In the early treatment of axSpA, the proportion of users of self-injected bDMARDs was quite low, but initiation of a bDMARD appeared to reduce these patients' opioid consumption. Overall, the increasing life expectancy of the population and the fact that the treatment of IA patients often requires long-term monitoring in rheumatology clinics, the burden of IA on the health care system and especially on the specialist will probably increase in the future.
Definition of inflammatory arthritis (IA)
- Rheumatoid arthritis (RA)
- Undifferentiated arthritis (UA)
- Axial spondyloarthritis (axSpA)
- Other IAs
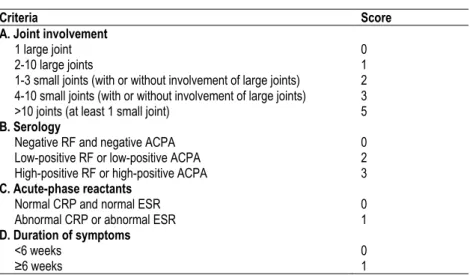
Modified New York criteria for the classification of ankylosing spondylitis (AS) (modified from Linden et al. 1984) Clinical criteria. 2009 classification criteria for axial spondyloarthritis by the Assessment of Spondyloarthritis International Society (ASAS) (Rudwaleit et al. 2009a).
Epidemiology of IA
- RA
- UA
- AxSpA
- Other IAs
In this study, the case definition was based on a rheumatologist's clinical diagnosis of RA and the need to start anti-arthritic medication rather than on the fulfillment of the ACR criteria (Puolakka et al. 2010). The estimates of AS prevalence (from 36 eligible studies) for each of the major global continents were reported by Dean et al.
Aetiopathogenesis of IA
RA
Obesity has also been recognized as a risk factor for RA in association with smoking status (Crowson et al. 2013). A positive correlation between obesity and ACPA-negativity has been shown, especially in women (Wesley et al. 2013).
AxSpA
They maintain chronic inflammation and lead to tissue destruction, and they are the target of rheumatic therapies (Lin et al. 2020). The association between smoking and ACPA appears most clearly in RA patients with SE (Hedström et al. 2019).
Assessment of IA
RA
The most recent ACR/EULAR remission criteria for clinical trials were established in 2011 (Felson et al. 2011). Plain radiographs show the radiological progression of RA, and various scoring methods have been developed to quantify the damage (irreversible erosions typically in the small joints of the hands and feet) (Larsen et al. 1977, van der Heijde 2000).
AxSpA
Two or more of these lesions on the same image or one lesion on two consecutive images is considered a positive MRI finding (Rudwaleit et al. 2009b). Chronic inflammatory lesions in axSpA include fat deposits, subchondral sclerosis, erosions and ankylosis of the sacroiliac joints or spine, and the formation of syndesmophytes in the spine (Canella et al. 2013).
Drug treatment of early IA
- Conventional synthetic disease modifying anti-rheumatic
- Biological DMARDs
- Targeted synthetic DMARDs
- Glucocorticoids
- Drug treatment recommendations of early IA
- RA
- UA
- AxSpA
- Implementation of drug treatment in early IA
- RA
- AxSpA
Its effectiveness in the treatment of axSpA is low and limited to peripheral arthritis (Haibel et al. 2005a). The risk of tuberculosis appears to be increased with the use of TNFs (Sepriano et al. 2020).
Pain in IA
Mechanisms of pain
In one study, 40% of axSpA patients still experienced persistent pain after seven years of TNFi treatment (Arends et al. 2017). Neuropathic pain is caused by a lesion or disease of the somatosensory system (Colloca et al. 2017) and may also be present in IA patients.
Measurements of pain
Pain medication
- Non-steroidal anti-inflammatory drugs
- Paracetamol
- Opioids
- Neuropathic pain medication
- New drugs for IA pain
Among Australian RA patients (N=3225) who entered the ARAD registry (biological registry) between 2001 and 2015, the prevalence of baseline opioid use was 33%, comprising mainly (26%) low-potency opioids such as code combinations and tramadol (Black et al. 2019). Opioid use among AS patients has been associated with subjective measures (depression, BASDAI, BASFI) rather than objective measures of disease activity (Dau et al. 2018). In the general population, lower socioeconomic status has been associated with greater opioid use (Hooten et al.
First-line drugs for the treatment of neuropathic pain include gabapentinoids (gabapentin and pregabalin), serotonin and norepinephrine reuptake inhibitors (duloxetine and venlafaxine), and tricyclic antidepressants (amitriptyline, nortriptyline) (Attal et al. 2010).
Background
Drug Purchase Register
Reimbursement Register
Patient cohort
IBD-associated arthritis could not be analyzed from the registry as the majority of incident patients already had SR for DMARDs due to their colitis. The day of the first reimbursement decision was defined as the index date in this study.
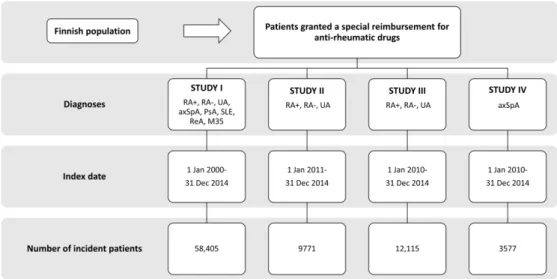
Controls
Drug purchases
Among the pain medications, the main interest was in opioids [mild opioids (codeine combination products and tramadol), moderate opioids (buprenorphine) and strong opioids (morphine, hydromorphine, oxycodone and fentanyl)], but also the purchases of NSAIDs and paracetamol were analysed. Opioid, NSAID and paracetamol purchases were evaluated one year before and after the index date, further dividing the observation time into 3-month periods (study III and IV). In study IV, the opioid purchase frequencies of group B patients were examined one year before and one year after starting self-injection bDMARD therapy to study whether starting a bDMARD had an impact on the amount of opioid use.
To this end, the Defined Daily Doses (DDDs) described by the World Health Organization (WHO) were used as a tool to assess opioid use one year before and one year after starting a bDMARD.
Statistical analysis
In study IV, generalized linear models were applied to estimate odds ratios (ORs) and risk ratios (RRs). In study IV, the Kaplan-Meier estimate served to illustrate data on the cumulative use of bDMARDs. Cox proportional hazard models were used to estimate the hazard ratios (HR) adjusted for age, gender and education level (basic, middle level, lower high level and upper high level).
Data on education levels were obtained from the Population Census Center (Statistics Finland) (studies III and IV).
Ethical considerations
Demographic data of IA cohorts
Trends in the incidences of IAs
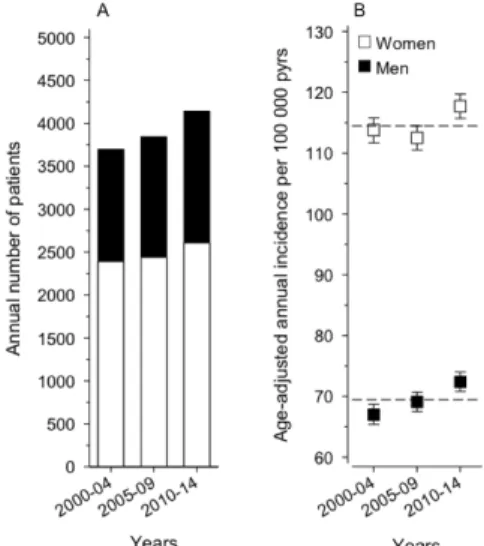
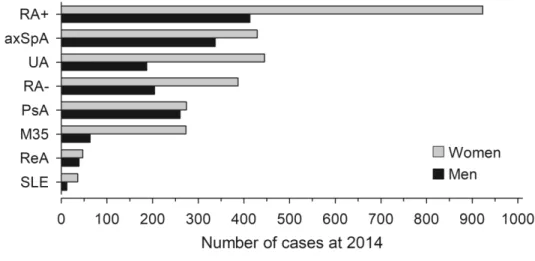
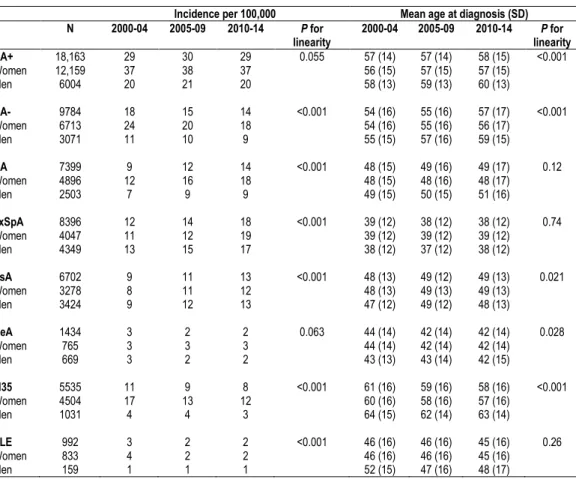
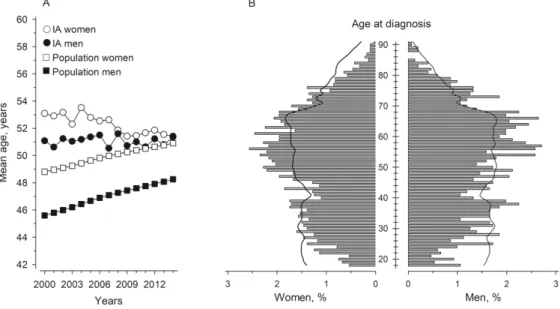
The mean age at diagnosis increased statistically significantly in seropositive and seronegative RA and PsA, and decreased in ReA and M35. The age distribution of all patients eligible for SR for antirheumatic drugs as well as the age structure of the general population (according to Statistics Finland) in 2014 are shown in Figure 8B. Figure 8. a) Average age at diagnosis of IA and average age of the adult population in the period 2000–2014 in Finland. White dots refer to the average age of women and black dots to the average age of men at the time of IA diagnosis.
The white squares refer to the mean age of the total female adult population and the black squares to the mean age of the male adult population.

DMARD purchases
RA and UA patients
Baseline characteristics and the numbers and proportions (%) of DMARD and PRD buyers among patients with seropositive RA, seronegative RA and UA by the end of the first month post-ID. Baseline characteristics and the numbers and proportions (%) of DMARD and PRD buyers among patients with seropositive RA, seronegative RA and UA by the end of the first year after ID. The numbers of DMARD purchases by the patients during the first year after diagnosis are also shown.

AxSpA patients
Baseline characteristics and numbers and proportions of DMARD purchasers among group A and B axSpA patients throughout the first year after ID.
Opioid purchases
The proportion (%) of opioid, NSAID and paracetamol buyers among patients with axSpA and their controls one year before and after the ID. The risk ratios of opioid purchases among patients with seropositive RA, seronegative RA, UA and axSpA (group A and B axSpA patients separately) compared to their controls one year before and after the ID. Long-term opioid use was more common among IA patients both before and after the ID compared with their controls.
Proportion (%, with 95% CI) of individuals who purchased opioids at least once or were long-term opioid users among patients with seropositive RA, seronegative RA, UA, and axSpA and their controls one year before and after ID.

Temporal trends in the incidences of IAs
The possible other reasons for the observed growth in incidence rates can only be speculated. Also, the aging of the population, especially the baby boom generation (those born between 1946 and 1964), is likely to have caused an increase in the gross incidence of some IA groups. A decrease in the average age at diagnosis was found among women, mainly caused by the increasing number of patients in the diagnosis groups who had such a disease at a younger age.
However, in the absence of clinical and health behavior data, this study does not provide clear explanations for these points.
DMARD use in early IA
RA and UA patients
In real life, implementation of recommendations is often suboptimal, but over time they lead to improvement in DMARD use (Judge et al. 2015). In the treatment of early UA, EULAR recommendations favor MTX as the first-line agent (Combe et al. 2017). In rheumatoid arthritis, bDMARDS are used as second-line therapy after failure of csDMARDs, although a few meta-analyses have shown their short-term efficacy in csDMARD-naïve RA patients (Singh et al.
However, the long-term efficacy results of initial bDMARD (TNFi) treatment are not entirely clear (Gulácsi et al. 2019).
AxSpA patients
In addition, due to the latest classification criteria, the diagnosis of seronegative RA requires the involvement of at least 10 joints, which corresponds to highly active disease; thus, some patients in this group may not respond to traditional treatments. For example, peripheral spondyloarthritis, which does not fit any specific disease criterion, may have previously been recorded as the ICD-10 code M46, but today it is more commonly recorded as M13.9 (UA). This may explain some differences in the incidence and drug use of Finnish IA patients compared to those in other countries.
In the present study, women in group B appeared to be less responsive to bDMARDs than men, as their opioid use after initiation of bDMARDs was greater compared to men.
IA patients’ opioid use
Patients with seronegative RA have been shown to experience higher disease activity and delayed remission, partly due to changed diagnostics and demands for more joint involvement at diagnosis (Coffey et al. 2017), which may partly explain the differences in opioid use between the two RA serotypes . A similar finding was observed in a large US study, where long-term opioid use among patients with various inflammatory rheumatic diseases (RA, SLE, PsA and AS) was most common (RR 2.73) among AS patients compared to age and sex. matched patients with hypertension (Chen et al. 2019a). During the year after ID, long-term opioid use was seen in 3–6% of RA and UA patients, 11% of axSpA patients who initiated a bDMARD during follow-up (group B), and 5% of axSpA patients treated with csDMARDs only (group A).
A decrease in opioid use was found after ID, as the patients were presumably monitored by the rheumatologists, but the numbers did not reach population levels during follow-up.
Strengths and limitations
Changes in health care utilization after initiation of etanercept in patients with rheumatoid arthritis: a retrospective analysis of claims. Prevalence and risk of osteoporotic fractures in patients with rheumatoid arthritis: a multicenter comparative study of FRAX and WHO criteria. Changes in co-therapy after initiation of disease-modifying antirheumatic drug therapy in patients with rheumatoid arthritis.
Changes in opioid use after tumor necrosis factor inhibitor initiation in patients with rheumatoid arthritis. Metabolic and cardiovascular benefits of hydroxychloroquine in patients with rheumatoid arthritis: a systematic review and meta-analysis. Effect of methotrexate on cardiovascular disease in patients with rheumatoid arthritis: a systematic review of the literature.