INTRODUCTION
Furthermore, very limited human histological data demonstrating the effects of bioabsorbable membranes in the treatment of intrabony defects can be found in the literature [111]. There is increasing evidence in the literature showing that the formation of a new attachment and new bone are not necessarily related phenomena.
QUESTIONS TO BE ANSWERED
CLINICAL STUDIES
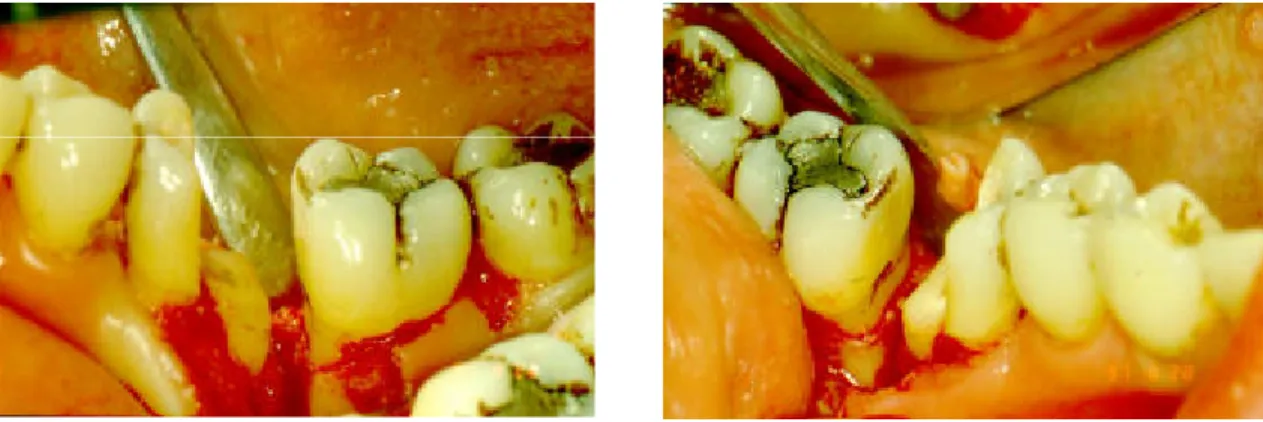
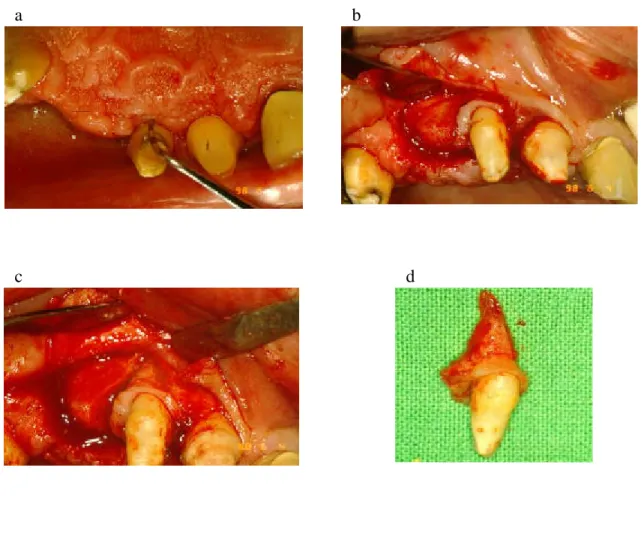
After a healing period of six months, the teeth were extracted together with their surrounding soft and hard tissues and analyzed according to the method described in the next section. After a healing period of six months, the teeth were extracted along with some of their surrounding soft and hard tissues and analyzed as described in the next section.
MATERIALS AND METHODS
Human studies
- Pre-treatment protocol
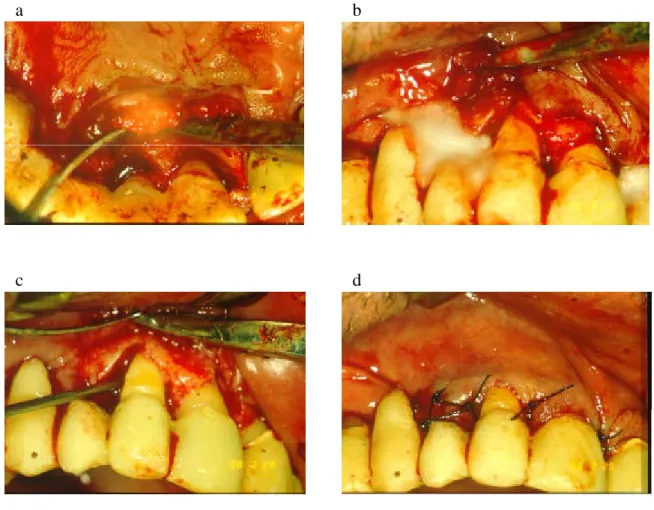
- Surgical procedures
- Surgery at GTR sites
- Surgery at EMD sites
- Post-operative care
- Analytical procedures
- Clinical examinations
- Radiographic examinations
- Histological procedures
The immunohistochemically labeled streptavidin-biotin (LSAB) technique using the DAKO LSAB kit (DAKO, Copenhagen, Denmark) was used according to the manufacturer's instructions. Only sections representing the central part of the defect were analyzed histologically and immunohistochemically.

Experimental protocol in monkeys
- Creating experimental defects
- Surgical interventions
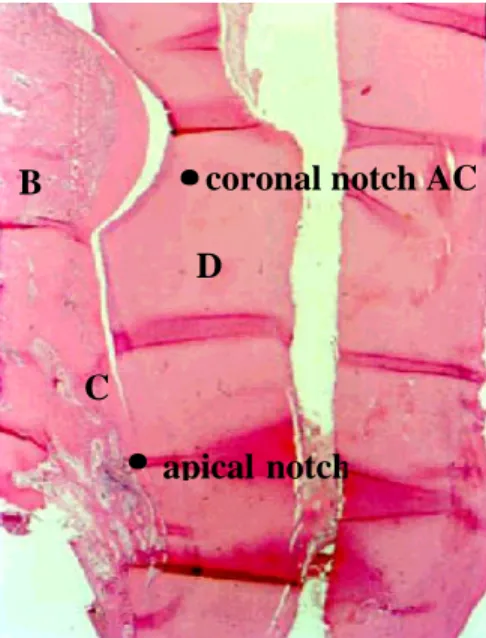
- Histological procedure
Seven weeks after the onset of the defects, the mucoperiosteal flaps were raised, the granulation tissue removed from the defects, and the root surfaces scaled and abraded. A notch indicating the most apical part of the defect was made on the root surface by a slowly rotating circular bur.
Statistical analysis
RESULTS
Guided tissue regeneration (GTR)
As shown in the tables, clinical parameters improved significantly during the first year after surgery regardless of the specific membrane used (p < 0.001). The clinical results recorded 3 years after the intervention did not show further progression of the healing process compared to the first year results. No significant differences between the mean changes in any of the clinical parameters (PPD, GR and CAL) have been revealed in the three different treatment groups.
Histological analysis showed the neoformation of cellular cement with the insertion of collagen fibers accompanied by new alveolar bone as a result of the regenerative procedure. In the second GTR study, 52 defects were treated in 48 patients and clinical outcomes were evaluated one and two years after the regenerative procedure (Study 2). Membrane exposure associated with mild soft tissue inflammation was observed in 20 of 52 sites and was limited to the first month after surgery.
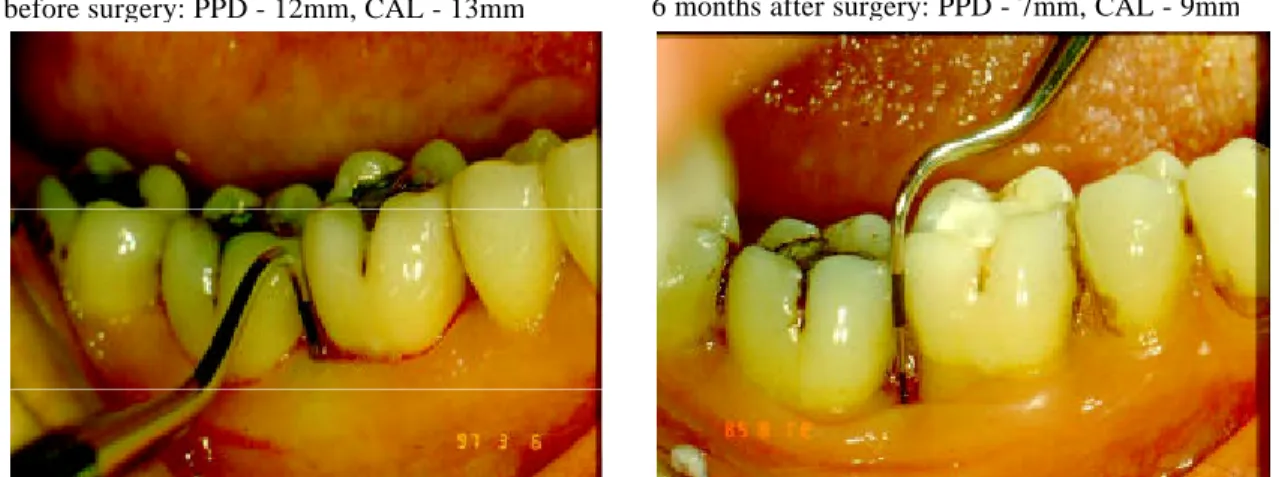
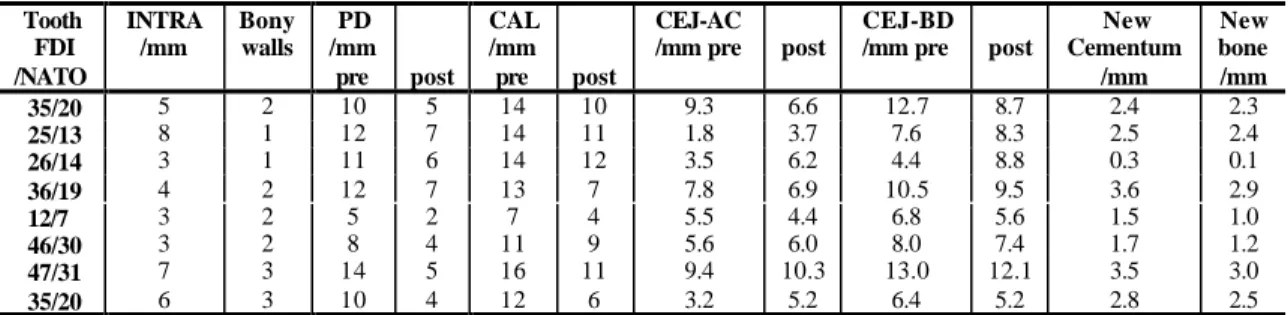
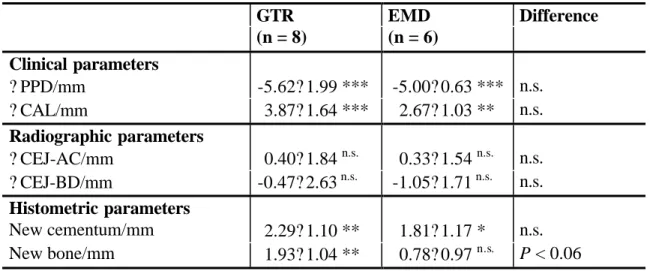
Clinical and radiographic data measured at baseline and 6 months after surgery, along with the histometric results for each individual defect, are summarized in Table 6.
Enamel Matrix Derivate (EMD) -treated defects
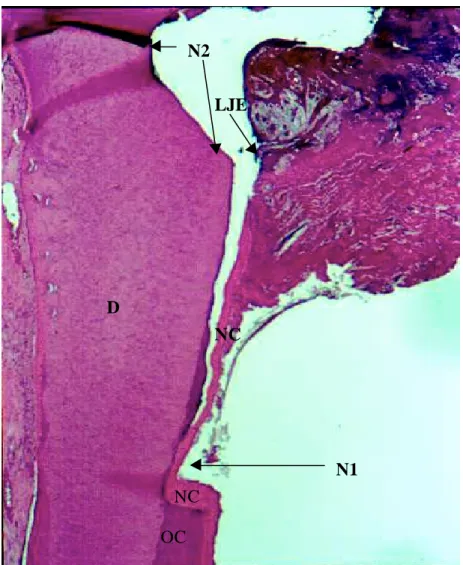
The histological assessment revealed the formation of 4.82 mm of new cementum with inserted collagen fibers covering the previously diseased root surface. An artifact (a gap between the new cementum and the dentine surface) was observed along the entire root surface. New cementum (NC), with the insertion of collagen fibers, has formed on the root surface in the area delimited by the apical (N1) and the coronal notch (N2).
In contrast to case 1 in which new cementum formed without any bone formation, in case 2 almost the same amount of cementum and new bone was recorded. In our second EMD study, clinical and radiographic outcomes were compared with histologically detected new tissue growth in teeth treated with EMD planned for extraction (Study 4). In two cases, a slight swelling of the operated areas was observed after surgery, which was probably caused by surgical trauma.
The current results suggest that treatment of intrabonal defects with EMD can lead to significant improvements in all clinical parameters studied, although the new cement was not always associated with new bone formation.
Comparing GTR and EMD procedures
No statistically significant differences were observed in any of the clinical and radiographic parameters between the GTR and EMD groups. Histometrically, statistically significant amounts of new cement were observed in both groups and of new bone in the GTR group, whereas the amount of new bone in the EMD group could not be proven statistically significant. This means that the GTR procedure provides a more favorable regeneration of new bone within the relatively short time horizon of the study (6 months).
Clinical, radiographic and histometric data show different projections of the healing process after regenerative surgery. Both CAL gain and radiographic data (BD) correlate (to varying degrees) with the amount of new cement formed as a result of regenerative therapy. The CAL increase is also linearly related to the new bone, but BD fails to correlate with this hard outcome measure.
Overall comparison of regenerative procedures
The mean PlI, GI and BOP for each of the four treatment groups at baseline and 1 year after surgery (Study 8). At baseline, no statistically significant differences were found in any of the investigated parameters between the four groups. The gingival condition improved significantly compared to baseline (p < 0.001) by the end of the first year after surgery, but this improvement was found to be similar in the different groups.
At the end of the first year, PPD decreased significantly in all groups (p < 0.001). CAL also improved significantly in each group (p < 0.001) regardless of the regenerative surgery used. However, a statistically significant difference was found between EMD, GTR, EMD+GTR on the one hand and the control treatment on the other (p < 0.05).
Membrane exposure occurred at six sites treated with GTR alone and at five sites treated with EMD+GTR.
Histological observations
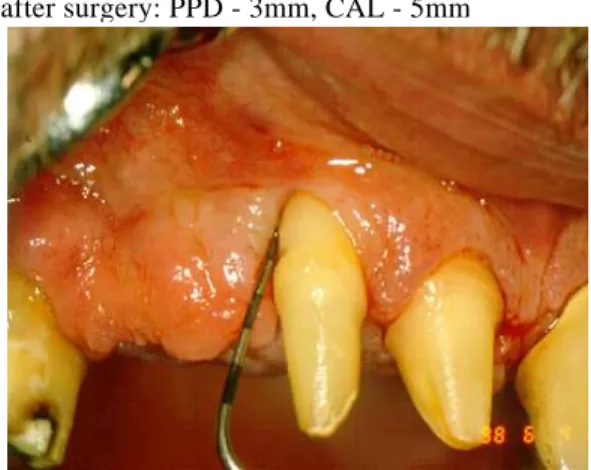
The exposed parts of the membranes disintegrated within a few days of exposure without any side effects. Higher magnification of the regenerated area: The newly formed cementum, periodontal ligament and bone are clearly distinguishable. In the healthy site of the extracted root samples serving as a control, oxytalan fibers with more elastic connections were registered using the connective tissue differentiating staining.
These fibers showed a mainly apico-occlusal orientation with localization closer to the cementum than to the alveolar bone. The regenerated oxytalan fibers were always closer to the newly formed cementum than to the alveolar bone and had a similar morphological appearance to that observed in sites with an intact periodontal ligament. Collagen fibers were incorporated into the newly formed cement in all samples showing reattachment.
In one of the samples, the healing resulted in a long junctional epithelium (LJE) to the base of the defect.
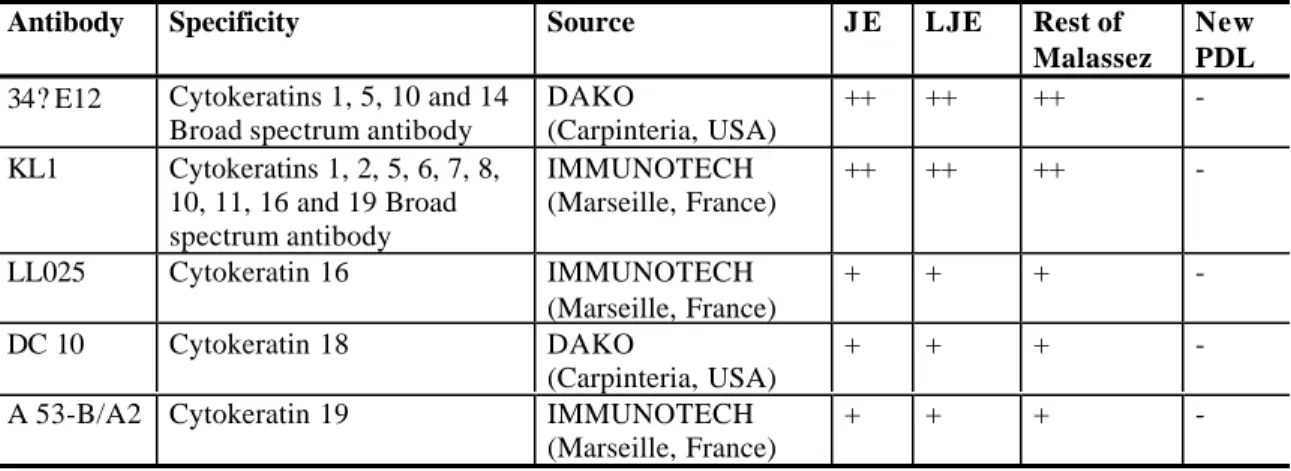
Immunohistochemical findings
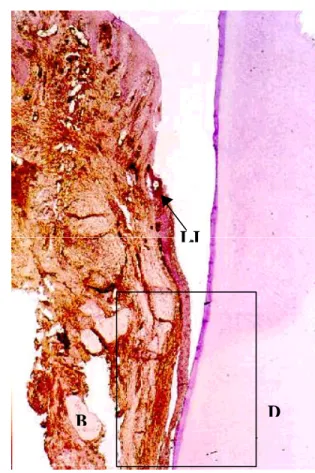
The reformed junctional epithelium showed a similar pattern of cytokeratin expression to that observed in untreated specimens. Histological images of the reformed junctional epithelium after reparative therapy with conventional flap surgery are shown in Figures 17-19. The healing result was primarily a long junctional epithelium (LJE) and no cementum and periodontal ligament formation.
Healing resulted mainly in a long junctional epithelium (LJE) and only limited bone formation (B) at the bottom of the defect. No cytokeratin expression was present after staining with any of the broad-spectrum or individual monoclonal antibodies in the newly formed monkey and human PDL. The newly formed PDL was always continuous with the original PDL present in the apical part of the defects.
No staining with KL1 broad-spectrum monoclonal antibody against cytokeratins is observed in the regenerated area.
DISCUSSION
The clinical impact of the different regenerative interventions
- Healing following GTR treatment
- Healing following EMD therapy
- Combined therapy
- Comparing healing following GTR and EMD treatments
In the first long-term (3-year) evaluation of the GTR procedure with non-resorbable membranes, Gottlow et al. These results are consistent with our long-term (3-year) observation, in which the majority of postoperative CAL gains occurred over 3 years could be kept. Deviations in the results can be explained by the different configuration and/or depth of the initial defects treated.
In addition, it has been demonstrated that in situations where the space between the internal surface of the membrane and the root surface can be maintained, regeneration of new attachment and alveolar bone can be achieved simultaneously [81]. In those studies, the treatment with EMD + GTR predictably led to new attachment and new bone formation, but the amount of the newly formed tissue was not better compared to single therapies [2, 86]. It cannot be excluded that with a further improvement of the plaque control a higher CAL increase can be obtained.
Treatment with EMD has been shown to result in the formation of a new connective tissue attachment and to some extent bone regeneration in 6 of 7 treated defects, while GTR treatment resulted in the formation of new cementum and new bone in 7 of 8 defects .
Histological evidence about the type of healing after regenerative therapy
- Oxytalan fibres
- Expression of cytokeratin
- Vimentin expression
This is consistent with our finding that the formation of new bone was less pronounced in the EMD group at 6 months after treatment. Animal studies indicated that regenerative treatments can, to a certain extent, result in the formation of new cementum and new bone [92]. Recently, in a monkey experiment, oxytalan fibers have been observed in the newly formed periodontal ligament after regenerative periodontal treatment [93].
It was indicated that Malassez's epithelial remnants may show different patterns of cytokeratin expression depending on the degree of inflammation present in the periodontal ligament [83]. In contrast, no cytokeratin expression was observed when healing occurred in the formation of a new PDL. In our present study, no differences were found in the cytokeratin expression between epithelial remnants of Malassez and junctional epithelium.
In the inflamed periodontium, the probe does not stop exactly at the coronal level of the attachment of the connective tissue.
CONCLUSIONS
Guided tissue regeneration in Class II furcation involved maxillary molars: a controlled study of 8 cleft mouth cases. Histological assessment of new attachment after treatment of a human buccal recession by means of a guided tissue regeneration procedure. Clinical evaluation of guided tissue regeneration in the treatment of maxillary class II molar furcation intrusions.
New attachment and bone formation in periodontal defects after treatment of submerged roots with guided tissue regeneration. Comparison of intrabony defect treatments with enamel matrix derivative, guided tissue regeneration with a nonresorbable membrane, and a modified Widman flap. Generalizability of additional benefits of guided tissue regeneration in the treatment of deep intraosseous defects.
Factors influencing the healing response of intrabony defects after guided tissue regeneration and access flap surgery.