REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Intrathecal
sufentanil
for
coronary
artery
bypass
grafting
Caetano
Nigro
Neto
a,∗,
Jose
Luiz
Gomes
do
Amaral
b,
Renato
Arnoni
a,
Maria
Angela
Tardelli
b,
Giovanni
Landoni
caInstitutodeCardiologiaDantePazzanese,UniversidadeFederaldeSãoPaulo,SãoPaulo,SP,Brazil bUniversidadeFederaldeSãoPaulo,SãoPaulo,SP,Brazil
cUniversitàVita-SaluteSanRaffaele,Milano,Italy
Received11May2012;accepted11December2012 Availableonline11October2013
KEYWORDS
Cardiacsurgery; Spinalanesthesia; Sufentanil; Interleukin6
Abstract
Context: Cardiacsurgerypatientsundergoingcoronaryarterybypassgraftingwith cardiopul-monarybypass.
Objective: Evaluatetheeffectofaddingintrathecalsufentaniltogeneralanesthesiaon hemo-dynamics.
Design:Prospective,randomized,notblindedstudy,afterapprovalbylocalethicsinResearch Committee.
Setting: Monocentricstudy performedatDantePazzaneseInstituteofCardiology,SaoPaulo, Brazil.
Patients:40consentingpatientsundergoingelectivecoronaryarterybypass,bothgenders.
Exclusioncriteria:Chronickidneydisease;emergencyprocedures;reoperations; contraindica-tion tospinalblock;leftventricularejectionfractionlessthan40%;bodymassindexabove 32kg/m2anduseofnitroglycerin.
Interventions:Patientswererandomlyassignedtoreceiveintrathecalsufentanil1g/kgornot. Anesthesiainducedandmaintainedwithsevofluraneandcontinuousinfusionofremifentanil.
Mainoutcomemeasures: Hemodynamicvariables, bloodlevelsofcardiactroponin I,B-type natriureticpeptide,interleukin-6andtumornecrosisfactoralfaduringandaftersurgery.
Results:Patientsinsufentanilgrouprequiredlessinotropicsupportwithdopaminewhen com-paredtocontrolgroup(9.5%vs58%,p=0.001)andlessincreasesinremifentanildoses(62% vs 100%, p=0.004).Hemodynamic dataateight differenttimepointsandbiochemicaldata showednodifferencesbetweengroups.
Conclusions: Patientsreceivingintrathecalsufentanilhavemorehemodynamicalstability, as suggestedbythereducedinotropicsupportandfeweradjustmentsinintravenousopioiddoses. © 2013SociedadeBrasileirade Anestesiologia.Publishedby ElsevierEditoraLtda.Allrights reserved.
∗Correspondingauthor.
E-mail:caenigro@uol.com.br(C.NigroNeto).
0104-0014/$–seefrontmatter©2013SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Allrightsreserved.
Introduction
Intrathecalopioidsincombination withgeneralanesthesia reducepainintensityandanestheticsconsumption facilitat-ingearlyremovaloftheendotracheal tube andimproving postoperative analgesia in patients undergoing coronary arterybypassgrafting(CABG)withcardiopulmonarybypass (CPB). Furthermore, they can decrease surgical stress response and have cardioprotective effects.1---5 In CABG
surgery, prevention of perioperative adverse events, such as tachycardia and myocardial infarction, is advisable. Hemodynamicstabilityandreductionofstressresponse con-tribute,inpart,toreducemyocardialdamage.1,6
Compared tomorphine,intrathecal sufentanil provides faster and more intense analgesia.3,7 In fact, because of
morphine’slipidsolubility,analgesiceffectsafter intrathe-calinjectionaredelayed andonly largeintrathecal doses (10mg)mayinitiatereliableintraoperativeanalgesiainthis setting.3Besidesthat,someauthorssuggestthat
intrathe-calsufentanilprovidesbetterhemodynamicstabilitywhen comparedtootheropiods.2,8
Theaimofthisstudywastoevaluate,forthefirsttime, thehemodynamiceffectsofaddingintrathecalsufentanilto generalanesthesiain patients undergoingcoronaryartery bypassgraftingwithcardiopulmonarybypass.
Methods
Ethicalapprovalforthisstudy(protocolnumberCEP3458) wasprovidedbytheEthicalCommitteeCEPIstitutoDante PazzaneseofSãoPaulo,Brasilon29August2006.After writ-teninformedconsentweenrolled40patientsscheduledto undergoelectiveCABGwithCPBwithtwotofourgrafts,with onegraftalwaysbeingtheleftinternalmammaryarteryand theothersthesafenamagnavein.
Exclusion criteriawere: chronic kidney disease; emer-gencyprocedures;reoperations;contraindicationtospinal blockaccordingto2002AmericanSocietyofRegional Anes-thesia Consensus Conference9; left ventricular ejection
fractionlessthan40%;bodymassindex(BMI)above32kg/m2 anduseofnitroglycerin.
Patients were randomly assigned to two different anesthetic protocols (sufentanil group or control group) dependingonreceivingornotintrathecalsufentanil.A com-putergeneratedrandomtable determinedin whichgroup patients were allocated. The participants’ randomization assignmentwasconcealedinanenvelopeuntilthelast avail-ablemoment(startofanesthesia).
Patientsreceivedtheirusualmedicationsuntilthedayof operation,withtheexceptionoforalhypoglycemicagents, whichwerediscontinuedand/orreplacedbyinsulinatleast threedaysbeforesurgery. Allpatients received7.5mgof midazolamintramuscularly1hbeforesurgery.
Monitoring included continuous electrocardiography of theDIIandmodifiedV5,analysisoftheSTsegmentinDII, DI and modified V5 derivations, pulse oximetry, invasive meanbloodpressure(MAP)positionedintheradialartery, analysisof the bispectral index (BIS),capnography, blood gasanalysis,temperaturemeasurementat thelowerthird of the esophagus, urinary catheterization, assessment of neuromuscularfunctionwithTOFWATCHandevaluationof
hemodynamicdatamadewithapulmonaryarterycatheter (Swan-Ganzmodel, continuous output),positioned onthe right subclavianvein (monitor VigilanceII®, Edwards Life-sciences,Irvine,CA,USA).
In sufentanil group, after initial monitoring, patients were placed in a sitting position and underwent lumbar punctureintheL3---L4spacewitha25gaugeWhitacre nee-dle. After confirmation of puncture of the subarachnoid space,successfulspinalwasgiventoallthesepatients,5mL of saline solution 0.9% containing 1g/kg sufentanil (and
never morethan 100g) wasinjected over a 10s period.
Generalanesthesiawastheninitiated.
Incontrolgroup,generalanesthesiawasinitiated imme-diatelyafterinitialmonitoring.
Allpatients underwentinhalation induction asfollows: facialmask withusing2% sevofluranein 100%oxygen and fresh gas flow of 6L/min for 30s. Inspired concentra-tion ofsevoflurane wasthen increasedto 7%until loss of consciousness and then reduced to 2%. Next, intravenous infusion of remifentanil began at a dose of 1g/kg for
1min and 0.1mg/kg pancuroniumwas administered3min before tracheal intubation. Volume-controlled ventilation was started with the following parameters: tidal volume 8---10mL/kg,respiratoryrateadequatetomaintainendTidal CO2 between 30 and 35mmHg and fresh gas flow of 2L with60%fractionofinspiredoxygenmixedwithcompressed air.
Themaintenanceofanesthesiaintheperiodbeforeand after CPB was performed withsevoflurane in the expired fraction with variationbetween 0.5% and 2% to maintain theBISbetween40and65.Remifentanilwasadministered at aninfusion rateupto0.4g/kg/mintomaintainmean
arterialpressurelevelsbetween 60and80mmHg.Abolus of0.02mg/kgpancuroniumwasadministeredwhenthethird responsetothesequenceoffourstimuliappearedintheTOF WATCHmonitoruntiltheendoftheprocedure.
DuringCPB,anesthesiawasmaintainedwithsevoflurane atlevelsbetween0.5%and2%administeredtogetherwitha mixtureofoxygenandcompressedairintheoxygenator cir-cuitthroughcalibratedvaporizertomaintaintheBISvalue between40and65andremifentanilupto0.4g/kg/minfor
controlofmeanarterialpressurebetween45and70mmHg. Uponcompletionofthesurgicalprocedure,allpatients receivedacontinuousintravenousinfusion of2g/kg/min
propofol as a sedative and were transferred to the ICU, wheretheyremainedsedatedfora1-hperiod.The analge-siaprotocolwasinitiatedwithinthefirst24hwithasingle intravenous dose of 1g/kg fentanyl togetherwith 1g of
dypirone.The same dose of dypironewasrepeated every 6h.
After tracheal extubation, patient control analgesia (venous PCA) with aVigon® PCA pump wasthen installed withthefollowingparameters:bolusonlymode,1mgbolus and a fixed 7-min lockout interval. During this period, if therewassignificantpain(VAS>7),100mgoftramadolwas administeredintravenously.DischargefromtheICUand hos-pitalwerefollowedbylocalprotocols.
HypotensionwasdefinedasaMAP<60mmHg(<45mmHg duringCPB),formorethan30s.Hypertensionwasdefined as MAP>80mmHg (>70mmHg during CPB), for more than 30s.
Management of hypotension included phenylephrine 0.1mg bolus (when anesthetic agents were at mini-mum levels,could be repeated every minute), dopamine (when anesthetic agents were at minimum levels, fill-ing pressures were high and when CI was less than 2.4L/m2/min) at a dose of 5
g/kg/min with
incre-ments of 1g/kg/min until the desired MAP level was
reached, norepinephrine (when the CI remained below 2.4L/m2/minatdopaminedosesof10
g/kg/min)atadose
of 0.1g/kg/min,with incrementsof 0.1g/kg/min until
thedesiredMAPlevelwasreached.Dopamineuse,asa pri-maryendpoint,wasstrictlyregulatedbyprotocols,suchas documentedlow CI(less than 2.4L/m2/min), high CVP or PCWP.
Hypertension managementincludedremifentanil(bolus 0.5g/kg followed by an infusion dose increase of
0.1g/kg/min with the sequence repeated every minute
till a maximum infusion rate dose of 0.4g/kg/min),
fol-lowedbysodiumnitroprusside(0.5g/kg/minandincreased
by 0.5g/kg/min increments until the maximum dose of
2g/kg/min was reached). Sevoflurane was used when
the BIS value exceeded 65. The inspired sevoflurane concentration was increased to 4% and fresh gas flow to 6L/min for 1min while the fresh gas flow was returned to2L/minandthesevofluraneconcentrationwasreduced to 2%. If the BIS did not return to pre-established lev-els,the procedure wasrepeated andin the absence of a response, a dose of 0.05mg/kg midazolam was adminis-tered.
Clampingoftheaorta(maximumduration15minwithan intervalofatleast2min)wasperformedinmild hypother-mia(34◦C).Salinesolutionwasusedtofillthemembrane
oxygenator(Vital®---Nipro,Brazil).
Alldata werecollectedbytrainedobservers whowere notblindedtotheanestheticregimenused.
Blood tests included cardiac troponin I (cTnI), mea-sured using an immunoassay method (CMIA --- Architect®; Abbott Laboratories, Brazil, --- the normal range being 0---0.3ng/mL), B-typenatriureticpeptide(BNP),measured using an immunoassay method (MEIA --- AxSIM® system; Abbott Laboratories, Brazil --- with values of 1400pg/mL for patients with NYHA functional classI and 3400pg/mL for thosewithfunctional classII being considered normal limits), interleukin 6 (IL-6) and tumor necrosis factor ␣
(TNF␣)measured usingan immunometricassaymethodby
theIMMULITE®system---SiemensMedical,USA---thenormal rangebeing<3.4pg/mLforIL6and<8.1pg/mLforTNF␣.All
bloodtestsweremeasuredatbaselinewhileBNPandcTnI weremeasured24hafterCPBandIL-6andTNF␣10minafter
anesthesiainduction,15min,6h,24hafterCPBand4days postoperatively.
On the basis of previous personal data we anticipated thattheamountofpatientsneedinginotropicsupportwith dopaminewouldhave been10% and50%in sufentaniland control group, respectively. We calculated thatwe would need a sample size of 20 patientsper group. Allpatients were analyzed according to the intention-to-treat princi-ples,beginningimmediatelyafterrandomization.
1000
100
T0 GroupN GroupST0
T1 T1
Log
10
(pg/mL)
T2 T2
T3 T3
T4 T4
T5 T5 10
1
IL 6
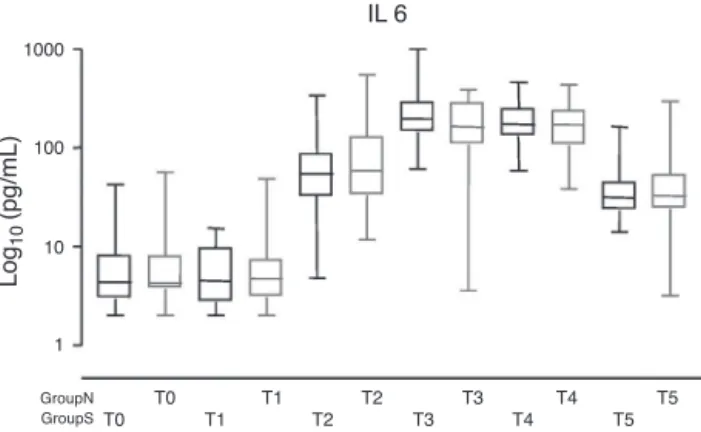
Figure1 Bloodlevelsofinterleukin6(IL-6).
Statistical
analysis
Data were expressed as number (percentage), mean±standard deviation, or median (interquartile range). Student’s t-test, Fisher’s exact test, Pearson’s chi-squaredanalysisandMann---Whitneynonparametrictest wereusedwhen appropriateusingthe Statistical Package for the Social Sciences software (SPSS). ANOVA analysis wasusedfor repeatedmeasurescontinuous data,such as biochemicalmarkers.
Results
Preoperativedatawere well balanced betweensufentanil and control group (Table 1). Patients in sufentanil group requiredless inotropicsupportwithdopamine at weaning fromCPB andafter CPBwhen comparedto controlgroup (9.5%vs58%p=0.001)andlessincreasesinremifentaniluse (62%vs100%p=0.004)asshowedinTable2.
Cardiac troponin I was detectable in all patients postoperatively, with no differences between groups: 1.62 (0.80---5.59)ng/mL in sufentanil group vs 1.68 (0.73---3.53)ng/mL in control group (p=0.506). Similarly, BNP was detectable in all patients postoperatively, with nodifferences between groups (p=0.667). BNPincreased from36.13 (21.70---73.79)pg/mL preoperatively to 207.58 (89.95---236.77)pg/mLpostoperativelyinsufentanilgroupvs 39.15(25.77---54.88)pg/mLto188.97(84.31---247.96)pg/mL in control group. Blood levels of IL-6 (Fig. 1) and TNF␣
(Fig.2)weresimilarbetweengroups.
1000
100
T0 T0 T1
T1
Log
10
(pg/mL)
T2
T2 T3 T3 T4
T4 T5
T5 10
1
TNFα
GroupN GroupS
Table1 Patients’characteristicsandsurgicaltimes.Dataareexpressedasnumber andpercentagesorasmean±standard deviations.
Controlgroup
n=19
Sufentanilgroup
n=21
Preoperativedata
Femalegender 6(32%) 7(33%)
Age(years) 56±7.2 58±6.7
Bodymassindex(kg/m) 26±3.9 27±2.5
ASAII 19(100%) 20(95%)
ASAIII 0 1(4.8%)
NYHAI 7(37%) 9(43%)
NYHAII 12(63%) 12(57%)
DiabetesMellitus 6(32%) 9(43%)
Hypertension 15(79%) 19(90%)
Dyslipidemia 11(58%) 16(76%)
Smoking 5(26%) 10(48%)
Previousmyocardialinfarction 5(26%) 6(28%)
Intra-operativedata
Durationofanesthesia(min) 299±57 292±39.4
Durationofsurgery(min) 235±51.7 223±35.5
Durationofischemia(min) 52±14.9 50±15.0
Durationofperfusion(min) 74±23.0 69±20.0
Hemodynamicdataat eightdifferenttimepoints (sup-plementalmaterialIonline)showednodifferencesbetween groupswithexceptionofminordifferenceafterCPB.
Noepisodesofawarenessweredetectedinthisstudy.
Table3 shows similarconsumptionof analgesicsduring
thefirst24postoperativehoursbetweengroups.
Timeonmechanicalventilationwas300(212---450)vs255 (230---315)min incontrolandsufentanilgrouprespectively (p=0.4), while ICU stay was 2.7+0.89 vs 3.9+3.75 days (p=0.2)andhospital stay was8.9+6.98 vs 9.1+6.1 days, respectively.
Table4showsthattherewasnodifferencein postopera-tivecomplicationsexceptfortheneedforbloodtransfusion, whichwassignificantlyhigherincontrolgroup(4patients, 21%)vssufentanilgroup(nopatient),p=0.042.
Onepatientinsufentanilgroupdiedonthefifth postop-erativedaybecauseofacomputedtomographydocumented strokethatoccurredonthethirdpostoperativeday.
Discussion
The main result of this study is that patients in sufen-tanilgroup had more hemodynamic stabilityas suggested byreducedinotropicsupportandfewadjustmentsin intra-venousopioiddoses.
Ourstudy alsoconfirms that neuraxial techniques pro-duce effective analgesia in patients undergoing cardiac surgeryasdemonstratedbyareducedconsumptionof intra-venousremifentanilinpatientsofsufentanilgroup.
Onthe contrary,nodifferencewasnoted in inflamma-tory markers (IL6 and TNF␣) and in cardiac biomarkers
(cTnIandBNP).Theirreleasepattern(cTnI,IL6andTNF␣)
along time was the same as observed by Meng et al.,10
confirming thatin bothgroups inflammatory responsedue to elevation in IL6 and TNF␣ was not attenuated and,
no cardiac protection due to reduction in cTnI and BNP occurred.
Table2 Drugsusedintheintra-operativeperiod.Dataarepresentedasnumber(percentages)ormean±standarddeviation.
Controlgroup
n=19
Sufentanilgroup
n=21
p
Vasoactivedrugs
Dopamine 11(58%) 2(9.5%) 0.001
Phenylephrine 12(63%) 9(43%) 0.2
Sodiumnitroprusside 17(89%) 19(90%) 0.9
Anestheticagents
Sevofluraneincreases 0 3(14%) 0.2
Remifentanilbolus 19(100%) 13(62%) 0.004
Sevoflurane(mL/h) 14±2.4 14±2.5 0.8
Table3 Postoperativedata.Dataareexpressedasnumber(percentage),median±standarddeviationormedian(interquartile range).
Variables Controlgroup
n=19
Sufentanilgroup
n=21
p-Value
Tramadolwithin24h,no.ofpatients 13(68%) 18(86%) 0.3
Bolusofmorphine,numberofboluses perpatient
1.5±1.26 1.2±0.98 0.5
PCAmorphineconsumption24h,mg perpatient
8.0±3.15 7.6±3.25 0.8
Abbreviation:PCA,patientcontrolledanalgesia.
Our study could only be compared to that of Bet-tex and colleagues4 who performed the only randomized
study administering or not intrathecal sufentanil in cardiac surgery, although they added morphine to sufen-tanilintrathecal. Theirpostoperative results showed that combinedsufentanilandmorphineallowedashorter post-operative duration of intubation and adequate analgesia comparedwithastandardintravenoustechnique,which dif-fersfromours,thatshowednodifferenceontheseresults. In a non-randomized study, Swenson and colleagues2
foundthatthecombinationof50gintrathecal sufentanil
and 500g intrathecal morphine in general anesthesiain
patientsundergoingCABGpromotedgreaterintraoperative hemodynamicstabilityandreducedtheintraoperative con-sumptionofintravenousopioids.Inourstudy,althoughwe didnotusemorphine,wenotedthattheuseofintrathecal sufentanil reduced intraoperative consumption of intra-venousopioids.
Hansdottir and colleagues11 performed the first study
aboutplasmaandcerebralspinalfluidpharmacokineticsof sufentanil administeredintrathecal inthoracic surgery. In their experience, they concluded that in patients under-going thoracotomy, administrationof 15g of intrathecal
sufentanilincombinationwithgeneralanesthesiaproduced a more potent analgesic effect with a faster onset of action and a shorter duration compared to equipotent doses of morphine or meperidine. This was attributed to the high lipid solubility of sufentanil when present in the cerebrospinal fluid and to a fast transfer to the plasma. However, the same author showed that the cerebrospinal fluid (CSF) and plasma concentrations of sufentanildidnotreachequilibriumeven10hafterinitial
injection. In fact, 10h after initial injection, the CSF concentrationwasstill10timeshigherthanplasmaticone. This study clarified that the principal analgesic effect of sufentaniladministered insubarachnoid spaceis via local ratherthansystemicabsorption.
Thereareseveralfactorsthatmaydeterminethe occur-rence of pain, including an increase in time required to extubation and the occurrence of adverse events that resultindeteriorationsinventricularfunctionduring post-operative period immediately after cardiac surgery.12,13
Postoperative pain relief following cardiac surgery is dif-ficult tocontrol. In our study,there were nostatistically significantdifferencesbetweengroupswithrespecttototal consumptionofanalgesicsovera24-hperiodafter extuba-tion.Theseresultsdemonstratedthattheproposedscheme ofasinglehighdoseofintrathecal sufentanilwasnot suf-ficienttopromoteadequateanalgesiaovertheinitial24-h periodfollowingremovaloforotrachealcannula.
Hansdottirandcolleagues11 alsoshowedthat,although
sufentanilismorelipophilicandiseliminatedmorequickly from cerebrospinal fluid than other opioids such as mor-phine, when 15g dosesof sufentanilwere injected into
thesubarachnoidspace,theconcentrationofopioidin cere-brospinalfluid remainedat residualconcentrations 15±5 timeshigherthaninplasmaforupto10h(600min) follow-ingtheinjection.Fournierandcolleagues,14inastudywhere
patientsunderwentsurgeryfortotalhipreplacement, con-cluded that a single 7.5g dose of intrathecal sufentanil
was sufficient to reduce pain intensity and maintain the VAS value below 3 for a period of 224±100min. In our study,dosesofintrathecalsufentaniladministeredwereup toseventimeshigherthanthoseproposedbyHansdottirand
Table4 Postoperativecomplications.Dataareexpressedasnumber(percentages).
Variables Control
n=19
Sufentanil
n=21
p-Value
Reoperation 1(5.3%) 0 0.5
Re-intubation 0 1(4.8%) 0.9
MajorArrhythmias 2(11%) 0 0.2
Peri-operativeawareness 0 0
---Nauseaand/orvomiting 5(26%) 1(4.8%) 0.085
Pruritus 0 0
---Death 0 1(4.8%) 0.9
14timeshigherthanthoseproposedbyFournierbutstillhad effectonlyinperioperativeperiodandnotinpostoperative paincontrol.
Increasedneedforpackedcellsincontrolgroupwasan unexpectedfindingandauthorscannotfinda physiopatho-logicalhypothesistojustifyit(itisprobablyaneffectofthe smallsamplesize).
In our institution, we considered inhalation induction for cardiac surgery becauseit is easy toperform evenin adultpatientsandithasbetterhemodynamicstability com-paredto some intravenous agents, asdescribed by other authors.15,16
Thespinaldoseof1g/kg,limitedto100g,isusedin
ourinstitutionbecauseweagreewithauthorsthatconclude themainactionofsufentanilisinthespinalcord,11andso,
dosesrelatedtoweightorheightwouldguaranteegreater CSFdispersioninpatientswithmoreweightorheight, result-inginhigherlevelsofanalgesiaandhencebettercontrolof stimulifromthehighthoracicincision,differentfrom Swen-sonandBettex,2,4thatdescribeasingleintrathecaldoseof
50gofsufentanilforcardiacsurgery.
Limitationsofthestudy
Thestudywasnotblindedtouseofintrathecalsufentanil. Nonetheless,allprotocols included inthe study were fol-lowedrigorously.
Conclusion
The main result of this study is that patients receiving intrathecal sufentanil have more hemodynamic stability whencomparedtothosereceivingastandardtreatment,as suggestedbyreducedinotropicsupport(dopaminesupport at weaningfromCPB andduring the perioperative period tomaintainhemodynamicvalues) andfewadjustments in intravenousopioiddoses.
Funding
This work was supported by Dante Pazzanese Institute of CardiologyandFederalUniversityofSãoPaulo(UNIFESP).
Conflicts
of
interest
Theauthorshavenoconflictsofinteresttodeclare.
References
1.ChaneyMA.Intrathecalandepiduralanesthesiaandanalgesia forcardiacsurgery.AnesthAnalg.2006;102:45---64.
2.SwensonJD,HullanderRM,WinglerK,LeiversD.Early extuba-tionaftercardiacsurgeryusingcombinedintrathecalsufentanil andmorphine.JCardiothoracVascAnesth.1994;8:509---14.
3.ChaneyMA.Intrathecalandepiduralanesthesiaandanalgesia forcardiacsurgery.AnesthAnalg.1997;84:1211---21.
4.Bettex DA,SchmidlinD, ChassotPG, SchmidER. Intrathecal sufentanil-morphine shortens theduration ofintubation and improvesanalgesiainfast-trackcardiacsurgery.CanJAnaesth. 2002;49:711---7.
5.KowalewskiRJ,MacAdamsC,FroelichJ.Anesthesiafor coro-nary artery bypass surgery supplementedwith subarachnoid bupivacaineandmorphine:areportof18cases.CanJAnesth. 1994;41:1189---95.
6.CantoPM.Regionalanesthesiainheartsurgery.Expectationor reality?RevEspAnestesiolReanim.2003;50:319---25.
7.VicentyC,MaloneB,MathruM.Comparisonofintrathecaland intravenousmorphineinpostcoronaybypasssurgery.CritCare Med.1985;13:308.
8.Deshpande CM, Mohite SN, Kamdi P. Sufentanil vs fen-tanil for fast track cardiac anesthesia. Indian J Anaesth. 2009;53:455---62.
9.HorlockerTT,WedelDJ,BenzonH,etal.Regionalanesthesiain theanticoagulatedpatient:definingtherisks(thesecondASRA ConsensusConferenceonNeuraxialAnesthesiaand Anticoagu-lation).RegAnesthPainMed.2003;28:172---97.
10.MengQH,ZhuS,SohnN,et al.Releaseofcardiac biochemi-calandinflammatorymarkersinpatientsoncardiopulmonary bypassundergoingcoronaryarterybypassgrafting.JCardSurg. 2008;23:681---7.
11.HansdottirV,HednerT,WoestenborghsR,NordbergG.TheCSF and plasma pharmacokinetics of sufentanil after intrathecal administration.Anesthesiology.1991;74:264---9.
12.HawkesCA,DhileepanS,FoxcroftD.Earlyextubationforadult cardiacsurgical patients.CochraneDatabase SystRev.2003. CD003587.
13.ChengDC,KarskiJ,PenistonC,etal.Morbidityoutcomeinearly versusconventionaltrachealextubationaftercoronaryartery bypassgrafting: aprospective randomizedcontrolledtrial.J ThoracCardiovascSurg.1996;112:755---64.
14.FournierR,WeberA,GamulinZ.Intrathecalsufentanilismore potentthanintravenousforpostoperativeanalgesiaafter total-hipreplacement.RegAnesthPainMed.2005;30:249---54.
15.HallJE,EbertTJ,HarmerM.Inductioncharacteristicswith3% and8%sevofluraneinadults:anevaluationofthesecondstage ofanaesthesiaanditshaemodynamicconsequences. Anaesthe-sia.2000;55:545---50.