244
Rev Bras Oftalmol. 2015; 74 (4): 244-7
1 Faculdade de Medicina do ABC – FMABC - Santo André (SP) - Brazil 2 Faculdade de Medicina do ABC - FMABC - Santo André (SP) - Brazil. 3 Faculdade de Medicina do ABC - FMABC - Santo André (SP) - Brazil. 4 Faculdade de Medicina do ABC - FMABC - Santo André (SP) - Brazil. 5 Faculdade de Medicina do ABC - FMABC - Santo André (SP) - Brazil.
C
ASER
EPORTReceived for publication 11/06/2012 - Accepted for publication 03/09/2012 The authors declare no conflicts of interest
Flávia Marques Rodrigues
1, Nilson Lopes da Fonseca Junior
2, José Ricardo Carvalho Lima Rehder
3, Celso Lopez Fernandez
4,
Debora Mayumi Sugano
5Atypical presentation of Graves’
ophthalmopathy
Apresentação atípica da oftalmopatia de Graves
R
ESUMOA oftalmopatia de Graves é a doença orbitária mais comum e acomete 25 a 50 % dos pacientes portadores da Doença de Graves sendo mais frequente no sexo feminino, entre a segunda e quinta décadas de vida. A doença apresenta uma fase aguda e uma crônica, evoluindo lenta e progressivamente até estabilizar, sendo raros os casos de resolução espontânea. O tratamento dependerá da fase em que a doença se encontra sendo baseado principalmente na corticoterapia via oral e endovenosa e/ou radioterapia, sendo a colchicina empregada em casos isolados. No seguinte relato de caso, abordaremos uma forma atípica de manifestação clínica da Oftalmopatia de Graves em paciente eutireoidéia com anticorpos negativos na sua apresentação inicial.
Descritores: Oftalmopatia de Graves; Eutireoidea; Manifestação atípica; Anticorpos negativos; Colchicina; Relatos de casos
A
BSTRACTGraves ‘ophthalmopathyis themost commonorbital diseaseand affects25-50% of the patients withGraves’ disease. It`s morecommon in females, between the second andfifth life`s decade. The disease hasanacute andachronic stage, slowly progressing until it stabilizes, with rarecasesof spontaneous resolution.The treatment depends on thestage andthe disease ismainly treated withoralor intravenous corticosteroids with or without radiotherapy;colchicine is usedin individual cases. In the followingcase report, we discuss an atypicalmanifestation ofGraves’ ophthalmopathyin an euthyroid patientwith negative antibodiesin the inicial presentation.
Keywords: Graves’ ophthalmopathy;Euthyroid;Atypical manifestation; Negative antibodies; Colchicine; Case reports
Study conducted in the Discipline of Ophthalmology at the Medicine College of ABC - FMABC - Santo André (SP) - Brazil.
245
I
NTRODUCTIONT
he Graves ophthalmopathy is the most common orbital disease, and it affects 25-50% of patients with Graves’ disease(1). It is an autoimmune disease characterized bythe deposition of immune complexes antithyroglobulin in the extraocular muscles. In the early stages of the disease, there is an infiltration of adipose, muscle, and connective tissues in the orbit by T lymphocytes, mast cells, macrophages and plasma cells(2-4). It
is believed that activated T lymphocytes directed against the thyroid follicular cells recognize and bind to similar antigens present in the orbital tissues. Macrophages and dendritic cells initiate the immune response, which is propagated by the recruitment of sensitized T cells(2-4). Then various inflammatory
mediators are released (IFN gamma, TNF, IL-1), which stimulate fibroblasts to produce glycosaminoglycans, which have a hydrophilic characteristic that draws water into the fat, muscle and connective tissues, causing edema and consequently fibrosis of all the periorbit, with hypertrophy of the extraocular muscles, particularly the medial and lower rectus and orbital fat, resulting in increased orbital volume, causing mainly proptosis(2-4).
Although the Graves ophthalmopathy is more common between the second and fifth decades of life, it can occur in any age group. It is eight times more frequent in women, but in men the involvement is more serious. It usually occurs when there is thyroid dysfunction, but the ocular or orbital changes may pre-cede or follow the thyroid dysfunction in up to 18 months(2).
Currently there are important systems to rate the severity and activity of the disease. In this context we may mention the NOSPECS which includes the following criteria: class 0 for patients who have no signs or symptoms, class 1 for presenting only signs (retraction of upper eyelid, stare, retraction of the upper eyelid to look down and proptosis above 22mm) and without symptoms, class 2 in those with soft tissue involvement (symptoms and signs), class 3 in patients with proptosis, class 4 when there is involvement of the extraocular muscles, class 5 when there is corneal involvement and class 6 in those with a loss of visual acuity (involvement of the optic nerve) and CAS (clinical activity score), including signs of acute inflammation such as hyperemia, pain, edema, and secondary functional impairment to the presence of inflammation(1-3).
The disease develops slowly and progressively until stabilization, with rare cases of spontaneous resolution being reported. It usually manifests clinically in the acute phase with ocular hyperemia, chemosis, eyelid edema, proptosis of varying degrees, diplopia, impairment of ocular extrinsic muscles, with the most affected muscles being the lower, the medial, the upper and finally the side rectus, respectively. The most frequent signs are: retraction of the upper eyelid when looking down (lidlag), retraction of the lower eyelid (which worsens in the attempt to look up), reduced frequency of blinking, decreased convergence, inability to keep fixation on the side look and look scared in the attempt to fixate (Kocher’s sign). In the chronic phase of the inflammatory process, some patients develop restricted, fibrotic muscles which can increase the deviation observed in the acute phase(2,3).
The treatment is based on the phase in which the disease is (acute or chronic). In the acute phase, the anti-inflammatory treatment of choice is the corticosteroid therapy orally or intravenously. Corticosteroid therapy is associated with the use of radiation, using the linear accelerator in ten continuous sessions in the most severe cases or ten weekly sessions with
total doses of 2000cGy. Another drug treatment option is the use of colchicine, with a dosage of 0.5 to 1.5 mg/day, alone or combined with radiotherapy and/or corticosteroids, with good therapeutic response.
Except for the emergency cases in which there is the risk of vision loss by exposure of the cornea or compressive optic neuropathy, surgical treatment should be indicated in the inactive phase of Graves’ orbitopathy. This treatment consists of orbital decompression, treatment of strabismus, and correction of eyelid retraction and aesthetic blepharoplasty, in that order(2,3).
The following case report will discuss an atypical form of clinical manifestation of Graves’ ophthalmopathy.
C
ASER
EPORTEMS, 49, female, brown, single, general services assistant, from São Bernardo do Campo – SP, referred to the Orbit Sector in the Discipline of Ophthalmology at the Medicine College of ABC complaining of pain in the left eye for 5 months associated to red eye, double vision, blurred vision, eyelid swelling and intense pain on eye movement. She denied personal and family history of eye disease. As systemic personal history she had a history of cervical cancer treated 8 years ago.
The visual acuity with the best correction was 20/25 RE and 20/40 LE. Upon inspection changes were found only in the left eye: bipalpebral edema 2+/4+, exotropia and conjunctival hyperemia 2+/4+. The ocular extrinsic motility presented limitation to lateroversions, being mild to adduction and severe to abduction. Direct and consensual pupillary light reflexes were preserved. The intraocular pressure was measured with the flattening technique and presented 12 mmHg in the RE and 36 mmHg in the LE (01pm). There were no changes in the anterior segment or in fundoscopy. Initially the following serum dosages were asked: TSH, free T4, anti-thyroglobulin antibody (anti-TG Ab), anti-thyroid peroxidase antibody (Anti-TPO Ab) and TRAb, Antinuclear (ANA) Ab, native DNA Ab, Sm Ab, Anti-histone Ab, VDRL, CH50, ACE, Lysozyme, Calcium, RF, ANA, HSS, c-ANCA and p-ANCA. In addition to said dosages, the following tests were requested: PPD, chest X-ray, abdominal ultrasonography, orbit CT, urinary calcium dosage and complete gynecological examination. Colchicine was introduced orally (0.5 mg every 12 hours), timolol maleate and brimonidine tartrate both 1 droplet every 12 hours in the left eye.
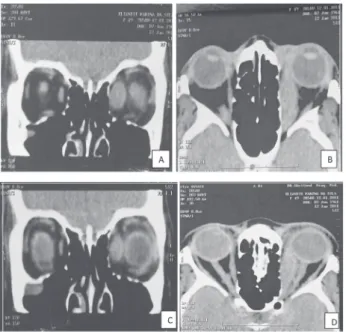
After 4 weeks, the patient returned with partial reduction of pain, eyelid edema and conjunctival hyperemia, but still complaint of diplopia. The IOP measured was: RE - 13 mmHg, and LE - 16 mm Hg (01pm). The extrinsic motility showed limitations to lateroversions and supraversion of the LE. Among the exams requested, only the following were outside the nor-mal range: 1) The orbit CT (Figure 1) showed a thickening of the medial rectus muscle of the left eye, 2) PPD (19mm = strong reactor), 3) HSS of the first hour (40mm) and 4) the chest X-ray revealed the presence of multiple diffuse consolidations in the pulmonary parenchyma in the hilar region, suggestive of pulmonary cicatrization change (Figure 2). Thus, a biopsy of the medial rectus muscle of the LE under general anesthesia was suggested, and the patient was referred for assessment of the Pulmonologist who requested: 1) computed tomography of the chest showing multiple hyperattenuating lesions in the lung parenchyma suggestive of calcification and ancient cicatrization process (Figure 1), direct BK search with negative result.
246 Rodrigues FM, Fonseca Junior NL, RehderJRCL, Fernandez CL, Sugano DM
Rev Bras Oftalmol. 2015; 74 (4): 244-7
D
ISCUSSIONThyroid ophthalmopathy is classified into acute or inflammatory disease, progressive and histologically associated to lymphocytic infiltration and edematous changes, and in chronic or inactive disease associated with fibrotic changes and fat infiltration in the retro-orbital tissues, especially the extraocular muscles(5,6). The acute phase of the disease presents as main
symptoms: pain, conjunctival hyperemia, edema and eyelid hyperemia, proptosis, caruncle edema, chemosis, diplopia and blurred vision(3). The involvement is bilateral in 80% of cases;
and usually manifests in patients with hyperthyroidism, involving two or more extraocular muscles without tendon involvement(7).
In this case, the initial manifestation was unilateral, involving only one extraocular muscle (MRI LE) and its respective tendon in a patient in clinical and laboratory euthyroid state. The literature reveals that only 10% of patients with thyroid ophthalmopathy do not develop hyperthyroidism as the initial manifestation of the disease(7). From these, 3% presented
hypothyroidism, and 7% euthyroid(7). Among the euthyroid
patients (7%), only 2.5% did not have positive results for Anti-TG Ab, Ant-TPO Ab and/or TRAb, revealing the atypical form of the initial clinical presentation of the disease in this case.
The biopsy should be indicated in cases where the diagnosis is doubtful based only on the clinical profile and additional exams or when there is recurrence or resistance to the treatment being very important to rule out differential diagnoses.
Colchicine, a drug used to treat the patient in question, inhibits mobility, chemotaxis, adhesion and phagocytosis of granulocytes; reduces the levels of adhesion molecules; inhibits the action and proliferation of fibroblasts and lymphocytes, and inhibits the synthesis of collagen. This drug was indicated due to the patient being strong reactive to PPD, in this case being contraindicated the use of systemic corticosteroids.
One study compared the use of colchicine to prednisone in the treatment of 22 patients during the inflammatory phase of Graves’ ophthalmopathy. All the patients were similar regarding age, sex and smoking habits, and suffered euthyroidism for at least 3 months. They were randomized into 2 groups. Group 1 The results of all the exams described above and the clinical
approval for the surgical procedure proposed were obtained after 7 weeks. On hospitalization the patient had were significantly better in signs and symptoms of the LE and acute impairment of the RE. At extrinsic motility, there were moderate limitations to lateroversions and supraversions of the RE (Figure 3). So the choice was a new imaging study (orbit CT), and after the analysis of the images (Figure 1) the biopsy of medial and lower rectus of the RE was indicated under general anesthesia, and also a new serum dosage of TSH, free T4 , Anti-TG Ab, Anti-TPO Ab and TRAb.
The anatomic and pathological study revealed the presence of striated skeletal muscle tissue with intense lymphoplasmocytic inflammatory infiltrate with a predominance of T lymphocytes and the presence of macrophages found consistent with the inflammatory phase of Graves’ ophthalmopathy. The serum dosage of TRAb was 35U/L, interpreted as a positive result. The other results are within the normal limits.
Figure 1: Computed tomography of orbit - A) Coronal section (soft tissue window). B) Axial section (soft tissue window). Thickening of the medial rectus muscle of the left eye with tendon involvement at the time of initial care of patient. C) Coronal section (soft tissue window). D) Axial section (soft tissue window). Diffuse thickening of the extraocular muscles of the right eye before surgery immediately before the biopsy.
Figure 2: Image Exam. A) Chest X-ray - presence of multiple diffuse consolidations in the pulmonary parenchyma in the hilar region suggestive of pulmonary cicatrization change. B) Computed tomography of the chest - presence of multiple hyperattenuating lesions in the lung parenchyma suggestive of calcifications and ancient cicatrization process.
247
Corresponding author:
Flavia Marques Rodrigues
Rua de Ceuta 222 Jardim Lusitânia São Paulo (SP) ZIP Code 04031-01
Email: flaviamarques102@yahoo.com.br
(G1) received colchicine (1.5 mg/day), and group 2 (G2) was treated with prednisone (0.75 mg/kg/day). Although it was verified a reduction in the clinical activity of the disease in the 2 groups, the patients treated with colchicine did not suffer the side effects of prednisone such as weight gain, stomach problems, weakness, depression and changes in blood pressure, as observed in the present case(8).
The orbital radiotherapy is an important adjuvant treatment of severe Graves’ orbitopathy in activity due to its anti-inflammatory effects and local immunosuppressants. About 60% of patients treated showed a favorable response(9). The
successful approach will depend on the correct selection of patients, showing better results the earlier it is established.
R
EFERENCES1. Kuriyan AE, Phipps RP, Feldon SE.The eye and thyroid disease. Curr Opin Ophthalmol.2008;19(6):499-506.
2. Höfling Lima AL, Morales PH, Manso PG, Farah ME. Alterações oculares de doenças sistêmicas: retinopatia diabética e oftalmopatia de Graves. RBM Rev Bras Med.2006;63(5). 3. Saraci G, Treta A.Ocular changes and approaches of
ophthalm-opathy in basedow - graves- parry- flajani disease. Maedica (Buchar). 2011;6(2):146-52.
4. Weetman AP. Thyroid-associated eye disease: Pathophysiology. Lancet. 1991;338(8758):25-8. Review.
5. Fung S, Malhotra R, Selva D. Thyroid orbitopathy. Aust Fam Phy-sician. 2003;32(8):615-20. Review.
6. Yokoyama N, Nagataki S, Uetani M, Ashizawa K, Eguchi K. Role of magnetic resonance imaging in the assessment of disease activity in thyroid-associated ophthalmopathy.Thyroid. 2002;12(3):223-7. 7. Stamato FJ, Manso PG, Maciel JR, Wolosker AM, Maciel RM,
Furlanetto RP. Colchicine as a new option for the clinical treat-ment of Graves’ ophthalmopathy. Proceedings of the VIth Inter-national Symposium on Graves’ Ophthalmopathy, Amsterdam, November 27 to 28, 1998, p. 22.
8. Stamato FJ, Maciel RM,Manso PG, Wolosker AM, Paiva ER, Lopes AC,et al. Colchicina no tratamento da fase inflamatória da oftalmopatia de Graves: um estudo prospectivo e randomizado com prednisona. Arq Bras Oftalmol.2006;69(6):811-6.
9. Pitz S, Kahaly G, Rösler HP, Krummenauer F, Wagner B, Stübler M, et al. [Retrobulbar irradiation for Graves’ ophthalmopathy — long-term results]. Klin Monbl Augenheilkd. 2002;219(12):876-82.German.
Atypical presentation of Graves’ ophthalmopathy