SEVERE FORMS OF NEUROCYSTICERCOSIS
TREATMENT W I T H ALBENDAZOLE
SVETLANA AGAPEJEV*, MARIA DORVALINA DA SILVA**, ANETE K. UEDA***
ABSTRACT - Study of 22 patients with the severe form of neurocysticercosis treated with albendazole (ABZ) administered in 6 different schedules ranging from 15 to 30 mg/kg/day for 21 to 60 days. Dextrochloropheniramine and ketoprofen were the adjuvant drugs. Multiple symptoms were observed in 90.9% of patients. Intracranial hypertension was manifested in 90.9%. Hydrocephaly occurred in 86.4%. Evolution was satisfactory in 10
patients, 8 died and 4 had sequelae. Tomographic studies showed the appearance of an isolated IVth
ventricle in 9 patients, after ventriculoperitoneal shunt, before ABZ treatment in 3 of them, during in 5 and after treatment in one. Median clinical follow-up duration was 10 months for the patients who died and 3-4 years for survivors. In 3 patients there was an increase in cyst size during the administration of the 15 mg/kg/day A B Z dose, which was not observed in any patient when the 30 mg/kg/day dose was used.
KEY W O R D S : cysticercosis, neurocysticercosis, severe forms, treatment, albendazole, d e x t r o -chloropheniramine, ketoprofen.
Formas graves da neurocisticercose: tratamento com albendazol
RESUMO - Estudo de 22 doentes, com a forma grave de neurocisticercose, tratados com albendazol (ABZ), administrado em 6 diferentes e s q u e m a s , que variaram de 15 a 30 mg/kg/dia, durante 21 a 60 dias. A dextroclorofeniramina e o cetoprofeno foram as drogas coadjuvantes. Múltiplos sintomas ocorreram em 20 doentes. Hipertensão intracraniana foi manifestação mais comum em 20. Hidrocefalia foi detectada e m 19. A evolução foi satisfatória em 45,4%, faleceram 36,4% e 18,2% ficaram com sequelas. Na evolução tomográfica
apareceu IVo
ventrículo isolado em 40,9%, após derivação ventriculoperitoneal, em 3 deles antes do tratamento com ABZ, em 5 durante e, em um, após o tratamento. A mediana estatística do período de seguimento clínico foi 10 meses para aqueles que faleceram e 3-4 anos para os sobreviventes. Em 3 doentes houve aumento no tamanho dos cistos durante a dose de 15 mg/kg/dia de ABZ, não observado na vigência de 30 mg/kg/dia.
PALAVRAS-CHAVE: cisticercose, neurocisticercose, formas graves, tratamento, albendazol, dextro-clorofeniramina, cetoprofeno.
T h e manifestations o f n e u r o c y s t i c e r c o s i s ( N C C ) may b e c l a s s i f i e d into b e n i g n and malignant, or s e v e r e , f o r m s5
' M
. In t h e first, t h e p a r a s i t e s u s u a l l y are p a r e n c h y m a t o u s , n o n - c i s t e r n a l c o r t i c o m e n i n g e a l or, to a l e s s e r extent, ventricular. T h i s form represents the clinical e x p r e s s i o n o f Cysticercus cellulosae. T h e patients m a y b e a s y m p t o m a t i c or report h e a d a c h e and epileptic s y n d r o m e as predominant s y m p t o m s . Skull c o m p u t e d t o m o g r a p h y ( C T ) reveals small l e s i o n s c o m p a t i b l e w i t h
Division of Neurology, D e p a r t m e n t of N e u r o l o g y and Psychiatry and D e p a r t m e n t of Pathology, B o t u c a t u S c h o o l of M e d i c i n e , S t a t e U n i v e r s i t y of S ã o P a u l o ( U N E S P ) . * M . D . , P h . D . , A s s i s t e n t Professor(Neurology); * * M . D . , Assistent Physician ( N e u r o l o g y ) ; * * * M . D . , Ph.D., Assistent Professor (Pathology). A c e i t e : 1 7 - s e t e m b r o - 1 9 9 5 .
v e s i c l e s , calcifications and/or granulomas distributed throughout the cerebral parenchyma. Prognosis is g o o d , the therapeutic r e s p o n s e is rapid, and survival is l o n g . In the s e v e r e f o r m the parasites are g e n e r a l l y l o c a t e d in a c i s t e r n a l or v e n t r i c u l a r s u b a r a c h n o i d p o s i t i o n . V a s c u l i t i s i s frequent. H y d r o c e p h a l y is the m o s t c o m m o n manifestation and m a y result both from basal arachnoiditis and f r o m the p r e s e n c e o f intraventricular c y s t i c e r c o s i s . T h i s is the clinical manifestation o f Cysticercus racemosus. T h e r e are m u l t i p l e s y m p t o m s or m a n i f e s t a t i o n s o f intracranial h y p e r t e n s i o n (ICH). P r o g n o s i s is bad, the therapeutic r e s p o n s e is s l o w and poor, and survival is short. T h e high morbidity and mortality rates o f N C C , s p e c i a l l y w h e n the clinical manifestation is I C H , reflect the severity o f this neuroparasitosis. Surgical and s y m p t o m a t i c treatment has b e e n m o s t often indicated for the s e v e r e f o r m s , s p e c i a l l y in the p r e s e n c e o f I C H6 , 2 8
.
T h e o b j e c t i v e o f the present study w a s to report o n the e v o l u t i o n o f 2 2 patients with the s e v e r e form o f N C C treated with A B Z plus d e x t r o c h l o r o p h e n i r a m i n e and ketoprofen as adjuvants.
CASES AND METHODS
Of the 138 patients with NCC treated with ABZ from January 1985 to February 1993, were selected 22 who presented the severe form of the disease. The criterion of severity was based on the classification of Camargo Lima5
and Estanol1 4
, with some modifications (Table 1). Patients with inflammatory cells in the cerebrospinal fluid (CSF) but with no clinical signs of ICH, patients with a clinical and tomographic picture compatible with benign ICH (pseudotumor cerebri), patients with hydrocephaly, derived or not, but without signs of ICH, patients with manifestations of ischemic cerebral vascular episodes without ICH, patients with a small or questionable isolated increase of the IVt h
ventricle, and all patients who abandoned follow-up at the outpatient clinic for a period of less than 2 years after the end of the therapeutic schedule proposed were excluded from the study.
Among the 22 patients who participated in the study, 15 (68.2%) were males and 7 (31.8%) were females, ranging in age from 15 to 62 years. All subjects were white.
Among the immunologic reactions for cysticercosis performed at the CSF Laboratory from 1984 to 1993, the complement fixation reaction (CFR) was not performed in 75 to V , of the tests, and the
immunofluorescence (IFC) reaction was not performed in ¾ of the tests.
It was possible to submit all patients to a CT scan before and after ABZ treatment, but only 14 of them were submitted to a CT scan during treatment.
A definitive diagnosis of cysticercosis was made in 10 of the 22 patients (45.4%) by autopsy or biopsy. A ventriculoperitoneal shunt (VPS) was implanted when clinical or tomographic evidence of hypertensive hydrocephaly was observed (19 patients). Except for2 patients whose diagnosis of NCC was made postoperatively, craniotomy was indicated whenever maintenance of clinical signs and symptoms occurred (5 patients) after the end of ABZ treatment.
Patient evolution was studied in the presence of various schedules of ABZ treatment (Table 2) as an effort to define the best and efficacious dose. None of the patients was submitted to corticotherapy immediately before, during or after the use of ABZ. In cases in which clinical exacerbation of ICH occurred, no matter how mild, ketoprofen (150 to 300 mg/day), 20% manitol (5 to 10 ml/kg/day) and acetazolamide (250 to 500 mg/day) were administered at doses depending on the intensity of clinical manifestation. Patients with epileptic seizures received anticonvulsants. The antihistamine dextrochlorpheniramine (DCP) was administered (12 to 24 mg/ day) to all patients and was maintained for 4 to 12 months after the end of the therapeutic schedule used. A new treatment with ABZ was performed for a period of 6 months (2 patients) to 1 - 2 years (2 patients) after the end of the first schedule due to the maintenance of clinical signs and symptoms.
The period of clinical observation covered the patients treated from January 1985 to February 1993, with follow-up at the outpatient clinic up to February 1995.
RESULTS
Clinical evolution
During treatment, severe ICH was observed only in one patient (Case 15) and hydrocephaly occurred in 2 (Cases 1 and IS, both with a history of more than one hospitalization due to meningitis). Epileptic seizures did not increase during ABZ treatment, but rather decreased in intensity and frequency.
All patients with hydrocephaly were submitted to VPS implantation at different times in relation to the therapeutic schedule with ABZ (Table 4). One patient (Case 13) was submitted to exeresis of a cystic tumor (biopsy = racemose cysts) in the right sylvian region before ABZ treatment (performed in another service) and 3 years after ABZ treatment for the removal of a left occipital cystic lesion (biopsy = degenerated and fibrotic cysticercus). Four patients (Cases 8 , 9 , 1 2 , 1 9 ) were submitted to surgery on the posterior fossa to reach the IV* ventricle, where arachnoiditis of varying intensity was observed in 3 of them (Cases 9, 12, 19). In the case 8 who had been submitted to surgery before A B Z treatment, the cysts were racemose and were intact, and in another (Case 19), submitted to surgery approximately 10 months after the end of ABZ treatment, the cysts were degenerate. Of these 4 patients, only one survived (Case 8), although with paraparesis as sequelae.
The evolution (Table 2) was good in 45.5% (10:22) of patients, who were able to fully assume their normal activities. In these patients, the epileptic seizures were controlled with very low doses of anticonvulsants. The neurologic sequelae limited the normal activities of 18.2% patients (4:22). Patient mortality was 36.4% (8:22): 3 (37.5%) of them (Cases 1, 2, 3) died during treatment with 15 mg/kg/day ABZ, and 5 (62.5%) after the end of treatment. Of these 5 patients, 80% (4:5) died within less than 36 months and only one (Case 9) died 6 years after the end of ABZ treatment. Of the 8 patients who died, 5 (62.5%) were males and 3 (37.5%) were females.
Ventricular localization of the parasites was suggestive in 10 patients (45.4%), on the basis of the appearance of an isolated IV* ventricle in 8 of them, and as observed during surgery in 2 (Cases 8, 19). Of these, 3 (30%) had a good evolution, 3 (30%) died and 4 (40%) evolved with sequelae (Table 2). In one of the patients with an isolated IV"1
ventricle (after VPS), the appearance of the angulo-ponto-cerebellar region syndrome was observed during treatment with IS mg/kg/day ABZ, with regression within approximately 2 years after the use of 30 mg/kg/day ABZ for 60 days (Fig 3; Case 20).
Of the 8 patients who died, 3 (Cases 2, S, 12) were not submitted to autopsy, although their deaths were clinically attributed to pulmonary infection or ICH. Of the 5 patients submitted to autopsy, 40% (2:5) had pulmonary problems as the causa mortis, and in the remaining ones (3:5), the direct cause of death was ICH. Autopsy of the cases who had used a maximum of 15 mg/kg/day ABZ (Cases 1,2) revealed intact and degenerating cysts (Fig 2; Case 1). In the patients who had used 30 mg/kg/day of the drug for 60 days, the cysts were degenerated or calcified (Fig 2; Case 18).
clinical worsening ranged from 5 days to 54 months (median = 2 months). Survival time (Table 5) either starting from the first symptoms or from clinical worsening and/or treatment with ABZ was more than 4 years, including one death in 59.1% of patients.
Evolution of CSF
Examination of the CSF of punctured patients showed variable alterations (Table 6) depending on the time of collection.
Before ABZ treatment, negativity of immunologic reactions was observed in 2 cases. CSF exacerbation occurred in 50% (9:18) of the patients submitted to CSF puncture before, during and after ABZ treatment.
After the end of A B Z treatment, in a variable time interval, the last CSF samples in the medical records showed decreased cellularity in all patients, an increase in eosinophilorrachia in 16.7% (3:18), 2 of whom died, elevation of proteinorrachia in 44% (8:18) and a decrease in glucorrachia in 27.8% (5:18). The only patient who presented plasmocytorrachia also died. As to the reactions for cysticercosis, CFR remained positive in 46.2% (6:13) and IFC became positive in 25% (2:8).
Tomographic evolution
Skull CT before ABZ treatment was altered in all patients. The lesions observed were associated with one another in 86.4% (19:22) and were single in 13.6% (3:22). Among these 3 patients with a single lesion, diffuse cerebral edema occurred in 2 (Cases 12,15) and a single giant cyst in one (Case 7). Among the associated lesions, hydrocephaly was the most common (16:22), followed by the presence of racemose cysts (11:22). These, in turn, were multiple (2 to 3) in 81.8% of cases (9:11) and localized in the sylvian region (unilateral in 5 patients and bilateral in 3), in base cistemae (7 patients), in the median frontal region (Cases 1 , 3 , 18) and around the brain stem (Case 1). The topography of the racemose cysts present at a single location was left parietal lobe(Case 11) and in the IVl h
ventricle (Case 8). Calcifications (6:22) and multiple parenchymatous cysts (8:22) were associated with several aspects of the lesion and did not appear as single lesions.
During treatment with ABZ, CT showed that the parenchymatous cysts decreased in size or disappeared during the final phase of the 15 mg/kg/day ABZ schedule. Hydrocephaly decreased spontaneously in 1 patient (Case 14), appeared in 3 (Cases 1 , 2 , 1 5 ) and worsened in 1 (Case 22). An isolated IV* ventricle occurred in 2 patients without previous hydrocephaly and in 3 patients with previous hydrocephaly corrected by VPS. Cerebral edema appeared in 1 patient, remained unchanged in 4 and regressed in 3. The number of calcifications increased in 2 patients and remained unchanged in the other 6. Of the 11 patients with racemose cysts, only 5 were submitted to CT during treatment, and an increase in the cysts was observed in 2 of them (Fig 2; Case 1, Fig 3; Case 10). In a patient with VPS due to previous hydrocephaly, a previously undetected giant cystic lesion occurred in the left angulo-ponto-cerebellar region in addition to an isolated IV"1
DISCUSSION
A s o l d as the k n o w l e d g e o f the e x i s t e n c e o f c y s t i c e r c o s i s ( A r i s t o p h a n e s , ca. 4 0 0 b . C . )2 1
are the attempts at treatment o f the t e n i a s i s / c y s t i c e r c o s i s c o m p l e x . Treatment o f teniases with an extract o f male w i l d fern roots (Theophrastus, ca. 3 3 0 b . C . )1 0
w a s o n l y replaced with synthetic antiparasitic agents in 1 9 6 02 0
. W h e n an o p t i o n m u s t b e taken b e t w e e n surgical indication and p h a r m a c o l o g i c a l t h e r a p y4 , 6 1 2
"1 , 2 7
'3 0 , 3 3
, c o n t r o v e r s y still e x i s t s , s p e c i a l l y w h e n the c y s t is o f ventricular or subarachnoid l o c a l i z a t i o n9
'1 1 1 9 , 2 4 , 2 9
. E v e n s o , a c o m m o n c o n s e n s u s can be reached about the fact that the therapeutic conduct s h o u l d b e i n d i v i d u a l i z e d for e a c h p a t i e n t1 , 8
-9 , 3 3
, s i n c e the s e r u m and C S F l e v e l s o f c y s t i c i d e s present a w i d e individual v a r i a t i o n1 7
not related to a g e , s e x , p r e s e n c e o f an inflammatory p r o c e s s or therapeutic efficacy, but d e p e n d i n g o n the individual pharmacokinetic differences.
H o w e v e r , w h e n pharmacologic therapy is c h o s e n , further controversy arises, n o w related to the concentration of the cysticide, to time o f treatment, localization o f the parasite and clinical form o f m a n i f e s t a t i o n1 , 3
'1 1 , 1 3
'2 7
'3 1
'3 3
. O n the other hand, there are no longer any doubts about the fact that A B Z i s
more effective than praziquantel8 , 2 6
'3 1
, also because it better penetrates the subarachnoid s p a c e1 7
.
A l t h o u g h t e c h n o l o g i c a l a d v a n c e s s u c h as E L I S A in C S F and n e u r o i m a g i n g b e c a m e a v a i l a b l e in our s e r v i c e o n l y in 1 9 9 4 , w e o n l y included in our series the patients treated until 1 9 9 3 b e c a u s e w e felt that a f o l l o w - u p o f l e s s than 2 years m a y g i v e a falsely favorable impression, or e v e n an unfavorable
impression, as w e l l demonstrated b y the e v o l u t i o n o f our patients, a m o n g w h o m there w a s o n l y o n e death after this f o l l o w - u p period ( C a s e 9 ) . Furthermore, the appearance o f fatal e p i s o d e s ( C a s e s 1 , 2 , 3 , 5 , 1 2 , 1 8 , 1 9 ) or o f c o m p l i c a t i o n s ( C a s e s 1 0 , 1 3 , 1 9 , 2 1 ) is m o r e frequent during this p e r i o d1
-5 , 6 , 1 4 , 2 2
.
A point c o m m o n to m o s t reports o n the treatment w i t h c y s t i c i d e s , either a l b e n d a z o l e or
praziquantel, is the e x c l u s i o n o f patients with s i g n s o f I C H3 , 2 7
-3 1
and the diversification o f treatment s c h e d u l e s . T h e p r e s e n c e o f l o c a l i z i n g neurological s y m p t o m s has a l s o b e e n a criterion for e x c l u s i o n
o f pharmacological t r e a t m e n t4 , 6 , 2 7
'3 0
. H o w e v e r , for us these w e r e the criteria for patient i n c l u s i o n in the present study. T h u s , an attempt at c o m p a r i n g our data with t h o s e o f any other study in the
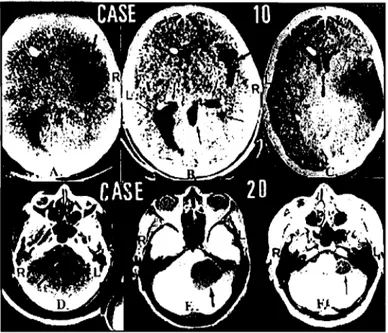
Fig 3. Case 10. A (before the 1st
ABZ treatment): multiple hypodense lesions (arrow) suggesting racemose cysticercosis. B(5 months after the 1st
ABZ treatment): observe the appearance of cysts not detected in A (arrows) and a decrease of the cyst previously present. C (28 months after the use of 30 mg/kg/day ABZ for 60 days): disappearance of the cysts.[R, right; L, left.] Case 20, D (before ABZ treatment): a medium to small isolated IVth
ventricle (arrow), apparently without lesions in an angulo-ponto-cerebellar region. E (during the 3rd
week of 15 mg/ kg/day ABZ): observe the appearance of a cystic lesion in this region (arrow). F (20 months after the ABZ schedule): an encapsulated cystic area continues to be present in the same region, although smaller in size. [R, right; L, left].
C a s e s 1 and 18 ( F i g 2 ) , v e r y similar i n clinical, C S F and t o m o g r a p h i c terms, differed in the
A B Z s c h e d u l e u s e d , i n the c a u s a mortis and in the aspect o f the c y s t i c e r c i detected. In C a s e 1, w h o r e c e i v e d d o s e s o f u p to 15 m g / k g / d a y for a shorter period o f t i m e , the i m m e d i a t e c a u s e o f death w a s
ICH and the parasites w e r e intact and i n different s t a g e s o f d e g e n e r a t i o n ; in addition there w a s an increase in r a c e m o s e c y s t s during treatment. In contrast, i n c a s e 1 8 , w h o r e c e i v e d h i g h e r d o s e s and for l o n g e r p e r i o d s o f t i m e , the i m m e d i a t e c a u s e o f death w a s not n e u r o l o g i c a l and all parasites w e r e
in an e q u a l l y a d v a n c e d p h a s e o f d e g e n e r a t i o n . O n the other hand, o n e s h o u l d k e e p in m i n d the g o o d e v o l u t i o n o f C a s e s 2 0 ( F i g 3 ) and 2 2 , a n d o f C a s e 1 0 , w h o presented an i n c r e a s e o f the c y s t s w h i l e
taking a l o w e r d o s e o f the drug o v e r a shorter period o f treatment; further treatment w a s n e e d e d , and o n l y then d i d the patient s h o w g o o d r e c o v e r y ( F i g 3 ) .
T h e study o f t h e s e patients supports the u s e o f h i g h d o s e s o f A B Z o v e r a p r o l o n g e d period o f time, e s p e c i a l l y in s e v e r e c a s e s , although D e l B r u t t o1 0
and S o t e l o2 7
stated that better results are not
obtained with higher d o s e s or l o n g e r treatment.
T h e p r e s e n c e o f h y d r o c e p h a l y i s , o f itself, s u f f i c i e n t t o q u a l i f y a s s e v e r e t h e f o r m o f manifestation o f cysticercosis in the C N S1 4
. A n d w h e n it occurs as the first manifestation, the p r o g n o s i s is w o r s e3 2
. T h i s w a s c l e a r l y d e m o n s t r a t e d b y our s e r i e s , i n w h i c h all p a t i e n t s w h o d i e d h a d
hydrocephaly.
clinical manifestations o f ICH are absent but t o m o g r a p h i c s i g n s o f p e r i e p e n d y m a l e d e m a are present, h y d r o c e p h a l y s h o u l d be r e l i e v e d as s o o n as p o s s i b l e and p h a r m a c o l o g i c a l treatment s h o u l d be instituted i m m e d i a t e l y after (Table 4 ) . T h i s c o n d u c t has greatly i m p r o v e d patient p r o g n o s i s and d e c r e a s e d the n u m b e r o f r e v i s i o n s o f the shunt s y s t e m .
O n the other hand, w h e n an isolated I V * ventricle occurred, our experience in approaching the posterior fossa with or without the previous installation o f a V P S s y s t e m w a s disastrous (Cases 9 , 1 2 , 19). T h i s highly negative experience m a y perhaps have b e e n d u e to the fact that surgery w a s carried out after pharmacological treatment in all 3 patients. This treatment, by b e i n g effective, led to arachnoiditis w h i c h , o f itself, is a contraindication o f an approach to the I V * v e n t r i c l e6 , 2 4
. Perhaps, if this approach had b e e n carried out before clinical treatment, the evolution might h a v e b e e n different. H o w e v e r , the hypertensive hydrocephaly o f these patients w a s detected o n l y after the u s e o f A B Z , representing o n e more factor o f prognostic worsening. In the remaining c a s e s with an isolated I V * ventricle, V P S w a s performed before A B Z treatment, except for C a s e 15 w h o s e V P S w a s installed during clinical treatment. After 4 - 5 years had passed without the need for revision of the V P S s y s t e m , spontaneous regression of the I V * ventricle occurred in this patient (Case 15). T h e remaining patients with this type o f ventricular lesion have not yet c o m p l e t e d 4 years o f f o l l o w - u p at the outpatient clinic.
A l t h o u g h m e n presented a higher incidence o f the severe form o f N C C ( 6 8 . 2 % ) , a fatal evolution or an e v o l u t i o n with s e q u e l a e w a s m o r e c o m m o n a m o n g w o m e n . A m o n g f e m a l e patients, 4 2 . 8 % ( 3 : 7 ) d i e d or s u r v i v e d with s e q u e l a e at the s a m e proportion. O n e w o m a n ( C a s e 16) also had the spinal form o f c y s t i c e r c o s i s . T h i s p r e v a l e n c e o f the p a t h o l o g y in the m a l e s e x and the higher fatal
o u t c o m e a m o n g w o m e n h a v e b e e n w i d e l y d i s c u s s e d in the literature2 , 2 1
.
In 1 9 8 4 , w h e n w e started the study o f A B Z in N C C , w e u s e d to c o m b i n e d e x a m e t h a s o n e as an adjuvant in the first 3 patients. H o w e v e r , s e v e r e u n c o n t r o l l a b l e c o m p l i c a t i o n s such as arterial hypertension and diabetes w h i c h arose in these 3 patients led to the n e e d to replace the g l u c o c o r t i c o i d w i t h the a n t i h i s t a m i n e . T h i s r e p l a c e m e n t w a s b a s e d o n k n o w l e d g e about the i m m u n o a l l e r g i c m e c h a n i s m s7 , 1 5
o f the manifestations o f this neuroparasitosis and o n the n o t i o n that g l u c o c o r t i c o i d s d o not inhibit the antigen-antibody reaction and the c o n s e q u e n t release o f h i s t a m i n e and other active s u b s t a n c e s2 2
, w h e r e a s antihistamines c o m p e t e w i t h histamine in their receptors and therefore impair its a c t i o n1 6
. T h u s , e n c o u r a g e d b y the g o o d clinical response o b s e r v e d in the first 3 patients and those w h o f o l l o w e d , w e a b o l i s h e d the c o r t i c o i d and introduced the a n t i h i s t a m i n e as an adjuvant in the cysticidal s c h e d u l e .
K e t o p r o f e n ( K P ) , a n o n - h o r m o n a l anti-inflammatory agent ( N H A I ) , w a s first u s e d o n l y as an a n a l g e s i c . H o w e v e r , in s o m e patients presenting p l e o c y t o s i s and h e a d a c h e , w e o b s e r v e d , in addition to the d e c r e a s e or disappearance o f h e a d a c h e , a discrete d e c r e a s e in C S F cellularity. In v i e w o f this p o s s i b l e p a s s a g e through the b l o o d brain barrier2 3
, K P is b e i n g a d m i n i s t e r e d as a first-choice drug in the p r e s e n c e o f h e a d a c h e , before manitol, in the p r e s e n c e or a b s e n c e o f c o n c o m i t a n t p l e o c y t o s i s in the C S F , w i t h g o o d results.
R e p l a c e m e n t o f corticosteroids with the routine u s e o f an antihistamine and an N H A I o v e r the last 10 years w a s o n l y unable to prevent the o n s e t o f s i g n s o f s e v e r e and fatal ICH in 3 patients ( C a s e s 1, 2 and 3 ) , all o f them with a previous history o f clinical w o r s e n i n g in the presence o f corticotherapy. In the r e m a i n i n g C a s e s , clinical e x a c e r b a t i o n occurred b e t w e e n the 15 1
and 5 * day o f A B Z u s e and did not last m o r e than 3 d a y s , regressing satisfactorily with the u s e o f KP, a c e t a z o l a m i d e and manitol. A l t h o u g h it is k n o w n3 4
that epileptic s e i z u r e s are better c o n t r o l l e d after the u s e o f A B Z in patients with p a r e n c h y m a t o u s c y s t s , w e n o t e d that in patients with the s e v e r e form o f c y s t i c e r c o s i s this control is e v e n higher during the u s e o f A B Z , s u g g e s t i n g a p o s s i b l e antiepileptic action o f the c y s t i c i d e . H o w e v e r , experimental studies are n e e d e d to c o n f i r m this clinical o b s e r v a t i o n .
T h e study o f the C S F o f these patients w i t h the s e v e r e form o f N C C s u g g e s t s that e l e v a t i o n s a b o v e the statistical m e d i a n o f the p e r c e n t a g e o f e o s i n o p h i l s and p l a s m o c y t e s during and after A B Z
d o e s not o c c u r w h e n these percentages d e c r e a s e or d o not increase during and after the u s e o f t h e c y s t i c i d e . In other w o r d s , the m o r e p r o l o n g e d the i m m u n o a l l e r g i c r e s p o n s e to treatment, the w o r s e the prognosis s e e m s to be. C o n s e q u e n t l y the study o f the C S F in clinical treatment is o f high prognostic value in the e v a l u a t i o n o f the survival o f t h e s e patients.
W e d o not think that c y s t n u m b e r or s i z e is important to d e f i n e the t i m e o f treatment, as s u g g e s t e d in the literature3 3
. T h e l o c a l i z a t i o n and m a i n l y the form o f presentation o f t h e s e c y s t s
s e e m s to better define the therapeutic s c h e d u l e to b e used.
Our o b s e r v a t i o n s o v e r a period o f m o r e than 10 years o f A B Z treatment o f the s e v e r e f o r m o f N C C permits us to s u g g e s t that:
1) the therapeutic c o n d u c t , clinical or surgical, s h o u l d be i n d i v i d u a l i z e d ;
2 ) in the presence o f h y p e r t e n s i v e hydrocephaly, e v e n w i t h o u t clinical s i g n s o f I C H , e v o l u t i o n is better w h e n the patients are submitted to a ventricular C S F shunt i m m e d i a t e l y b e f o r e the s p e c i f i c pharmacological s c h e d u l e ;
3 ) the approach to t h e posterior f o s s a , s p e c i f i c a l l y to the I Vt h
ventricle, is contraindicated after cysticidal treatment;
4 ) the p r e s e n c e , or the s i m p l e s u s p i c i o n , o f p a r e n c h y m a t o u s cysticerci appears to render a little m o r e b e n i g n the clinical c o u r s e o f the patients;
5 ) the s i m p l e p a r e n c h y m a t o u s f o r m s respond w e l l and rapidly to a d o s e o f 15 m g / k g / d a y o f A B Z for a period o f 2 0 - 3 0 d a y s ;
6 ) the multiple r a c e m o s e forms o f ventricular and/or subarachnoid localization s e e m to e v o l v e better w h e n treated w i t h 3 0 m g / k g / d a y o f A B Z for 6 0 d a y s ;
7 ) w h e n the p r e s e n c e o f r a c e m o s e c y s t s o f any l o c a l i z a t i o n or o f s i n g l e c y s t s o f ventricular
localization and m a i n l y in the I Vt h
ventricle is s u s p e c t e d or c o n f i r m e d , the d o s e o f 15 m g / k g / d a y should be a v o i d e d to permit the short- or long-term g r o w t h o f t h e s e c y s t s probably b y s l o w i n g d o w n their d e g e n e r a t i o n p r o c e s s ;
8 ) in the patients studied, the 3 0 m g / k g / d a y d o s e o f A B Z , in c o m b i n a t i o n with D C P and KP, did not c a u s e short- or l o n g - t e r m s i d e effects and m i n i m i z e d the effects o f clinical and laboratory
exacerbation c o m m o n l y occurring during the first w e e k o f cysticidal treatment;
9 ) s i n c e t h e s e are s e v e r e l y ill patients, a m i n i m u m t i m e o f 4 years o f f o l l o w - u p is n e e d e d to reach any c o n c l u s i o n s ;
10) these c a s e s require constant rigorous v i g i l a n c e s i n c e , n o matter h o w small an interfering e v e n t m a y b e , intervention s h o u l d b e as prompt as p o s s i b l e to insure a better e v o l u t i o n .
N o t e - S i n c e February 1 9 9 3 , for the s e v e r e forms o f N C C w e h a v e b e e n u s i n g a s c h e d u l e o f 3 0 m g / k g / d a y A B Z for 3 0 d a y s to not r a c e m o s e forms or 6 0 d a y s to the r a c e m o s e f o r m s , w h e t h e r the c y s t s are o f ventricular, subarachnoid or parenchymal l o c a l i z a t i o n .
Acknowledgments - The authors are grateful to the Discipline of Tropical Diseases, specially in the person of Professor Domingos Alves Meira, M.D., for their collaboration and encouragement that permitted the start and the maintenance of the study on treatment of neurocysticercosis. They are also grateful to Mrs. Elettra Greene for revising the English text.
REFERENCES
1. A g a p e j e v S, M e i r a D A , B a r r a v i e r a B , M a c h a d o J M , P e r e i r a P C M , K a m e g a s a w a A, U e d a A K . Neurocysticercosis: treatment with albendazole and dextrochloropheniramine. Trans R Soc Trop Med H y g 1989; 83:377-383.
2. Agapejev S. Incidence of neurocysticercosis at the University Hospital, Faculty of Medicine of Botucatu, State University of São Paulo (Abstract). Thesis, Ribeirão Preto, 1994. Arq Neuropsiquiatr 1995; 53: 170-171. 3. Andrade AS F°, Galdino G S , Mattos GR, Moreno O A , Ancilon M, Rollemberg JC P . Albendazol e m
neurocisticercose: relato de 5 casos. Rev Bras Neurol 1991; 27:115-120.
5. Camargo-Lima JG. Cisticercose encefálica: aspectos clínicos. Thesis, Escola Paulista de Medicina São Paulo, 1966. 6. Colli B O , Martelli N, Assirati JA Jr, Machado HR, Salvarini CP, Sassoli VP, Forjaz SV. Cysticercosis of the central nervous system: I.Surgical treatment of cerebral cysticercosis - a 23 years experience in the Hospital das Clínicas of Ribeirão Preto Medical School. Arq Neuropsiquiatr 1994; 52:166-186.
7. Correa D, Dalma D, Espinoza B, Plancarte A, Rabiela MT, Madrazo I, Gorodezky C, Flisser A. Heterogeneity of humoral immune components in human cysticercosis. J Parasitol 1985; 7 1 : 535-541.
8. Cruz M, Cruz I, Horton J. Albendazole versus praziquantel in the treatment of cerebral cysticercosis : clinical evaluation. Trans R Soc Trop Med Hyg 1991; 85:244-247.
9. Davis LE, Kornfeld M. Neurocysticercosis: neurologic, pathogenic, diagnosis and therapeutic aspects. Eur Neurol 1991; 31:229-240.
10. Del Brutto OH, Sotelo J. Neurocysticercosis:an update. Rev Infect Dis 1988; 10:1075-1087.
11. Del Brutto OH, Sotelo J. Albendazole therapy for subarachnoid and ventricular cysticercosis. J Neurosurg 1990; 72:816-817.
12. Del Brutto O H , Sotelo J, Aguirre R, Díaz-Calderón E, Alarcón JA . Albendazole therapy for giant subarachnoid cysticerci. Arch Neurol 1992; 49:535-538.
13. Escobedo F, Penagos P, Rodriguez J, Sotelo J. Eficácia de albendazol en el tratamiento médico de la cisticercosis cerebral: estúdio controlado tomográficamente. Invest Méd Internat 1988, 15(Supl): 23-26. 14. Estanol B , Corona T, Abad P. A prognostic classification of cerebral cysticercosis : therapeutic implications.
J Neurol Neurosurg Psychiatry 1986; 49:1131-1134.
15. Flisser A, Perez-Monfort R, Larralde C. The immunology of human and animal cysticercosis : a review. Bull W H O 1979; 57:839-856.
16. Gilman AG, Goodman L S , Rail RW, Murad F. The pharmacological basis of therapeutics.Ed 7. New York: Macmillan 1980: 627-629.
17. Jung H, Hurtado M, Sanchez M, Medina MT, Sotelo J. Plasma and C S F levels of albendazole and praziquantel in patients with neurocysticercosis. Cl Neuropharmacol 1990; 13:559-564.
18. Livramento JA, Machado LR, Spina-França A. Immunology of neurocysticercosis. In Fejerman N, Chamoles NA (eds). New trends in pediatrics neurology. Amsterdam: Elsevier, 1993; 307-312.
19. Lobato R, Lamas E, Portillo JM, Roger R, Esparza J, Rivas JJ, Muñoz MJ. Hydrocephalus in cerebral cysticercosis: pathogenic and therapeutic considerations. J Neurosurg 1981; 55:786-793.
20. Malagón F. Elementos del binomio taeniasis/cisticercosis: una sintesis. In Flisser A, Malagón F (eds). Cisticercosis humana y porcina: su conocimiento e investigación en México. Ciudad de México: Li musa, 1989: 3-6.
2 1 . Moreira EL. Neurocisticercose. Clínica, patologia e tratamento da forma ventricular bloqueante. Thesis,. Faculdade de Medicina de Ribeirão Preto. Ribeirão Preto, 1984.
22. Miller O. Curso de corticoterapia. J Bras Med 1978. (ed esp): 7-11.
2 3 . Netter P, Lapique F, Bannwarth B, Tamisier JN, Thomas P, Royer RJ. Diffusion of intramuscular ketoprofen into the cerebrospinal fluid. Eur J Clin Pharmacol 1985; 29:319-321.
24. Salazar A, Sotelo J, Martinez H, Escobedo F. Differential diagnosis between ventriculitis and fourth ventricle cyst in neurocysticercosis. J Neurosurg 1983; 59:660-663.
2 5 . Sotelo J, Marin C. Hydrocephalus secondary to cysticercotic arachnoiditis, a long-term follow-up review. J Neurosurg 1987; 66:686-689.
26. Sotelo J, Escobedo F, Penagos P. Albendazole vs praziquantel for therapy for neurocysticercosis: a controlled trial. Arch Neurol 1988: 45:532-534.
27. Sotelo J, Del Brutto O H , Penagos P, Torres B, Rodriguez-Carbajal J, Rubio-Donnadieu F. Comparison of therapeutic regimen of anti-cysternal drugs for parenchymal brain cysticercosis. J Neurol 1990; 237:69-72. 2 8 . Spina-França A. Síndrome liquórica da neurocisticercose. Arq Neuropsiquiatr 1961; 19:307-314. 2 9 . Spina França A. Cysticercosis of the central nervous system. In Chopra JS et al (eds). Advances in neurology.
Amsterdam Elsevier, 1990: 283-291.
30. Stepien L, Choróbski J. Cysticercosis cerebri and its operative treatment. Arch Neurol Psychiat 1949; 61:499-527. 3 1 . Takayanagui O M , Jardim E. Therapy for neurocysticercosis. Comparison between albendazole and
praziquantel. Arch Neurol 1992; 49:290-294.
32. Torrealba G, Del Villar S, Tagle P, Arriagada P, Kase C S . Cysticercosis of the central nervous system: clinical and therapeutic considerations. J Neurol Neurosurg Psychiatry 1984; 47:784-790.
3 3 . Vasconcelos D, Cruz-Segura H, Mateos-Gomez H, Zenteno-Alanis G. Selective indications for the use of praziquantel in the treatment of brain cysticercosis. J Neurol Neurosurg Psychiatry 1987; 50:383-388. 34. Vazquez V, Sotelo J. The course of seizures after treatment for cerebral cysticercosis. N Engl J Med 1992;