Many of the consequences can only become apparent in the long term, during the child's later development (Bandstra et al. 2010, Conners et al. 2004). It has also been demonstrated that they hinder the progress of the child's development (Steinhausen et al. 2007) and interfere with mother-infant interaction (Salo et al. 2010).
Transition to motherhood
Psychoanalytic perspective
If the mother is preoccupied with her own emotional problems, she can easily transfer her negative states of mind to the interaction with the infant (Fraiberg et al. 1987, Stern and Bruschweiler-Stern 1998). This protects the child from the burdens of the mother and from repeating its own troubled past (Fraiberg et al. 1987).
Developmental psychoanalysis and neurobiology
On the other hand, the generalized model of an insensitive relationship may predict the infant's inadequate self-regulation (Fonagy et al. 2002). It can thus give him/her stress, which is detrimental to his/her ability to cope (Swanson et al. 2000).
Attachment perspective
Thus, in good parenting, the parent values the child's integrity, the adult's own emotions and thoughts, as well as the intentional nature of his/her child's behavior (Fonagy et al. 2002, Slade, 2002). For example, the mother's ability to mentalize about her own child has been shown to be weaker if the mother has been traumatized in her early attachment relationships (Fonagy et al. 2002).
Substance-dependence and early motherhood
Background characteristics and cumulative stressors
For example, in a Finnish study, 40% of pregnant women in residential care tested positive for depression (Pajulo et al. 2001). Personality disorders (Haller and Miles, 2004), anxiety (Haller et al. 1993) and bipolar affective disorders are also common among these women (Ashley et al. 2003).
Coping strategies among substance-abusing women
Maternal substance-abuse and early interaction…
Substance-abusing mothers usually have fragile and unreal, either negative or idealized experiences and expectations of motherhood (Flykt et al. 2012, Suchman et al. 2005). In addition, substance-abusing mothers have been shown to be lower in sensitivity and generally poorer in emotional availability (Fraser et al. 2010;.
Therapeutic interventions for pre- and postnatal substance-abusing
Comprehensive treatment programs
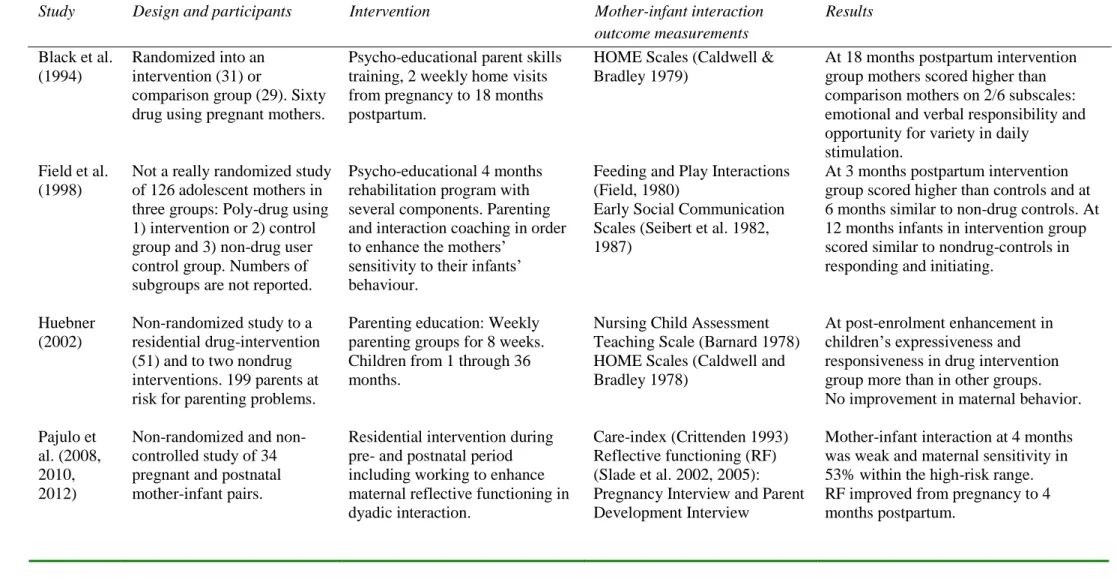
In addition, it is important to consider the mother's trauma perspective when planning treatment programs for substance-abusing mothers (Conners et al. 2006, Pajulo et al. 2012). Two main approaches to comprehensive treatment programs can be distinguished: one emphasizes practical and psychoeducational help and awareness of substance abuse and its causes and consequences (Black et al.
Psycho-educational interventions
Psychotherapeutic mother-infant interventions
Like the mother in the first months of the baby's life, therapists verbalize the group's desires, conflicts, and fears and look for and show ways to alleviate them. They emphasized that the therapist should help the mother to ensure that she can process those traumatic experiences later, after the group therapy, and the therapist should return and direct the focus of the group discussion to current parenting issues.
Outcome studies on mother-infant interventions
Treatment completion and reduction of substance abuse
Maternal mental health as a criterion of treatment
Quality of mother-infant interaction as a criterion of
Among high-risk mothers, which also included substance abusers and their children younger than 27 months, dyadic mother-child interaction improved response more in a group intervention based on short-term analytic attachment than in a control group receiving routine care (Smith et al. 2010). Mother-infant interaction at 4 months was poor and maternal sensitivity at 53% within the high-risk range.
Procedure
- Psychodynamic mother-infant group therapy intervention
- Psychosocial support (PSS)
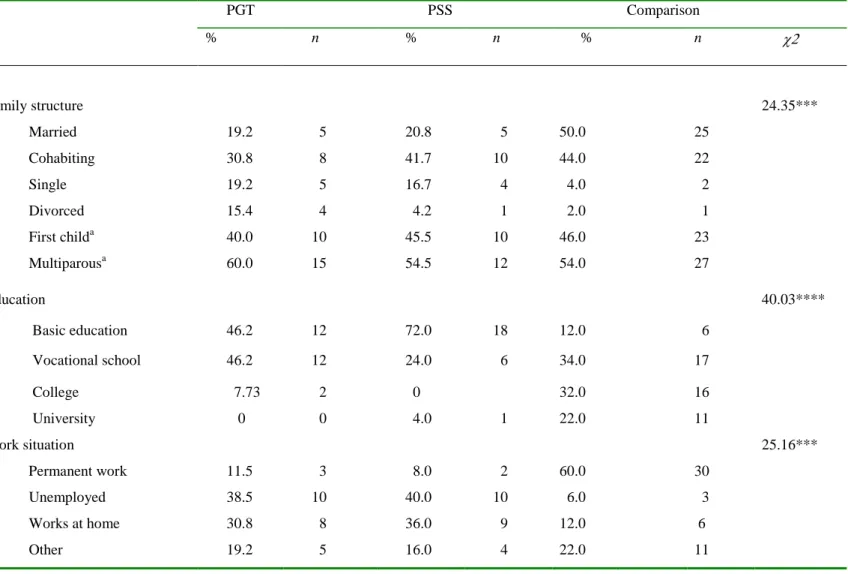
- Recruitment in Study I
- Recruitment in Studies II, III and IV
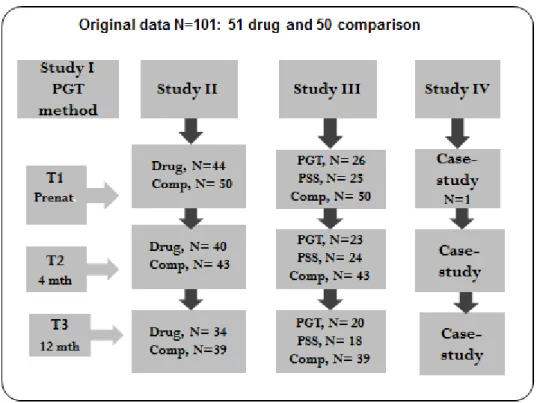
- Participants in Studies II and III
- The participants in Study IV
Comprehensive experiences of security and appreciation are considered the most important healing elements in the PGT intervention. Women in the comparison group were consecutively recruited from a maternity outpatient clinic in Lahti district.
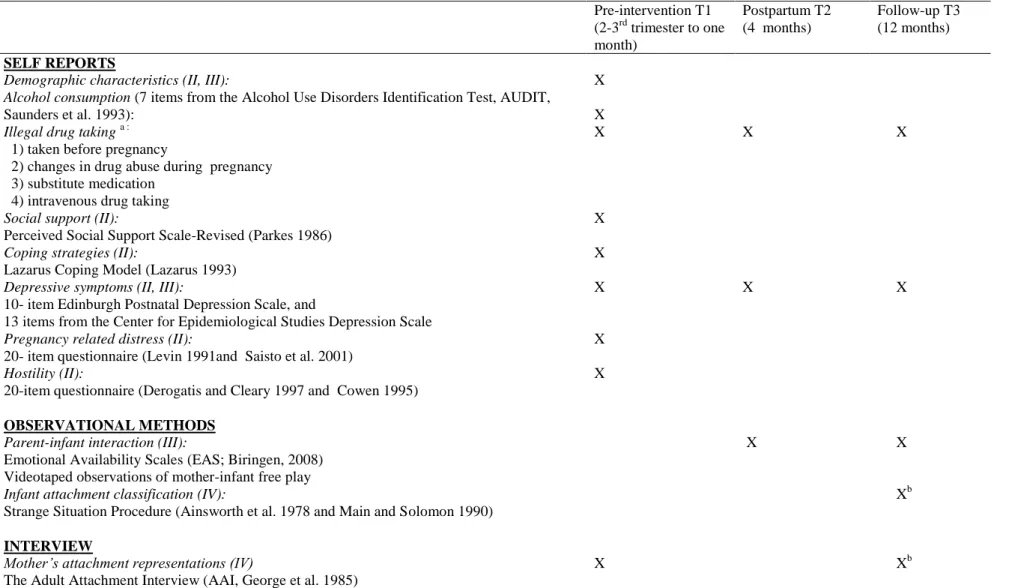
Measures in Studies II, III and IV
Self-reported measures
Finally and fourthly, seeking social support involves responses such as 'I like to share my bad experience with others' and 'I feel that I will recover when I get comfort and understanding from others'. I feel uncertain about parental responsibility' and 'I feel that I am not yet able to take care of my family'.
Observational methods in Studies III and IV
Disorganized infants display behavior characterized by caregiver anxiety or disorganization and disorientation to the strange situation environment. They exhibit contradictory, unpredictable, and inexplicable behavior patterns, and they lack a clear, organized behavioral strategy (i.e., safety, resistance, or avoidance) to meet the demands of the strange situation.
Interview
Infant scoring and classification in Study IV was completed by a reliable researcher trained in 2004 by Alain Sroufe and Elizabeth Carlson at the Institute of Child Development, University of Minnesota (USA). Scoring and classification of the AAI was completed by a reliable researcher trained in 2004 by Anders Broberg and Tord Ivarsson at the University of Gothenburg.
Statistical analyses in Studies II and III.…
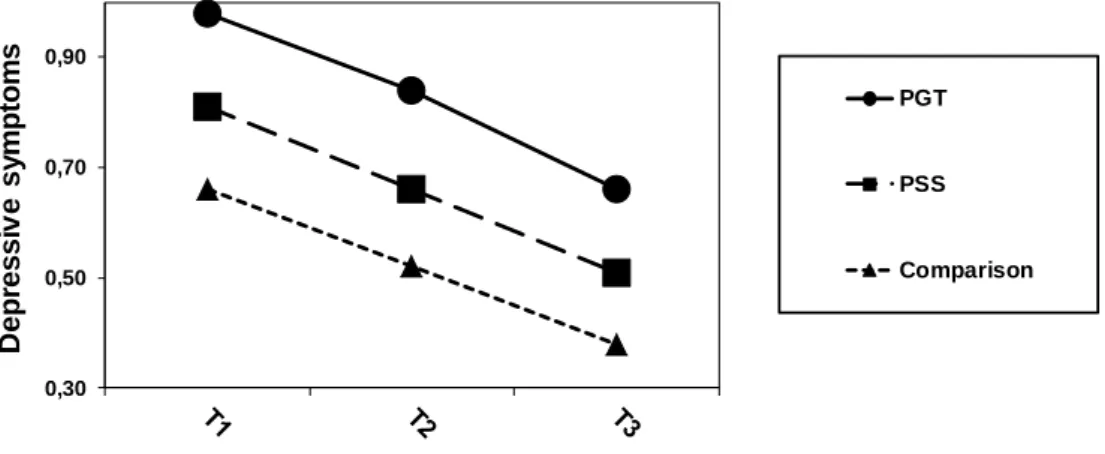
The impact of the PGT and PSS interventions on changes in maternal depressive symptoms from preintervention (T1) through 4 months postpartum (T2) to follow-up at 12 months (T3), and on the quality of the mother-infant interaction from T2 to T3 were measured. MANOVAS were applied to compare changes in substance abuse severity in the substance abuse intervention groups (PGT and PSS).
Ethics
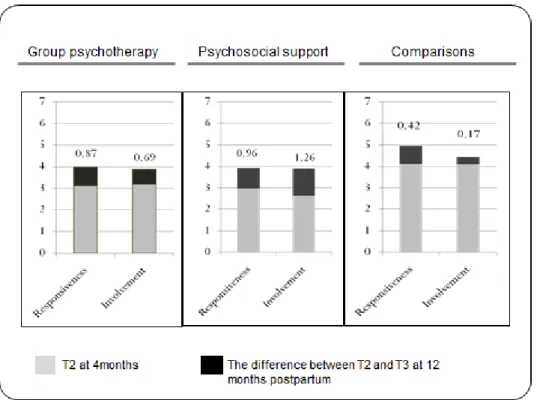
In the second step, the control variables of education, marital status, and economic hardship were entered in the third step, social support and coping strategies, and in the fourth, pregnancy-related distress and hostility. Further one-way MANCOVA with post-hoc Tukey-b analyzes were applied to compare EA scores between groups at T2 and T3.
Clinical findings with respect to the PGT method (Study I)
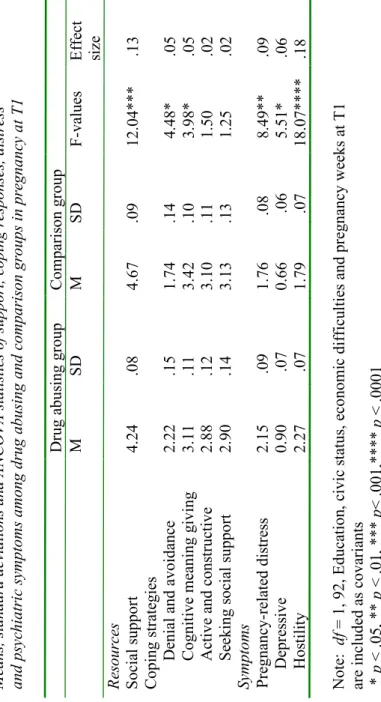
Resources and symptoms in pregnancy among drug-abusing and
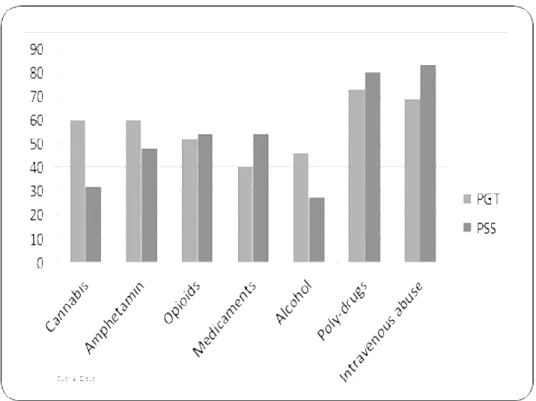
Substance abuse characteristics and treatment completion (Studies
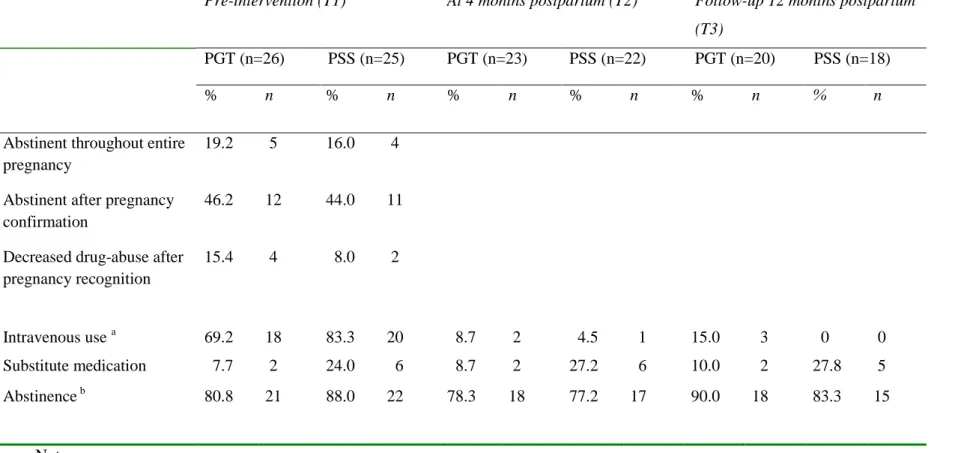
All women in both intervention groups reported stopping or significantly reducing their use of illicit drugs during pregnancy. Ten (40%) mothers in both intervention groups reported consuming small amounts of alcohol during the intervention.
Intervention effects on maternal depressive symptoms (Studies
Intervention effects on the quality of mother-child interaction
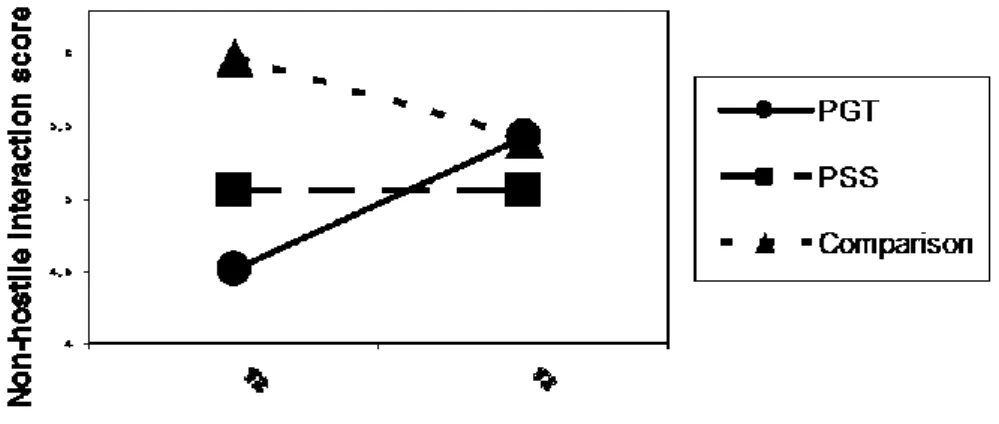
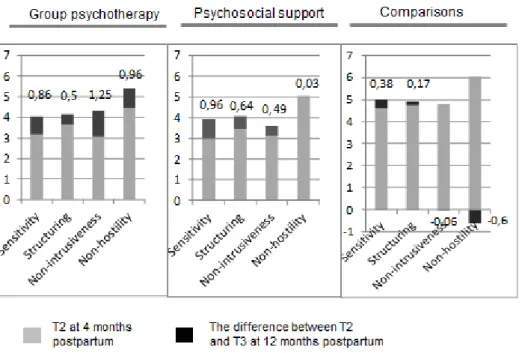
In addition, Figure 7 illustrates that non-intrusive maternal behavior approached that of the comparison group, and increased in both substance abuse intervention groups (FWilk's Lambda p < but more markedly in the PGT group. Changes in maternal non-hostility in Emotional Availability scales from 4 months postpartum (T2) to (T2) to the PGT month and the follow-up groups in the PGT and Changes in the PGT and the comparison groups. statistics es significant (p < .008) in the PGT intervention group (This figure is partially based on the figure published in Infant Mental Health Journal.
Factors that may mediate and prevent the intergenerational
In particular, the AAI was an important tool for understanding the mother's childhood experiences and identifying her unresolved trauma and loss. The attachment-derived methods (AAI, EA, and SSP) confirmed that the coherence of the mother's state of mind improved, her strange behavior decreased, and emotional availability to the infant also improved. The case study specifically illustrated that a safe therapy relationship offered the mother a safe place to explore her unresolved experiences while keeping the child in mind.
Strengths and limitations
Some of the questionnaire methods used in this study have not been widely used or validated. Self-reporting has limitations, as participants may underestimate the abuse and give overly positive responses (Suchman et al. 2005). The author's dual role as therapist and researcher was challenging, as the author had to be simultaneously immersed in the therapy process and also in the object of the study.
Results
Psychodynamic mother-infant group therapy
Drug-abusing mothers' resources and mental burden during
As also noted in previous studies (eg, Knight et al. 2001, Nair et al. 2003, Suchman et al. 2005), the drug-using mothers in the present study suffered from an accumulation of stressful life circumstances. However, and consistent with the findings of Field et al. (1998), maternal depressive symptoms decreased in both intervention groups. This idea is supported by the finding based on the same data (Flykt et al. 2012) that the PGT mothers showed increasingly realistic and optimistic representations of themselves as mothers and of their babies from gestation to 12 months postpartum.
Preconditions for program completion and abstinence among
Substance-addicted individuals often grew up in unstable attachment relationships during childhood and adolescence, making them particularly vulnerable to the fragmentation of treatment services (Luthar et al. 2007). It may be that especially positive relationship experiences with other peers (Harwood 2006, Grella et al. 2000) as well as the experiences of success in the maternal role contributed to their commitment to treatment (Pajulo et al. Just like earlier studies, pregnancy recognition before the intervention was the most effective motive to stop using substances (et al. 20 et al. 20).
Effects of interventions on mother-infant interaction quality
The trauma perspective is central, because a drug-free pregnancy forces the mother to confront her painful experiences and current problems underlying the substance abuse (Medrano et al. 2002). It is possible that both substance abuse recovery and traumatization were reasons that prevented the mother from listening to and responding to her baby's needs and communication (Kaiz et al. 2009). The finding supports the observations of Pajulo et al. 2012) that substance-addicted mothers, with greater exposure to physical and emotional trauma, are particularly difficult to treat.
Effects of interventions on infant’s behavior
It is noteworthy that the PGT infants in Study III were more engaged than the PSS infants at 4 months. The duration of the PGT intervention may partially explain this phenomenon, as the PGT infants were only 4–7 months old when the group therapy process ended. As the mothers in the PGT group in study I reported, they also wanted a longer group therapy process.
Attachment-based therapeutic methods in preventing
When the "ghosts have left the room," the mother becomes her child's protector against a repeat of her troubled past (Fraiberg et al., 1987). There may be dual identifications—the therapist and group members may identify with both the neglected child in the mother and her real child. Mary later describes, “Things from my childhood flood my mind and disturb my concentration.
In our groups we used the 'good grandmother transference' and emphasized mothers' positive resources and assets rather than psychopathology and conflicts (Stern, 1995). 1999) "The role of psychopathology in the parenting of drug-addicted women." preliminary evaluation of a pilot project by Fernanda Pedrina'.Group Analysis. Characteristics of substance abuse. The self-administered semi-structured questionnaire was constructed to collect information about drug abuse behavior.
Linda described it this way: 'The untreated traumas were like an attack on me, because the difficult experiences at the beginning of the pregnancy also reawakened the past monsters after Olivia's birth.