Validity and internal consistency of the American Orthopedic Foot and Ankle Society Midfoot Scale in patients with Lisfranc injury. The results of the randomized controlled trial will be finalized after the publication of this thesis.
Anatomy and biomechanics of the midfoot
Lisfranc joint
The medial column is formed by the first metatarsal bone and the medial cuneiform. The central column is formed by the second and third metatarsals and the intermediate and lateral cuneiform bones.
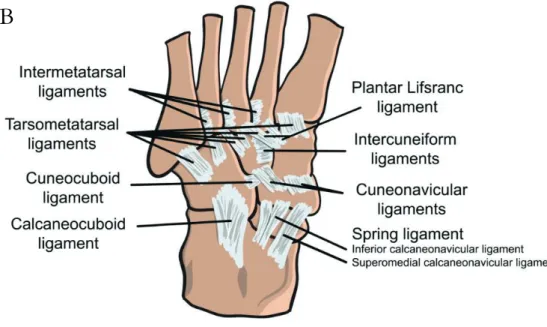
Chopart joint
The plantar and interosseous ligaments are stronger and stiffer than the dorsal ligaments and therefore play an important role in providing stability over the joint (Kaar, Femino, & Morag, 2007; Solan et al., 2001). The dorsolateral calcaneocuboid ligament extends from the anterior process of the calcaneus and inserts into the dorsal aspect of the cuboid, forming part of the joint capsule.
Biomechanics
Epidemiology of midfoot injuries
Lisfranc injuries
The two most cited studies investigating the epidemiology of Lisfranc injuries were published in the 1960s (Aitken & Poulson, 1963; English, 1964). As the Lisfranc injury was previously defined as a complete dislocation of the TMT joints, all less severe injuries were neglected.
Chopart injuries
English (1964) reported that 24 Lisfranc injuries were treated in their hospital among 11,000 fractures, giving a rate of 0.2% of all fractures. In total, 66 Lisfranc injuries were detected over ten years, resulting in an incidence rate of person-years.
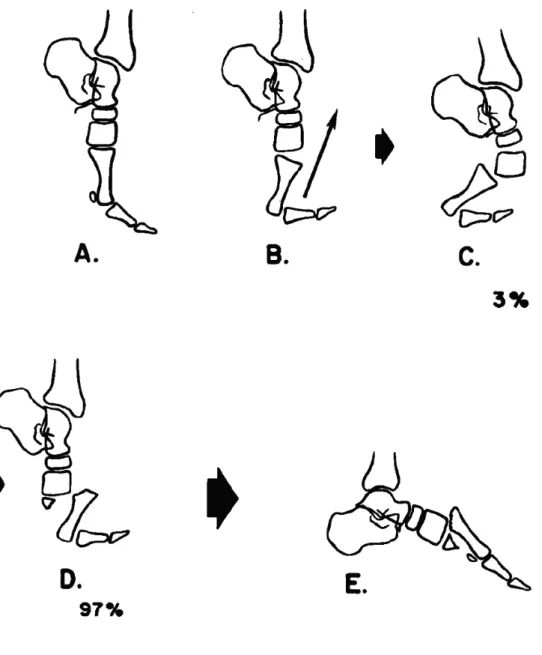
Injury mechanisms
Lisfranc injuries
They presented that the subtle type of injury is most common in athletes, such as football players or soccer players. 2017) studied the features of Lisfranc injuries detected by CT. They found that the majority (60%) of Lisfranc injuries were caused by low-energy trauma mechanisms, such as playing sports, turning at ground level, and falling from a height of less than 1.2 m.
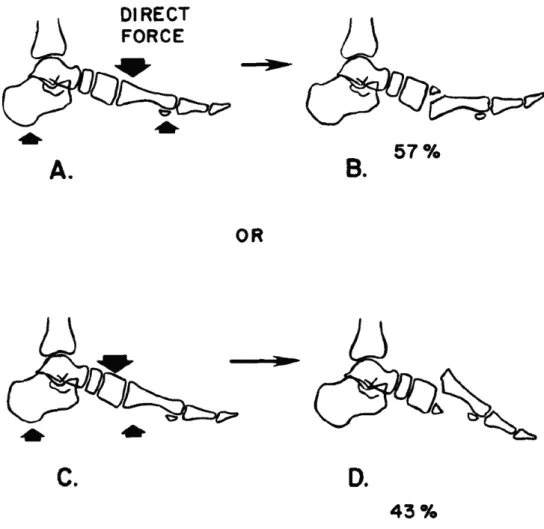
Chopart injuries
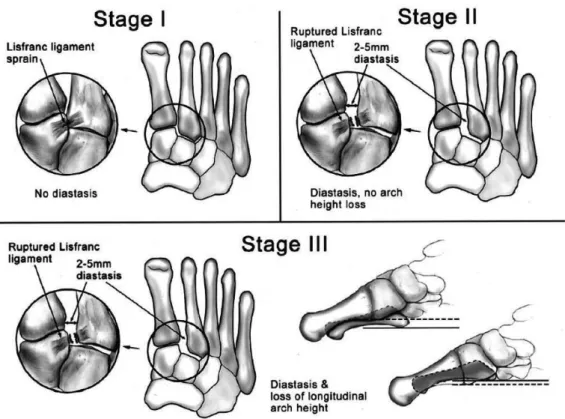
Since the publication of Nunley and Vertull's (2002) classification, the subtle Lisfranc type of injury has been widely recognized. However, the use of CT might allow detection of injuries missed in previous studies using conventional radiographs.
Classifications
Lisfranc injuries
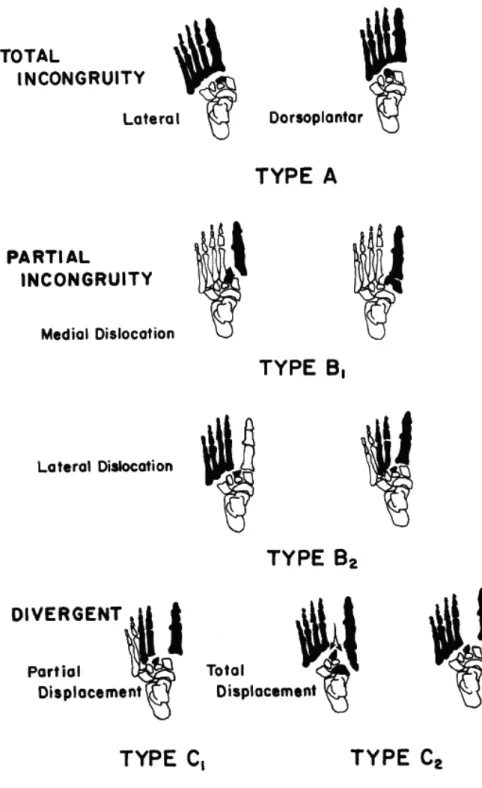
In C1 type (partial dislocation) injuries, one or more of the four lateral metatarsals are displaced laterally and the first metatarsal is displaced medially. 2006 (Talarico, Hamilton, Ford, & Rush, 2006) and the inter- and intra-observer reliability of the Myerson version of the classification by Mahmoud et al.
Chopart injuries
Fracture-dislocations are caused by high-force subtalar dislocation of the foot and a tear of the interosseous talocalcaneal ligament. Although the classification by Main and Jowett is the only classification for Chopart lesions, it was developed based on a study sample of only 31 patients, and therefore the study results should be interpreted with caution.
Diagnostics of Lisfranc injury
- Clinical signs
- Conventional radiographs
- Weightbearing radiographs
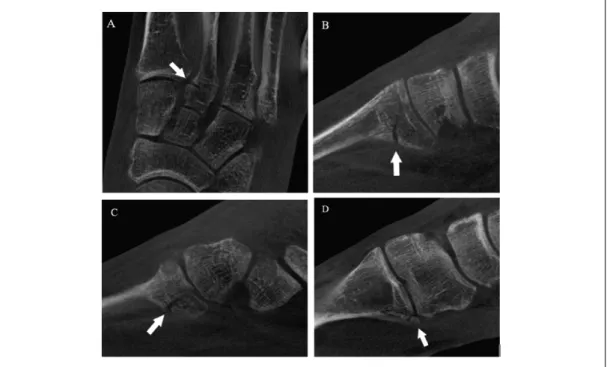
- Computed tomography (CT)
- Magnetic resonance imaging (MRI)
- Weightbearing cone beam computed tomography
- Instability
The study by Goiney et al. 1985) was the first to propose CT as an imaging modality for the detection of Lisfranc lesions. Furthermore, MRI is suggested to be the best imaging modality for detecting a rupture of the Lisfranc ligament (Potter et al., 1998; Preidler et al., 1996a; Preidler et al., 1996b).

Outcome measures
Of these, the American Orthopedic Foot and Ankle Society (AOFAS) clinical scoring systems are by far the most widely used PROMs for the foot and ankle (Hunt & Hurwit, 2013; Kitaoka et al., 1994). However, there are numerous valid and reliable instruments that can be used to assess outcomes after foot and ankle surgery.
Treatment of Lisfranc injuries
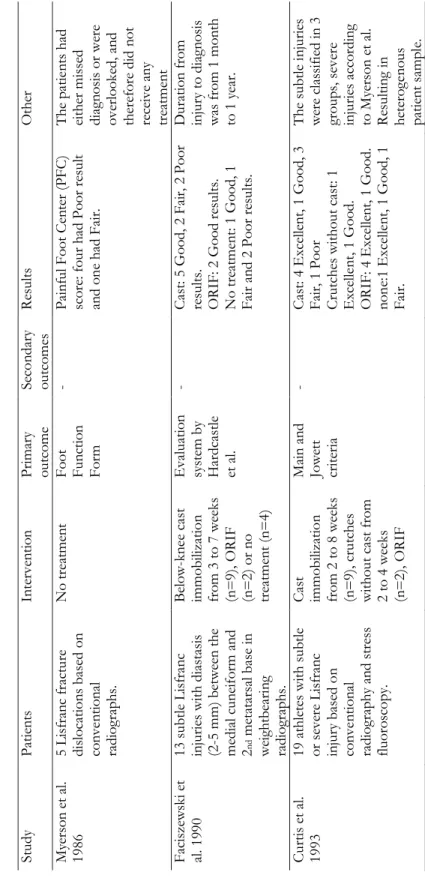
Non-operative treatment
For example, the study by Myerson et al. 1986) presented results following the nonoperative treatment of dislocated Lisfranc injury. Four of the patients resulted in a poor outcome and one resulted in a fair outcome according to the Painful Foot Center scoring systems (Myerson et al., 1986).
Operative treatment
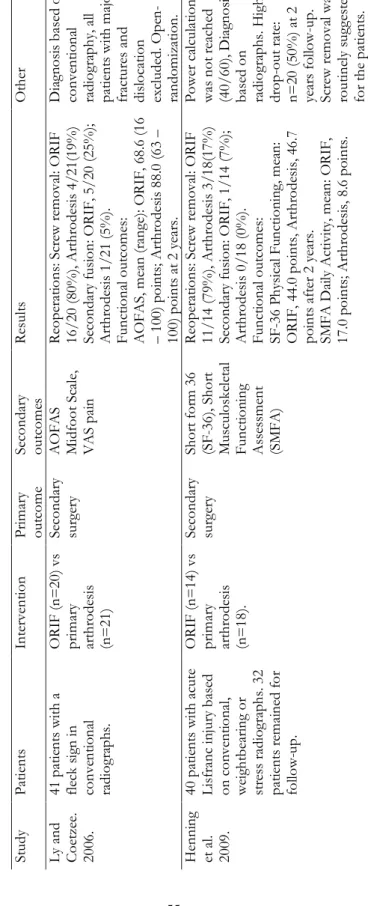
This finding was also common in more recent studies, where patients with non-anatomic reduction more often developed post-operative osteoarthritis and resulted in lower clinical scores (Arntz et al., 1988; Buzzard & Briggs, 1998; Kuo et al. , 2000; Myerson et al., 1986). However, it has been found that mild radiographic findings of osteoarthritis are present in almost every patient treated with ORIF, but the functional results do not correlate with the radiological findings (Mulier et al., 2002; Myerson et al., 1986). Primary arthrodesis has been proposed as an option for ORIF to prevent reoperations and the development of painful posttraumatic osteoarthritis (Cochran et al., 2017; Henning et al., 2009; Ly & Coetzee, 2006; Smith et al., 2015).
Retrospective data (I, II, III, IV)
- CT and CBCT settings (I, II, IV, V)
- Definition of Lisfranc injury (I, II, III, IV)
- Radiograph data (II)
- Validation data (III)
- Retrospective case-series (IV)
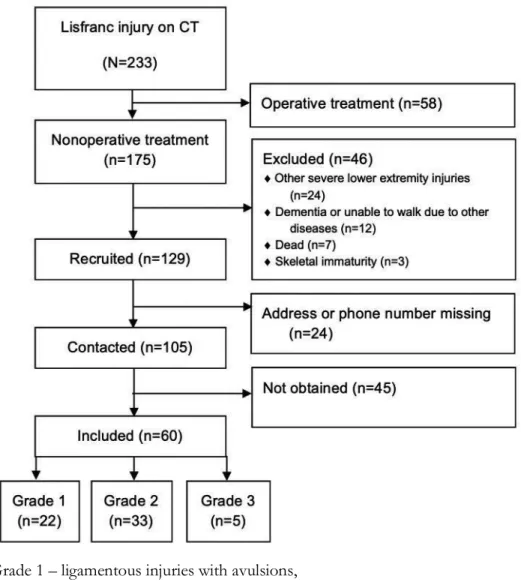
High-energy mechanisms accounted for 37% (n=85) and low-energy mechanisms for 55% (n=128) of Lisfranc injuries.
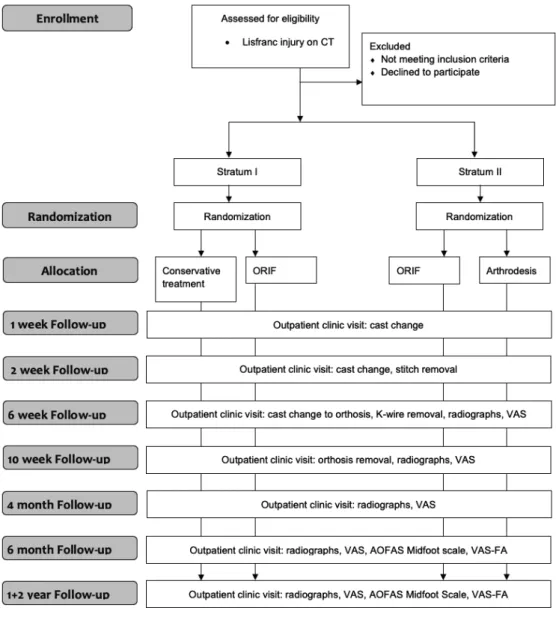
Prospective data (IV, V)
Patient selection and methods
The final decision on inclusion will be made after a discussion between the patient and one of the foot surgeons in the study group. Randomization will be performed by the research coordinator at Tampere University Hospital, who will not otherwise participate in the study. Eligible patients for stratum II will be randomized to the ORIF or primary arthrodesis groups.
Treatment protocols
The result of the randomisation will be kept in sealed envelopes and opened in numerical order after the recruitment has been confirmed.
Treatment techniques (IV, V)
Surgical operations will be performed with one or two incisions, depending on the location of the injury. If displaced injuries occur in TMT IV or V joints, open reduction and temporary K-wire fixation is performed for these injured joints. Despite the removal of the articular surfaces, both operations will be performed in a similar manner in terms of incisions, fixation, and temporary fixation of the lateral TMT joints.
Outcome measures (III, IV, V)
Visual Analogue Scale Foot and Ankle
The VAS-FA has been shown to have acceptable validity in the evaluation of outcomes after foot or ankle surgery (Angthong, Chernchujit, Suntharapa, & Harnroongroj, 2011; Gur et al., 2017; Repo et al., 2018). Intra-class correlation coefficient (ICC) for the total score has been 0.97 and its different subscales from 0.95 to 0.97, indicating high reliability (Repo et al., 2018). The Finnish version of the VAS-FA has also been shown to have high validity and reliability (Repo et al., 2018).
American Orthopaedic Foot and Ankle Society
The topics are divided into three submodules: Pain, which contains four topics; Functioning, containing 11 items, and Other complaints, containing five items (Richter et al., 2006). Internal consistency has been shown to be high, as Cronbach's alphas for the instrument's subscales have been 0.91 for Pain, 0.94 for Function and 0.81 for Other complaints (Repo et al., 2018).
Statistical analysis
For the validation of the AOFAS Midfoot Scale, hypotheses were defined in advance and the results were interpreted according to the Consensus-based Standards for the selection of health status Measuring Instruments (COSMIN) checklist (Mokkink et al., 2010b). Linear regression analyzes were used to determine the strength of the relationship between the AOFAS Midfoot Scale and the VAS-FA. Age- and sex-standardized regression coefficient β indicates how strongly the score of the AOFAS Midfoot scale is related to the total and the sub-scores of the VAS-FA.
Ethical considerations
Instruments (COSMIN) (Mokkink et al., 2010b) and the Strengthening Reporting of Observational Studies in Epidemiology (STROBE) statement (Von Elm et al., 2007).
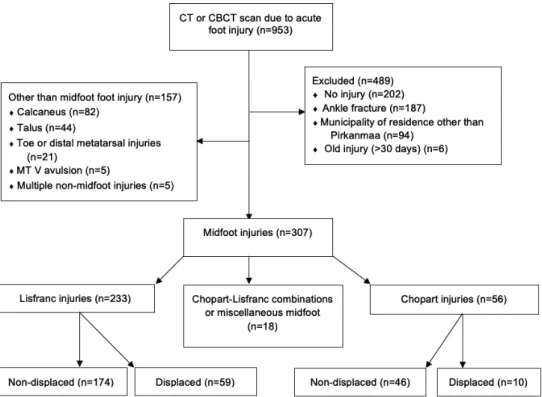
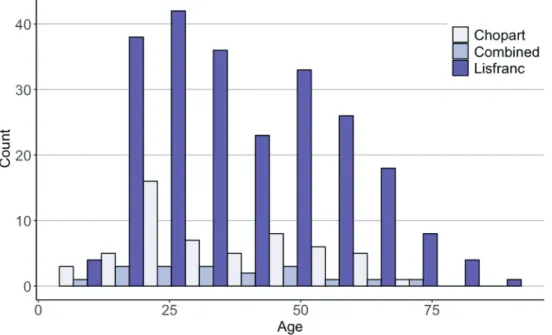
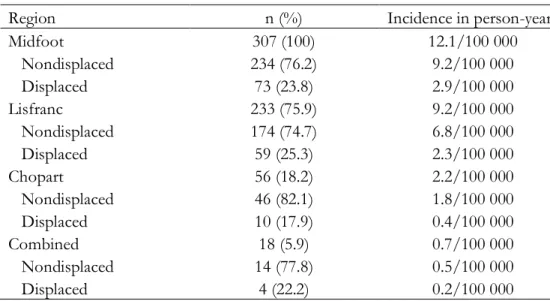
Incidence and characteristics of midfoot injuries (I)
No association was found between trauma energy and injury severity in Lisfranc injuries (p=0.069). High-energy mechanisms accounted for 14% (n=8), and low-energy mechanisms accounted for 86% (n=48) of Chopart injuries. In Chopart-Lisfranc combinations or various injuries, the majority of injuries were caused by high-energy trauma mechanisms (56%), such as traffic accidents 28% (n=5) and direct injury 22% (n=4) (Figure 14).
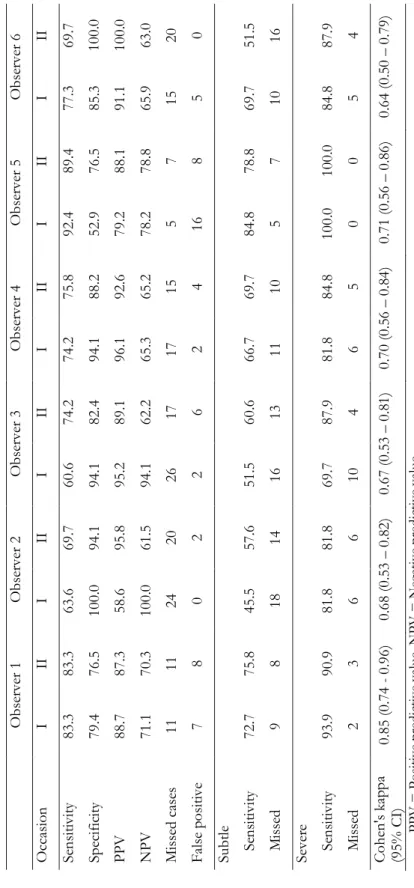
Inter and intraobserver reliability of radiographs (II)
In our study, only 6% (n=13) of Lisfranc injuries had such a morphology that they could be classified using the Myerson classification.
Validation of the AOFAS Midfoot Scale (III)
Default hypotheses for validation of the American Orthopedic Society Foot and Leg Midfoot Scale. All AOFAS midfoot scale items had correctly ranked thresholds between response categories (Figure 20). A person-item distribution map shows that item difficulty matched the study sample coverage of the AOFAS Midfoot Scale relatively well (Figure 21).
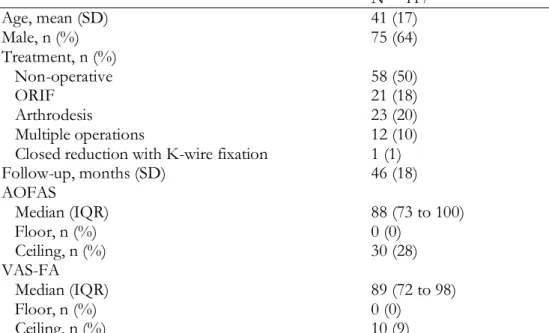
Retrospective case-series (IV)
One of the Grade 1 patients underwent secondary surgery (arthrodesis of the second TMT joint) ten months after the primary injury. Characteristics of the Non-Surgically Treated Lisfranc Injuries Classified by the Modified Schepers and Rammelt Classification. The injuries of the patients in this grade involved one to five TMT joints (Table 9).
Randomized controlled study (V)
Of the grade 3 patients, 60% (n=3) scored above 90 points on both the pain and function subscales of the VAS-FA. One patient with TMT I-III fractures with comminuted MT I scored below 60 points on the VAS-FA.
Incidence (I)
A study by Renninger et al. 2017) examined the differences between low- and high-energy Lisfranc injuries. They classified sports activities and twists and falls of less than 4 feet (1.2 m) as low-energy injuries. Automobile and motorcycle vehicle collisions, crush injuries, and falls of more than 4 feet (1.2 m) were classified as high-energy injuries.
Diagnostics (II)
Recently, weight-bearing CBCT imaging has been introduced as an alternative modality for radiological imaging of metatarsal injuries (Tuominen et al., 2013). Theoretically, the precision of standard CT and the stress aspect of weight-bearing radiographs could be combined in weight-bearing CBCT. However, the use of weight-bearing CBCT in primary diagnostics can be a notable problem due to pain and difficulty in bearing weight immediately after the injury.
Outcome measures (III)
Therefore, current methods to detect and evaluate Lisfranc joint instability seem unreliable. In addition, there is still no consensus on how to assess the instability of the Lisfranc injury. Our primary interest was to evaluate the validity of the instrument as it was the only widely used foot score with previously published MCID values (Dawson et al., 2007).
Outcomes after non-operatively treated Lisfranc injury (IV)
Accurate job classification should also provide estimates of outcomes after the chosen treatment (Burstein, 1993). Although the results of surgery may not depend on the primary dislocation, it is an important factor when considering nonoperative treatment. The main finding of the retrospective case series was that nondisplaced Lisfranc injuries involving up to three TMT joints can be treated nonoperatively with good functional outcomes.
Randomized controlled study (V)
An obvious limitation of the study of outcomes after non-surgically treated Lisfranc injuries was not using a clinical examination or imaging of the patients. The limitation of the prospective study is that the power calculations are based on the AOFAS Midfoot Scale, which is why it is currently reported as the primary outcome measure. A second limitation of the study is that the inclusion criteria for subtle and severe injuries were based on our study group.
Challenges for future studies
The role of reduction and internal fixation of Lisfranc fracture dislocations: a systematic review of the literature. No association was found between trauma energy and injury severity (non-displaced/displaced) in Lisfranc injuries (p = 0.069). The role of reduction and internal fixation of Lisfranc fracture dislocations: a systematic review of the literature.
Lisfranc injury was originally described as a partial or complete dislocation of the tarsometatarsal (TMT) joints, although the definition and classifications of the injury have changed over the years [39, 45]. There have been no previous randomized studies of the nonoperative versus operative treatment of Lisfranc injuries.