Porto
Biomedical
Journal
h tt p://w w w . p o r t o b i o m e d i c a l j o u r n a l . c o m /Review
article
A
biopsychosocial
approach
to
the
interrelation
between
motherhood
and
women’s
excessive
weight
Ana
Henriques
a,∗,
Ana
Azevedo
a,baEpidemiologyResearchUnit(EPIUnit)–InstituteofPublicHealth,UniversityofPorto,Porto,Portugal
bDepartmentofClinicalEpidemiology,PredictiveMedicineandPublicHealth,UniversityofPortoMedicalSchool,Porto,Portugal
a
r
t
i
c
l
e
i
n
f
o
Articlehistory: Received27November2015 Accepted16February2016 Keywords: Excessiveweight Motherhood Weightcontrola
b
s
t
r
a
c
t
Portugalischaracterizedbyahighprevalenceofoverweightandobesityamongwomen,whoseweight increasesmostrapidlyinearlyadulthood.Individualgeneticfeaturesandbehaviours,alongwithsocial, culturalandenvironmentalfactorsinteractincomplexrelationshipswithbodyweightandwithits variationthroughouttime.Motherhoodmaytriggeranincreaseinweight,potentiallyinfluencingthe associationsbetweenexcessiveweightandseveralotherhealthdeterminants.Takingintoaccountthe qualityofprenatalcarewithinPortugal’shealthcaresystem,regardingcoverageandsuccessinimproved outcomes,wetheoreticallydemonstratewhypregnancyandmotherhoodshouldbeseenasopportunities forpreventionandwhyadeeperknowledgeabouttheinterplayofbiological,socialand psychologi-caldeterminantsofweightatthisstageoflifecanbeusefultodesignmoreeffectiveweightcontrol interventionstowardsthispopulation.
©2016PublishedbyElsevierEspa ˜na,S.L.U.onbehalfofPBJ-Associac¸˜aoPortoBiomedical/Porto BiomedicalSociety.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http://
creativecommons.org/licenses/by-nc-nd/4.0/).
Women’sweightbefore,duringandafterpregnancy
Motherhoodis oneofthemostchallengingexperiences that canoccurinwomen’slifeand itcanbeconcomitantly distress-ingandmeaningful.Theseambivalentfeelingsarenotnecessarily aproblem,butmoreresearchisneededtounderstandtheir speci-ficitiesandhowtheycaninteractwithweightmanagementinthis periodoflife.Thegrowingnumber ofobesewomenworldwide hasmanyimplications,notonlyonmother’shealthoutcomesbut alsofortheirchildren,asdemonstratedbytheassociationbetween prepregnancyobesityandcertainmajorbirthdefects1andahigher
likelihoodofhavingmacrosomicinfants.2Additionally,caesarean
deliveryriskisincreasedby50%inoverweightwomenandismore thandoubleforobesewomencomparedtowomenwithnormal bodymassindex(BMI).3
Thepostpartumperiodcanbecriticalforthedevelopmentof obesityinmidlife.Evidenceconsistentlyshowsthatexcessive ges-tationalweightgain(GWG)contributestohigherpostpartumbody weight4–6andthatoverweightandobesewomenhavemorethan
doublethechancetoexceedtheweightgainrecommendations duringpregnancythanotherBMIgroups.2,7Moreover,excessive
∗ Correspondingauthor.
E-mailaddress:alhenriques@med.up.pt(A.Henriques).
GWGisassociatedwithabdominaladiposity8yearsafterdelivery, whichmayincreaseawoman’sriskofcardiovascularandmetabolic diseases.8
Several pregnancy cohort studies from developed countries havereportedindependentdirectassociationsbetween prepreg-nancybodyweightorBMIandpostpartumweightretention.9,10
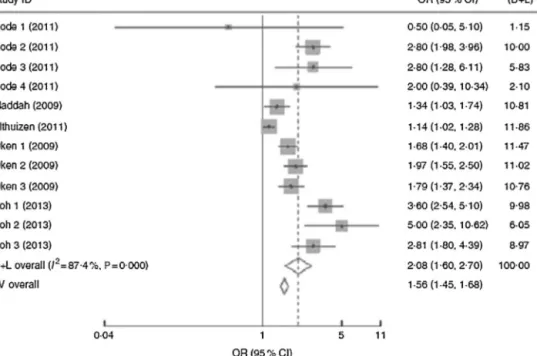
However,arecentmeta-analysisanalyzedtheassociationofGWG orprepregnancyBMIwithpostpartumweightretentionand,as illustratedinFig.1,GWG,ratherthanprepregnancyBMI, deter-minestheshorter-orlonger-termpostpartumweightretention. Whenpostpartumtimespanswerestratifiedinto1–3months,3–6 months,6–12months,12–36monthsand≥15years,the associa-tionbetweeninadequateGWGandpostpartumweightretention fadedovertimeandbecameinsignificantafter15years.11
Most studiesconducted sofarfocus onweight changeonly until thefirst year postpartum, and few studies have obtained serial measurements for longer periods to assess patterns of weightchange.Characterizationoftheinterrelationshipsbetween prepregnancybodyweight,GWG andpostpartumweight reten-tion is essential for a deeper knowledge of weight changes afterpregnancyandobesityratesinchildbearingage.Giventhe modifiable nature of this risk factor, thepreconception, prena-tal, and postpartum periods may present critical windows to implement interventions to prevent weight retention and the developmentofoverweightandobesityinwomenofchildbearing age.12
http://dx.doi.org/10.1016/j.pbj.2016.04.003
2444-8664/©2016PublishedbyElsevierEspa ˜na,S.L.U.onbehalfofPBJ-Associac¸˜aoPortoBiomedical/PortoBiomedicalSociety.ThisisanopenaccessarticleundertheCC BY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Fig.1. Forestplotofthestudiesontheriskofpostpartumweightretentionof≥5kgforwomenwithexcessivegestationalweightgain(GWG)vs.womenwithadequate GWG.Thestudy-specificORand95%CIarerepresentedbythegreysquareandhorizontalline,respectively;thesizeofthedatamarker(greysquare)isproportionaltothe weightofthestudyinthemeta-analysis(note:weightsarefromrandom-effectsanalysis).ThecentreoftheopendiamondpresentsthepooledORanditswidthrepresents thepooled95%CI.11ReprintedwiththepermissionofCambridgeUniversityPress.
Increasingparitycontributestothelong-termdevelopmentof obesityinwomen13–15butthisrelationshipdiffersbymaternalBMI
inyoungadulthood,numberofbirths,race-ethnicityandlengthof follow-up.FindingsfromarepresentativecohortfromtheUnited StatesofAmerica(USA)showedthatblackandwhiteprimiparae andmultiparaetendedtohavegreaterBMIincreasesthan nulli-paraeover10years,thisassociationbeingstrongeramongwomen withhighBMIbeforepregnancy.However,25yearslater,thesame studyshowedthat onlyblack womenwho wereoverweight at baselineanddeliveredmorethan onechildgained significantly moreweightthanthosenotgivingbirth.16Womenoftenreport
theirobesitytobetriggeredbypregnancy–asmanyas40–50% in oneSwedish study. Yet,for 30% of thewomen in the same study,pregnancywasassociatedwithweightloss.17Additionally,
placeofresidence,ethnicity,aswellasindividualsocioeconomic position(SEP)andlifestylefactorscanconsiderablyexplain this association.18,19Allofthesedataalludetoacomplexparity–weight
relationshipforwomenwitharangeofconfoundingfactorsthatact acrossthelifecourse,withthepossibilityforfurthervariations.20
Thus, further researchis needed toconfirm the links between parityandweightgain,aswellasmoreinformationregarding con-foundersofthisassociationframedinsocialandcurrenteconomic conditions.
Theriskofweightgainisnotequalthroughoutallpregnancies. Inlargecohortstudies,whencomparingnulliparouswith primi-parouswomen,weightgainduetochildbearingwasgreatestafter thefirstbirth,andweightgainwasgreaterwithincreasingbaseline maternalbodyweight.Averageweightgainassociatedwith hav-ingafirstchildwas3–6kgamongwomenwhowereoverweight beforepregnancy,andabout1kgamongwomenwithnormalBMI. Afterthefirst pregnancy, weightgain is smallerin subsequent pregnancies.12,21,22Furthermore,multiparityispositively
associ-atedwithabdominalgirthfrompreconceptiontoseveralyearsafter delivery.21,23
Despite somedisparities, evidence supports that substantial weightgainassociatedwithchildbearingisanimportantrisk fac-torforthedevelopmentofoverweightandobesityinadultwomen.
Futurestudiesshouldidentifywomenmoresusceptibletobenefit frominterventionstopreventweightgainandwhicharethe crit-icalperiodstointervenemosteffectively:before,duringorafter pregnancy.
Theimpactofpsychosocialdeterminantsonweight,around motherhood
Sincesocial10andpsychologicalcharacteristics24haveimpact
onmaternalexcessiveweight,thepsychosocialcontextshouldbe studiedindepth.Areviewoftheimplicationsofbodyimageand socioeconomicpositionisprovidedbelow.
Bodyimage
Pregnancy,due toitsconcomitantchanges in bodysize and shape,canhaveasignificantimpactonawoman’sbodyimage.25
Thisisoftenthefirsttimeweightgainisexpectedandaccepted andsomewomenviewbodychangesastransientanduniquetothe childbearingendeavoursotheyareabletoassimilatethesechanges withoutdistress.26
Researchresultsonbodyimageinpregnancyhavebeen con-tradictory,withsomestudieshighlightingthat womenareable toassimilatethebodilychangesofpregnancywithoutanegative shiftinbodyimagesatisfaction(BIS),27,28andotherstudies
find-ingadecreasedBISduringpregnancy29andpostpartum.30Also,
prepregnancyBMIhasanimpactonBISduringpregnancy,with overweightwomenreportinganincreaseintheirsatisfactionand womenwithnormalBMIreportingadecrease.29Thosewhohad
beenoverweightbeforetheirpregnancymayviewtheirpregnancy asexcusingthemfromunpleasantcommentsorfeeling uncomfort-ableinactivitiesexposingtheirbody,suchasswimming.31
Inthepostpartumperiod,despitesomevariation,bodyimage isgenerallymorenegative,whenwomen’sconstructionsoftheir postpartumbodyindicatethatoncethebabywasborn,theyno longer perceived any excuse to not adhere to their perceived sociallyconstructedidealsilhouette.32Harrisandcolleaguesalso
foundthatwomenwhowerelesssatisfiedwiththeirbodies post-partumhadsignificantlygreaterlongtermweightgainsthanthose womenwhodisplayednoincreaseindissatisfactionwiththeir bod-iesafterpregnancy.14Onepossiblereasonforthisdisappointment
isthatwomen(especiallyprimiparouswomen)tendtoexpectthat theirbodieswillreturntotheirpre-pregnancyweightandshape shortlyafterthebirthoftheirchild.33
Arecentreviewsynthesizedtheexistingqualitativeliterature describingwomen’sexperiencesoftheirpregnancyand postpar-tumbodyimage. Hodgkinsonandcolleagues25 highlightedthat
women’sperceptionoftheirpregnancybodyimageisvariedand dependsonthestrategiestheyusetoprotectagainstsocial con-structionsoffemalebeauty.Womenoftenperceivedthepregnant body tobeout oftheircontrol andas transgressingthe physi-calmanifestationofthesociallyconstructedideal,againstwhich they tried to protect their BIS. Body dissatisfaction dominated thepostpartumperiod,emphasizingthewomen’sneedfor addi-tionalsupportatthismoment.Moreover,healthprofessionalsare reportedtofeeluncomfortableaboutdiscussingweightasanaspect ofbodyimageduetolackofknowledgeandfearofbeing consid-eredinsensitive.34However,sinceduringpregnancywomenare
morereceptivetoconversationsaboutweight-relatedaspectsof theirbodyimage,communicationskillstrainingcouldincrease pro-fessionals’confidenceinexploringwomen’sbodyimageinorder toimprovetheirweightmanagementstrategiesindependentlyof theirBMI.25
WhileitseemsclearthatBISbeforepregnancyhasa consid-erableimpactonpostpartumweightchanges,furtherresearchis neededtoassessifthissameconstructcaninfluenceweightovera longer-term.
Socioeconomicposition
Femalereproductivehealthishighlysensitivetothephysical andsocialenvironmentthroughoutlife.Womenarecurrentlyless likelytobemarriedandmorelikelytobesingleorcohabiting,35,36
morewomenareremainingchildlessorhavingfewerchildrenand theproportionofwomen’slivesspentrearingtheirchildrenhas beenreduced.37Ifsocialfactorschange,theirimpactonwomen’s
reproductivelifecanalsochange;therefore,adeepstudyofthis relation,togetherwithpsychologicalandbiologicalattributes,is stillachallengetobefaced.
MaternalSEPisknowntobeastrongcorrelateofnumerous maternalandchildhealthoutcomes.LowindividualSEP(e.g. edu-cationandincome)hasbeenassociatedwithadversepregnancy andbirthoutcomes38,39anddelayedprenatalcare.40Arecentlarge
population-basedstudycomparedthedirectionandmagnitudeof individualandneighbourhoodsocialinequalitiesacrossmultiple maternalandchildhealthoutcomes(maternalandinfanthealth statusindicators;prenatalcare;maternalexperienceoflabourand delivery;neonatalmedicalcare;andpostpartuminfantcareand maternalperceptionsofhealthcareservices)andrevealedthatSEP measureshadstrongerassociationswithoutcomesbelongingto thehealthstatusofthemotherandinfant,asopposedtotheother groups.Themagnitudeofmaternalandchildhealthinequalities washigherwhenindividual-levelSEPwasusedthanwhen con-sideringneighbourhoodSEP.Inparticular,educationshowedthe greatestgradientscomparedtohouseholdincome,neighbourhood SEP,andcombinedSEP(combinationoflowandhighindividual andneighbourhoodSEP).41
ArelationbetweenSEPandobesityhasbeenwellestablished foralongtime,42alsoinchildbearingwomen,43withthosewho
havealowerSEPbeingtheoneswithahigherriskofbeingobese. However,somespecificitiesofthisassociationconsideringyoung adultwomenremainunclear.Inadulthood,reproductionmayhave anaddedinfluenceonobesityriskinwomen,althoughresearchis
lackingonhowadultinfluencescombine,namelysocialand psy-chologicalones,forthedevelopmentofexcessiveweightinthis particularperiod.
Additionally,researchonchildhoodgrowthhaspointedtothe possibilitythatearlylifemaybeanimportantstageinthe devel-opmentofobesityandlongitudinalstudiesconsistentlyshowthat alowerSEPinchildhoodincreasestheriskofexcessiveweightin adulthood.44TheseassociationsbetweenchildhoodSEPandadult
healtharealsoobservedinthecontextofmotherhood.IntheBritish 1958birth cohortstudy,45 it wasobservedthat,as thelevelof
povertyinchildhoodincreases,theproportionofwomenhaving theirfirstbabybytheageof20alsoincreases.
Thiscontinuityindisadvantagethroughoutlifeisanimportant partofthelinkbetweenchildhooddisadvantageandpooradult health,withSEPacrosschildhoodand adulthoodemergingasa stronger predictorofadulthealth thanSEPatanyone pointin time.45
Socialtrajectoryisalifelongevolutionofthevolumeand com-positionofanindividual’scapital(social,cultural,economicand/or symbolic),combinedwithhis/herparents’assetvolumeand struc-tureandcanbedescribedasupward,downwardorstationary.46
Most of the findings concerningobesity and socioeconomic characteristicshavebeenbasedonwomen’sSEPinadulthoodbut, recently,evidenceisemergingabouttheimpactof intergenera-tionalsocialtrajectorytakingintoaccountalifecourseperspective. Inordertostudytheinfluenceofsocialclassinchildhood,young adulthoodandmiddleage,andintergenerationalmobility,onadult centralandtotalobesity,astudywasconductedusinga population-basedbirthcohort.Inwomenat53years,father’ssocialclasswas inverselyassociatedwithallmeasuresofobesity,bothadultsocial classes(atages26and43years)wereinverselyassociatedwithall obesitymeasuresatage53andwomenwithanupward intergener-ationalsocialmobilityhadlowerlevelsofcentralandtotalobesity comparedwiththosewhoremainedinthesamesocialclassastheir father.47
Changes in social circumstances,or intergenerational move-ment betweensocial classes,might entaila transitionin terms ofprioritiesand resourcesrelatedtoweightandappearance,or ashiftinexperienceofsocialnormsregardingtheappealof par-ticularbodytypes,48particularlywhenconsideredinthecontext
ofwomen whohave recentlygivenbirth.Knowing thatsociety influenceswomen’sperceptionofgoodorbadappearance,future studiesshouldbetterassessthesocialdeterminantsofBISin child-bearingwomen,consideringalifecourseapproach.
Motherhoodasanopportunityforprevention
Some authors defend that the preconception period should be seen as a privileged time for prediction and prevention of noncommunicablediseases,thus notonly improvingpregnancy outcomesandmaternalhealth,butalsopromotinglong-term ben-eficialeffectsforboththemotherandthechild.49Prepregnancy
weightlosscanreduceobesity-relatedcomplications,whichcan haveaconsiderableimpactonimprovingobesity-relatedperinatal complications–gestationaldiabetesmellitus,hypertensive disor-ders,macrosomia,andlargeforgestationalagebabies.50
Women’s health in Portugal hasexperienced a huge overall improvementsincethelate1970sandtheimplementationofthe National Health System, which ensures all citizens nearly free accesstoprimarycarecentresandpublichospitals.51Moreover,
prenatalcareisoneofPortugal’shealthcaresystem’smost suc-cessfulareas,withpractically100%coverageandadequateprenatal careinthevastmajorityofpregnancies.52However,astudy
per-formed in the north of the country showed that, whilst good prenatalsurveillanceexists,only27%ofthepuerperalwomenhad
• The romanticized image • The motherself • Type of mothering received • The influential ‘others’ • The ‘wished-for’ baby • Relationship with baby • Partner’s involvement • Self and others • Confidence in body • Labour as indicator of motherliness • Dealing with uncertainty • Information seeking Parental self-efficacy Concept of motherhood Mother-infant dyad Anticipated social support
Fig.2. Themesandsub-themesidentifiedwithinthe‘Expectationsandbeliefsaboutmotherhoodviews’.57ReprintedwiththepermissionofElsevier.
preconceptioncare.53Also,astudyperformedinmothersofthe
GenerationXXIbirthcohortshowedanadversecardiovascularrisk profilesincethepreconceptionperiod,54supportingtheideathat
interventionsshouldstartearlierinchildbearingwomen.
Thelabel“teachable moment”hasbeenusedtocharacterize lifetransitionsorhealtheventsthatincreaseperceptionsof per-sonalriskandoutcomeexpectancies,promptstrongaffectiveor emotional responses, and redefine self-concept or social roles. Inotherwords,a cognitiveresponseprecedesmotivation,skills acquisitionandself-efficacythatinturn,increasethelikelihood ofceasingadverselifestyles.Additionalkeyfactorstoconsiderare predisposingfactorssuchasage,dispositionalandcultural charac-teristicsthatmayinfluenceanindividual’scognitiveandemotional response.Pregnancyhasbeenwidelyreferred toasa teachable momentbecauseofmothers’strongmotivationtoprotectthe well-beingofthefoetusandstrongsocialpressuretoavoidunhealthy habits,suchassmokingduringpregnancy.55,56
Somepsychological issues should also be highlighted when discussing a pregnancy’simpact onwomen’s life. A qualitative studyexploredbeliefsand expectationsaboutmotherhood, and the main themes are illustrated in Fig. 2. Since a discrepancy betweenwomen’sexpectationsandrealitywasfound,a psycho-logicalpreparation for motherhoodshouldbe consideredwhen preparingwomenfortheirnewrole.Suchpreparationpromotesa sensibleimageofmotherhood,theinfant,thenoveltyofthefuture andrelationshipswithothers,anddiscussingthesethemesmaybe particularlyrelevanttowomenvulnerabletopostnatal psycholog-icaladjustmentdifficulties.57
AccordingtoastudyperformedintheUnitedKingdombetween 1998and2003,therewasasignificantreductioninsmoking, alco-holconsumptionand intakeofcaffeinateddrinkswhen women becamepregnant,althoughlittlechangeoccurredinfruitsand veg-etablesintake.58InPortuguesemothers,althoughalmosthalfof
smokersceasedtobaccoconsumptionduringpregnancy, approxi-matelytwothirdsresumedsmokingwithin4yearsafterdelivery,59
leadingustobelievethat,althoughpregnancyenhancesthe per-ceivedneedofadoptinghealthylifestyles,thatdoesnotmeanthat healthyhabitswillpersistthroughouttime.Sincefertileagewomen arepronetochangehealthyhabitswhentheyreceivehealthcare provider’sadvices,60interventionstothissegmentofthe
popula-tionshouldberestructured,focusingmoreonwomen’sintrinsic motivationsandexpectations,whichisprovedtoresultin long-lastingbehaviourchange.61
Insummary, weightmanagement before, duringand after a pregnancyhasadvantages for both mother andchild.
Monitor-ingofprepregnancyBMI,GWG,andpostpartumweightwillallow theidentificationofwomenwhoaremoresusceptibleofhaving aninadequateweightthroughoutchildbearingyears. Preconcep-tionisanimportantperiodandobesewomenshouldbetargeted forinterventionbeforetheygetpregnantforthefirsttime. Like-wise,healthcareprovidersinvolvedinthecareofpregnantwomen shouldbetrainedtoprovideamoreeffectiveapproachforweight control.
Metabolicfeaturesafterpregnancy:thehealthyobesity phenotype
The numbersregarding obesity are alarming,largely due to itsassociationwithseveralcardiovascular diseases.However, a healthyobesephenotypehasbeenrecentlyidentifiedandthese individualsappeartobeatnoincreasedcardiovascularrisk.62,63
This clinical condition,termed benign obesityor metabolically healthyobesity,isrestrictedtoauniquesubsetoftheobese pop-ulationwhich, despiteexcessive BMI, are insulin sensitive and haveanormalbloodpressure,lipid,inflammationandhormonal profile.62–66 The relevance of establishing such a phenotype is
underlinedbydatathatsuggeststhatweightlossamonghealthy obese may adversely impact their favourable cardiometabolic profile.67
Theabsenceofauniformdefinitionforthissubtypeofobesity isoneofthemainlimitationsofthistopic,withprevalences rang-ingfrom6%to37%,68–70dependingonthecriteriatodefinethe
phenotype.However,evenwhenuniquecriteriaareused, consider-ablevariabilityintheprevalenceofhealthyobesityisfoundacross differentEuropeancountries71and,tothebestofourknowledge,
therearenoestimatesforPortugal.Normally,metabolicallyhealthy obesepersonshavefamilymemberswithuncomplicatedobesity, earlyonsetobesity,fastingplasmainsulinwithinanormalrange andanormaldistributionoftheexcessfat.72Additionally,some
lifestylefeaturesareassociatedwiththismetabolicprofile,suchas moderateandhigherlevelsofphysicalactivityandhigherdietary quality.70
Somecontroversyexistsconsideringtherelevanceofthis phe-notype.Arecentsystematicreviewandmeta-analysisshowedthat, comparedwithmetabolicallyhealthynormalweightindividuals, obesepersonsareatanincreasedriskofadverselong-term out-comesevenintheabsenceofmetabolicabnormalities,suggesting thatthereisnohealthypatternofincreasedweight.73Also,another
studythatevaluatedthe3-yearincidenceofcardiometabolicrisk factorsconcludedthat anincrease inBMI duringthefollow-up
period wassignificantly associated withthe occurrence of car-diometabolicalterations.74Moreresearchconcerningthissubject
isstillneededandlongerlongitudinalanalysesshouldbeprovided inordertoclarifyiftheseindividualsareprotectedduringtheir entirelifeorwhetherhealthyobesitysimplyrepresentsdelayed onsetofobesityrelatedcardiometabolicproblems.Also,mostof thestudiesthatassessedhealthyobesityusedsamplescomprising womenabove40yearsofage66,75,76andinformationconcerning
childbearingwomenisstilllacking.
Theincreaseindepositionoffatinabdominalvisceraladipose tissue is favouredafter pregnancy,due to increasedabdominal compliance,renderingwomenmoresusceptibletoabdominal obe-sity after childbirth.13 Abdominal fat distribution, visceral and
ectopicfataccumulationarealsokeycharacteristicsforthe devel-opmentofunhealthyobesity.77 Thus,itwould beinterestingto
characterizetheobesityphenotypein womenwho hada child, toassesstowhich extenttheirobesityis healthyor is convey-ing a higher risk of CVD,thus supportingor not the need for preventiveactiondirectedatthissegmentofthepopulation. Fur-therstudiesexaminingdifferentsubtypesofobesitywillallowfor understandingobesity’s heterogeneousnaturethat couldresult inmoreappropriateweightlossrecommendations,evenamong childbearingwomen.
Conclusion
Inconclusion,theaccumulatedevidencesuggeststhatthereare severalfactorsthatcouldleadachildbearingwomantobe over-weightor obeseand a biopsychosocialapproach contributesto understandtheserelationscomprehensively.
Pregnancyhasbeenwidelyreferredtoasateachablemoment andfutureresearchshouldidentifywomenmoresusceptibleto benefit from interventions to prevent weight gain during this period,preferably,startingatthepreconceptionperiod.BIS, socioe-conomiceconomiccharacteristicsacrossthelifespanandmetabolic featuresshouldbeconsideredwhendesigningfutureinterventions forweightmanagementtargetingthisspecificpopulationand lon-gitudinalresearchisneededinordertoassessiftheimpactofthese variablesonweightisobservedthroughouttime.
Conflictsofinterest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
AgrantfromFundac¸ãoparaaCiênciaeTecnologiaisgratefully acknowledged(SFRH/BD/72723/2010).
References
1.CorreaA,MarcinkevageJ.Prepregnancyobesityandtheriskofbirthdefects:an update.NutrRev.2013;71Suppl.1:S68–77.
2.BrawarskyP,StotlandNE,JacksonRA,Fuentes-AfflickE,EscobarGJ,Rubashkin N,etal.Pre-pregnancyandpregnancy-relatedfactorsandtheriskofexcessive orinadequategestationalweightgain.IntJGynaecolObstet.2005;91:125–31.
3.PoobalanAS,AucottLS,GurungT,SmithWC,BhattacharyaS.Obesityasan independentriskfactorforelectiveandemergencycaesareandeliveryin nulli-parouswomen–systematicreviewandmeta-analysisofcohortstudies.Obes Rev.2009;10:28–35.
4.HeX,HuC,ChenL,WangQ,QinF.Theassociationbetweengestationalweight gainandsubstantialweightretention1-yearpostpartum.ArchGynecolObstet. 2014;290:493–9.
5.OlsonCM,StrawdermanMS,HintonPS,PearsonTA.Gestationalweightgainand postpartumbehaviorsassociatedwithweightchangefromearlypregnancyto 1ypostpartum.IntJObesRelatMetabDisord.2003;27:117–27.
6.EndresLK,StraubH,McKinneyC,PlunkettB,MinkovitzCS,SchetterCD,etal. Postpartumweightretentionriskfactorsandrelationshiptoobesityat1year. ObstetGynecol.2015;125:144–52.
7.Chasan-TaberL,SchmidtMD,PekowP,SternfeldB,SolomonCG,Markenson G.PredictorsofexcessiveandinadequategestationalweightgaininHispanic women.Obesity(SilverSpring).2008;16:1657–66.
8.McClureCK,CatovJM,NessR,BodnarLM.Associationsbetweengestational weightgainandBMI,abdominaladiposity,andtraditionalmeasuresof car-diometabolicriskinmothers8ypostpartum.AmJClinNutr.2013;98:1218–25.
9.HarrisHE,EllisonGT,HollidayM,LucassenE.Theimpactofpregnancyonthe long-termweightgainofprimiparouswomeninEngland.IntJObesRelatMetab Disord.1997;21:747–55.
10.ParkerJD,AbramsB.Differencesinpostpartumweightretentionbetweenblack andwhitemothers.ObstetGynecol.1993;81Pt1:768–74.
11.RongK,YuK,HanX,SzetoIM,QinX,WangJ,etal.Pre-pregnancyBMI,gestational weightgainandpostpartumweightretention:ameta-analysisofobservational studies.PublicHealthNutr.2014:1–11.
12.GundersonEP.Childbearingandobesityinwomen:weightbefore,during,and afterpregnancy.ObstetGynecolClinNorthAm.2009;36:317–32,ix.
13.GundersonEP,SternfeldB,WellonsMF,WhitmerRA,ChiangV,Quesenberry CPJr,etal.Childbearingmayincreasevisceraladiposetissueindependentof overallincreaseinbodyfat.Obesity(SilverSpring).2008;16:1078–84.
14.HarrisHE,EllisonGT,ClementS.Relativeimportanceofheritablecharacteristics andlifestyleinthedevelopmentofmaternalobesity.JEpidemiolCommunity Health.1999;53:66–74.
15.LuotoR,MannistoS,RaitanenJ.Ten-yearchangeintheassociationbetween obesityandparity:resultsfromtheNationalFINRISKPopulationStudy.Gend Med.2011;8:399–406.
16.AbramsB,HeggesethB,RehkopfD,DavisE.Parityandbodymassindexin US women:aprospective25-yearstudy.Obesity(SilverSpring).2013;21: 1514–8.
17.RossnerS.Weightgaininpregnancy.HumReprod.1997;12Suppl.1:110–5.
18.LeeSK,SobalJ,FrongilloEA,OlsonCM,WolfeWS.Parityandbodyweightin theUnitedStates:differencesbyraceandsizeofplaceofresidence.ObesRes. 2005;13:1263–9.
19.Wolfe WS, Sobal J, Olson CM, Frongillo EA Jr. Parity-associated body weight:modificationbysociodemographicandbehavioralfactors.ObesRes. 1997;5:131–41.
20.MishraG,KuhD.Commentary:therelationshipbetweenparityandoverweight –alifecourseperspective.IntJEpidemiol.2007;36:102–3.
21.GundersonEP,MurtaughMA,LewisCE,QuesenberryCP,WestDS,SidneyS. Excessgainsinweightandwaistcircumferenceassociatedwithchildbearing: theCoronaryArteryRiskDevelopmentinYoungAdultsStudy(CARDIA).IntJ ObesRelatMetabDisord.2004;28:525–35.
22.RosenbergL,PalmerJR,WiseLA,HortonNJ,KumanyikaSK,Adams-Campbell LL.Aprospectivestudyoftheeffectofchildbearingonweightgainin African-Americanwomen.ObesRes.2003;11:1526–35.
23.TroisiRJ,WolfAM,MasonJE,KlinglerKM,ColditzGA.Relationofbodyfat dis-tributiontoreproductivefactorsinpre-andpostmenopausalwomen.ObesRes. 1995;3:143–51.
24.BogaertsA,DevliegerR,VandenBerghBR,WittersI.Obesityandpregnancy,an epidemiologicalandinterventionstudyfromapsychosocialperspective.Facts ViewsVisObgyn.2014;6:81–95.
25.HodgkinsonEL,SmithDM,WittkowskiA.Women’sexperiencesoftheir preg-nancyandpostpartumbodyimage:asystematicreviewandmeta-synthesis. BMCPregnancyChildbirth.2014;14:330.
26.RichardsonP.Women’sexperiencesofbodychangeduringnormalpregnancy. MaternChildNursJ.1990;19:93–111.
27.DaviesK,WardleJ.Bodyimageanddietinginpregnancy.JPsychosomRes. 1994;38:787–99.
28.BoscagliaN,SkouterisH,WertheimEH.Changesinbodyimagesatisfaction dur-ingpregnancy:acomparisonofhighexercisingandlowexercisingwomen.Aust NZJObstetGynaecol.2003;43:41–5.
29.FoxP,YamaguchiC.Bodyimagechangeinpregnancy:acomparisonofnormal weightandoverweightprimigravidas.Birth.1997;24:35–40.
30.JenkinW,TiggemannM.Psychologicaleffectsofweightretainedafter preg-nancy.WomenHealth.1997;25:89–98.
31.OgleJP,TynerKE,Schofield-TomschinS.Jointlynavigatingthereclamationof the“womanIusedtoBe”:negotiatingconcernsaboutthepostpartumbody withinthemaritaldyad.ClothTextResJ.2011;29:35–51.
32.UptonRL,HanSS.Maternityanditsdiscontents–“Gettingthebodyback”after pregnancy.JContempEthnogr.2003;32:670–92.
33.TiggemannM.Bodyimageacrosstheadultlifespan:stabilityandchange.Body Image.2004;1:29–41.
34.SmithDM,CookeA,LavenderT.Maternalobesityisthenewchallenge;a qual-itativestudyofhealthprofessionals’viewstowardssuitablecareforpregnant womenwithaBodyMassIndex(BMI)≥30kg/m2.BMCPregnancyChildbirth.
2012;12:157.
35.CopenCE,DanielsK,MosherWD.FirstpremaritalcohabitationintheUnited States:2006–2010NationalSurveyofFamilyGrowth.NatlHealthStatReport. 2013:1–15.
36.CopenCE,DanielsK,VespaJ,MosherWD.FirstmarriagesintheUnitedStates: datafromthe2006–2010NationalSurveyofFamilyGrowth.NatlHealthStat Report.2012:1–21.
37.TheEURO-PERISTATproject.Healthandcareofpregnantwomenandbabiesin Europein2010.Paris:EURO-PERISTAT;2012.
38.MorgenCS,BjorkC,AndersenPK,MortensenLH,NyboAndersenAM. Socioeco-nomicpositionandtheriskofpretermbirth–astudywithintheDanishNational BirthCohort.IntJEpidemiol.2008;37:1109–20.
39.MortensenLH,Helweg-LarsenK,AndersenAM.Socioeconomicdifferencesin perinatalhealthanddisease.ScandJPublicHealth.2011;39Suppl.:110–4.
40.Feijen-deJongEI,JansenDE,BaarveldF,vanderSchansCP,SchellevisFG, ReijneveldSA.Determinantsoflateand/orinadequateuseofprenatal health-care in high-income countries: a systematic review. EurJ Public Health. 2012;22:904–13.
41.DaoudN,O’CampoP,MinhA,UrquiaML,DzakpasuS,HeamanM,etal.Patterns ofsocialinequalitiesacrossmultiplepregnancyandbirthoutcomes:a compar-isonofindividualandneighborhoodsocioeconomicmeasures.BMCPregnancy Childbirth.2014;14:393.
42.SobalJ,StunkardAJ.Socioeconomicstatusandobesity:areviewoftheliterature. PsycholBull.1989;105:260–75.
43.WardleJ,WallerJ,JarvisMJ.Sexdifferencesintheassociationofsocioeconomic statuswithobesity.AmJPublicHealth.2002;92:1299–304.
44.HardyR,WadsworthM,KuhD.Theinfluenceofchildhoodweightand socioe-conomicstatusonchangeinadultbodymassindexinaBritishnationalbirth cohort.IntJObesRelatMetabDisord.2000;24:725–34.
45.Graham H, Power C. Childhood disadvantage and health inequalities: a frameworkforpolicybasedonlifecourseresearch.ChildCareHealthDev. 2004;30:671–8.
46.BourdieuP.Distinction:asocialcritiqueofthejudgmentoftaste.Cambridge, MA:HarvardUniversityPress;1984.
47.LangenbergC,HardyR,KuhD,BrunnerE,WadsworthM.Centralandtotal obesityinmiddleagedmenandwomeninrelationtolifetimesocioeconomic status:evidencefromanationalbirthcohort.JEpidemiolCommunityHealth. 2003;57:816–22.
48.McLarenL,KuhD.Women’sbodydissatisfaction,socialclass,andsocialmobility. SocSciMed.2004;58:1575–84.
49.HadarE,AshwalE,HodM.Thepreconceptionalperiodasanopportunityfor pre-dictionandpreventionofnoncommunicabledisease.BestPractResClinObstet Gynaecol.2015;29:54–62.
50.Schummers L, HutcheonJA, Bodnar LM,LiebermanE, Himes KP. Risk of adversepregnancyoutcomesbyprepregnancybodymassindex:a population-basedstudytoinformprepregnancyweightlosscounseling.ObstetGynecol. 2015;125:133–43.
51.BentesM,DiasC,SakellaridesC,BankauskaiteV.Healthcaresystemsin tran-sition:Portugal.Copenhagen:WHORegionalOfficeforEuropeonBehalfofthe EuropeanObservatoryonHealthSystemsandPolicies;2004.
52.LunetN,RodriguesT,CorreiaS,BarrosH.Adequacyofprenatalcareasamajor determinantoffolicacid,iron,andvitaminintakeduringpregnancy.CadSaude Publica.2008;24:1151–7.
53.PinheiroL,SilvaN,PereiraA.PreconceptionandprenatalcareinSãoMarcos Hospital,athirdlevelPortugueseHospital.SaúdeInfantil.2009;31:59–62.
54.AlvesE,CorreiaS,BarrosH,AzevedoA.Prevalenceofself-reported cardiovascu-larriskfactorsinPortuguesewomen:asurveyafterdelivery.IntJPublicHealth. 2012;57:837–47.
55.McBrideCM,EmmonsKM,LipkusIM.Understandingthepotentialof teach-ablemoments:the caseofsmokingcessation. HealthEduc Res.2003;18: 156–70.
56.PhelanS.Pregnancy:a“teachablemoment”forweightcontrolandobesity pre-vention.AmJObstetGynecol.2010;202:e1–8.
57.StanevaA,Wittkowski A.Exploringbeliefs andexpectations about moth-erhood in Bulgarian mothers: a qualitative study. Midwifery. 2013;29: 260–7.
58.CrozierSR, RobinsonSM,Borland SE, GodfreyKM, CooperC, InskipHM. Dowomenchangetheirhealthbehavioursinpregnancy?Findingsfromthe SouthamptonWomen’sSurvey.PaediatrPerinatEpidemiol.2009;23:446–53.
59.AlvesE,AzevedoA,CorreiaS,BarrosH.Long-termmaintenanceofsmoking cessationinpregnancy:ananalysisofthebirthcohortgenerationXXI.Nicotine TobRes.2013;15:1598–607.
60.BombardJM,RobbinsCL,DietzPM,ValderramaAL.Preconceptioncare:the perfectopportunityforhealthcareproviderstoadviselifestylechangesfor hypertensivewomen.AmJHealthPromot.2013;27Suppl.:S43–9.
61.TeixeiraPJ, SilvaMN, Mata J, Palmeira AL,Markland D. Motivation, self-determination, and long-term weightcontrol. Int JBehav Nutr PhysAct. 2012;9:22.
62.Karelis AD. Metabolically healthy but obese individuals. Lancet. 2008;372:1281–3.
63.WildmanRP.Healthyobesity.CurrOpinClinNutrMetabCare.2009;12:438–43.
64.Aguilar-SalinasCA,GarciaEG,RoblesL,Ria ˜noD,Ruiz-GomezDG,García-Ulloa AC,etal.Highadiponectinconcentrationsareassociatedwiththemetabolically healthyobesephenotype.JClinEndocrinolMetab.2008;93:4075–9.
65.BluherM.Thedistinctionofmetabolically‘healthy’from‘unhealthy’obese indi-viduals.CurrOpinLipidol.2010;21:38–43.
66.StefanN,KantartzisK,MachannJ,SchickF,ThamerC,RittigK,etal.Identification andcharacterizationofmetabolicallybenignobesityinhumans.ArchIntern Med.2008;168:1609–16.
67.Karelis AD, MessierV, Brochu M,Rabasa-LhoretR. Metabolically healthy but obese women: effect of an energy-restricted diet. Diabetologia. 2008;51:1752–4.
68.BrochuM,TchernofA,DionneIJ,SitesCK,EltabbakhGH,SimsEA,etal.Whatare thephysicalcharacteristicsassociatedwithanormalmetabolicprofiledespite ahighlevelofobesityinpostmenopausalwomen?JClinEndocrinolMetab. 2001;86:1020–5.
69.KukJL,ArdernCI.Aremetabolicallynormalbutobeseindividualsatlowerrisk forall-causemortality?DiabetesCare.2009;32:2297–9.
70.PhillipsCM,PerryIJ.Doesinflammationdeterminemetabolichealthstatusin obeseandnonobeseadults?JClinEndocrinolMetab.2013;98:E1610–9.
71.vanVliet-OstaptchoukJV,NuotioML,SlagterSN,DoironD,FischerK,FocoL, etal.Theprevalenceofmetabolicsyndromeandmetabolicallyhealthyobesityin Europe:acollaborativeanalysisoftenlargecohortstudies.BMCEndocrDisord. 2014;14:9.
72.Sims EA. Are there persons who are obese, but metabolically healthy? Metabolism.2001;50:1499–504.
73.KramerCK,ZinmanB,RetnakaranR.Aremetabolicallyhealthyoverweightand obesitybenignconditions?Asystematicreviewandmeta-analysis.AnnIntern Med.2013;159:758–69.
74.Bobbioni-HarschE,PatakyZ,MakoundouV,LavilleM,DisseE,AnderwaldC, etal.Frommetabolicnormalitytocardiometabolicriskfactorsinsubjectswith obesity.Obesity(SilverSpring).2012;20:2063–9.
75.PhillipsCM,DillonC,HarringtonJM,McCarthyVJ,KearneyPM,FitzgeraldAP, etal.Definingmetabolicallyhealthyobesity:roleofdietaryandlifestylefactors. PLOSONE.2013;8:e76188.
76.VelhoS,PaccaudF,WaeberG,VollenweiderP,Marques-VidalP.Metabolically healthyobesity:differentprevalencesusingdifferentcriteria.EurJClinNutr. 2010;64:1043–51.
77.DespresJP,LemieuxI.Abdominalobesityandmetabolicsyndrome.Nature. 2006;444:881–7.