Efectiveness of post-pyloric tube placement using
magnetic guidance
Efetividade da sondagem pós-pilórica usando guia magnético
intrODUctiOn
Appropriate nutritional support is important to the outcomes of critically ill patients.(1) Early enteral feeding is beneicial and is recommended by important guidelines.(1-4) However, it is recognized that up to 60% of patients receiving an enteral diet are not able to achieve their scheduled energy values.(5) his is perhaps due to the signiicant portion of severely ill patients with intestinal motility issues, which lead to increased gastric residual volumes.(6)
Enteral post-pyloric diet administration has been suggested as an option to improve feeding tolerance, with lower associated aspiration and pneumonia rates.(3,7) However, there are serious complications related to the placement of this device, which are associated with higher costs and longer times and can delay the start of the diet infusion.(8-10)
Renata Andrea Pietro Pereira Viana1, Ederlon Rezende1, Maria Aparecida Oliveira Batista¹, Carla Marta da Silva¹, Miguel Costa Ribeiro Neto¹, Tatiane Akemi Setoyama¹, João Manoel Silva Junior1, Amanda Maria Ribas Rosa de Oliveira1
1. Service of Intensive Care Medicine of Hospital do Servidor Público Estadual “Francisco Morato de Oliveira” – HSPE-FMO - São Paulo (SP), Brazil.
aBStract
Objective: Appropriate nutritional support is important to the outcomes of critically ill patients. However, a signii-cant portion of these patients experience intestinal motility problems. Adminis-tration of enteral nutrition by means of tubes placed in the post-pyloric position has been suggested to improve the nu-trition tolerance. he aim of this study was to compare the rate of successful post-pyloric placement using a real-time electromagnetic positioning device to the success rate using the conventional placement method.
Methods: his was a prospective,
randomized and controlled study, con-ducted in a tertiary hospital over a pe-riod of three months. he patients were randomized to one of two groups: elec-tromagnetically guided system group, whose patients underwent real-time monitoring of post-pyloric tube place-ment; or the control group, whose pa-tients underwent tube placment using
to the conventional blinded technique. he rates of successful post-pyloric placement and the procedure times were assessed and compared between the groups.
results: hirty-seven patients were enrolled, 18 in the electromagnetic group and 19 in the control group. he inal tube position was evaluated using radiography. he electromagnetic guided group showed better success rates and shorter procedure times when compared to the control group. Additionally, in the electromagnetic guided group, higher pH values were found in the luids aspirated from the probe, suggesting successful post-pyloric placement.
conclusion: he
electromagneti-cally guided method provided better placement accuracy than did the con-ventional technique.
Keywords: Nutrition therapy;
Enteral nutrition/instrumentation; Enteral nutrition/methods; Intubation, gastrointestinal
his study was developed by the Service of Intensive Care Medicine of the Hospital do Servidor Público Estadual “Francisco Morato de Oliveira” – HSPE-FMO - São Paulo (SP), Brazil.
conlicts of interest: he study device and electromagnetic tubes were donated by the manufacturer (VIASYS MedSystems).
Submitted on March 3, 2011 Accepted on April 4, 2011
corresponding author:
Renata Andrea Pietro Pereira Viana Rua Pedro de Toledo, 1800 - 6º andar – Vila Clementino
Zip Code: 04039-901 - São Paulo (SP), Brazil.
Several techniques have been described for post-pyloric tube placement. Endoscopy and luoroscopy have high success rates, but are limited by cost, availability and the need for transferring the patient out of the intensive care unit (ICU). herefore, Heyland et al. recommeds routine post-pyloric diet infusion only in institutions where it can be conveniently and quickly achieved.(11)
his scenario provides a rationale for the evaluation of safe and cost-efective bedside post-pyloric tube place-ment techniques. Recently, a new technique was develo-ped to ease the insertion of nasoenteral tubes; it utilizes an electromagnetic device in the tip of the tube that transmits the path of the tube to a monitor screen (Figure 1).
Figure 1 - a - Post-placement abdominal x-ray; B - Screenshot example of an electromagnetically guided tube.
he objective of the present study is, thus, to evaluate the success rate of post-pyloric placement using a technique that follows the probe’s path using real-time electromagnetic positioning compared to the traditionally used method.
MEtHODS
his was a prospective, randomized and controlled trial that was conducted in a general ICU of a tertiary hospital. he monitoring device used in this study and the electromagnetic tip tubes were donated by the manufacturer (VIASYS MedSystems™). he manufacturer had no participation in this study design and/or analysis. Prior to the study, approval from the Institutional Ethics Committee was granted, and informed consent was signed by each patient or by the patient’s legal representative.
he procedures were performed from September 1, 2008 to December 31, 2008. Inclusion criteria were age greater than 18 years old and at least one of the follow-ing criteria: requirement of a nasoenteral tube for enteral diet administration, indication for post-pyloric
positio-ning, evidence of delayed gastric emptying, aspiration of large amounts of gastric content, repeated gastric aspirations, history of pulmonary aspiration of gastric contents, high-risk status, and severe acute pulmonary disease (Figure 2).
352 ICU admissions
37 Patients randomized 140 Eligible patients
(EN required)
103 Patients excluded: 63 Excluded by the assisting physician
39 Did not sign consent 1 Severe thrombocytopenia
19 Conventional
grup 18 in the EM group
ICU – intensive care unit; EN – enteral nutrition; EM – electromag-netically guided
Figure 2- Patient inclusion lowchart.
Exclusion criteria were active gastrointestinal bleeding, history of esophageal or gastric varices, severe thrombocytopenia (<50,000), recent esophageal or stomach surgery, pharyngeal or laryngeal obstruction, psychomotor agitation, contraindications for >30º angle of the head of the bed, head or face trauma, and requirement of non-invasive mechanic ventilation (Figure 2).
Twenty-ive patients were required for each group, considering a 5% alpha error, calculated for an 80% power assuming success rates of 55% and 20% for the intervention and control groups, respectively. How-ever, due to shortness of device supplies, the study was stopped early.
Patients meeting the inclusion criteria were randomized by means of envelopes, with the group names distributed at a 1:1 rate. he two groups were the electromagnetically guided (EM) group, in which the patients underwent tube placement under real-time monitoring of the probe’s tip via magnetic transmission (CortrakTM), and the control group, in which the conventional blinded nasoenteral tube placement technique was used.
equip-ment including a mask, procedure gloves and protective goggles were donned. he tip of the tube was positioned by the tip of nose and mouth and was measured to the earlobe and then to the xiphoid process. Following injec-tion of mineral water into the tube for lubricainjec-tion pur-poses and application of nostril and tube tip lubrication with lidocaine gel, the tube was slowly introduced. After approximately 10 cm of introduction, the patient was asked to lex the neck and make swallowing movements to facilitate the introduction. he remaining portion of the tube was inserted continuously and delicately to the previously measured distance. he gastric position of the tube was assessed using two techniques: gastric contents aspiration and then epigastric auscultation for sounds following a small air injection (10 to 20 mL) through the tube. his was followed by post-pyloric placement, which consisted of lowering the head, positioning the patient on his/her right side, and then carefully intro-ducing the tube an additional 10 to 15 cm. he guide wire was removed and discarded, and the probe position in the duodenum was checked using a 20-mL air injec-tion with diicult return and less than 10 mL recovered, or measurement of pH ≥ 6.0. In all patients, abdominal radiography was performed to check the tube position. his procedure was performed in standardized fashion by one of ive specially trained nurses, each of whom had at least three years of experience, in cooperation with other nursing team members.
For the electromagnetically guided tube placement, the steps were similar to the traditional method. However, in this method, the device transmitted the tube tip’s path to a computer that showed it graphically on a screen (Figure 1).
Following randomization, demographic, clinical and laboratory information were collected to verify a balanced distribution between the groups. After the tube was installed, distal luid was aspirated for pH assessment, and then 15 mL contrast was given 15 minutes before the abdominal X-ray was performed to assess the nasoenteral tube position. he radiographic examination was conducted up to one hour after the tube placement. he duration of the entire procedure was recorded, including the time for tube passage, location, migration and ixation.
he ICU admission Acute Physiologic and Chronic Health Evaluation (APACHE II) and Sequential Organ Failure Assessment (SOFA) scores were calculated within the irst 24 hours following admission.
No patient-appropriate therapy was refused due to study participation. Patients were withdrawn from the
study if any medical necessity prevented compliance with the protocol. Medical necessity was deined as changes in hemodynamic or respiratory parameters that were life-threatening, such as gastrointestinal bleeds.
Statistical analysis
he two groups were compared in terms of demo-graphic and clinical data and the APACHE II and SOFA scores. he data were expressed as mean ± standard de-viation, median and 25-75 percentiles, or percentages, according to the variable’s distribution. he continuous quantitative variables were analyzed via parametric tes ting (Student’s t-test), if they were normally distributed, or via non-parametric testing (Mann-Whitney U test) if they were irregularly distributed. For nominal variables, the Fisher exact test was used, with conidence intervals based on a normal approximation of a binomial distribution.
he data were entered into an electronic databank and later analyzed using SPSS (version 13.0) software. Values of p < 0.05were considered signiicant.
rESUltS
hirty-eight patients were enrolled; one of them was subsequently excluded due to thrombocytopenia. A total of 18 patients were included in the EM group and 19 were included in the control group. he mean patient age was 67.3 years; the mean APACHE II and SOFA scores were 22.0 and 6.7, respectively. Pulmonary causes of respiratory failure were the diagnoses found in most of the medical patients (ten patients), followed by acute re-nal failure (three patients), heart failure (three patients), and stroke (one patient). In surgical patients, vascular surgery (eight patients) was most common, followed by heart surgery (three patients), neurosurgery (three pa-tients), urologic surgery (three papa-tients), gastric surgery (two patients) and orthopedic surgery (one patient). he comparison between the EM and control groups showed no statistically signiicant diference between the groups regarding demographics or clinical data (Table 1).
table 1- group comparison
Variables All
(N=37)
EM group (N=18)
Control group (N=19)
p value
Age (years) 67.3 ± 14.2
67.0 (68.0-78.0)
65.8 ± 11.3 65.5 (57.0- 74.0)
68.7 ± 16.7 68.0 (63.2- 81.5)
0.54 0.41
Female gender 54.1 55.6 52.6 0.56
Weight (kg) 78.6 ± 19.9
75.0 (65.0-87.2)
84.3 ± 22.5 80.0 (70.0- 92.5)
73.5 ± 16.2 70.0 (63.5- 83.7)
0.10 0.12
Height (cm) 165.2 ± 8.6
165.0 (160.0-170.0)
167.4 ± 8.8 168.0 (160.0 - 171.2)
163.2 ± 8.1 164.0 (156.2 - 170.0)
0.14 0.16
APACHE II 22.0 ± 5.9
23.0 (18.0-26.0)
21.2 ± 5.8 22.5 (17.0-25.0)
22.9 ± 6.1 23.0 (18.0-27.5)
0.38 0.49
SOFA 6.7 ± 2.7
7.0 (4.5-9.0)
6.2 ± 2.7 6.0 (4.0- 9.0)
7.2 ± 2.8 7.0 (5.2- 8.7)
0.31 0.23
Clinical patients 45.9 38.9 52.6 0.48
Elective surgery patients 29.7 38.9 21.1 0.48
Emergency surgery patients 24.3 22.2 26.3 0.48
Invasive mechanical ventilation patients 90.0 92.3 88.2 0.60
Use of vasopressors 38.9 29.4 47.4 0.22
Use of gastric protectors 50.0 44.5 55.6 0.75
Fluid from digestive tube aspiration 47.2 58.8 36.8 0.16
Tube replacement required 5.4 5.6 5.3 0.97
APACHE – Acute Physiologic Chronic Health Evaluation; SOFA – Sequential Organ Failure Assessment; EM - electromagnetically guided. he values expressed are mean ± standard deviation, median (25-75 percentiles), or percentages.
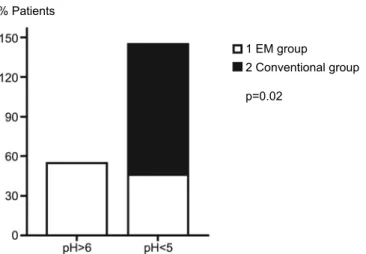
1 EM group
2 Conventional group
p=0.02 % Patients
1 EM group
2 Conventional group
p<0.001
Pre-pyloric Post-pyloric
he dark column shows the Conventional group percentage, and the pale column the EM group. No Conventinal group patient had pH>6. EM - electromagnetically guided.
Figure 3 – group comparison for the percentage of patients with >6 and <5 pH values in the aspired luids.
EM - Electromagnetically guided
DiScUSSiOn
Comparing groups with similar characteristics, post-pyloric tube placement using the real-time electromagnetic monitoring system showed higher success rates relative to placement using the conven-tional technique, as assessed by means of the mea-sured pH of the fluid aspirated from the tube and by abdominal radiography.
The main indication for enteral diet is the high incidence of gastroparesis in the ICU population (50% in mechanically ventilated patients and 80% in head trauma patients).(12-17) There are several causes of gastroparesis, such as abdominal surgery, hemodynamic instability, severe burns, electrolytic disorders, volume overload and use of vasoactive or sedative drugs. An enteral diet may improve these patients’ tolerance.(18,19) One of the obstacles to star-ting enteral nutrition is difficulty in tube installa-tion. Thus, there is a need for this new system, given its bedside feasibility.
Evidence of the benefits of an enteral diet is favorable, as reported Hsu et al.(20) Nasoduodenal tubes allow for better nutritional support and less vomiting and pneumonia. Additionally, Heyland et al. showed in a systematic review that an enteral diet provides better nutrition, reduces the time to nutritional target achievement and reduces the incidence of mechanical ventilation-associated pneumonia.(7)
p<0.001
EM group Conventional group Time (minutes)
EM - Electromagnetically guided
Figure 5 – group comparison of time required to perform the procedure.
On the other hand, Heyland states that a post-pyloric enteral diet is only recommended in institu-tions where the tube can be conveniently and quickly placed, considering the technical difficulties and the possible delay related to nasoenteral tube installation when compared with nasogastric tubes.(11)
In this context, the results of this trial, which tested the technique of nasoenteral tube placement monitored by magnetic transmission, suggest that this method may allow more institutions to be able to routinely place post-pyloric tubes.
The time elapsed in the EM group for the entire procedure was shorter than that for the control group. Also, when using the conventional technique, the correct probe position always has to be checked using radiographic testing, which causes additional delays in starting the diet infusion; this delay is not trivial, as there is evidence that early diet is beneficial.(1-3)
Several studies have shown the effectiveness of this electromagnetically guided system.(21-24) One study evaluated post-pyloric tube placement in 50 severely ill patients using the electromagnetically guided system and showed that the method is easi-ly performed and has high success rates.(21) Another study conducted on 107 children found that the electromagnetic method is safe, effective and has low hospital costs.(22) Recently, a study in burn patients showed that the technique reduced energy deficit, X-ray exposure and costs of placement.(23) In another study, a multicenter trial, this new technique was shown to be effective and fast in ICU patients.(24)
This trial has some limitations. The main limita-tion is the sample size, which was limited, as the study was discontinued due to supply shortage. However, the study was shown to have sufficient statistical power to confirm the study hypothesis. The second limitation of this study is that no comparisons were made regarding the amount of diet infused, presence of vomiting or pneumonia and cost, which would have been useful for a better evaluation of its clinical impact. Additional studies with larger samples are necessary to provide more definitive conclusions.
cOnclUSiOn
rESUMO
Objetivos: Suporte nutricional adequado tem papel impor-tante na evolução de pacientes graves. Entretanto, signiicativa porcentagem destes pacientes evolui com dismotilidade intestinal, provocando alto volume gástrico residual. A administração de dieta enteral através de sonda em posição pós-pilórica tem sido sugerida como método para melhorar a tolerância. Objetivo deste estudo foi comparar a taxa de sucesso no posicionamento pós-pilórico da sonda nasoenteral por utilização de equipamento, que permi-te acompanhar a progressão da sonda através da visualização por transmissão eletromagnética em tempo real, em comparação com o método tradicional.
Métodos: Estudo prospectivo, randomizado, controlado, rea-lizado em um hospital terciário durante três meses. Os pacientes foram randomizados para dois grupos: grupo com guia eletromag-nético, pacientes submetidos à passagem de sonda nasoenteral sob
auxilio do aparelho com visualização em tempo real e transmissão magnética e grupo convencional, passagem de sonda nasoenteral às cegas. O sucesso no posicionamento pós-pilórico e o tempo de duração do procedimento foram avaliados entre os grupos.
resultados: Foram incluídos no estudo 37 pacientes, sendo 18 do grupo com guia eletromagnético e 19 do grupo conven-cional. A localização da sonda por meio da radiograia mostrou que o grupo com guia eletromagnético apresentou mais posicio-namento pós-pilorico do que o grupo convencional, com menor tempo para realização do procedimento, com maior valor do pH do líquido aspirado pela sonda.
conclusões: O método de passagem e visualização a beira leito por transmissão eletromagnética garante de forma segura a monito-rização e acurácia frente à sondagem nasoenteral.
Descritores: Terapia nutricional; Nutrição enteral/ instrumentação; Nutrição enteral/métodos; Intubação nasogástrica
rEFErEncES
1. Heyland DK, Dhaliwal R, Drover JW, Gramlich L, Dodek P; Canadian Critical Care Clinical Practice Guidelines Committee. Canadian clinical practice guidelines for nutrition support in mechanically ventilated, critically ill adult patients. JPEN J Parenter Enteral Nutr. 2003;27(5):355-73.
2. Kreymann KG, Berger MM, Deutz NE, Hiesmayr M, Jolliet P, Kazandjiev G, Nitenberg G, van den Berghe G, Wernerman J; DGEM (German Society for Nutritional Medicine), Ebner C, Hartl W, Heymann C, Spies C; ESPEN (European Society for Parenteral and Enteral Nutrition). ESPEN Guidelines on Enteral Nutrition: Intensive care. Clin Nutr. 2006;25(2):210-23.
3. Marik PE, Zaloga GP. Early enteral nutrition in acutely ill patients: a systematic review. Crit Care Med. 2001;29(12):2264-70. Erratum in: Crit Care Med. 2002;30(3):725.
4. White H, Sosnowski K, Tran K, Reeves A, Jones M. A randomised controlled comparison of early post-pyloric versus early gastric feeding to meet nutritional targets in ventilated intensive care patients. Critical Care. 2009;13(6):R187.
5. Dempsey DT, Mullen JL, Buzby GP. he link between nutritional status and clinical outcome: can nutritional intervention modify it? Am J Clin Nutr. 1988;47(2 Suppl):352-6.
6. Alverdy J, Chi HS, Sheldon GF. he efect of parental nutrition on gastrointestinal immunity. he importance of enteral stimulation. Ann Surg. 1985;202(6):681-4. 7. Heyland DK, Drover JW, MacDonald S, Novak F, Lam
M. Efect of postpyloric feeding on gastroesophageal regurgitation and pulmonary microaspiration: results
of a randomized controlled trial. Crit Care Med. 2001;29(8):1495-501.
8. Kaufman JP, Hughes WB, Kerstein MD. Pneumothorax after nasoenteral feeding tube placement. Am Surg. 2001;67(8):772-3.
9. Kools AM, Snyder LS, Cass OW. Pneumothorax: complication of enteral feeding tube placement. Dig Dis Sci. 1987;32(10):1212-3.
10. Wendell GD, Lenchner GS, Promislof RA. Pneumothorax complicating small-bore feeding tube placement. Arch Intern Med. 1991;151(3):599-602.
11. Heyland DK, Dhaliwal R, Day A, Jain M, Drover J. Validation of the Canadian clinical practice guidelines for nutrition support in mechanically ventilated, critically ill adult patients: results of a prospective observational study. Crit Care Med. 2004;32(11):2260-6.
12. Tarling MM, Toner CC, Withington PS, Baxter MK, Whelpton R, Goldhill DR. A model of gastric emptying using paracetamol absorption in intensive care patients. Intensive Care Med. 1997;23(3):256-60.
13. Boivin MA, Levy H. Gastric feeding with erythromycin is equivalent to transpyloric feeding in the critically ill. Crit Care Med. 2001;29(10):1916-9.
14. Kortbeek JB, Haigh PI, Doig C. Duodenal versus gastric feeding in ventilated blunt trauma patients: a randomized controlled trial. J Trauma. 1999;46(6):992-6; discussion 996-8. 15. Montecalvo MA, Steger KA, Farber HW, Smith BF,
Dennis RC, Fitzpatrick GF, et al. Nutritional outcome and pneumonia in critical care patients randomized to gastric versus jejunal tube feedings. he Critical Care Research Team. Crit Care Med. 1992;20(10):1377-87.
17. Kao CH, ChangLai SP, Chieng PU, Yen TC. Gastric emptying in head-injured patients. Am J Gastroenterol. 1998;93(7):1108-12.
18. Mentec H, Dupont H, Bocchetti M, Cani P, Ponche F, Bleichner G. Upper digestive intolerance during enteral nutrition in critically ill patients: frequency, risk factors, and complications. Crit Care Med. 2001;29(10):1955-61. 19. Mutlu GM, Mutlu EA, Factor P. GI complications
in patients receiving mechanical ventilation. Chest. 2001;119(4):1222-41.
20. Hsu CW, Sun SF, Lin SL, Kang SP, Chu KA, Lin CH, Huang HH. Duodenal versus gastric feeding in medical intensive care unit patients: a prospective, randomized, clinical study. Crit Care Med. 2009;37(6):1866-72. 21. Mathus-Vliegen EM, Dulou A, Spanier MB, Fockens P.
Nasoenteral feeding tube placement by nurses using an
electromagnetic guidance system (with video). Gastrointest Endosc. 2010;71(4):728-36.
22. October TW, Hardart GE. Successful placement of postpyloric enteral tubes using electromagnetic guidance in critically ill children. Pediatr Crit Care Med. 2009;10(2):196-200.
23. Hemington-Gorse SJ, Sheppard NN, Martin R, Shelley O, Philp B, Dziewulski P. he use of the Cortrak Enteral Access System™ for post-pyloric (PP) feeding tube placement in a Burns Intensive Care Unit. Burns. 2011;37(2):277-80. 24. Holzinger U, Brunner R, Miehsler W, Herkner H,