J of Evolution of Med and Dent Sci/ eISSN- 2278-4802, pISSN- 2278-4748/ Vol. 4/ Issue 48/ June 15, 2015 Page 8266
MINILAPAROTOMY, POST LSCS TUBECTOMY AND DOUBLE PUNCTURE
LAPAROSCOPIC (DPL) STERILIZATION TECHNIQUES FOR TUBAL
STERILIZATION: AN EXPERIENCE AT TERTIARY CARE CENTRE
N. Chandraprabha1, L. Jhansi Rani2, Prasad Usha3, Divya Shravani Kaminedi4, Prasad Uma5
HOW TO CITE THIS ARTICLE:
N. Chandraprabha, L. Jhansi Rani, Prasad Usha, Divya Shravani Kaminedi, Prasad Uma. Minilaparotomy, Post LSCS Tubectomy and Double Puncture Laparoscopic (DPL) Sterilization Techniques for Tubal Sterilization: An Experience at Tertiary Care Centre . Journal of Evolution of Medical and Dental Sciences 2015; Vol. 4, Issue 48, June 15; Page: 8266-8270, DOI: 10.14260/jemds/2015/1199
ABSTRACT: BACKGROUND: For tubal sterilization many techniques are available which are safe with minimal complications. There are few published articles in India which compare the efficacy of various techniques and their failure rates. In the present study an effort was made to assess the failure rates of various commonly adopted procedures. AIM OF THE STUDY: To assess the failure rates and complications of minilaparotomy, post LSCS tubectomy and double puncture laparoscopy (DPL). MATERIAL AND METHODS: This is a five year study from April 2010 to March 2015 at a tertiary care Centre. The number of cases which underwent minilaparotomy (Pomeroy technique), post LSCS tubectomy and double puncture laparoscopy (DPL) were recorded. Their failure rates and complications were documented. RESULTS: Total number of cases who underwent sterilization procedures were 8264. The cases who adopted minilap (Pomeroy technique) as sterilization procedure were 2427/8264 (29.36%), double puncture laparoscopy with falope rings were 1601/8264 (19.37%) and tubectomy after LSCS were 4236/8264 (51.25%). The failure rates in minilap was 0.206%, DPL was 0.562% and post LSCS tubectomy was 0.613%. CONCLUSION: At a tertiary care Centre DPL and post LSCS tubectomy can be adopted easily as it need expertise. In tubectomy camps minilap (Pomeroy technique) is still preferable.
KEYWORDS: DPL, Minilap, Post LSCS tubectomy, Tubal sterilization.
INTRODUCTION: Sterilization techniques just like other surgical techniques have undergone evolution and many techniques have come into effect. The techniques for sterilization commonly implemented in India are; minilaparotomy with occlusion by the modified Pomeroy technique, minilaparotomy with occlusion by the tubal ring, laparoscopy with occlusion by the tubal ring and tubal ligation after caesarian section. In developed countries sterilization is generally done by laparoscopy rather than by minilaparotomy but in developing countries, where the resources are limited for the purchase and maintenance of the more sophisticated laparoscopic equipment, minilaparotomy may still be the most common approach. In the present study a review was done to known the methods of sterilization preferred at our centre and their failure rates.
J of Evolution of Med and Dent Sci/ eISSN- 2278-4802, pISSN- 2278-4748/ Vol. 4/ Issue 48/ June 15, 2015 Page 8267
for surgery. All the patients were starved overnight. For minilaparotomy the patient was injected with appropriate doses of Fortwin and phenergan. A small (Usually less than 5 cm) suprapubic incision was given, the abdomen was opened in layers, and the tubes were ligated either by rings or by ligating both ends after cutting a portion of the tube. Standard surgical instruments were used. For double puncture laparoscopic method injection atropine sulfate 0.5 mg was given intramuscularly half an hour before the operation. The laparoscopic approach uses a long thin needle inserted through the umbilicus into the peritoneal cavity, through which gas (primarily CO2) is introduced to
induce pneumoperitoneum. Tubal occlusion was achieved with Falope rings. All sterilization procedures were performed by gynecologist with DPL training. After an uneventful operation, the patients were discharged on the same day. With development of any complication, they were treated appropriately and kept under observation till such time as it was deemed safe to discharge them. All the patients were followed up for detecting late complications and failure of sterilization procedure.
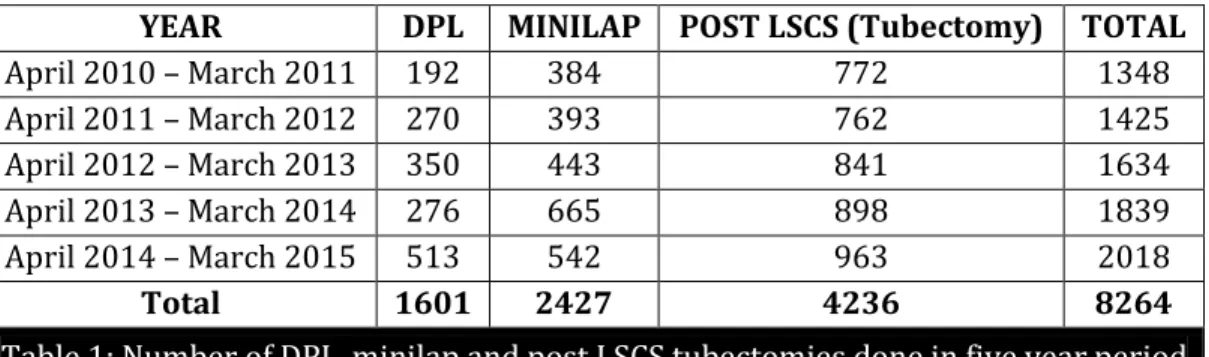
RESULTS: Total number of cases who underwent sterilization procedures were 8264. The cases who adopted minilap (Pomeroy technique) as sterilization procedure were 2427/8264(29.36%), double puncture laparoscopy with falope rings were 1601/8264(19.37%) and tubectomy after LSCS were 4236/8264(51.25%). The proportion of cases adopting double puncture laparoscopy with falope rings when compared with minilap procedure increased from year 2010 to 2015. (1:2 to 1:1). (Table 1). The failure rates in minilap was 0.206%, DPL was 0.562% and post LSCS tubectomy was 0.613%. (Table 2). The commonest complications encountered with double puncture laparoscopy with falope rings was infection at the port site(0.62%) and bleeding from port site (0.24%) followed by surgical emphysema (0.12%). The complications in minilap procedure was bowel injury(0.24%), infection (0.16%) and bladder injury(0.12%).Complications commonly associated with post LSCS tubectomy was infection (0.35%).(Table 3)
DISCUSSION: Laparoscopic tubal ligation is an outpatient surgery with a rapid recovery, allowing patients to return quickly to work or home. Laparoscopic tubal ligation is attractive to surgeons because many gynecologists are well trained in laparoscopic techniques and it involves a short operating time. Very few studies are documented in English literature comparing minilaparotomy (Pomeroy technique), post LSCS tubectomy and double puncture laparoscopy (DPL) for tubal sterilization.
Mumford SD et al [1] in their study compared minilaparotomy (Pomeroy technique) and
double puncture laparoscopy (DPL)for tubal sterilization from 23 countries. Number of cases who underwent laparoscopy with occlusion by the tubal ring was 7053, and minilaparotomy with occlusion by the modified Pomeroy technique was 5081 cases. The failure rate was 0.60% for laparoscopy/ring and 0.30 per 100 women for minilaparotomy/Pomeroy. The surgical complication rate for laparoscopy/ring (2.04%) was more than twice that for minilaparotomy/Pomeroy (0.79%). The technical failure rate of minilaparotomy/Pomeroy was twice that of laparoscopy/ring but the complication was less. They preferred minilaparotomy procedure for many women than laparoscopy procedure.
Peterson HB et al[2] in their study the failure of laparoscopic sterilization by Falope ring was
J of Evolution of Med and Dent Sci/ eISSN- 2278-4802, pISSN- 2278-4748/ Vol. 4/ Issue 48/ June 15, 2015 Page 8268
morbidity and mortality patterns in minilaparotomy and laparoscopic procedures and their observations were: there was no difference in major morbidity between the 2 groups. Minor morbidity was significantly less in the laparoscopy group. Duration of operation was about 5 minutes shorter in the laparoscopy group. J H Meyer[4] reports five experiences with laparoscopic falope ring
tubal sterilization: The few complications encountered were mostly of a technical nature and considered minor. With 90% of the patients available for follow-up there has been no evidence of long-term adverse effects.
Alexander W. Huber et al[5] evaluated whether intra- and post-operative morbidity varies
according to the method used for female sterilization for a period of nine years. He divided the cases into three groups (1) interval laparoscopic sterilization unrelated to pregnancy (n=20,325); (2) postpartum laparoscopic sterilization (n=2233); (3) postpartum sterilization by minilaparotomy (n=5095). Intra-operative and post-operative complications were compared according to the surgical approach. The proportion of major complications was higher in group 3 than in group 1 but not statistically different between groups 1(0.10%) and 2(0.18%). Minor complications were statistically significantly more frequent in group 3(0.82%) than in group 1(0.26%) or group 2(0.27%). There was no case of intra-operative or post-operative death in the study population.
In the present study the method of sterilization adopted most commonly was post LSCS tubectomy with failure rate of 0.613%. The failure rates in minilap (0.206%) and double puncture laparoscopic method with falope rings was 0.562%. The commonest complications encountered with double puncture laparoscopy with falope rings was infection at the port site (0.62%). The complications in minilap procedure was bowel injury (0.24%) and post LSCS tubectomy was infection (0.35%).
CONCLUSION: When available, a laparoscopic approach should be chosen for female sterilization. After uneventful pregnancy course and delivery, it does not seem justified to delay the endoscopic sterilization to a later time. Disadvantages of laparoscopic tubal ligation include the need for anesthesia and cost of laparoscopic equipment. All sterilization methods have risks of failure. Laparoscopic tubal occlusion is seen to be a safe, simple and effective means of female sterilization which can be performed by gynecologists trained in laparoscopy.
REFERENCES:
1. Mumford SD, Bhiwandiwala PP, Chi IC. Laparoscopic and minilaparotomy female sterilization compared in 15 167 cases. Lancet. 1980 Nov 15; 2(8203): 1066-70.
2. Peterson HBl, Xia Z, Hughes JM, Wilcox LS, Tylor LR, Trussell J. The risk of pregnancy after tubal sterilization: findings from the U.S. Collaborative Review of Sterilization. Am J Obstet Gynecol. Apr 1996; 174(4): 1161-8.
3. Kulier R, Boulvain M, Walker D, Candolle G, Campana A. Minilaparotomy and endoscopic techniques for tubal sterilization. Cochrane Database Syst Rev. 2004; (3): CD001328.
4. J H Meyer. A five experience with laparoscopic falope ring sterilization. Int J Gynaecol Obstet 1982; 20(3): 183-7.
J of Evolution of Med and Dent Sci/ eISSN- 2278-4802, pISSN- 2278-4748/ Vol. 4/ Issue 48/ June 15, 2015 Page 8269 YEAR DPL MINILAP POST LSCS (Tubectomy) TOTAL
April 2010 – March 2011 192 384 772 1348 April 2011 – March 2012 270 393 762 1425 April 2012 – March 2013 350 443 841 1634 April 2013 – March 2014 276 665 898 1839 April 2014 – March 2015 513 542 963 2018
Total 1601 2427 4236 8264
Table 1: Number of DPL, minilap and post LSCS tubectomies done in five year period
Procedure Number of Cases Failure Rate in Percentage
MINILAP 5 0.206
DPL 9 0.562
POST LSCS 26 0.613
Table 2: Failure rate of various procedures
COMPLICATIONS NUMBER OF CASES PERCENTAGE MINILAP
Hemorrhage Infection Bowel injury Bladder injury
2427 2 4 6 3
0.08 0.16 0.24 0.12 DPL
Surgical emphysema Bleeding from port site
Omental prolapse Incisional Hernia Infection of port site
Neurogenic shock
1601 2 4 1 1 10
1
0.12 0.24 0.062 0.062 0.62 0.062 Post LSCS tubectomy
Infection Bowel injuries
Hemorrhage
4236 15
1 1
0.35 0.023 0.023
J of Evolution of Med and Dent Sci/ eISSN- 2278-4802, pISSN- 2278-4748/ Vol. 4/ Issue 48/ June 15, 2015 Page 8270
AUTHORS:
1. N. Chandraprabha 2. L. Jhansi Rani 3. Prasad Usha
4. Divya Shravani Kaminedi 5. Prasad Uma
PARTICULARS OF CONTRIBUTORS:
1. Assistant Professor, Department of Obstetrics & Gynaecology, Andhra Medical College, Visakhapatnam, Andhra Pradesh. 2. Associate Professor, Department of
Obstetrics & Gynaecology, Andhra Medical College, Visakhapatnam, Andhra Pradesh. 3. Assistant Professor, Department of
Obstetrics & Gynaecology, Andhra Medical College, Visakhapatnam, Andhra Pradesh.
FINANCIAL OR OTHER
COMPETING INTERESTS: None
4. House Surgeon, Andhra Medical College, Visakhapatnam, Andhra Pradesh. 5. Associate Professor, Department of
Pathology, RIMS, Srikakulam, Andhra Pradesh.
NAME ADDRESS EMAIL ID OF THE CORRESPONDING AUTHOR:
Dr. Prasad Uma, Q. No. 49-3-3, Lalithanagar,
Visakhapatnam-530016, Andhra Pradesh.
E-mail: usha1966411@gmail.com