SAGE Open
July-September 2016: 1 –12 © The Author(s) 2016 DOI: 10.1177/2158244016669547 sgo.sagepub.com
Creative Commons CC-BY: This article is distributed under the terms of the Creative Commons Attribution 3.0 License (http://www.creativecommons.org/licenses/by/3.0/) which permits any use, reproduction and distribution of
the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
Article
Introduction
It is well known that individuals living with chronic illness are at increased risk for psychological distress and mental health problems, which negatively affect the overall health of these individuals, as well as their capacity to function in everyday life (Kessler, Ormel, Demler, & Stang, 2003; Naylor et al., 2012; Vogeli et al., 2007). Specifically, chronic illnesses such as heart disease and diabetes constitute signifi-cant risk predisposing individuals to mental health problems that can negatively affect their work, socioeconomic status, social support, capacity for self-management, and adaptation to other illnesses (Brands et al., 2007; Dewa, Lin, Kooehoorn, & Goldner, 2007; Egede & Ellis, 2010; Livneh, Lott, & Antonak, 2004; Munir et al., 2007). It has also been docu-mented that as the severity of physical illness increases, so
will concurrent mental illness (Sederer, Silver, McVeigh, & Levy, 2006). Furthermore, untreated psychological distress and mental health problems frequently follow a chronic course (Chapman, Perry, & Strine, 2005; Monroe, Slavich, Torres, & Gotlib, 2007), resulting in a tremendous level of burden for the individual, family, community, and health care system (Drake, Bond, Thornicroft, Knapp, & Goldman, 2012). Despite this high degree of need, there is evidence to
1
Ryerson University, Toronto, Ontario, Canada
2
St. Michael’s Hospital, Toronto, Ontario, Canada
Corresponding Author:
Elizabeth McCay, Professor, Daphne Cockwell School of Nursing, Ryerson University, 350 Victoria Street, 4th Floor Reception, Toronto, Ontario, Canada M5B 2K3.
Email: bmccay@ryerson.ca
Evaluation of Mindfulness-Based Cognitive
Therapy to Reduce Psychological Distress
and to Promote Well-Being: A Pilot Study
in a Primary Health Care Setting
Elizabeth McCay
1, Rachael Frankford
2, Heather Beanlands
1,
Souraya Sidani
1, Enza Gucciardi
1, Rebecca Blidner
2, Audrey
Danaher
1, Celina Carter
1, and Andria Aiello
1Abstract
The objective of this study was to assess the effectiveness of an 8-week mindfulness-based cognitive therapy (MBCT) group intervention to reduce psychological distress as well as to strengthen self-esteem, resilience, and general well-being for individuals living with a chronic illness and/or other health challenges. This pilot study employed a pre–posttest design to evaluate the outcome of the intervention for individuals receiving care in a Community and Family Medicine department and a Women’s Health Centre located in an urban downtown hospital. A total of 42 patients were enrolled in the study and 35 participants completed the intervention. Thirty-five of 42 enrolled participants completed the intervention. Twenty-eight participants completed the pretest and posttest assessments, which demonstrated statistically significant improvement on most outcome measures, including the Center for Epidemiological Studies–Depression Rating Scale (CES-D), Depression Anxiety Stress Scale (DASS), Affect Balance Scale (ABS), the Resilience Scale (RS), and the Five-Item World Health Organization Well-Being Index (WHO-5). Large effect sizes were observed for the CES-D, the ABS, and the DASS Stress subscale. Observed improvements were sustained at 4 weeks posttreatment. Results are consistent with studies indicating that MBCT offers promise in alleviating psychological distress for those who are seeking care in primary health care settings. Continued focus on how to best implement MBCT in primary health care, particularly for those with comorbid physical and mental health conditions, supports the World Health Organization’s recommendation to integrate evidence-based mental health care within primary health care to promote equitable access to care for those most in need.
Keywords
suggest that access to quality care is limited; with the institu-tional and professional separation of mental and physical health care resulting in fragmented approaches to care (Naylor et al., 2012; Vasiliadis, Tempier, Lesage, & Kates, 2009; Vogeli et al., 2007).
Overall, there is an aversion to seeking mental health care (Gaynor & Brown, 2013), regardless of whether these mental health concerns are in the context of chronic physical illness (Roberge, Fournier, Duhoux, Nguyen, & Smolders, 2011). Moreover, globally, two thirds of adults are not receiving effective mental health care services (Chisholm et al., 2007; Ngui, Khasakhala, Ndetei, & Roberts, 2010). To increase access to quality mental health care for vulnerable groups, the World Health Organization (WHO, World Organization of National Colleges, Academies, & Academic Associations of General Practitioners/Family Physicians, 2008) identified the integration of evidence-based mental health care into pri-mary health care as one of the most effective approaches. Primary care settings provide care where people live and work, and thus support a population-based approach to care that is accessible (Naylor et al., 2012) and less stigmatizing (Zeiss & Karlin, 2008). Evidence-based mental health inter-ventions are ideally suited to primary care environments as they are less intensive and can address the health concerns of individuals with physical and/or chronic illness, as well as mental health challenges (Cape, Whittington, Buszewicz, Wallace, & Underwood, 2010; Cully et al., 2010; Jané-Llopis, Barry, Hosman, & Patel, 2005; Zaretsky, Segal, & Fefergrad, 2007).
One major barrier to the effective integration of dence-based strategies in primary care is the lack of evi-dence regarding effective interventions to prevent and reduce psychological distress in the context of chronic ill-ness (de Lusignan, Chan, Parry, Dent-Brown, & Kendrick, 2011; Spurgeon, Hicks, Barwell, Walton, & Spurgeon, 2005; Taylor et al., 2007). To date, public health strategies to address mental health problems are directed primarily toward the detection, diagnosis, and medical treatment of depression (Gilbody, Whitty, Grimshaw, & Thomas, 2003; Stewart, 2008; van Weel, van Weel-Baumgarten, & van Rijswijk, 2009). Evidence indicates that best practice for depression is the combination of medication and psycho-logical interventions (Parikh et al., 2009); however, evi-dence-based psychological treatments, such as cognitive therapy or mindfulness-based approaches, are not readily available in primary care (Naylor et al., 2012; Patten & Juby, 2008; Shafran et al., 2009). As such, current policy is focused on how best to support the integration of evidence-based approaches within primary care settings, as exempli-fied by the United Kingdom’s commitment to expand access to psychological therapies, known as “talking therapies” (Department of Health, 2011) among the general popula-tion. Furthermore, Canada’s Mental Health Strategy advo-cates for increased access to psychological therapies, as well
as increased integration of mental health services within primary care (Mental Health Commission of Canada, 2012).
Mindfulness-Based Cognitive Therapy (MBCT; Segal, Williams, & Teasdale, 2012) is an empirically supported mental health intervention that is administered in a group format and teaches individuals to disengage from repetitive patterns of negative thinking by shifting perspective from mindless cognitive processing to a more engaged mindful processing of experience (Segal et al., 2012). MBCT extends mindfulness-based stress reduction (MBSR; Kabat-Zinn, 1991) by combining mindfulness-based strategies with ele-ments of cognitive therapy. A review of research findings demonstrates that MBCT is highly effective in preventing relapse for individuals who have experienced three or more episodes of depression (Ma & Teasdale, 2004; Teasdale et al., 2000). A recent meta-analysis of randomized con-trolled trials (RCTs) concerning the effectiveness of mindful-ness-based interventions, namely, MBCT and MBSR, extended these findings and found that MBCT is particularly beneficial for people with a depressive disorder who are cur-rently experiencing symptoms (Strauss, Cavanagh, Oliver, & Pettman, 2014).
Indeed, studies employing mindfulness-based interven-tions, specifically MBCT and MBSR, for patient adjustment to chronic illness have shown promising results. However, given the emphasis in MBCT on developing skills to cope with the negative thinking patterns frequently associated with a wide range of long-term health challenges and con-cerns, it may be that MBCT has a particular advantage in alleviating psychological distress experienced by individuals seeking care in primary care settings. To the best of our knowledge, few studies have been undertaken that evaluate the effectiveness of MBCT for individuals with long-term illness and health concerns, implemented by frontline clini-cians in primary care settings. In two exploratory studies where MBCT was evaluated in primary care settings (Finucane & Mercer, 2006; Radford et al., 2012), MBCT was offered to participants who were either experiencing elevated depression and/or anxiety, or were vulnerable to increased depression and/or anxiety. Results of these preliminary stud-ies suggest that MBCT may be effective in addressing depression and anxiety in primary care settings; however, these studies do not indicate whether participants were also experiencing additional health challenges, such as chronic illness and/or other stressful life events. A randomized con-trolled clinical trial by Wong et al. (2011; Wong et al., 2016) supported the effect of MBCT on generalized anxiety disor-der among Chinese community patients in Hong Kong. While the participants were recruited by referral from doc-tors who worked in an Outpatient Clinic and a website avail-able to the general public, it is unclear where the intervention took place and whether MBCT was in fact implemented within a primary care setting. Furthermore, three instructors with experience in either MBSR or MBCT led the MBCT groups; however, it is uncertain whether these instructors were connected to existing primary care teams. The same limitation is true for the study by van Ravesteijn et al. (2013), which reported on findings of an RCT to assess the cost-effectiveness of MBCT for a heterogeneous group of patients with medically unexplained symptoms. These patients belonged to the 10% most frequently attending patients of the participating general practitioners. While MBCT was on average shown to be more effective than enhanced usual care, the MBCT trainers were not integrated into the existing care team. As is evident from this review of the literature, the majority of MBCT studies do not address the generalizability of MBCT to real world primary care settings (Kuyken et al., 2010; Lilja, Broberg, Norlander, & Broberg, 2015).
As such, the purpose of this pilot study was to evaluate the effectiveness of MBCT, implemented by frontline clinicians within primary care, to improve psychological well-being for individuals living with persistent illness and/or other health challenges (e.g., life stressors). It was hypothesized that par-ticipation in the MBCT intervention would reduce psycho-logical distress, specifically depression and anxiety, as well as strengthen self-esteem, resilience, and general well-being for individuals living with a chronic illness and/or other
health challenges. The ultimate purpose was to provide pilot data to support larger well controlled studies to increase access to effective primary mental health care services.
Method
This study employed a pre–posttest design. The study mea-sures were administered to all participants at baseline, imme-diately after the completion of the intervention, and at a 4-week follow-up.
Participants
A total of 42 patients were recruited from the Department of Community and Family Medicine and from the Women’s Health Care Centre at an urban downtown hospital. To be eligible, participants identified that they were experiencing elevated levels of psychological distress related to a chronic illness and/or other health challenges for 2 years or less. In addition, participants were older than 18 years of age, under the care of a physician, as well as able to speak and under-stand English and provide informed consent. Eligible partici-pants were invited to participate in the study by their primary care physician at each clinic. Forty-two participants agreed to participate in the study. Thirty-five of the 42 participants completed the intervention with seven participants dropping out. Individuals reported a number of reasons for dropping out including scheduling conflicts and challenges engaging in MBCT. Of the 35 participants who completed the inter-vention, 28 completed both the pretest and posttest question-naires. A total of 20 participants completed the questionnaires at all three time points: pretest, posttest, and at a 4-week follow-up. Although 35 out of 42 participants completed the MBCT intervention, a number of participants were unable to complete the follow-up questionnaires at posttest (7) and at the 4-week follow-up (8), due to time demands.
Table 1 provides the demographic characteristics for those participants who completed the intervention (N = 35). Participants ranged in age between 23 and 71 years with a mean age of 43.74. The majority of participants (68.6%) were female. Most participants reported being single (40%) or married (31.4%). At the start of the intervention, five of the 35 participants were attending school (14.3%), and approximately half of the sample was employed (48.6%). The majority of participants did not have any children (74.3%), and 35% of the sample were born outside of Canada (e.g., Africa, China, India, Europe). Most of the participants spoke English at home (77.1%).
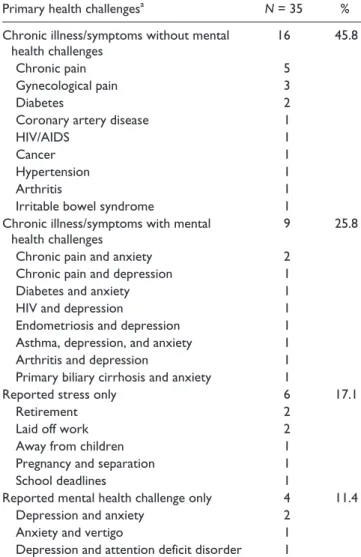
Table 2. Indicating Primary Health Challenges and Stressors of
Participants (N = 35).
Primary health challengesa N = 35 %
Chronic illness/symptoms without mental health challenges
16 45.8
Chronic pain 5
Gynecological pain 3
Diabetes 2
Coronary artery disease 1
HIV/AIDS 1
Cancer 1
Hypertension 1
Arthritis 1
Irritable bowel syndrome 1
Chronic illness/symptoms with mental health challenges
9 25.8
Chronic pain and anxiety 2
Chronic pain and depression 1
Diabetes and anxiety 1
HIV and depression 1
Endometriosis and depression 1
Asthma, depression, and anxiety 1
Arthritis and depression 1
Primary biliary cirrhosis and anxiety 1
Reported stress only 6 17.1
Retirement 2
Laid off work 2
Away from children 1
Pregnancy and separation 1
School deadlines 1
Reported mental health challenge only 4 11.4
Depression and anxiety 2
Anxiety and vertigo 1
Depression and attention deficit disorder 1
a
The primary health challenges are identified; participants identified multiple health challenges and stressors.
in Table 2. A number of participants (n = 9) experienced men-tal health challenges such as anxiety and depression in con-junction with chronic illness or symptoms although all participants identified elevated psychological distress, which was an inclusion criteria for the study. Furthermore, a small number of participants (n = 4) identified a mental health chal-lenge such as anxiety, depression, or attention deficit disorder as their primary symptom. As well, some participants (n = 6)
identified coping with stressors, such as being laid off work, retirement, and coping with pregnancy under trying circum-stances as their primary health challenge. In addition, all par-ticipants, with the exception of one, identified a range of life stressors such as unemployment, retirement, financial issues, or family challenges such as divorce, or stress pertaining to children, in conjunction with the primary health challenges identified.
Procedure
As identified above, participants were recruited from the Department of Community and Family Medicine Program and from the Women’s Health Care Centre at a downtown urban hospital in Toronto. Prior to conducting the study, ics approval was obtained from the appropriate research eth-ics boards. Two social workers met with each participant to explain MBCT and the expectations of involvement in the
Table 1. Demographic Characteristics of Study Participants
(N = 35).
Sample characteristics M SD
Age (years) 43.74 14.36
Length of education (years) 17.78 4.52
Length of time in Canada (years) 32.42 17.16
n %
Gender
Male 10 28.6
Female 24 68.6
Transgendered (male to female) 1 2.9
School (current)
Yes 5 14.3
No 30 85.7
Employment (1 participant missing)
Yes 17 48.6
No 17 48.6
Marital status
Single 14 40.0
Married 11 31.4
Common law 2 5.7
Divorced 5 14.3
Separated 2 5.7
Widowed 1 2.9
Sexual orientation (6 participants missing)
Straight 22 62.9
Gay 5 14.3
Bisexual 2 5.7
Living situation
Alone 13 37.1
Spouse, partner, significant other 12 34.3
Partner and children 2 5.7
Parents 2 5.7
Friends 1 2.9
Other 5 14.3
Children (1 missing participant)
Yes 8 22.9
No 26 74.3
Place of birth (1 missing participant)
Canada 22 64.7
The United States 1 2.9
Other 11 32.4
Language spoken at home
English 27 77.1
intervention. Prior to the start of the study, informed consent was obtained from the study participants. The intervention was conducted by two social workers employed within the Department of Family and Community Medicine and at the Woman’s Health Care Centre who possess a depth of knowl-edge and clinical experience in mindfulness and cognitive-behavioral strategies, including personal experience with meditation. The intervention was conducted in a local com-munity setting affiliated with a downtown Toronto hospital.
Measures
The study questionnaires were selected in accordance with the study purpose and hypothesis to assess mental health challenges and strengths for the participants, and have sound psychometric properties. Relevant sociodemographic char-acteristics were included to provide a comprehensive description of the sample.
Affect Balance Scale (ABS). The ABS is a 10-item scale that contains five statements reflecting positive feelings and five statements reflecting negative feelings (Bradburn, 1969). The focus of the scale is on overall psychological well-being with responses of “yes” or “no” to each question. The indi-vidual is asked to focus on his or her feelings during the past week. This scale has strong test–retest reliability and high levels of internal consistency (Schiaffino, 2003). A higher score on this scale represents an overall positive mood state. A constant of 15 was added to the ABS scores to yield a dis-tribution of positive numbers.
Center for Epidemiological Studies–Depression Scale (CES-D). The CES-D scale is 20-item measure of psychological distress and depression that has been used in studies with young people and adults. Excellent levels of internal consis-tency have been reported, as well as concurrent and construct validity (Radloff, 1977). A higher score on the CES-D scale indicates a greater degree of depression.
Depression Anxiety Stress Scale (DASS). The DASS is a 42-item self-report instrument that is used to measure an individual’s depression, anxiety, and stress within the past week (Antony, Bieling, Cox, Enns, & Swinson, 1998). The DASS has dem-onstrated strong internal consistency, as well as robust con-vergent and discriminant validity in large clinical samples (Brown, Chorpita, Korotitsch, & Barlow, 1997). Higher scores on each subscale indicate greater distress.
Rosenberg Self-Esteem Scale (RSES). The RSES (Rosenberg, 1979) is a well-validated 10-item self-report inventory developed to measure global self-worth. The RSES has been shown to have high levels of internal consistency as well as convergent and discriminant validity (Sinclair et al., 2010). A higher score on the RSES signals a higher level of self-esteem.
The Resilience Scale (RS). The RS (Wagnild & Young, 1993) is a 25-item self-report scale with a 7-point Likert-type response format. Resilience is a positive characteristic that enhances individual adaptation and is conceptualized as comprising personal competence and acceptance of self and life. Reliability and concurrent validity have been demon-strated with adults (Wagnild & Young, 1993), as well as for homeless adolescents (Rew, Taylor-Seehafer, Thomas, & Yockey, 2001).
Five-Item World Health Organization Well-Being Index (WHO-5; 1998 version). The WHO-5, 1998 version, is a five-item questionnaire using a 6-point rating scale from 0 to 5, where individuals are asked to select a response based on how they have been feeling in the past 2 weeks. Five indicates the highest level of well-being and 0 indicates the lowest level of well-being. The five items are based on how the individual feels, specifically; relaxed, cheerful, fresh, rested, and spend-ing time dospend-ing thspend-ings that interest him or her (WHO, 1998). This measure of well-being has been shown to have high lev-els of internal and external validity, and concurrent validity in a range of populations, including the older adult popula-tion with depression (Heun, Bonsignore, Barkow, & Jessen, 2001) and adolescents diagnosed with diabetes (De Wit, Pouwer, Gemke, Delemarre-van de Waal, & Snoek, 2007). Scores are transformed to a scale of 0 to 100 by multiplying by 4, with higher scores indicating a greater feeling of well-being.
Demographic characteristics. Participants reported their age, gender, years of education, school attendance, employment status, marital status, sexual orientation, living arrangements, number of children (if any), place of birth, parents’ place of birth, length of time in Canada, language spoken at home, primary health challenges, current stressors, and reasons for attending the group. This information was collected by a self-report questionnaire devised for this study.
Intervention
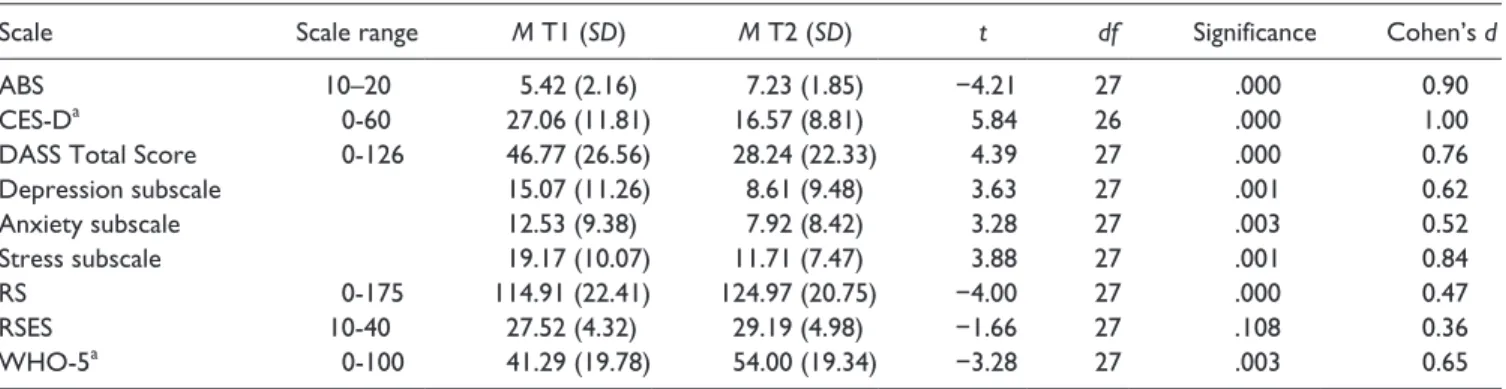
Table 3. Paired-Sample t Tests for Participants Pretest (T1) and Posttest (T2; n = 28).
Scale Scale range M T1 (SD) M T2 (SD) t df Significance Cohen’s d
ABS 10–20 5.42 (2.16) 7.23 (1.85) −4.21 27 .000 0.90
CES-Da 0-60 27.06 (11.81) 16.57 (8.81) 5.84 26 .000 1.00
DASS Total Score 0-126 46.77 (26.56) 28.24 (22.33) 4.39 27 .000 0.76
Depression subscale 15.07 (11.26) 8.61 (9.48) 3.63 27 .001 0.62
Anxiety subscale 12.53 (9.38) 7.92 (8.42) 3.28 27 .003 0.52
Stress subscale 19.17 (10.07) 11.71 (7.47) 3.88 27 .001 0.84
RS 0-175 114.91 (22.41) 124.97 (20.75) −4.00 27 .000 0.47
RSES 10-40 27.52 (4.32) 29.19 (4.98) −1.66 27 .108 0.36
WHO-5a 0-100 41.29 (19.78) 54.00 (19.34) −3.28 27 .003 0.65
Note. ABS = Affect Balance Scale; CES-D = Center for Epidemiological Studies–Depression Scale; DASS = Depression, Anxiety and Stress Scale; RS = Resilience Scale; RSES = Rosenberg Self-Esteem Scale; WHO-5 = Five-Item World Health Organization Well-Being Index.
a
Missing one participant. *p < .006.
was no emphasis on providing education about depression and preventing relapse/recurrence, particularly in Session 7. Furthermore, there was more attention to promoting cogni-tive and psychological insights around illness experiences and challenges in particular, and to developing skills to cope with these, specifically skills that recognize negative think-ing patterns, especially in Weeks 2, 3, 4, and 5.
As stated above, the structured 8-week group intervention was conducted by two social workers (employed in the iden-tified study settings) who possessed a depth of knowledge and clinical experience in mindfulness and cognitive-behav-ioral strategies, including personal experience with medita-tion. Each session was 120 min, and included formal and informal mindfulness practices, as well as teaching cogni-tive-behavioral skills. Participants were assigned homework and were expected to do a formal meditation practice for 30 to 45 min a day, 6 days a week. They were also given read-ings and worksheets to complete and discuss in the following sessions.
The first session of the intervention introduced the partici-pants to mindfulness, and included the raisin exercise and body scan. These are two different methods of building awareness of the present moment. The raisin exercise requires individuals to mindfully hold, examine, feel, smell, and taste a raisin. The body scan requires individuals to lie or sit still while slowly bringing awareness and relaxation to each body part at a time. The second session consisted of awareness of breath and an introduction to CBT, including dealing with barriers to practice. The pleasant events calen-dar was introduced for homework. The third session involved a mindful seeing exercise, breath and body meditation, and the CBT concepts of mind traps, wise mind, and automatic thoughts. In the fourth session, participants were introduced to the meditation of sound and a CBT exercise recognizing mind traps was introduced. The fifth session included walk-ing meditation and the 3-min breathwalk-ing space. The sixth week was devoted to a 3-hr retreat session followed by a half hour discussion. Loving kindness practice intended to
strengthen an attitude of compassion was discussed, with the majority of time used for silence in meditation. Participants were also asked to complete the stressful communication calendar. The seventh session was devoted to the concept of being mindful with others, and included choice-less aware-ness (i.e., perceiving things as they really are) and walking practice. The eighth and final session consisted of a review of the group, including intentions for ongoing practice. A list of community resources to support continued mindfulness practice was offered to all participants.
Data Analysis
The data were analyzed with the SPSS for Windows, Version 20. The sample frequencies, means, and standard deviations were calculated. To compare characteristics and baseline study variables between those who completed the interven-tion and those who dropped out, independent t tests for con-tinuous data and chi-square (χ2) tests for categorical data were conducted. Paired-sample t tests were calculated on the study measures to assess the degree of change between base-line and posttest for those participants who completed the pretest and posttest questionnaires. Paired-sample t tests were also calculated on the study measures to assess the degree of change from posttest assessment to the 4-week follow-up assessment. To correct for the use of multiple paired-sample t tests, the Bonferroni correction formula was calculated and indicated a significance value of p = .006 or below.
Results
Participants who completed the intervention and the posttest assessment demonstrated a significant improvement in scores on the ABS, t(27) = −4.21, p = .000; CES-D, t(26) = 5.84, p = .000; DASS, t(27) = 4.39, p = .000; RS, t(27) = −4.00, p = .000; and WHO-Five, t(27) = −3.28, p = .003. The scores obtained on the DASS subscales also demonstrated significant improvement in participants’ levels of depres-sion, stress, and anxiety (see Table 3). Cohen’s d statistic was computed for all of the study variables (see Table 3) and yielded a large effect size on the ABS (0.90), CES-D (1.00), and DASS Stress subscale (0.84). In addition, a medium effect size was obtained for the DASS Total Score (0.76), DASS Depression subscale (0.62), DASS Anxiety subscale (0.52), and the WHO-Five (0.65). As well, a medium effect size was obtained for the RS (0.47) and a small effect size for the RSES (0.36).
For Cohen’s d values: d = 0.2 to 0.5, small effect; d = 0.5 to 0.8, medium effect; and d = 0.8 to 1.0, large effect.
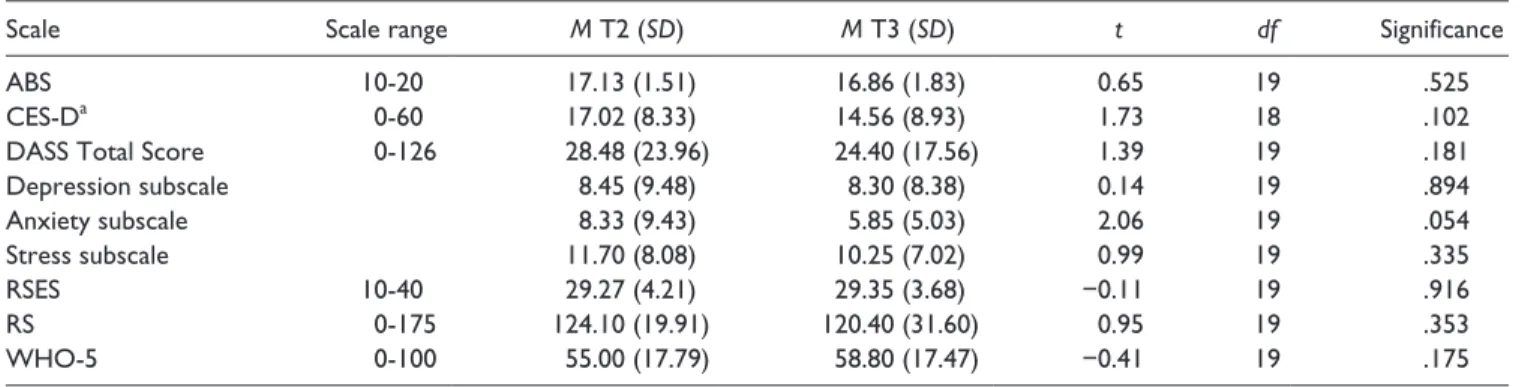
Table 4 describes the results of the paired-sample t tests for study measures at posttest and at a 4-week follow-up for participants who completed the intervention and the ques-tionnaires at all three time points: baseline, immediately pos-tintervention, and at a 4-week follow-up. No significant differences were observed between participant scores imme-diately postintervention and at the 4-week follow-up, indi-cating that observed improvements were sustained at 4 weeks posttreatment. The improvement observed on the anxiety subscale of the DASS was not considered significant as the significance level for the study was set at p = .006 or below, based on the Bonferroni correction.
Discussion
The findings from this pilot study suggest that MBCT is a promising intervention for individuals seeking treatment in primary health care settings who are experiencing elevated levels of psychological distress in the context of chronic ill-ness and/or other stressful health-related challenges. As
hypothesized, participants experienced significantly decreased levels of depression, anxiety, and stress, as well as significantly increased levels of resilience and well-being following the completion of the 8-week MBCT intervention. The overall effect size for depression, positive mood states, and stress was large, and is comparable with previous studies that have also documented large effect sizes for depression following MBCT (Hofmann et al., 2010; Kenny & Williams, 2007). These gains were also sustained 1 month following completion of the study intervention. The sustained improve-ment may be related to continued practice of MBCT skills that were acquired over the 8-week intervention although the degree to which individuals engaged in MBCT practice fol-lowing the intervention is unknown.
It is noteworthy that scores for depression and anxiety in the current study population were high and comparable with those reported in the literature for other chronic illness popu-lations, such as HIV/AIDS (Plach, Stevens, & Heidrich, 2006), chronic pain (R. Taylor, Lovibond, Nicholas, Cayley, & Wilson, 2005), multiple sclerosis (Chwastiak et al., 2002), diabetes (Glasgow, Boles, Mckay, Feil, & Barrera, 2003; Wagner et al., 2001), as well as irritable bowel syndrome (Nickel et al., 2010), underlining the similarities between the current sample and other normative studies. Taken together, these results convey a high level of mental health need among individuals with chronic illness and other health challenges.
Specifically, all participants in the present study experi-enced psychological distress and many experiexperi-enced symp-toms of depression and anxiety in the context of chronic illness and physical symptoms. It is well known that comor-bid anxiety and depression in the context of chronic illness greatly increases the likelihood that individuals will experi-ence increased medical symptoms, such as increased pain, angina, dyspnea, as well as poor self-care (Katon, Lin, & Kroenke, 2007). Furthermore, comorbid mental health prob-lems, including psychological distress, constitute significant risk factors that can negatively affect the capacity for work,
Table 4. Paired-Sample t Tests for Participants Posttest (T2) and Follow-Up (T3; n = 20).
Scale Scale range M T2 (SD) M T3 (SD) t df Significance
ABS 10-20 17.13 (1.51) 16.86 (1.83) 0.65 19 .525
CES-Da 0-60 17.02 (8.33) 14.56 (8.93) 1.73 18 .102
DASS Total Score 0-126 28.48 (23.96) 24.40 (17.56) 1.39 19 .181
Depression subscale 8.45 (9.48) 8.30 (8.38) 0.14 19 .894
Anxiety subscale 8.33 (9.43) 5.85 (5.03) 2.06 19 .054
Stress subscale 11.70 (8.08) 10.25 (7.02) 0.99 19 .335
RSES 10-40 29.27 (4.21) 29.35 (3.68) −0.11 19 .916
RS 0-175 124.10 (19.91) 120.40 (31.60) 0.95 19 .353
WHO-5 0-100 55.00 (17.79) 58.80 (17.47) −0.41 19 .175
Note. ABS = Affect Balance Scale; CES-D = Center for Epidemiological Studies–Depression Scale; DASS = Depression, Anxiety, and Stress Scale; RSES = Rosenberg Self-Esteem Scale; RS = Resilience Scale; WHO-5 = Five-Item World Health Organization Well-Being Index.
a
socioeconomic status, and social support; dramatically affecting overall quality of life (Brands et al., 2007; Egede & Ellis, 2010; Livneh et al., 2004; Munir et al., 2007) and fur-ther emphasizing the profound need for early mental health intervention in primary care.
The results of this study add to the emerging body of evi-dence that suggests that MBCT is likely an effective low intensity mental health intervention that can be adopted in primary health care settings. This is one of very few studies that have evaluated MBCT with individuals who experi-enced psychological distress in the context of chronic illness, physical symptoms, and life stressors, implemented by pri-mary care frontline clinicians within a pripri-mary health care setting. Although there is a scarcity of studies undertaken in primary care, the current findings align with two studies that have previously evaluated MBCT in primary care settings (Finucane & Mercer, 2006; Radford et al., 2012). It is impor-tant to note that these two studies evaluated MBCT in pri-mary care where individuals were living with recurrent depression and anxiety in the absence of comorbid chronic illness (Finucane & Mercer, 2006; Radford et al., 2012), unlike the current study where the majority of individuals were living with comorbid medical conditions, as well as psychological distress and stressful life circumstances. These studies also demonstrated an improvement in anxiety and depressive symptoms.
The application of MBCT to a range of clinical popula-tions in primary care settings is a logical extension of MBCT. MBCT was developed to address the chronic and relapsing nature of depression over time and specifically to prevent recurrence. The theoretical orientation of MBCT takes into account the capacity to recognize and disengage from sive and ruminative thought patterns, which underlie depres-sion and psychological distress, through engaging in mindfulness, an approach that has been found to effectively prevent the recurrence of depressive episodes (Chiesa & Serretti, 2011; Segal et al., 2012). Psychological distress and depression are commonly experienced by many living with chronic medical conditions and across a broad spectrum of challenging health problems. As such, implementing MBCT in primary care promises to offer ready access to treatment that has the potential to prevent the chronic and disabling course of depression and distress in these populations.
Current health care policy emphasizes the need to reorient health care toward prevention rather than waiting to intervene in periods of acute illness. Furthermore, it is well recognized that approaches directed toward building competence, self-responsibility, and positive behavioral change are highly bene-ficial to at-risk individuals, helping them to take control of their overall health to better manage their lives (Khanlou, 2003; McCabe Ruff & Mackenzie, 2009; WHO, World Organization of National Colleges, Academies, & Academic Associations of General Practitioners/Family Physicians, 2008). The findings from this study suggest that MBCT supports the orientation toward competence and self-responsibility, as evidenced by
significantly improved levels of resilience (the internalized sense of capacity to withstand stress and manage challenge; Wagnild & Young, 1993) and well-being following participa-tion in the MBCT intervenparticipa-tion.
The results also underline the broader issue of building capacity among health care providers in delivering psycho-logical interventions, such as MBCT. In this pilot study, the intervention was delivered by two social workers but could be provided by other members of the health care team, such as registered nurses or family physicians, with adequate training and personal commitment to ongoing mindfulness practice. Increasing the number of health care providers who work in primary care and who are trained in MBCT can enhance much-needed access to mental health services in a manner that is acceptable and accessible. Given the limited availability and cost of mental health care in tertiary care set-tings, the integration of MBCT within primary care to treat psychological distress for clients experiencing chronic ill-ness has been identified as an imperative that is both feasible (Naylor et al., 2012; van Ravesteijn et al., 2013) and effec-tive (Radford et al., 2012).
Limitations
This study used a pre–posttest design to evaluate the effec-tivenesss of MBCT in primary care and did not include a control group, and consequently the findings cannot be directly attributed to participation in MBCT. Another limita-tion is the relatively small sample size, which reduces the generalizability of the current study findings. Future research studies evaluating MBCT in primary care would benefit from the addition of a control group and a larger sample, to provide increased confidence regarding the study findings. Further details regarding MBCT practice, such as continued homework, were not explored and would provide additional understanding regarding the mechanisms of change observed in the current study.
Conclusion
promote equitable access to care for those most in need. Given the magnitude and chronicity of mental health problems worldwide (Chapman et al., 2005; Monroe et al., 2007; Roberge et al., 2011), the importance of policy relevant research focusing on scaling up MBCT to other primary health care programs and sectors should not be overlooked. The cur-rent study highlights the potential of MBCT to equip individu-als with a range of skills to manage their distress early in the illness trajectory, thus averting serious mental health problems and contributing to an improved quality of life.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research and/or authorship of this article: The authors grate-fully acknowledge the funding from the Faculty of Community Services, Ryerson University, for this study.
References
Antony, M. M., Bieling, P. J., Cox, B. J., Enns, M. W., & Swinson, R. P. (1998). Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales (DASS) in clinical groups and a community sample. Psychological
Assessment, 10, 176-181.
Bradburn, N. M. (1969). The structure of psychological well-being. Chicago, IL: Aldine.
Brands, A., Van den Berg, E., Manschot, S., Biessels, G., Kappelle, L., DeHaan, E., & Kessels, R. (2007). A detailed profile of cognitive dysfunction and its relation to psychological dis-tress in patients with type 2 diabetes mellitus. Journal of the
International Neuropsychological Society, 13, 288-297.
Brown, T. A., Chorpita, B. F., Korotitsch, W., & Barlow, D. H. (1997). Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behaviour Research
and Therapy, 35, 79-89.
Cape, J., Whittington, C., Buszewicz, M., Wallace, P., & Underwood, L. (2010). Brief psychological therapies for anxi-ety and depression in primary care: Meta-analysis and meta-regression. BMC Medicine, 8(1), Article 38.
Chapman, D. P., Perry, G. S., & Strine, T. W. (2005). The vital link between chronic disease and depressive disorders. Preventing
Chronic Disease, 2(1), 1-10.
Chiesa, A., & Serretti, A. (2011). Mindfulness based cognitive ther-apy for psychiatric disorders: A systematic review and meta-analysis. Psychiatry Research, 187, 441-453.
Chisholm, D., Flisher, A. J., Lund, C., Patel, V., Saxena, S., & Thornicroft, G., . . . Lancet Global Mental Health Group. (2007). Scale up services for mental disorders: A call for action. The Lancet, 370, 1241-1252.
Chwastiak, L., Ehde, D. M., Gibbons, L. E., Sullivan, M., Bowen, J. D., & Kraft, G. H. (2002). Depressive symptoms and sever-ity of illness in multiple sclerosis: Epidemiologic study of a large community sample. American Journal of Psychiatry,
159, 1862-1868.
Crowe, M., Jordan, J., Burrell, B., Jones, V., Gillon, D., & Harris, S. (2016). Mindfulness-based stress reduction for long-term physical conditions: A systematic review. Australian & New
Zealand Journal of Psychiatry, 50, 21-32.
Cully, J. A., Stanley, M. A., Deswal, A., Hanania, N. A., Phillips, L. L., & Kunik, M. E. (2010). Cognitive-behavioral therapy for chronic cardiopulmonary conditions: Preliminary outcomes from an open trial. Primary Care Companion to the Journal of
Clinical Psychiatry, 12(4), 1-6.
de Lusignan, S., Chan, T., Parry, G., Dent-Brown, K., & Kendrick, T. (2012). Referral to a new psychological therapy service is associated with reduced utilisation of healthcare and sickness absence by people with common mental health problems: A before and after comparison. Journal of Epidemiology &
Community Health, 66(6), e10.
Department of Health. (2011). Talking therapies: A four-year plan
of action. London, England: Author.
Dewa, C. S., Lin, E., Kooehoorn, M., & Goldner, E. (2007). Association of chronic work stress, psychiatric disorders, and chronic physical conditions with disability among workers.
Psychiatric Services, 58, 652-658.
De Wit, M., Pouwer, F., Gemke, R. J., Delemarre-van de Waal, H. A., & Snoek, F. J. (2007). Validation of the WHO-5 Well-Being Index in adolescents with type 1 diabetes. Diabetes Care, 30, 2003-2006.
Drake, R. E., Bond, G. R., Thornicroft, G., Knapp, M., & Goldman, H. H. (2012). Mental health disability: An international per-spective. Journal of Disability Policy Studies, 23, 110-120. Egede, L. E., & Ellis, C. (2010). Diabetes and depression: Global
perspectives. Diabetes Research and Clinical Practice, 87, 302-312.
Eisendrath, S., Chartier, M., & McLane, M. (2008). Adapting mind-fulness-based cognitive therapy for treatment-resistant depres-sion. Cognitive and Behavioral Practice, 18, 362-370.
Evans, S., Ferrando, S., Findler, M., Stowell, C., Smart, C., & Haglin, D. (2008). Mindfulness-based cognitive therapy for generalized anxiety disorder. Journal of Anxiety Disorders, 22, 716-721.
Finucane, A., & Mercer, S. W. (2006). An exploratory mixed meth-ods study of the acceptability and effectiveness of mindfulness-based cognitive therapy for patients with active depression and anxiety in primary care. BMC Psychiatry, 6(1), 1-14.
Fitzpatrick, L., Simpson, J., & Smith, A. (2010). A qualitative analysis of mindfulness-based cognitive therapy (MBCT) in Parkinson’s disease. Psychology and Psychotherapy: Theory,
Research and Practice, 83, 179-192.
Foley, E., Baillie, A., Huxter, M., Price, M., & Sinclaire, E. (2010). Mindfulness-based cognitive therapy for individuals whose lives have been affected by cancer: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 78, 72-79. Gaynor, K., & Brown, J. (2013). Self-referrers to community work-shops: Who are they and why do some participants not consult with their GP about their mental health difficulties? Journal of
Mental Health, 22, 227-236.
Glasgow, R. E., Boles, S. M., Mckay, H. G., Feil, E. G., & Barrera, M., Jr. (2003). The D-net diabetes self-management program: Long-term implementation, outcomes, and generalization results.
Preventive Medicine, 36, 410-419.
Gotlink, R. A., Chu, P., Busschback, J. J. V., Benson, H., Fricchione, G. L., & Hunink, M. G. M. (2015). Standardised mindfulness-based interventions in healthcare: An overview of systematic reviews and meta-analyses of RCTs. PLoS ONE,
10(4), e0124344.
Heun, R., Bonsignore, M., Barkow, K., & Jessen, F. (2001). Validity of the five-item WHO Well-Being Index (WHO-5) in an elderly population. European Archives of Psychiatry and
Clinical Neuroscience, 251(2), 27-31.
Hofmann, S. G., Sawyer, A. T., Witt, A. A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical
Psychology, 78, 169-183.
Jané-Llopis, E., Barry, M., Hosman, C., & Patel, V. (2005). Mental health promotion works: A review. Global Health Promotion,
12(2, Suppl.), 9-25.
Kabat-Zinn, D. (1991). Full catastrophe living: Using the wisdom
of your body and mind to face stress, pain, and illness. New
York, NY: Delta Trade Paperbacks.
Katon, W., Lin, E., & Kroenke, K. (2007). The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. General Hospital
Psychiatry, 29, 147-155.
Kenny, M. A., & Williams, J. M. G. (2007). Treatment-resistant depressed patients show a good response to mindfulness-based cognitive therapy. Behaviour Research and Therapy, 45, 617-625. Kessler, R. C., Ormel, J., Demler, O., & Stang, P. E. (2003).
Comorbid mental disorders account for the role impairment of commonly occurring chronic physical disorders: Results from the National Comorbidity Survey. Journal of Occupational
and Environmental Medicine, 45, 1257-1266.
Khanlou, N. N. (2003). Mental health promotion education in mul-ticultural settings. Nursing Education Today, 23, 96-103. Kuyken, W., Byford, S., Byng, R., Dalgleish, T., Lewis, G., Taylor,
R., & Morant, N. (2010). Study protocol for a randomized con-trolled trial comparing mindfulness-based cognitive therapy with maintenance anti-depressant treatment in the prevention of depressive relapse/recurrence: The PREVENT trial. Trials,
11(1), Article 99.
Lilja, J. L., Broberg, M., Norlander, T., & Broberg, A. G. (2015). Mindfulness-Based cognitive therapy: Primary care patients’ experiences of outcomes in everyday life and relapse preven-tion. Psychology, 6, 464-477.
Livneh, H., Lott, S., & Antonak, R. (2004). Patterns of psychosocial adaptation to chronic illness and disability: A cluster analytic approach. Psychology, Health & Medicine, 9, 411-430. Ma, H., & Teasdale, J. (2004). Mindfulness-based cognitive
ther-apy for depression: Replication and exploration of differential relapse prevention effects. Journal of Consulting and Clinical
Psychology, 72, 31-40.
McCabe Ruff, K., & Mackenzie, E. R. (2009). The role of mind-fulness in healthcare reform: A policy paper. Explore: The
Journal of Science and Healing, 5, 313-323.
Mental Health Commission of Canada. (2012). Changing
direc-tions, changing lives: The mental health strategy for Canada.
Calgary, Alberta: Author.
Monroe, S. M., Slavich, G. M., Torres, L. D., & Gotlib, I. H. (2007). Major life events and major chronic difficulties are differen-tially associated with history of major depressive episodes.
Journal of Abnormal Psychology, 116, 116-124.
Munir, F., Yarker, J., Haslam, C., Long, H., Leka, S., Griffiths, A., & Cox, S. (2007). Work factors related to psychological and health-related distress among employees with chronic ill-nesses. Journal of Occupational Rehabilitation, 17, 259-277. Naylor, C., Parsonage, M., McDaid, D., Knapp, M., Fossey, M., &
Galea, A. (2012). Long-term conditions and mental health: The
cost of co-morbidities. London, England: The King’s Fund.
Ngui, E. M., Khasakhala, L., Ndetei, D., & Roberts, L. W. (2010). Mental disorders, health inequalities and ethics: A global per-spective. International Review of Psychiatry, 22, 235-244. Nickel, J. C., Tripp, D. A., Pontari, M., Moldwin, R., Mayer, R.,
Carr, L. K., & Nordling, J. (2010). Interstitial cystitis/pain-ful bladder syndrome and associated medical conditions with an emphasis on irritable bowel syndrome, fibromyalgia and chronic fatigue syndrome. The Journal of Urology, 184, 1358-1363.
Parikh, S. V., Segal, Z. V., Grigoriadis, S., Ravindran, A. V., Kennedy, S. H., Lam, R. W., & Patten, S. B. (2009). Canadian Network for Mood and Anxiety Treatments (CANMAT) clini-cal guidelines for the management of major depressive disor-der in adults. II. Psychotherapy alone or in combination with antidepressant medication. Journal of Affective Disorders, 117, S15-S25.
Parra-Delgado, M., & Latorre-Postigo, J. M. (2013). Effectiveness of mindfulness-based cognitive therapy in the treatment of fibromyalgia: A randomised trial. Cognitive Therapy and
Research, 37, 1015-1026.
Patten, S. B., & Juby, H. (2008). A profile of clinical depression
in Canada. Retrieved from
http://prism.ucalgary.ca/jspui/bit-stream/1880/46327/6/Patten_RSS1.pdf
Philippot, P., Nef, F., Clauw, L., de Romrée, M., & Segal, Z. (2011). A randomized controlled trial of mindfulness-based cognitive therapy for treating tinnitus. Clinical Psychology &
Psychotherapy, 19, 411-419.
Plach, S. K., Stevens, P. E., & Heidrich, S. M. (2006). Social roles and health in women living with HIV/AIDS: A pilot study.
Journal of the Association of Nurses in AIDS Care, 17, 58-64.
Radford, S. R., Crane, S. R., Eames, C., Gold, E., & Owens, W. G. (2012). The feasibility and effectiveness of mindfulness-based cognitive therapy for mixed diagnosis patients in primary care: A pilot study. Mental Health in Family Medicine, 9, 191-200. Radloff, L. S. (1977). The CES-D scale: A self-report
depres-sion scale for research in the general population. Applied
Psychological Measurement, 1, 385-401.
Ree, M., & Craigie, M. A. (2007). Outcomes following mindful-ness-based cognitive therapy in a heterogeneous sample of adult outpatients. Behaviour Change, 24, 70-86.
Rew, L., Taylor-Seehafer, M., Thomas, N. Y., & Yockey, R. D. (2001). Correlates of resilience in homeless adolescents.
Journal of Nursing Scholarship, 33, 33-40.
Roberge, P., Fournier, L., Duhoux, A., Nguyen, C. T., & Smolders, M. (2011). Mental health service use and treatment ade-quacy for anxiety disorders in Canada. Social Psychiatry and
Psychiatric Epidemiology, 46, 321-330.
Schiaffino, K. M. (2003). Other measures of psychological well-being. Arthritis Care & Research, 49(S5), S165-S174.
Sederer, L. I., Silver, L., McVeigh, K. H., & Levy, J. (2006). Integrating care for medical and mental illnesses. Preventing
Chronic Disease, 3(2), 1-3.
Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2012).
Mindfulness-based cognitive therapy for depression. New
York, NY: Guilford Press.
Shafran, R., Clark, D. M., Fairburn, C. G., Arntz, A., Barlow, D. H., Ehlers, A., & Wilson, G. T. (2009). Mind the gap: Improving the dissemination of CBT. Behaviour Research and Therapy,
47, 902-909.
Sharplin, G. R., Jones, S. B., Hancock, B., Knott, V. E., Bowden, J. A., & Whitford, H. S. (2010). Mindfulness-based cognitive therapy: An efficacious community-based group intervention for depression and anxiety in a sample of cancer patients. The
Medical Journal of Australia, 193(5), 79-82.
Sinclair, S. J., Blais, M. A., Gansler, D. A., Sandberg, E., Bistis, K., & LoCicero, A. (2010). Psychometric properties of the Rosenberg Self-Esteem Scale: Overall and across demographic groups living within the United States. Evaluation & the Health
Professions, 33, 56-80.
Spurgeon, P., Hicks, C., Barwell, F., Walton, I., & Spurgeon, T. (2005). Counselling in primary care: A study of the psycho-logical impact and cost benefits for four chronic conditions.
European Journal of Psychotherapy, Counselling & Health, 7,
269-290.
Stange, J. P., Eisner, L. R., Hölzel, B. K., Peckham, A. D., Dougherty, D. D., Rauch, S. L., & Deckersbach, T. (2011). Mindfulness-based cognitive therapy for bipolar disorder: Effects on cogni-tive functioning. Journal of Psychiatric Practice, 17, 410-419. Stewart, D. E. (2008). Battling depression. Canadian Medical
Association Journal, 178, 1023-1024.
Strauss, C., Cavanagh, K., Oliver, A., & Pettman, D. (2014). Mindfulness-based interventions for people diagnosed with a current episode of an anxiety or depressive disorder: A meta-analysis of randomised controlled trials. PLoS ONE, 9(4), e96110.
Taylor, L., Taske, N., Swann, C., Waller, S., Bernett-Page, E., & Seymour, L. (2007). Public health interventions to pro-mote positive mental health and prevent mental health
disor-ders among adults (Resource document). London, England:
National Institute for Health and Clinical Excellence.
Taylor, R., Lovibond, P. F., Nicholas, M. K., Cayley, C., & Wilson, P. H. (2005). The utility of somatic items in the assessment of depression in patients with chronic pain: A comparison of the Zung Self-Rating Depression Scale and the Depression Anxiety Stress Scales in chronic pain and clinical and commu-nity samples. The Clinical Journal of Pain, 21, 91-100. Teasdale, J., Williams, J., Soulsby, J., Segal, Z., Ridgeway, V.,
& Lau, M. (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of
Consulting and Clinical Psychology, 68, 615-623.
van Ravesteijn, H., Grutters, J., olde Hartman, T., Lucassen, P., Bor, H., van Weel, C., & Speckens, A. (2013). Mindfulness-based cognitive therapy for patients with medically unex-plained symptoms: A cost-effectiveness study. Journal of
Psychosomatic Research, 74, 197-205.
van Weel, C., van Weel-Baumgarten, E., & van Rijswijk, E. (2009). Treatment of depression in primary care. British Medical
Journal, 338, Article b934.
Vasiliadis, H. M., Tempier, R., Lesage, A., & Kates, N. (2009). General practice and mental health care: Determinants of outpatient service use. Canadian Journal of Psychiatry, 54, 468-476.
Vogeli, C., Shields, A. E., Lee, T. A., Gibson, T. B., Marder, W. D., Weiss, K. B., & Blumenthal, D. (2007). Multiple chronic conditions: Prevalence, health consequences, and implications for quality, care management, and costs. Journal of General
Internal Medicine, 22, 391-395.
Wagner, E. H., Grothaus, L. C., Sandhu, N., Galvin, M. S., McGregor, M., Artz, K., & Coleman, E. A. (2001). Chronic care clinics for diabetes in primary care: A system-wide ran-domized trial. Diabetes Care, 24, 695-700.
Wagnild, G. M., & Young, H. M. (1993). Development and psycho-metric evaluation of the Resilience Scale. Journal of Nursing
Measurement, 1, 165-178.
Wong, S. Y. S., Mak, W. W., Cheung, E. Y., Ling, C. Y., Lui, W. W., Tang, W. K., & Ma, H. S. (2011). A randomized, con-trolled clinical trial: The effect of mindfulness-based cogni-tive therapy on generalized anxiety disorder among Chinese community patients: Protocol for a randomized trial. BMC
Psychiatry, 11(1), Article 187.
Wong, S. Y. S., Yip, B. H. K., Mak, W. W. S., Mercer, S., Cheung, E. Y. L., Ling, C. Y. M., & Lee, T. M. C. (2016). Mindfulness-based cognitive therapy v. group psychoeducation for people with generalised anxiety disorder: Randomised controlled trial.
The British Journal of Psychiatry, 209, 68-75.
World Health Organization. (1998). WHO-Five Well-Being Index
(Resource document). Author. Available from http://www. who-5.org
World Health Organization, World Organization of National Colleges, Academies, & Academic Associations of General Practitioners/Family Physicians. (2008). Integrating
men-tal health into primary care: A global perspective. Geneva,
Switzerland: World Health Organization Press.
Zaretsky, A., Segal, Z., & Fefergrad, M. (2007). New developments in cognitive-behavioural therapy for mood disorders. Canadian
Journal of Psychiatry/Revue Canadienne De Psychiatrie,
52(1), 3.
Zeiss, A. M., & Karlin, B. E. (2008). Integrating mental health and primary care services in the Department of Veterans Affairs health care system. Journal of Clinical Psychology in Medical
Settings, 15, 73-78.
Author Biographies
Elizabeth McCay,RN, PhD is a professor in the Daphne Cockwell School of Nursing at Ryerson University, Toronto, Ontario, Canada and holds a status appointment at the University of Toronto, Department of Psychiatry.
Rachael Frankford, MSW, RSW is a social worker in Family Practice at St. Michael’s Hospital Toronto, Ontario, Canada.
Souraya Sidani, PhD is a professor & Tier 1 Canada Research chair in the Daphne Cockwell School of Nursing at Ryerson University, Toronto, Ontario, Canada.
Enza Gucciardi,PhD is an associate professor, School of Nutrition at Ryerson University, Toronto, Ontario, Canada.
Rebecca Blidner,MSW, RSW is a social worker, Neurosurgery and Trauma Program, at St. Michael’s Hospital, Toronto, Ontario, Canada.
Audrey Danaher, RN, MSc is a research associate, Daphne Cockwell School of Nursing at Ryerson University, Toronto, Ontario, Canada.
Celina Carter,RN, BScN, MN is a research assistant, Daphne Cockwell School of Nursing at Ryerson University, Toronto, Ontario, Canada.