopulationfromtheStateof Paraná,southernBrazil.RevBrasHematolHemoter. 2010;33(1):21–5.
26.Garcia-ClosasM,YeY,RothmanN,FigueroaJD,MalatsN, DinneyCP,etal.Agenoma-wideassociationstudyofbladder canceridentifiesanewsusceptibilitylocuswithinSLC14A1,a ureatransportergeneonchromosome18q12.3.HumMol Genet.2011;20(21):4282–9.
27.RafnarT,VermeulenSH,SulemP,ThorleifssonG,AbenKK, WitjesJA,etal.Europeangenome-wideassociationstudy
identifiesSLC14A1asanewurinarybladdercancer susceptibilitygene.HumMolGenet.2011;20(21): 4268–81.
28.KoutrosS,BarisD,FischerA,TangW,Garcia-ClosasM, KaragasMR,etal.Differentialurinaryspecificgravityasa molecularphenotypeofthebladdercancergenetic associationintheureatransportergene,SLC14A1.IntJ Cancer.2013;133(12):3008–13.
29.RanJ,WangH,HuT.Clinicalaspectsofureatransporters. SubcellBiochem.2014;73:179–91.