www.revportpneumol.org
ORIGINAL
ARTICLE
Obstructive
Sleep
Apnea:
Epidemiology
and
Portuguese
patients
profile
A.P.
Rodrigues
a,∗,
P.
Pinto
b,c,
B.
Nunes
a,
C.
Bárbara
b,caDepartamentodeEpidemiologia,InstitutoNacionaldeSaúdeDoutorRicardoJorge,Lisboa,Portugal
bProgramaNacionalparaasDoenc¸asRespiratórias,Direc¸ão-GeraldaSaúde,Servic¸odePneumologia,CentroHospitalarLisboa Norte,Lisboa,Portugal
cInstitutodeSaúdeAmbiental(ISAMB),FaculdadedeMedicina,UniversidadedeLisboa,Portugal
Received18July2016;accepted13January2017
KEYWORDS Sleepapnea; Publichealth; Prevalence; Portugal Abstract
Introduction:ObstructiveSleepApnea(OSA)ischaracterizedbyrecurrentepisodesofapnea and hypopnea, secondary to collapse ofthe upper airwaysduring sleep. OSA is frequently associatedtocardiovascularcomplications.InPortugal,itsmagnitudeisunknown.
Methods:In2014across-sectionalstudywasperformedusingthePortugueseGeneral Practi-tioner(GP)SentinelNetwork(RedeMédicosSentinela).ParticipantsGPreportedallOSAcases diagnosedandregisteredintheirlistsofusersonthe31December2013.
FrequencyofOSAhasbeenestimatedbysexandage.OSApatientswerealsocharacterized bymethodofdiagnosis,treatment,andunderlyingconditions.
AssociationbetweenriskfactorsandsevereOSA(oddsratio)wascalculatedusingalogistic regressionmodeladjustingconfounding.
Results:Prevalence of OSA on the population aged 25 years or more was 0.89% (95 CI: 0.80---1.00%);itwashigherinmales1.47%(95CI:1.30---1.67%)andinthoseagedbetween65and 74(2.35%).MosthadsevereOSA(48.4%).Hypertension(75.9%),obesity(74.2%)anddiabetes mellitus(34.1%)werethemostfrequentcomorbidities.Beingamale(OR:2.6;95CI:1.2---5.8) andhavingobesity(OR:4.0;95CI:1.8---8.6)wereassociatedwithanincreasedriskofsevere OSA.
Conclusion: FoundfrequencyofOSAwaslowerthanothercountriesestimates,whichmaybe explainedbydifferencesoncasedefinitionbutcanalsosuggestunderdiagnosisofthiscondition asreportedbyotherauthors.
©2017SociedadePortuguesadePneumologia.PublishedbyElsevierEspa˜na,S.L.U.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
∗Correspondingauthor.
E-mailaddress:ana.rodrigues@insa.min-saude.pt(A.P.Rodrigues). http://dx.doi.org/10.1016/j.rppnen.2017.01.002
2173-5115/©2017SociedadePortuguesadePneumologia.PublishedbyElsevierEspa˜na,S.L.U.ThisisanopenaccessarticleundertheCC BY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
The Obstructive Sleep Apnea (OSA) is characterized by recurrent episodes of apnea or hypopnea secondary to a collapseoftheupperairwaysduringsleep.
A widevariability in OSA prevalence is found between studiesduetoimportantdifferencesincasesdefinitionand studypopulation.1
It is estimated thatthe prevalence of OSA (definedby thepresenceof episodesofhypopnea andapnea and fre-quentdaytime sleepiness) in adult menvary between 1% and5%.1ConsideringOSAdefinitioncurrentlyused
(occur-renceofmorethan5episodesofapneaandhypopneaper hour),prevalence of OSA, accordinglysexand agegroup, canvarybetween2%and28%,halfofwhichisclassifiedas moderateorsevere.2,3PrevalenceofundiagnosedOSAmay
rangebetween0.3%and5%.4
AsOSAaffectsmainlymiddle-agedandobesemales,5it
isrecognizedthattheincreaseinobesitymaycontributeto anincreaseinOSAprevalence.
Inadditiontoitshighmagnitude,theclinicalimportance ofOSAcomesfromitscardiovasculareffects,consequences onmorbidity and mortality6,7 and also neuropsychological
changesthatincrease theoccurrenceof occupationaland trafficaccidents.8OSAisariskfactorforhypertensionand
itisalsoknownthathighbloodpressureriskincreaseswith severityof OSA.9 Infact,giventhehigh frequencyof OSA
withinindividuals withhypertension,10 thelatest standard
forhypertensiondiagnosticapproachrecommends perform-ingOSAdiagnosisincasesofhighbloodpressurewhichare resistanttotreatmentandhaveanon-dipperpatternon24h recordsofblood pressure.11,12 Itisalsoknownthat
preva-lenceofsleep-disorderedbreathingamongpatientswhohad strokesishigh,rangingbetween44%and74%,13emphasizing
thatthepresenceofOSAinthesepatientsisassociatedwith anincreasedriskofprematuremortality.14
TheassociationbetweenDiabetesandOSAhasrecently been described and thereis emerging evidence that OSA constitutesa risk factor for developmentof resistance to insulin15independentlyofobesity,whichmaybeinvolvedin
metabolicsyndromedevelopment.16
Another aspect that reinforces the importance of the diagnosis ofOSA is linked totheefficacy of nasal Contin-uous Positive Airway Pressure (CPAP) therapy in reversing neuropsychological disorders and reducing cardiovascular events.17 As a consequence of CPAP treatment, reduction
ofexcessivedaytimesleepinesscontributestoqualityoflife improvementandaccidentriskreductionbutalsothe occur-renceofhighbloodpressureisclearlylowerintheshortand longterm.18
Although Portuguese prevalence of OSA is unknown, consideringthehighprevalenceofadultobesityinPortugal19
ahighprevalenceofOSAcanbeexpectedintheadult Por-tuguesepopulation.NeitheristhepatientprofilewithOSA known,especiallyinterms of severity,treatment, comor-biditiesanduseofhealthservices.
As it is not currently feasible toimplement a popula-tionbasedsurveytoestimatethePortugueseprevalenceof OSA, the first approachtothe subject is to estimatethe frequencyofOSAknownwithinthepopulationunder obser-vationoftheGeneralPractitioner(GP)SentinelNetworkand tocharacterizeOSApatients.
Material
and
methods
Across sectionalstudy wasperformedwithinthe GP Sen-tinelNetwork(knownasRedeMédicosSentinela),whichhas nationaldistributionand117GPin2013.
At thebeginning of the study all Sentinel GPincluded in the RedeMédicos Sentinela in 2013 and also GPs that joinedthenetworkinthefirsttrimesterof2014(atotalof 7)wereinvitedtoparticipate.Invitationwassentbyemail andrenewedby phonecall.The studyprotocol, question-naireformsanddetailedstudyinstructionsweresenttoall doctorsthatacceptedtotakepartinthestudy.
GPparticipationconsistedinfillinginaquestionnairefor eachandalloftheirpatientsdiagnosedwithOSAat31stof Decemberof2013,usingexistingrecordedinformationdata tocollectfollowingdata:
1. Sexandage.
2. Diagnostic, including: diagnostic date, overnight poly-somnography or overnight respiratory polygraphy per-formance, apnea---hypopnea index, respiratory disturb index.
3. Comorbidities: diabetes, high blood pressure, obesity, coronary disease, stroke, acute myocardial infarction, arrhythmia,heartfailure,occurrenceoftrafficaccident (asdriver).
4. Treatment: CPAP, specialized sleep medical appoint-ment.
AnOSAcasewasdefinedassomeonehavingaprevious diagnosisofOSAperformedbyaspecialistandknownbythe patient’sfamilydoctor.
A Severe OSA was defined as someone having an apnea---hypopneaindexorrespiratorydisturbindexequalor higherthan30.
ProportionofOSA wasestimated bysexandage group using the sum of users aged25 yearsand more followed by each participating GPasdenominator (total of 34,909 individualsthatcomprisesthestudysample).
95Confidenceintervals(95CI)werecomputedusing Wil-sonmethod.20 Noestimateswerepresentedforagegroups
withlessthan5cases.
Mean(and95CI)andmedianwerecomputedfornumeric variables;proportions(and95CI)forcategoricalvariables. 2testwasusedtoidentifyvariablesassociatedtosevere
OSA anda logisticregression model, usingallvariables in which2significantlevelwas<0.20,wasperformedto
esti-mateadjustedOddsRatio(and95CI)ofhavingsevereOSA amongallOSApatients.
Model assumptions of the final regression model were checked by residual analysis.Hosmer and Lemeshowtest was used to check the goodness of the final regression model.
Results
29 (of 124) GP agreed toparticipate, giving a population underobservationof34,909individuals(Table1).AlltheGP that accepted participating in the study sent information relating to OSA cases, which corresponds to a 100% par-ticipationrate. Inrelation tosexandagedistribution,no
Table1 Studypopulationbysexandagegroup.
Agegroup(years) Male % Female % Total %
25---34 2,967 48.5 3,154 51.5 6,121 17.5 35---44 3,426 47.1 3,847 52.9 7,273 20.8 45---54 3,065 47.3 3,419 52.7 6,484 18.6 55---64 2,726 46.6 3,119 53.4 5,845 16.7 65---74 2,189 45.9 2,582 54.1 4,771 13.7 ≥75 1,699 38.5 2,716 61.5 4,415 12.6 Total 16,072 46.0 18,837 54.0 34,909 100.0
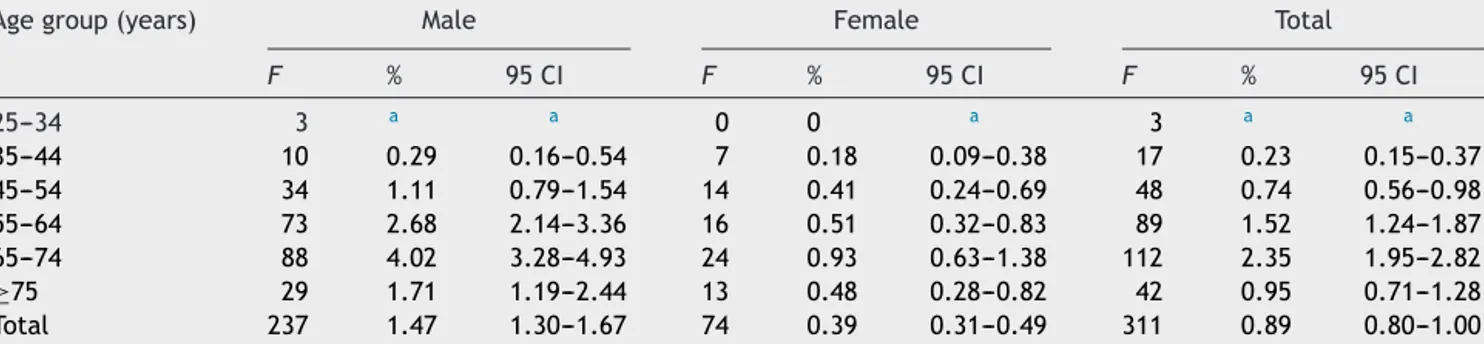
Table2 DistributionofObstructiveSleepApneabysexandage.
Agegroup(years) Male Female Total
F % 95CI F % 95CI F % 95CI 25---34 3 a a 0 0 a 3 a a 35---44 10 0.29 0.16---0.54 7 0.18 0.09---0.38 17 0.23 0.15---0.37 45---54 34 1.11 0.79---1.54 14 0.41 0.24---0.69 48 0.74 0.56---0.98 55---64 73 2.68 2.14---3.36 16 0.51 0.32---0.83 89 1.52 1.24---1.87 65---74 88 4.02 3.28---4.93 24 0.93 0.63---1.38 112 2.35 1.95---2.82 ≥75 29 1.71 1.19---2.44 13 0.48 0.28---0.82 42 0.95 0.71---1.28 Total 237 1.47 1.30---1.67 74 0.39 0.31---0.49 311 0.89 0.80---1.00
Note:F---frequency,95CI---95%confidenceinterval. a Lessthan5.
Table3 Comorbidities.
Comorbidities N F(%) 95CI
Obesity 302 224(74.2) 69.0---78.8
Highbloodpressure 303 230(75.9) 70.8---80.4 Diabetesmellitus 305 104(34.1) 29.0---39.6 Arrhythmia 294 35(11.9) 8.7---16.1 Trafficaccident 248 21(8.5) 5.6---12.6 Coronarydisease 294 33(11.2) 8.1---15.3 Heartfailure 295 28(9.5) 6.6---13.4 Stroke 297 18(6.1) 3.9---9.4
Acutemyocardialinfarction 295 19(6.4) 4.2---9.8 Note:N---numberofvalidobservations,F---frequency,95CI ---95%confidenceinterval.
differenceswerefound betweenthestudypopulation and thePortuguesepopulation(Supplementarymaterial).
311casesofOSAwereidentifiedinthatpopulation;the averageage was62.8 years(95 CI:61.6---64.1) andnoage differencewasfoundbetweensexes.
Proportion of cases aged 25 years and more has been 0.89% (95CI: 0.80---1.00). Ahigher proportionof OSA was foundinmales,namelybetween65and74years(4.02%;95 CI:3.28---4.93)(seeTable2).
97.3% (95 CI: 94.5---98.7) of all cases had undergone sleepstudyandofthose56.2%hadundergone polysomno-graphy.48.4%(95CI:40.8---56.1)hadaseveredisease(AHI or RDI≥30) andonly 17.6% (95CI:12.5---24.3) had amild disease[5≤(AHIorRDI)<15].
More than half of the cases (59.5%; 95 CI: 53.8---65.0) were followedthrough specializedmedicalappointments.
Continuous positive airway pressure treatment was pre-scribed to89.6% of all patients (95 CI:85.7---92.6), being thisproportionhigher(96.1%)for thosewhohada severe clinicalcondition.
Highbloodpressure(75.9%),obesity(74.2%)anddiabetes mellitus (34.1%) were the most frequent comorbidities in OSApatients(Table3).
InrelationtoOSAseverity,itwasfoundthatbeingmale (OR:2.6;95CI:1.2---5.8)andobese(OR:4.0;95CI:1.8---8.6) showedanassociationtoahigherriskofhavingsevere dis-easeamongallOSApatients(Table4).
Discussion
PrevalenceofObstructiveSleepApnea
AlthoughthisstudyfocusedonlyondiagnosedOSAcasesby familydoctors,thelowprevalenceofOSA(0.89%)found sug-geststhatlikeotherstudies2---4,8,21 thisclinical conditionis
actuallyunderdiagnosed.Nevertheless, ascase identifica-tionwas performed using medical registries that use the secondversionoftheInternationalClassificationforPrimary
Table4 RiskfactorsofSevereObstructiveSleepApnea.
OR(adjusted) 95CI p-value
Male 2.6 1.2---5.8 0.017
Obesity 4.0 1.8---8.6 <0.001
Note:ORadjustedbysex,obesity.OR---oddsratio,95CI---95% confidenceinterval.
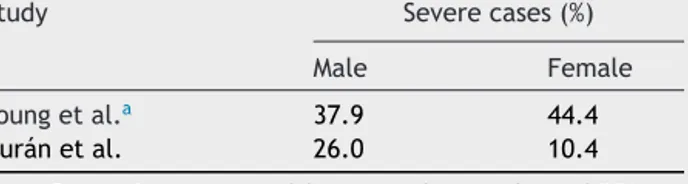
Table5 Proportionofseverecases.
Study Severecases(%)
Male Female
Youngetal.a 37.9 44.4
Duránetal. 26.0 10.4
Note:ProportionscomputedfromprevalencevaluesofOSA. aIncludesmoderateandseverecases(AHI≥15).
Care(ICPC2)wecannotexcludetheeffectoftheregistries’ characteristicsduringthecaseidentificationprocess.
On the other hand, compared to other countries2,3
(Table5)ahigherproportionofseverecaseswasfoundon ourstudy(48.4%),whichsuggeststhatOSApatientsknownin primaryhealthcaresettingarethosewithasevereclinical presentation. The legal requirementfor a treatment pre-scriptionperformedbyamedicaldoctorwithintheNational Health System is probably favors a better knowledge of severecases.
Consideringthehypothesisofunderdiagonisand accept-ingthefactthatseverecasesrepresents20%ofallOSAcases (a similar value was found in Spain3), OSA prevalence at
populationlevel(aged25yearsandmore)couldbearound 2.2%,whichisstilllowerthanthatfoundinUSA2(4%male,
2% female) and Spain3 (26.2% male, 28.0% female).
Sev-eralmethodologicaldifferencesbetweenstudieswerefound (namely in sampling framework, age groups, case selec-tionandcasedefinition1---3,21)thatlimitdatacomparability.
Nevertheless,ascasedefinitionusedinYoungetal.study2
includesthepresenceofsymptomsofOSAandanAHI≥5, weconsidered thatit canbecloser tothecase definition usedinthisstudythanthatusedbyDuránetal.3However,
givenourcase definition(previousdiagnosis performedby a specialist and knownby the patient’s familydoctor), a selectionbiascannotbeexcludedifOSAdiagnosishadbeen morefrequentlymadeinmalepatients,whichmayexplain ahighersexratioestimate(3.8male:1.0female)thanthat observedbyYoungetal.2(3:1).
The highest prevalence of OSA for both sexes found between65 and74 yearsof agecan indicatea late diag-noseofOSAwhencomparedtootherstudywhichshowthat thehighest prevalencein menwasobserved betweenthe 5thand 6th decadesof life.22 These results highlight the
hypothesisofunderdiagnosisof OSA,namelyamongyoung andlesshealthcareconsumerpopulation.
Comorbidities
TheunderlyingconditionsobservedinourOSApatientswere thosefrequentlyassociatedtoOSAasriskfactors(obesity) orascomplications(DMandhighbloodpressure).3,8,10,15,23---25
Asexpected,theproportionofOSApatientssufferinghigh bloodpressure(75.9%)ishigherthantheprevalenceofhigh bloodpressureobservedintheadultPortuguesepopulation (42%).26Nevertheless,contrarytowhathasbeensuggested
byother studies,10,23,24 noassociation betweenhigh blood
pressureandOSAseveritywasfoundwhichcanbeexplained by the high proportion of cases withhigh blood pressure andthe reduced number of cases (n=311). Alsothe high proportionofobesityinoursample27andtheoldageofthe
participantscouldcontributetothisnullassociationashigh bloodpressureislessassociatedtosevereOSAwithinolder andobesepatients.8
The association of male sex, obesity and severe OSA found is compatiblewith therole of these factors in the pathogenesisofthediseasedescribedelsewhere.2
Limitations
Asalimitation,itisimportanttomentionthatthestudy set-tingandcasedefinitionusedonlypermittedustoestimate theproportionofusersofprimarycaresufferingfromOSA insteadofanestimateoftherealprevalenceofOSA.Despite the large sample size used and its similar demographic structure, when compared to the Portuguese population, the distribution of participating GP does not guarantee a nationalrepresentativenessofthesample.
Conclusions
As far asweknow, thiswasthefirst approachtoworking out the burden of thisdisease on thePortuguese popula-tion.OurresearchfoundalowprevalenceofOSAwithinthe Portuguesepopulationaged25yearsandmore,whichmay indicateanunderdiagnosisofthishealthcondition.
Ethical
disclosures
Protection of human and animal subjects.The authors declarethatnoexperimentswereperformedonhumansor animalsforthisstudy.
Confidentialityofdata.Theauthorsdeclarethattheyhave followedtheprotocolsoftheirworkcenteronthe publica-tionofpatientdata.Alldataanalyzedbytheresearchteam areanonymizedanddidnotpermittoidentifyanypatient.
Righttoprivacyandinformedconsent.Asonlysecondary datausedinthisresearch,itwasnotpossibletocollectwrite informedconsent.Onlyanonymizeddatawereusedandno individualpatientdataappearinthisarticle.
Conflicts
of
interest
Theauthorshavenoconflictsofinteresttodeclare.
Acknowledgement
ToallthePrimaryHealthCaredoctorsthatparticipatedon thissurvey.
ToInêsBatistafortheadministrativesupportneededto realizethisstudy.
Appendix
A.
Supplementary
material
Supplementary material associated with this arti-cle can be found in the online version available at
References
1.DaviesRJO,StradlingJR.Theepidemiology ofsleep apnoea. Thorax.1996;51:S65---70.
2.YoungT,PaltaM,DempseyJ,SkatrudJ,WeberS,BadrS.The occurrenceofsleep-disorderedbreathingamongmiddle-aged adults.NEnglJMed.1993;328:230---1235.
3.Durán J, Esnaola S, Rubio R, Iztueta A. Obstructive sleep apnea---hypopneaandrelatedclinicalfeaturesina population-basesampleofsubjectsaged30to70years.AmJRespirCrit CareMed.2001;163Pt1:685---9.
4.LindbergE,GislasonT.Epidemiologyofsleep-related obstruc-tivebreathing.SleepMedRev.2000;4:411---33.
5.ChungF,SubramanyamR,Liao P,SasakiE,ShapiroC,SunY. HighSTOP BANGscoreindicatesahighprobabilityof obstruc-tivesleepapnea.BrJAnaesth.2012;108:768---75.
6.Lopez-JimenezF,KuniyoshiFHS,GamiA,SomersVK. Obstruc-tivesleepapnea:implicationsforcardiacandvasculardisease. Chest.2008;133:793---804.
7.ShaharE,WhitneyCW,RedlineS,LeeET,NewmanAB,NietoFJ, etal.Sleep-disorderedbreathing andcardiovasculardisease: cross-sectionalresultsoftheSleepHeartHealth Study.AmJ RespirCritCareMed.2001;163:19---25.
8.YoungT,PeppardPE,GottliebDJ.Epidemiologyofobstructive sleepapnea.AmJRespirCritCareMed.2002;165:1217---39. 9.Durán-CantollaJ,AizpuruF,Martínez-NullC,BarbéF.
Obstruc-tivesleepapnea/hypopneaand systemichypertension.Sleep MedRev.2009;13:323---31.
10.Lavie P, Herer P, Hoffstein V. Obstructive sleep apnea syn-dromeasariskfactorforhypertension:populationstudy.BMJ. 2000;320:479---82.
11.AmericanHeart Association. A scientificstatement from the American Heart Association Professional Education Commit-teeoftheCouncilforHighBloodPressureResearch.Resistant Hypertension:diagnosis,evaluationandtreatment. Hyperten-sion.2008;51:1403---19.
12.EuropeanSociety ofHypertension, European Societyof Car-diology. The Task Force for the Management of Arterial HypertensionoftheEuropean Societyof Hypertension(ESH) andoftheEuropeanSocietyofCardiology(ESC).2007 guide-linesforthemanagementofarterialhypertension.JHypertens. 2007;25:1105---87.
13.ParraO,ArboixA,BechichS,García-ErolesL,MontserratJM, LópezJA,etal.Timecourseofsleeprelatedbreathingdisorders infirst-everstrokeortransientischemicattack.AmJRespirCrit CareMed.2000;161:375---80.
14.SahlinC,SandbergO,GustafsonY,BuchtG,CarlbergB, Sten-lundH,etal.Obstructivesleepapneaisariskfactorfordeath inpatientswithstroke.A10-yearfollow-up.ArchInternMed. 2008;168:297---301.
15.PunjabiNM, SorkinJD, KatzelLI,GoldbergAP,Schwartz AR, SmithPL.Sleep-disorderedbreathingandinsulinresistancein
middle-agedandoverweightmen.AmJRespirCritCareMed. 2002;165:677---82.
16.Kono M, Tatsumi K, Saibara T, Nakamura A, Tanabe N, TakiguchiY,etal.Obstructivesleepapneasyndromeis asso-ciatedwithsomecomponents ofmetabolicsyndrome.Chest. 2007;131:1387---92.
17.PintoP,CristinaBárbaraC,MontserratJM,PatarrãoRS,Guarino MP,Carmo MM,et al.Effects ofCPAPonnitrateand norepi-nephrinelevelsinsevereandmild---moderatesleepapnea.BMC PulmMed.2013;13:1---7.
18.Haentjens P, Van Meerhaeghe A, Moscariello A, Weerdt S, Poppe K,DupontA, etal.Theimpactofcontinuouspositive airway pressure onblood pressure in patients with obstruc-tive sleep apnea syndrome. Evidence from a meta-analysis of placebo-controlled randomized trials. Arch Intern Med. 2007;167:757---65.
19.World Health Organization (WHO). Obesity: situation and trends. WHO; 2014 [Online]. Available in: http://apps. who.int/gho/data/node.main.A900[accessed30.11.14]. 20.Domenech JM, Granero R. Macro !CIP for SPSS statistics.
Confidence intervals for proportions [programa informático] V2012.07.13. Bellaterra:UniversitatAutònoma deBarcelona; 2012.Availablein:http://www.metodo.uab.cat/macros.htm 21.ZamarrónC,GudeF,OteroY,AlvarezJM,GolpeA,Rodriguez
JR. Prevalence of sleep disordered breathing and sleep apneain50-to70-yearoldindividuals.Respiration.1999;66: 317---22.
22.Bixler EO, Vgontzas AN, HAveTT, Tyson K, Kales A. Effects of age onsleep apnea inmen. Am JRespir Crit CareMed. 1998;157:144---8.
23.Young T, Peppard P, Palta M, Hla KM, Finn L, Morgan B, et al. Population-based study of sleep-disordered breathing asariskfactorfor hypertension.ArchIntern Med.1997;157: 1746---52.
24.PeppardPE,YoungT,PaltaM,SkatrudJ.Prospectivestudyof theassociationbetweensleep-disorderedbreathingand hyper-tension.NEnglJMed.2000;342:1378---84.
25.NietoFJ,YoungTB,LindBK,ShaharE,SametJM,RedlineS, etal.Associationofsleep-disorderedbreathing,sleepapnea, and hypertension in a large community-based study: Sleep HearthHealthStudy.JAMA.2000;283:1829---36.
26.PolóniaJ,MartinsL,PintoF,NazareJ.Prevalenceawareness, treatmentandcontrolofhypertensionandsaltintakein Portu-gal:changesoveradecade.ThePHYSAstudy.JHypertension. 2014;32:1211---21.
27.Carmo I, SantosO, Camolas J,Vieira J, Carreira M,Medina L, et al. Overweight and obesity in Portugal: national prevalence in 2003---2005. Obes Rev. 2007;9:11---9. World of obesity,2014[Online].Availablein:http://www.worldobesity. org/aboutobesity/world-map-obesity/[accessed18.08.14].