REVISTA
PAULISTA
DE
PEDIATRIA
www.rpped.com.br
ORIGINAL
ARTICLE
Pediatrician’s
knowledge
on
the
approach
of
functional
constipation
Mario
C.
Vieira
a,b,
Isadora
Carolina
Krueger
Negrelle
a,
Karla
Ulaf
Webber
a,
Marjorie
Gosdal
a,∗,
Sabine
Krüger
Truppel
b,
Solena
Ziemer
Kusma
aaPontifíciaUniversidadeCatólicadoParaná,Curitiba,PR,Brazil
bHospitalPequenoPríncipe,Curitiba,PR,Brazil
Received12February2016;accepted29May2016 Availableonline6September2016
KEYWORDS
Constipation; Pediatrics; Diagnostic; Treatment
Abstract
Objective: Toevaluatethepediatrician’sknowledgeregardingthediagnosticandtherapeutic approachofchildhoodfunctionalconstipation.
Methods: A descriptive cross-sectionalstudy was performedwith theapplication ofa
self-administered questionnaire concerning a hypothetical clinical case ofchildhood functional
constipationwithfecalincontinencetophysicians(n=297)randomlyinterviewedatthe36th BrazilianCongressofPediatricsin2013.
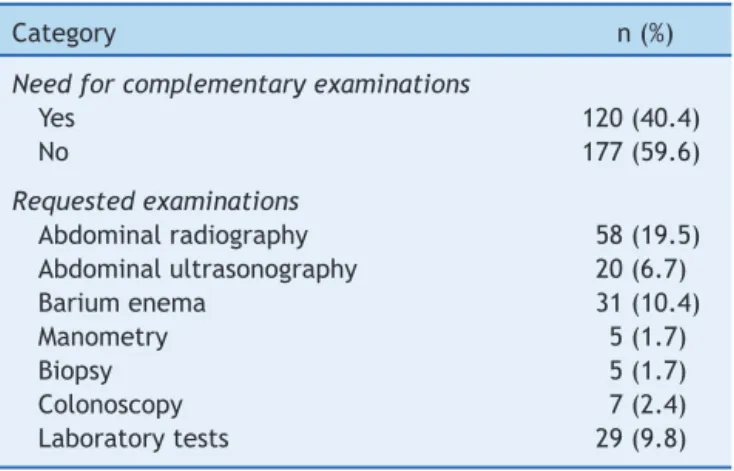
Results: The majorityoftheparticipants werefemales, the meanage was44.1years,the meantimeofprofessionalpracticewas18.8years;56.9%wereBoardCertifiedbytheBrazilian SocietyofPediatrics.Additionaltestswereorderedby40.4%;includingabdominal
radiogra-phy (19.5%), barium enema (10.4%), laboratory tests (9.8%), abdominal ultrasound (6.7%),
colonoscopy(2.4%),manometryandrectalbiopsy(both1.7%).Themostcommoninterventions
includedlactulose(26.6%),mineraloil(17.5%),polyethyleneglycol(14.5%),fibersupplement (9.1%)andmilkofmagnesia(5.4%).Nutritional guidance(84.8%),fecal disimpaction(17.2%) andtoilettraining(19.5%)werealsoindicated.
Conclusions: Ourresultsshowthatpediatriciansdonotadheretocurrentrecommendationsfor
themanagementofchildhoodfunctionalconstipation,asunnecessarytestswereorderedand
thefirst-linetreatmentwasnotprescribed.
©2016SociedadedePediatriadeS˜aoPaulo.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBYlicense(http://creativecommons.org/licenses/by/4.0/).
∗Correspondingauthor.
E-mail:marjorie.gosdal@hotmail.com(M.Gosdal).
http://dx.doi.org/10.1016/j.rppede.2016.06.003
PALAVRAS-CHAVE
Constipac¸ão intestinal; Pediatria; Diagnóstico; Tratamento
Conhecimentodopediatrasobreomanejodaconstipac¸ãointestinalfuncional
Resumo
Objetivo: Identificaroconhecimentodopediatraquantoaomanejodiagnósticoeterapêutico dacrianc¸acomconstipac¸ãointestinalfuncional.
Métodos: Estudo transversal descritivo comamostra constituída de médicos (n=297)
entre-vistados no 36◦ Congresso Brasileiro de Pediatria de 2013. Foi usado um questionário
autoadministradoreferenteaumcasoclínicohipotéticodeconstipac¸ãointestinal.
Resultados: Foiobservadamaiorproporc¸ãodepediatrasdosexofeminino,médiade44,1anos,
tempo de formac¸ão médio de 18,8 anos, 56,9% portadores de título de especialista pela
SociedadeBrasileiradePediatria.Examescomplementaresforamsolicitadospor40,4%,a
radio-grafia abdominalfoi omais requisitado(19,5%), seguidopor enemaopaco (10,4%),exames
laboratoriais(9,8%),ultrassonografia de abdome(6,7%),colonoscopia (2,4%),manometriae
biópsia(ambas1,7%).Paraomanejofoisugeridaaprescric¸ãodelactulose(26,6%),óleo min-eral(17,5%),polietilenoglicol(14,5%),suplementodefibras(9,1%)eleitedemagnésia(5,4%). Orientac¸ãoalimentar(84,8%),desimpactac¸ãofecal(17,2%)etreinamentodetoalete(19,5%)
tambémforamindicadas.
Conclusões: Evidencia-seumadiscordânciaentreomanejosugeridopelospediatrasea con-dutapreconizadapelaliteraturadisponívelatualmente,umavezqueforamsolicitadosexames
complementaresdesnecessáriosenãofoirecomendadaaorientac¸ãoterapêuticaconsiderada
deprimeiralinha.
©2016SociedadedePediatriadeS˜aoPaulo.PublicadoporElsevierEditoraLtda.Este ´eum artigoOpenAccesssobumalicenc¸aCCBY(http://creativecommons.org/licenses/by/4.0/).
Introduction
In clinical practice,intestinal constipation is a very com-monfindinginchildren,correspondingtoapproximately3% ofconsultationsingeneralpediatricoutpatientclinicsand 25%ofconsultationsinpediatricgastroenterology.1---4When
assessingthestudiesinBrazil,avariationof14.7---38.8%was
foundintheprevalenceofconstipation.5Thiswidevariation
isdueboth totheheterogeneityof thediagnosticcriteria
andthedifferencesinstudypopulationselection.5,6
TheRomeIIICriteria(2006)statesthatinchildrenolder
than 4 years, the diagnosis of constipation is established
when thereare ≤2 bowel movements per week; at least
oneepisodeoffecalincontinenceperweek;historyof
reten-tivepostureorexcessivevoluntarystoolretention;historyof
painfulbowelmovements;presenceofalargefecalmassin
therectalcanal;historyoflarge-caliberstoolsthatcanclog
thetoiletbowl.Thesymptomsmustbepresentatleastonce
aweekfora two-monthinterval.4However,thesecriteria
areconsidered by some experts as very restrictive.5 The
European Society of Pediatric Gastroenterology,
Hepatol-ogyand Nutrition (ESPGHAN) and North-American Society
of Pediatric Gastroenterology, Hepatology and Nutrition
(NASPGHAN)guidelinesrecommendusingtheRomeIII
crite-ria,exceptforsymptomduration,sincetherecommended
intervaloftwomonthscancontributetotreatmentdelayin
olderchildren.7
Thehighprevalenceofconstipationgenerateshighcosts
topublichealth,representinganexpenseofUS$3362per
childtreated annuallyin theUnitedStates.6 Studies have
shownthat thereis nopredominance of gender andin at
leasthalfofthecasesconstipationoccursinthefirstyear
of life, even if it is more often diagnosed in school age
children.1,3
Complications associated with constipation include
recurrentabdominalpain,fecalincontinence,rectal
bleed-ing, enuresis and urinary infection/retention.6 These
aggravatingfactors mayprogressivelyassociate and
nega-tivelyinfluencethequalityoflife,generatingcostsforboth
thefamilyandthegovernment.2,3
Althoughitisadiseasewitharelativelysimplediagnosis
andtreatment,constipationaffectsthechild’sphysicaland
emotional integrity.1 Taking intoaccount the prevalence,
clinical significance and impactof the disease, this study
aimstooutlineamanagementpanoramaadoptedby
Brazil-ianpediatricianswhen treatingacaseof constipationand
establishaparallelwiththeavailableliterature.
Method
Thiswasacross-sectional,descriptivestudy,withasample of297physicianschosenbynonrandomconvenience samp-ling,participatingin36thBrazilianCongressofPediatrics,in Curitiba,stateofParaná,inOctober2013.Thecongress par-ticipantswereapproachedbyindividualresearchersduring theintervalsofscientificactivitiesandinvitedtoparticipate andanswerthequestionnaire.
The study was approved by the Institutional Review Board of Pontifícia Universidade Católica do Paraná and written consent was obtained from all respondents. The study included pediatricians, general practitioners with a Specialist title in Pediatrics by the Brazilian Society of Pediatrics(SBP)andmedicalresidentsinPediatrics.A self-administeredquestionnaireconsistingoftwopartswasused astheresearchtool.
drawingtherespondent’s medicalprofile,by gender, age, origin,timesincegraduation,extendededucationandplace ofwork.
The second part of the questionnaire reported to the followingfictitiousclinicalcase: ‘‘J.L.C.,malegender, six yearsold,hasonebowelmovementeverythreeorfourdays, drystools,painandeffortatevacuation.Hesoilshisclothes threetofourtimesaweek.Onphysicalexamination:height 118cm and weight, 21.4kg. He shows palpable hardened fecesintheleftiliacfossainmoderatequantity.Nomore details’’.Thisstepcontaineddiscursiveopenquestions con-cerningthediagnosisandinitialclinicalmanagement,which were:I.Whatisthemostprobablediagnosisfor thiscase? II. Whatarethecriteriausedfor thisdiagnosis?III. Would youindicateanyfurtherexaminations?Ifso,whichones?IV. Whatwouldbethetherapeuticmanagementofthispatient? Ifyouchoose medication,whichwouldbethedrugandat whatdose? Atotalof412questionnairesweredistributed, of which346 were answered.Of these,49 questionnaires wereexcluded,astheywereincompleteorillegible.
The Rome III criteria (2006) were considered for the diagnosisoffunctionalconstipation.Theanswersobtained fromthe questionnaireswere transcribed and stored in a Microsoft Excel® 2010 spreadsheet. Mean, median,
mini-mum,maximumandstandarddeviationvalueswereusedto describequantitativevariables.Qualitativevariableswere described asfrequenciesandpercentages. The chi-square test or Fisher’sexact test wasusedtoevaluate the asso-ciationbetweentheparticipants’profilevariablesandthe prescription/indication variables.Pvalues<0.05were con-sidered statistically significant. Datawere analyzed using theIBMSPSSsoftwarev.20.0.
Results
A total of 297 questionnaires were included. Among the interviewedpopulation,therewasaslightpredominanceof females(58.9%).Themeanagewas44.1years(23---75)and the meannumber of the yearssince graduationwas 18.8 (0---52).Themajorityofrespondentscamefromthe South-eastregion(45.5%),followedbytheSouth(26.3%),Central West (8.4%), Northeast (12.1%) and North (7.7%) regions. Mostof theintervieweddoctors(60.9%) hada Board Cer-tificationtitleby theBrazilianSociety ofPediatrics(SBP), whiletherestconsistedofpediatricianswithoutboard certi-ficationandpediatricresidents.Ofthetotal,89doctorshad adegreeinthepediatricarea,ofwhichseven(2.4%)were pediatric gastroenterologists. General information about thestudypopulationisdetailedinTable1.
Thediagnosisofconstipationwasidentifiedby93.6%of
respondents.Complementarytestswereindicatedby40.4%,
with plain abdominal radiography being the most often
requested test(19.5%). Bariumenema (10.4%),abdominal
ultrasonography(6.7%), anorectal manometry (1.7%),
rec-tal biopsy (1.7%),colonoscopy (2.4%)and laboratory tests
(9.8%)werealsomentioned(Table2).
As for the management proposed by the respondents,
itis noteworthythat84.8% wouldmakerecommendations
relatedtothepatient’seatinghabits.Regardingother
non-pharmacological measures, they also mentioned the use
of additional fiber (9.1%) and toilet training (19.5%). A
Table1 Characteristicsofrespondents(n=297).
Variables Description n(%)
Gender Female 175(58.9)
Male 122(41.1)
Timesince graduation
Mean 18.8years
Region North 23(7.7)
Northeast 36(12.1)
Midwest 25(8.4)
Southeast 135(45.5)
South 78(26.3)
Educational back-ground
Residencyin PediatricswithBCPa
170(57.2)
Residencyin Pediatricswithout BCPa
64(21.6)
ResidentPhysician (1styear)
27(9.1)
ResidentPhysician (2ndyear)
25(8.4)
GeneralPractitioner andBCPa
11(3.7)
Pediatric spe-cialty
Gastroenterology 7(2.4) Others 82(27.6)
No 208(70.0)
a BCP,BoardCertificationinPediatricsgrantedbytheBrazilian
SocietyofPediatrics/BrazilianMedicalAssociation.
pharmacological approach was recommended by 64% of respondents and included the use of lactulose (26.6%), mineraloil(17.5%),polyethyleneglycol(PEG)(14.5%)and magnesiumhydroxide(5.4%).Noneoftheresponses recom-mendedtheuseofmorethanonelaxativesimultaneously. Fecal disimpaction was suggested by 17.2% of the inter-viewedphysicians(Table3).
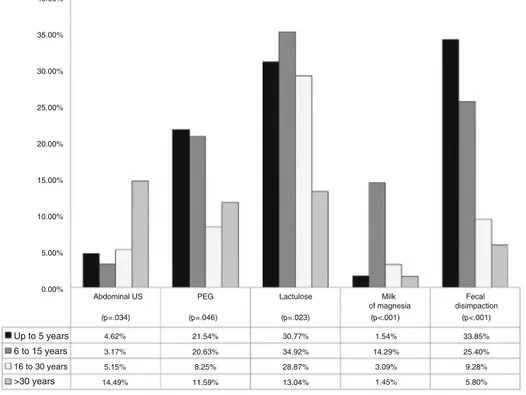
An association was identified between the time since
graduationandcertainconductsinthediagnosticand
ther-apeuticmanagement(Fig.1).Amongthedoctorsthathad
graduatedlessthansixyearsbefore,4.6%wouldrequestan
abdominalultrasound.Incontrast,14.4%ofthosethathad
Table2 Diagnosticmethodsproposedbyrespondents.
Category n(%)
Needforcomplementaryexaminations
Yes 120(40.4)
No 177(59.6)
Requestedexaminations
Abdominalradiography 58(19.5)
Abdominalultrasonography 20(6.7)
Bariumenema 31(10.4)
Manometry 5(1.7)
Biopsy 5(1.7)
Colonoscopy 7(2.4)
Table 3 Therapeutic management proposed by respondents.
Suggestedtreatment n(%)
Fecaldisimpaction 51(17.2)
Polyethyleneglycol 43(14.5)
Lactulose 79(26.6)
Mineraloil 52(17.5)
Magnesiumhydroxide 16(5.4)
Fibersupplement 27(9.1)
Nutritionalguidance 252(84.8)
Toilettraining 58(19.5)
graduated morethan 30 years beforewould dothe same (p=0.034).
Regarding the use of polyethylene glycol, it was indi-catedby21.5%ofdoctorsthathadgraduatedlessthansix yearsbeforeand20.6%ofthosegraduatedbetween6and 15 years before,with a lower percentage of prescription among the ones that had graduated more than 15 years before(p=0.046).
Approximately 30% of each group of respondents with timesincegraduationless than30yearsprescribed lactu-lose. Respondents that had graduated between 6 and 15 yearsprescribedmagnesiumhydroxideatahigher percent-age (14.3%) when compared to the other groups of time sincegraduation.This drugwasprescribedby1.4%of pro-fessionalsthat hadgraduated morethan 30 yearsbefore, by 1.5% among those with less than 5 years since grad-uation and 3.1% among those that had graduated 16---30 yearsbefore(p<0.001).Amongthosethathadgraduatedless than6yearsbefore,33.9%indicatedfecaldisimpaction,as 25.4%ofthosegraduated6---15yearsbefore;9.3%ofthose
graduated 16---30years beforeand5.8% ofthosethat had graduatedmorethan30yearsbefore(p<0.001).
Discussion
There can be several etiologies for constipation. Func-tional constipation is the most common, in which the most important originating factor seems to be voluntary fecal retention.2,4 Organic causes of constipation include
metabolicdisorders(hypothyroidism,cysticfibrosis,
hyper-calcemia and hypocalcemia), neuropathic (Hirschsprung’s
disease, myelomeningocele, spina bifida, cerebral palsy)
andimmunologicaldiseases(allergytocow’s milkprotein,
celiacdisease),aswell asthe useof medicationssuchas
ironsalts,antacids,anti-inflammatorydrugsandopioids.3,5
TheRomeIIICriteria(2006)istheonemostoftenusedto
determine constipationinchildhood.1,7---9 Inthe
aforemen-tionedclinicalcase,symptomdurationwasnotstated(if>2
months), a factor that can be considered a study
limita-tion.The ESPGHAN andNASPGHAN guidelinesrecommend
thattheRomeIIIcriteriabeusedtodefinethepresenceof
constipation,exceptforsymptomduration,consideringthat
thetwo-monthintervalrecommendedforolderchildrencan
contributetotreatmentdelay.7
The practical guide proposed by National Institute for
HealthandClinicalExcellence(NICE)statesthatadetailed
historyandathoroughphysicalabdominalexaminationare
enoughtoattainthediagnosis.10Thisisalsothefinal
conclu-sionoftheguidelinesproposedbyESPGHANandNASPGHAN,
suggesting thatthe diagnosisis primarily clinical andthat
complementary tests are not necessary to confirm the
disease.7 Nevertheless, 40.4% of the respondents deemed
necessarytorequestadditionaltests.
40.00%
35.00%
30.00%
25.00%
20.00%
15.00%
10.00%
5.00%
0.00%
Abdominal US PEG Milk
of magnesia
Lactulose Fecal
disimpaction (p=.034)
4.62% 3.17% 5.15% 14.49%
21.54% 20.63% 8.25% 11.59%
30.77% 34.92% 28.87% 13.04%
1.54% 14.29% 3.09% 1.45%
33.85% 25.40% 9.28% 5.80% (p=.046) (p=.023) (p<.001) (p<.001)
Up to 5 years 6 to 15 years
16 to 30 years
>30 years
A plain abdominal radiography may be useful to char-acterize fecal impaction in children and to evaluate the effectiveness of the initial treatment.11 However,despite
beingrequestedby58 physicians(19.5%),itis not
consid-ered necessary to attain a final diagnosis, as thereis no
association betweenthepresence ofsuggestive symptoms
and the accumulation of stool in the rectum.8 It is
note-worthythat therearenostudies associating theneed for
abdominalradiographywhenthepatientdoesnotmeetthe
clinicalcriteriaforconstipation.7,11,12
Abdominalultrasoundwasanotherveryoften-indicated
test. Twenty professionals (6.7%) found it necessary to
requestthisexaminationtoconfirmthediagnosis.Inspiteof
beingseen asasimple,noninvasivemethodfor evaluation
offecalretentionandmeasurementofthetransverserectal
diameter,itisnotconsideredanessentialexamination.1,7,13
Todate,thereisnotenough evidenceestablishingthatan
alterationinrectaldiametercanbeusedasapredictorfor
thepresenceofconstipationinchildren.11,14
The barium enema was indicated by 10.4% of
respon-dents.Accordingtotheliterature,thisis oneofthemain
testsusedtoruleoutthemostimportantdifferential
diag-nosisforfunctionalconstipationinchildren,Hirschsprung’s
disease.15,16However,thistestisnotrequiredforthefinal
diagnosis,unlessthechildhassuggestivesigns,suchasan
earlyonsetof constipation,delayedpassageof meconium
andsignificantabdominaldistension.7,15
The sameis truefor anorectalmanometry (ARM),
indi-catedbyfiveoftheinterviewedphysicians(1.7%).Thistest
also aimsto rule out Hirschsprung’s disease by disclosing
alterationsintheanorectalinhibitoryreflex.17---20However,
itisnoteworthythattheexaminationisnotessentialforthe
diagnosis,especiallyinchildrenaftertheneonatalperiod.7
Aswiththebariumenema, ARMshouldonlybeperformed
ifthereare datasuggestive ofHirschsprung’s disease and
inseverecasesrefractorytoadequatetreatment.7,17,20The
rectalbiopsyisconsideredthegoldstandardforthe
diagno-sisofHirschsprung’sdiseaseandshouldonlybeperformed
when the tests discussed above suggest itspresence.12 It
should not be performed at the patient’s initial
consul-tation, unlike what was proposed by seven professionals
interviewedinthisstudy(2.4%).7
Colonoscopy wasanotherexaminationsuggestedbythe
interviewedphysicians(1.7%).Aswiththeanalysisofcolonic
transit,thecolonoscopyshouldnotbeindicatedattheinitial consultations.7
Finally,laboratory testswererequestedby29
pediatri-cians (9.8%). Such tests may be indicated when there is
diagnosticuncertainty (patientdoes notmeet theclinical
criteria),orwhenthereisstrongsuspicionofanunderlying
organic disease, such ashypothyroidism, allergy tocow’s
milk proteinand celiacdisease and not for patients with
aclear pictureof functionalconstipation, asinthisstudy
case.1,7,10,15
Thehypothesisoffunctionalconstipation2shouldprevail
inthemanagementofthechildwithconstipation,ifthere
are no data in clinical history and physical examination
suggesting asecondary cause.Traditionally,the
therapeu-tic management consists of four steps, including general
recommendations and education, disimpactionwhen
nec-essary, re-impaction prevention and retraining of bowel
habits.4Whentransmittingthegeneralrecommendations,it
isimportanttoestablishacooperativerelationshipbetween
thephysicianandthefamily,includingthepatients,when
their age allows it.2,7,21 The basic understanding of the
pathophysiologyinvolvedhelpstoeasefamilytensionsand
feelingsofinsecurityorguilt.2,21
A balanced diet, including the consumption of whole
grains, fruits and vegetables, together with an adequate
waterintake,isrecommendedaspartofthemaintenance
treatmentforconstipationinchildren.4Amongthe
respon-dents,84.8%suggested sometypeof nutritionalguidance.
There are conflicting reports in the literature about the
roleoffiberintakeinchildrenwithconstipation.However,
supplementationwithsolublefiber, considered by9.1% of
thepediatricians,hasnotshownsufficientefficacyandits
useisnotindicated.4,7
The toilettraining goalshouldbe toretrain thebowel
habits.2,4 Thechild shouldbeadvised toremainsittingon
the toilet bowl for 5---10min after the main meals, in an
adequate position for the abdominal press, while using a
footrest.1,4Amongtheinterviewedphysicians,19.5%made
recommendationsaboutpatienttoilettraining.
The elimination of the fecaloma through fecal
disim-pactionshouldbeperformedwhenthepresenceofamass
isidentifiedduringabdominalpalpation,rectalexamination
orplain abdominalradiography.4 The disimpactioncanbe
madewithenemasorlaxatives,suchaspolyethyleneglycol
(PEG), with both being of similar efficacy.22 As the
pro-posedclinicalcase showedevidenceof fecalretention on
thephysicalexamination,fecaldisimpactionwouldbe
indi-cated.However,theprocedurewasconsideredbyonly17.2%
ofthepediatricians.Noneoftherespondentsspecifiedthe
typeoffecal disimpaction(orally or byenema). Itshould
be noted that the disimpaction before the maintenance
therapyisrecommendedtoincreasetreatmentsuccessand
reducetheriskoffecalincontinence.1,4,18 Oncethe
disim-paction is performed, the focus of the treatment should
be recurrence prevention with the use of maintenance
medications.1,21
The pharmacological approach was recommended by
64% of respondents. Among the drugs used totreat
con-stipation,polyethylene glycol (PEG) is the most effective
when comparedto lactulose, magnesium hydroxide,
min-eraloilor placebo.7PEGis acompoundofhighmolecular
weight,poorlyabsorbedbythebodyandnotmetabolizedby
intestinalbacteria.17,23 It exertsan osmotic,non-irritating
action, withconsequentincrease in the water contentof
stools.17,23 Itshouldbeconsideredasthefirst-line
mainte-nancetreatment ofintestinalconstipation.7,23 However,it
wasprescribed by only 14.5% of the respondents. A
con-siderablyhighernumberofpediatricians(26.6%)indicated
theuseoflactulose.Several studiescomparingtheuseof
PEGandlactulose suggestedthe superiorityof PEG
treat-ment,highersuccessratesinthetreatmentandprevention
offecalimpactionrecurrence,greaterreliefof abdominal
painandfewersideeffects.24---27Themaintenancetreatment
withlactuloseisrecommendedwhenPEGisnotavailable.7
Therefore,aninversionintheprescriptionratesofPEGand
lactulosecan beobserved inthe availableliterature. The
prescriptionofmagnesiumhydroxide,consideredby5.4%of
pediatriciansandofmineraloil,prescribedby17.5%,should
beusedasadjunctivetherapyorsecond-linetreatmentof
Early adequate treatment of constipation is
essen-tialto preventcomplications, suchasfecal incontinence,
describedinourcase. Whenanalyzing theconductstaken
bytherespondents,oneshouldconsiderthelocationwhere
each professionalworks,taking into accountpossible
dif-ferences in the availability of resources, both diagnostic
andtherapeutic.Some statisticallysignificantassociations
(p<0.05) were observed between the respondent’s profile
andsome of the approaches used.The professionals that
hadgraduatedmorethan30yearsbeforeweremorelikely
to request an abdominal ultrasound; 14.5% of this group
requested this test, considered unnecessary for the
dis-ease diagnosis. In contrast,this same group wasthe one
that showed the least number of lactulose prescriptions
in patient management: only 13.4% chose this drug,
ver-sus 34.9% of professionals that had graduated6---15 years
before(Fig.1).Polyethyleneglycolandfecaldisimpaction,
consideredthefirstchoiceforthepatientpresentedinthe
study, were more often indicated by physicians that had
lesstimesincegraduation.1,2InrelationtoPEG,itwas
pre-scribedby21.5%ofphysiciansthathadgraduatedlessthan
sixyearsbeforeand20.6%ofphysiciansthathadgraduated
6---15 yearsbefore.As for fecaldisimpaction, it was
indi-catedby33.8%oftheonesthathadgraduatedlessthansix
yearsbeforeand25.4%ofthosegraduated6---15yearsbefore
(Fig.1).Doctorsthathadgraduatedbetween6and15years
beforewere the ones that most often prescribed
magne-siumhydroxide(14.3%),which isconsidered asecond-line
or adjunctivetherapy drug(Fig.1).These results
demon-stratethegreatdisparityinthetypeofmanagementusedby
physicianswithlongertimesincegraduationandthosewith
lesstime,whichreinforcestheneedforconstantupdating
byhealthprofessionals.
Recent studies, published after data collection was
finished for this study, showed differences in behaviors
proposedbygeneralpractitioners, pediatriciansand
pedi-atric gastroenterologists.28,29 A study carried out in Saudi
Arabia, which used a questionnaire with questions about
practicalanddemographiccharacteristics,definition,
man-agement and treatment of constipation, showed that
pediatricians more often prescribed the use of lactulose
and indicated fecal disimpaction when compared to
gen-eral practitioners.28 A national study performed in 2009
withphysicians inthe state of Minas Gerais, showedthat
72.6%ofpediatricgastroenterologistsrequestedadditional
tests,whencomparedwith27.5%oftheotherinterviewed
physicians.29 The study alsodisclosedthatthe mostoften
recommendeddrugs bynon-gastroenterologists were
min-eral oil (72.6%), magnesium hydroxide (52.1%), lactulose
(41%)andPEG(25.2%).Amongthepediatric
gastroenterolo-gists,themostoftenrecommendeddrugsweremagnesium
hydroxide (91.7%), PEG (91.7%) and mineral oil (58.3%).
These studies included the administration of a
question-naireonconstipation,incomparisonwiththepresentstudy,
which used an open clinical case as part of the research
tool.
Thelimitationsofthepresentstudyincludethefactthat
itisacross-sectionalone,thatitidentifiedthephysician’s
circumstantialidea inrelation toa specific case, andthe
inclusionof physicians whowere pediatric residents. One
shouldalso considerthat the selection of respondents by
conveniencehastheadvantageofevaluatinganaccessible
population,butresultsintheincapacitytomakestatements
that can be strictly generalizable. The results obtained
mightdepictagoodimageoftheconductsuggestedbythe
pediatricians;however, itis notpossible touse statistical
toolstomeasuretheaccuracyofresults.
Despitetheabovementionedlimitations,theinadequacy
in diagnosticand therapeuticproceduresdemonstrated in
this study highlights the need for continuing education
programs in order to update pediatricians regarding the
managementofintestinalconstipation.Themistakesmade
indiagnosticmanagementsubjectthepatientto
unneces-sary tests, which are often invasive and do not influence
the recommendedapproach. The useof therapies
consid-eredassecond-lineonesasthefirsttreatmentoptionmay
resultintreatmentfailureorrefractorydisease.Treatment
delaysandinadequatetreatmentsmayresultintheonset
ofcomplications,negatively influencingthechild’squality
oflifeandgeneratecostsforboththefamilyandthehealth
system.
Funding
Thisstudydidnotreceivefunding.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Tabbers MM, Boluyt N, Berger MY, Benninga MA. Clinical practice:diagnosis andtreatmentoffunctional constipation. EurJPediatr.2011;170:955---63.
2.Morais MB, Maffei HV. Constipation. J Pediatr (Rio J). 2000;76:S147---56.
3.WaliaR,MulhearnN,KhanR,CuffariC.Chronicconstipationin children:anoverview.PractGastroenterol.2013;17:19---34.
4.ConstipationGuidelineCommitteeoftheNorthAmerican Soci-etyforPediatricGastroenterology,HepatologyandNutrition. Evaluationandtreatmentofconstipationininfantsand chil-dren: recommendations of the North American Society for PediatricGastroenterology,HepatologyandNutrition.JPediatr GastroenterolNutr.2006;43:e1---13.
5.MottaME, SilvaGA.Constipac¸ãocrônica.In:Lopez FA, Cam-posJúniorD,editors.Tratadodepediatria.SãoPaulo:Manole; 2010.p.983---93.
6.vandenBergMM,BenningaMA,DiLorenzoC.Epidemiologyof childhoodconstipation: asystematic review.AmJ Gastroen-terol.2006;101:2401---9.
7.TabbersMM,DiLorenzoC,BergerMY,FaureC,LangendamMW, NurkoS,etal.Evaluationandtreatmentoffunctional constipa-tionininfantsandchildren:evidence-basedrecommendations fromESPGHAN and NASPGHAN.JPediatrGastroenterolNutr. 2014;58:265---81.
8.BergerMY,TabbersMM,KurverMJ,BoluytN,BenningaMA.Value ofabdominalradiography,colonictransittime,andrectal ultra-soundscanning inthediagnosis of idiopathicconstipation in children:asystematicreview.JPediatr.2012;161:44---50.
10.Bardisa-EzcurraL,UllmanR,GordonJ.Diagnosisand manage-mentofidiopathic childhood constipation: summary ofNICE guidance.BMJ.2010;340:c2585.
11.BergerMY,TabbersMM,KurverMJ,BoluytN,BenningaMA.Value ofabdominalradiography,colonictransittime,andrectal ultra-soundscanning inthediagnosis ofidiopathic constipation in children:asystematicreview.JPediatr.2012;161:44---50,e1---2.
12.AfzalNA,TigheMP,ThomsonMA.Constipationinchildren.Ital JPediatr.2011;37:1---10.
13.Bijo´sA,Czerwionka-SzaflarskaM,MazurA,RomanczukW.The usefulnessofultrasoundexaminationofthebowelasamethod ofassessmentoffunctional chronic constipationinchildren. PediatrRadiol.2008;37:1247---52.
14.TabbersMM(Thesis)Evidence-basedguidelinedevelopmentin paediatricgastroenterology.Amsterdam:Universityof Amster-dam;2010.
15.BigélliRH,FernandesMI,GalvãoLC.Constipationinchildren. Medicina(Mex).2004;37:65---75.
16.EsayiasW,HawazY,DejeneB,ErgeteW.Bariumenemawith referencetorectalbiopsyfor thediagnosisand exclusionof Hirschsprungdisease.EastCentAfrJSurg.2013;18:141---5.
17.BenningaMA,VoskuijlWP,TaminiauJA.Childhoodconstipation: istherenewlightinthetunnel?JPediatrGastroenterolNutr. 2004;39:448---64.
18.Rajindrajith S, Devanarayana NM. Constipation in children: novelinsightintoepidemiology,pathophysiology,and manage-ment.JNeurogastroenterolMotil.2011;17:35---47.
19.PensabeneL, YoussefNN,GriffithsJM,DiLorenzo C.Colonic manometryinchildrenwithdefecatorydisorders.Rolein diag-nosisandmanagement.AmJGastroenterol.2003;98:1052---7.
20.NovielloC,CobellisG,PapparellaA,AmiciG,MartinoA.Role ofanorectalmanometryinchildrenwithsevereconstipation. ColorectalDis.2009;11:480---4.
21.PlunkettA,PhillipsCP,BeattieRM.Managementofchronic func-tionalconstipationinchildhood.PediatrDrugs.2007;9:33---46.
22.BekkaliNL,vandenBergMM,DijkgraafMG,vanWijkMP,Bongers ME,LiemO,etal.Rectalfecalimpactiontreatmentinchildhood constipation: enemasversushigh doses oralPEG.Pediatrics. 2009;124:e1108---15.
23.GomesPB,MeloMC,DuarteMA,TorresMR,XavierAT. Polyeth-yleneglycolinthetreatmentofchronicfunctionalconstipation inchildren.RevPaulPediatr.2011;29:245---50.
24.Lee-Robichaud H,ThomasK, Morgan J,Nelson RL.Lactulose versuspolyethyleneglycolforchronicconstipation.Cochrane DatabaseSystRev.2010;7:CD007570.
25.TackJ,Müller-LissnerS,StanghelliniV,BoeckxstaensG,Kamm MA,SimrenM,etal.Diagnosisandtreatmentofchronic con-stipation---anEuropeanperspective.NeurogastroenterolMotil. 2011;23:697---710.
26.CandyDC,EdwardsD,GeraintM.Treatmentoffaecalimpaction withpolyetheleneglycolpluselectrolytes(PGE+E)followedby adouble-blindcomparisonofPEG+Eversuslactuloseas main-tenancetherapy.JPediatrGastroenterolNutr.2006;43:65---70.
27.VoskuijlW,deLorijnF,VerwijsW,HogemanP,HeijmansJ,Mäkel W,etal.PEG3350(Transipeg)versuslactuloseinthetreatment of childhood functional constipation: a double blind, ran-domised,controlled,multicentretrial.Gut.2004;53:1590---4.
28.Hasosah M,Telmesani A, Al-BinaliA, SarkhiA, AlgnhamdiS, Alquair K,et al.Knowledgeand practicesstyles of pediatri-ciansinSaudiArabiaregardingchildhoodconstipation.JPediatr GastroenterolNutr.2013;57:85---92.