www.jped.com.br
ORIGINAL
ARTICLE
Neonatal
outcomes
according
to
different
therapies
for
gestational
diabetes
mellitus
夽
,
夽夽
Amanda
L.
da
Silva
a,∗,
Augusto
R.
do
Amaral
a,
Daniela
S.
de
Oliveira
a,
Lisiane
Martins
a,
Mariana
R.
e
Silva
a,
Jean
Carl
Silva
baUniversidadedaRegiãodeJoinville(UNIVILLE),Joinville,SC,Brazil bUniversidadeFederaldeSãoPaulo(UNIFESP),SãoPaulo,SP,Brazil
Received26January2016;accepted7April2016 Availableonline28June2016
KEYWORDS
Gestationaldiabetes mellitus;
Therapeutics; Outcomes
Abstract
Objectives: Tocomparedifferentneonataloutcomesaccordingtothedifferenttypesof treat-mentsusedinthemanagementofgestationaldiabetesmellitus.
Methods: This was a retrospective cohort study.The study population comprised pregnant womenwithgestationaldiabetestreatedatapublicmaternityhospitalfromJuly2010toAugust 2014.Thestudyincludedwomenagedatleast18years,withasingletonpregnancy,whomet thecriteriaforgestationaldiabetesmellitus.Bloodglucoselevels,fetalabdominal circumfer-ence,body massindexandgestationalagewereconsideredfor treatmentdecision-making. The evaluatedneonataloutcomeswere:type ofdelivery,prematurity, weightinrelationto gestationalage,Apgarat1and5min,andneedforintensivecareunitadmission.
Results: Thesampleconsistedof705pregnantwomen.Theneonataloutcomeswereanalyzed based onthe treatmentreceived. Women treatedwith metforminwere less likelyto have children who were smallfor gestationalage (95%CI:0.09---0.66)andmore likelytohave a newbornadequateforgestationalage(95%CI:1.12---3.94).Thosewomentreatedwithinsulin hadalowerchanceofhavingapretermchild(95%CI:0.02---0.78).Thecombinedtreatmentwith insulinandmetforminresultedinhigherchanceforaneonatetobebornlargeforgestational age(95%CI:1.14---11.15)andlowerchancetobebornpreterm(95%CI:0.01---0.71).Thetypeof treatmentdidnotaffectthemodeofdelivery,Apgarscore,andintensivecareunitadmission.
Conclusions: Thepediatricianinthedeliveryroomcanexpectdifferentoutcomesfordiabetic mothersbasedonthetreatmentreceived.
©2016SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/
4.0/).
夽
Pleasecitethisarticleas:SilvaAL,AmaralAR,OliveiraDS, MartinsL,SilvaMR,SilvaJC.Neonataloutcomesaccordingtodifferent
therapiesforgestationaldiabetesmellitus.JPediatr(RioJ).2017;93:87---93.
夽夽
StudycarriedoutatMaternidadeDarcyVargas,Joinville,SC,Brazil.
∗Correspondingauthor.
E-mail:Mandinha4265@hotmail.com(A.L.Silva). http://dx.doi.org/10.1016/j.jped.2016.04.004
PALAVRAS-CHAVE
Diabetesmellitus gestacional; Tratamento; Desfechos
Desfechosneonataisdeacordocomdiferentesterapêuticasdodiabetesmellitus gestacional
Resumo
Objetivos: Comparardiferentesdesfechosneonataisdeacordocomasdiferentesmodalidades detratamentosdodiabetesmellitusgestacional.
Métodos: Trata-sedeumacoorteretrospectiva.Apopulac¸ãodoestudofoicompostapor ges-tantescomdiabetesgestacionalatendidasemumamaternidadepúblicadesdeJulhode2010 aAgostode2014.Foramincluídasmulherescomidademínimade18anos,gestac¸ãoúnicae comcritériospara diabetes mellitusgestacional.Paradecisãoterapêuticaforam considera-dosglicemias,circunferênciaabdominalfetal,índicedemassacorporaleidadegestacional. Osdesfechosneonataisavaliadosforam:viadeparto, prematuridade,relac¸ãodopesocom idadegestacional,Apgarno1◦e5◦minutoenecessidadedeinternac¸ãoemunidadedeterapia
intensiva.
Resultados: Aamostrafoicompostapor705gestantes.Osdesfechosneonataisforamanalisados combasenaterapêuticarecebida.Mulherestratadascommetforminativerammenorchance deteremfilhospequenosparaaidadegestacional(IC95%:0,09-0,66)emaiorchancedeterem umfilhoadequadoparaaidadegestacional(IC95%:1,12-3,94).Agestantetratadacominsulina tevemenorchancedeterumfilhoprematuro(IC95%:0,02-0,78).Otratamentofeitocoma associac¸ãodeinsulinaemetforminaresultouemmaiorchancedeum recém-nascidogrande paraaidadegestacional(IC95%:1,14-11,15)emenorchancedeprematuridade(IC95%: 0,01-0,71).Amodalidadedetratamentonãointerferiunaviadeparto,Apgareinternac¸ãoemterapia intensiva.
Conclusões: Opediatranasaladepartopodeesperardiferentesdesfechosparaofilhodemãe diabética,combasenotratamentorecebido.
©2016SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Este ´eumartigo OpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4.
0/).
Introduction
According to a Latin American multicentric study, ges-tational diabetes mellitus (GDM) is the most prevalent metabolicdisorder during pregnancy.1 Itoccursin women whose pancreaticfunction is insufficient toovercomethe insulinresistanceduetothesecretionofdiabetogenic hor-monesbytheplacenta.2InBrazil,theestimatedprevalence ofGDMvariesfrom2.4%to7.2%.3
Both the mother and baby are affected by GDM, as bothhaveariskofdevelopingundesirableoutcomes.4GDM affectsthenewbornasitincreasesthechanceof macroso-mia,fetaldistress,metabolicdisorders,hyperbilirubinemia, growth imbalance, and other complications.5 In order to minimizetheconsequences,itisnecessarythatthedisease isdiagnosed andtreatedearly,becausethe outcomesare alsorelatedto theonset andduration of glucose intoler-ance,aswellastheseverityofGDM.5
InsulinhasbeenusedasthestandardtreatmentforGDM for along time.However,researchers havedemonstrated thesafetyoforalhypoglycemicagents,suchasmetformin, inthe initial treatment when diet aloneis not enough to achievethedesiredglucoselevels.6,7
Studiesthatcomparedtheuseofmetforminandinsulin inthemanagementofGDMdemonstratedbenefitswiththe use of oral hypoglycemic agents, such as fewer prema-turebirthsandcesarean deliveries,reductionin maternal weightgain,andfeweradverseneonataloutcomes,suchas
macrosomia,6,8 hypoglycemia, jaundice, and admission to specialneonatalcareservices.9
Thus,thestudyaimedtocomparedifferentneonatal out-comesaccordingtothedifferenttreatmentmodalitiesused inthemanagementofGDM.
Methods
Thiswasaretrospectivecohortstudybasedontheanalysis of medical records,carried outfrom July 2010 to August 2014. The study sample was chosen by convenience; the populationcomprisedpregnantwomenwithGDMtreatedat a high-risk pregnancy outpatientclinic of apublic mater-nity hospital.The project wasapproved by the Research EthicsCommitteeofHospitalRegionalHansDieterSchmidt, Joinville,SC,Brazil.
The study included all women aged ≥18 years with a singleton pregnancy andwho met the criteriafor GDM.10 The diagnosisofGDMwasmadebasedontheoralglucose tolerance test. The presence of at leastone of thethree following criteriaconfirmed the diagnosis: fastingglucose
≥92mg/dL,bloodglucosewithinthefirsthour≥180mg/dL, andglucoselevelsinthesecondhour≥153mg/dL.11Women whosebabieshadnomalformations,whowerefollowed-up at the outpatientclinic,and whose deliveredoccurredat thehospitalwereincluded.
combination of metformin and insulin and one had been treatedwithdietalone.
Thefirstfollow-upconsultationofdiabeticpatients usu-ally involves obstetrical ultrasound and routinescreening forGDM.Furthermore,thepregnantwomenalsoattended awelcomelecturewithanutritionist andaphysical ther-apist, in order to receive information regarding lifestyle changes(diet andphysical exercise). Then,blood glucose was measured twice on consultation day (fasting and 1h afterbreakfast)andoncepermonthatfourdifferenttimes (fastingand1hafterthestartofeachmeal).Theinterval betweenconsultationswasof15---21days.
Thebloodglucosemeasurements(fastingand postpran-dial), fetal abdominal circumference, body mass index (BMI),andgestationalagewereconsideredforthe therapeu-ticdecision-making.Diettherapywasrecommendedtoall pregnantwomen.InmildcasesofGDM,thechoiceof ther-apywasmetformin.Whennoglycemiccontrolwasachieved withamaximumdoseofmetformin(2.5g),itwasassociated withinsulintherapy;insulintherapywaspromptlystartedin moreseverecases,without anattempttousemetformin. GDM cases were considered severe when fetal abdominal circumference was >90th percentileand maternal fasting glucosewas>100mg/dLandpostprandial(1h)>140mg/dL. Thecollecteddatarelatedtothewomenwerefullname, dateoflastmenstrualperiod,probabledateofdelivery, ges-tationalage,numberofvaginaldeliveries,cesareansections andmiscarriages,pre-pregnancyweightandheight,results of oralglucose tolerancetest, treatment used,andblood glucoselevel.
Afterbirth,themedicalrecordsofthechildrenbornto diabeticmotherswereanalyzedinordertocollect informa-tionabouttypeof delivery,gestationalage atbirth,birth length andweight,Apgar score at thefirst andfifth min-utes,morphology,andadmissiontotheneonatalintensive careunit(NICU).
ThecollecteddatawerestoredinaMicrosoftExcel2013 (Microsoft®,USA)spreadsheet.Alltheinformationobtained
was analyzed using SPSS (IBM Corp. Released 2012. IBM SPSSStatisticsforWindows,Version21.0.USA).Meansand standard deviations were calculated for the quantitative variables,whereasabsoluteandrelativefrequencies were usedfor qualitative variables.Binomial logisticregression modelswereconstructed toassesstheinfluence of differ-enttherapies onneonataloutcomesandadjusttheeffect ofconfoundingvariables.95%confidenceintervals(95%CI) wereestablishedandpvalues<0.05wereconsidered signif-icant.
Results
The study sample consisted of 705pregnant women diag-nosed with GDM and their respective babies. After the medical records were analyzed, the participants were groupedintofourtreatmentgroups:(1)diet,(2)metformin, (3)insulin,and(4)metformin+insulin.
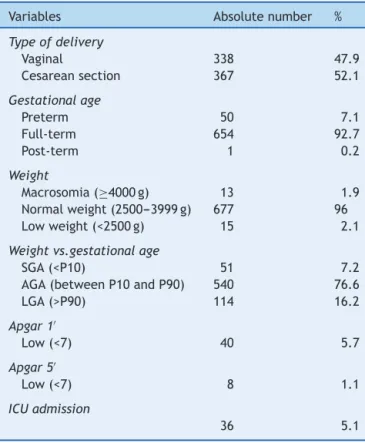
Table 1 shows the general characteristics of the study participants.Briefly, thepatients hada meanage of 30.6 years(SD±6.34)andmeannumberofpregnanciesof2.65 (SD±1.67). Cesarean section was the type of delivery in 52.1% of the cases. Regarding GDM treatment, most
Table 1 General characteristicsofthe pregnant women (n=705).
Variable Mean Standard
deviation
Age 30.58 6.34
Numberofgestations 2.65 1.67
Pre-gestationalBMI 29.34 6.17
Gestationalagea 28.53 7.09
Fastingglycemiab 89.23 13.65
Post-prandialglycemiac 117.08 17.57
BMI,bodymassindex.
a Gestationalageatthefirstconsultationinagestational
dia-betesmellitusoutpatientclinic.
b Meanvaluesobtainedduringgestation.
c Meanvaluesobtainedduringgestation.
pregnantwomenwereprescribeddiettherapyasthe treat-mentofchoice(41.6%);35.5%ofthewomenweretreated withmetformin,15%withinsulin,andtheremainderwitha metforminandinsulinassociation(7.9%).
Hypertensive disease of pregnancy was present in 72 patients.Twenty-sixmothersweretreatedwithmetformin, 16withdiettherapy,15withinsulinalone,and15withthe association ofinsulin andmetformin. Thosewhoreceived the combination of metformin and insulin had a higher chance of havinghypertensive disease of pregnancy(AOR 2.38[1.07---5.28])whencomparedwiththoseunderthediet treatment.TheotherGDMtreatmentsshowednodifference inrelationtothismaternaloutcome.
Table2 Generalcharacteristicsofthenewborns(n=705).
Variables Absolutenumber %
Typeofdelivery
Vaginal 338 47.9
Cesareansection 367 52.1
Gestationalage
Preterm 50 7.1
Full-term 654 92.7
Post-term 1 0.2
Weight
Macrosomia(≥4000g) 13 1.9
Normalweight(2500---3999g) 677 96
Lowweight(<2500g) 15 2.1
Weightvs.gestationalage
SGA(<P10) 51 7.2
AGA(betweenP10andP90) 540 76.6
LGA(>P90) 114 16.2
Apgar1′
Low(<7) 40 5.7
Apgar5′
Low(<7) 8 1.1
ICUadmission
36 5.1
SGA,smallfor gestationalage;AGA,adequateforgestational
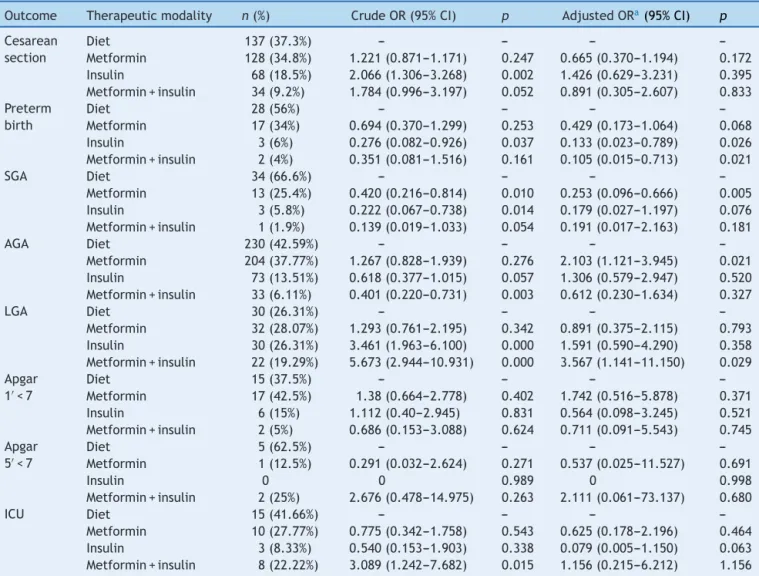
Table3 Multivariateanalysisofneonataloutcomesaccordingtotypeofgestationaldiabetesmellitustherapy(n=705).
Outcome Therapeuticmodality n(%) CrudeOR(95%CI) p AdjustedORa(95%CI) p
Cesarean section
Diet 137(37.3%) --- --- ---
---Metformin 128(34.8%) 1.221(0.871---1.171) 0.247 0.665(0.370---1.194) 0.172 Insulin 68(18.5%) 2.066(1.306---3.268) 0.002 1.426(0.629---3.231) 0.395 Metformin+insulin 34(9.2%) 1.784(0.996---3.197) 0.052 0.891(0.305---2.607) 0.833 Preterm
birth
Diet 28(56%) --- --- ---
---Metformin 17(34%) 0.694(0.370---1.299) 0.253 0.429(0.173---1.064) 0.068 Insulin 3(6%) 0.276(0.082---0.926) 0.037 0.133(0.023---0.789) 0.026 Metformin+insulin 2(4%) 0.351(0.081---1.516) 0.161 0.105(0.015---0.713) 0.021
SGA Diet 34(66.6%) --- --- ---
---Metformin 13(25.4%) 0.420(0.216---0.814) 0.010 0.253(0.096---0.666) 0.005 Insulin 3(5.8%) 0.222(0.067---0.738) 0.014 0.179(0.027---1.197) 0.076 Metformin+insulin 1(1.9%) 0.139(0.019---1.033) 0.054 0.191(0.017---2.163) 0.181
AGA Diet 230(42.59%) --- --- ---
---Metformin 204(37.77%) 1.267(0.828---1.939) 0.276 2.103(1.121---3.945) 0.021 Insulin 73(13.51%) 0.618(0.377---1.015) 0.057 1.306(0.579---2.947) 0.520 Metformin+insulin 33(6.11%) 0.401(0.220---0.731) 0.003 0.612(0.230---1.634) 0.327
LGA Diet 30(26.31%) --- --- ---
---Metformin 32(28.07%) 1.293(0.761---2.195) 0.342 0.891(0.375---2.115) 0.793 Insulin 30(26.31%) 3.461(1.963---6.100) 0.000 1.591(0.590---4.290) 0.358 Metformin+insulin 22(19.29%) 5.673(2.944---10.931) 0.000 3.567(1.141---11.150) 0.029 Apgar
1′<7
Diet 15(37.5%) --- --- ---
---Metformin 17(42.5%) 1.38(0.664---2.778) 0.402 1.742(0.516---5.878) 0.371 Insulin 6(15%) 1.112(0.40---2.945) 0.831 0.564(0.098---3.245) 0.521 Metformin+insulin 2(5%) 0.686(0.153---3.088) 0.624 0.711(0.091---5.543) 0.745 Apgar
5′<7
Diet 5(62.5%) --- --- ---
---Metformin 1(12.5%) 0.291(0.032---2.624) 0.271 0.537(0.025---11.527) 0.691
Insulin 0 0 0.989 0 0.998
Metformin+insulin 2(25%) 2.676(0.478---14.975) 0.263 2.111(0.061---73.137) 0.680
ICU Diet 15(41.66%) --- --- ---
---Metformin 10(27.77%) 0.775(0.342---1.758) 0.543 0.625(0.178---2.196) 0.464 Insulin 3(8.33%) 0.540(0.153---1.903) 0.338 0.079(0.005---1.150) 0.063 Metformin+insulin 8(22.22%) 3.089(1.242---7.682) 0.015 1.156(0.215---6.212) 1.156
OR,oddsratio;CI,confidenceinterval;SGA,smallforgestationalage;AGA,adequateforgestationalage;LGA,largeforgestational
age;ICU,intensivecareunit.
aAdjustedORforthefollowingvariables:maternalage,maternalbodymassindex,numberofpregnancies,typeofdelivery,gestational
ageatfirstconsultation,meanfastingglucose,meanpostprandialbloodglucose,andfetalabdominalcircumference(consideredbetween
28and32weeksgestation).
Regardingthecharacteristicsofthenewborns(Table2), themeanGAatdeliverywas38.6weeks(SD±1.38). Thirty-fourbabieswerepreterm(4.8%);40(5.6%) hadlowApgar score at the first minute and eight(1.1%) had low Apgar scoreat thefifthminute. Atotalof 114(16.1%)newborns werelargeforgestationalageand51(7.2%)werebornsmall forgestationalage.Thirty-six(5.1%)newbornsneededNICU admission.
TheneonataloutcomeswereanalyzedbasedontheGDM therapyused(Table3),takingintoaccountthatthe treat-mentswerecomparedwiththediettherapy.
Thetypeoftreatmentdidnotaffect theoutcometype ofdelivery,Apgarscoresatthefirstandfifthminutes,and needforNICUadmission.
Pregnantwomenwhoweretreatedwithmetforminhad alowerchanceofhavingasmallforgestationalage(SGA) child andalso had slightly over twice the chance of hav-ingababywithadequateweightforgestationalage(AGA). Motherswhoreceivedinsulintreatmenthadalowerchance
thattheirchildrenwouldbebornpreterm.Similarly, moth-erstreatedwiththecombinationofmetforminandinsulin werealsolesslikelytohavepretermchildren.Inaddition, womentreatedwiththiscombinationtherapyhadmorethan threetimesthechanceofhavingalargeforgestationalage (LGA)child.
Discussion
withatwo-foldhigherchanceofAGAnewborns(AOR2.10 [1.12---3.94]).
The percentage of preterm infants was 7.1%. Those treated with insulin had a lower chance for this out-come (AOR 0.13 [0.023---0.78]), as well as those treated with a combination of insulin and metformin (AOR 0.10 [0.01---0.71]).NICUadmissionratewas5.1%;thetreatment modalitiesdidnot affect theneed for it. The percentage ofcesarean deliveries was52.1%,and theGDMtreatment modalitiesdidnotaffectthetypeofdelivery.Therewasno increasedchanceoflowApgarscore,bothatthefirstand thefifthminutes,accordingtothetherapyused.
Thepresentstudyisimportant,becausealthoughinsulin isconsidered thestandard classicaltreatmentfor the dis-ease, metformin has demonstrated good results in GDM control and appears to attenuate the possible neonatal outcomes.6,7
ThephysiciansresponsibleforpregnantwomenwithGDM needtobeawareofthematernalandneonatalrisksrelated to this metabolic disorder.12 One of the most common complicationsofGDMisanLGAchild.12Whenthenewborn is classifiedas LGA,in additiontothe factthat thebirth is associatedwithincreased riskof obstetric traumasand shoulderdystocia,immediateeffectssuchashypoglycemia andrespiratorydysfunctionmayalsooccur.12
Inthepresent study,16.2%ofnewborns wereclassified asLGA.Intheliterature,thispercentagerangesfrom13.4 to30%.13---16Patientswhoreceivedtheassociationofinsulin andmetforminhada3.5-foldhigherriskofhavinganLGA baby. There wasno difference for the other treatments. TheliteratureshowedhigherratesofLGAbirthsinwomen treatedwithinsulinwhencomparedwiththosetreatedwith metforminordiettherapy.6
Among theperinatalcomplicationsof anLGAnewborn, arenoteworthytheincreasedriskofmeconiumaspiration, claviclefracture, perinatalhypoxia,hypoglycemia, hyper-bilirubinemia,transient tachypnea,brachialplexus injury, shoulderdystocia,andevenneonataldeath.17Thesebabies were also at increased risk at the moment of treatment choice,which wasmore aggressivedue tothefetal char-acteristicsobservedduringprenatalcare.
An intensive therapyfor GDM mayresultina decrease of fetal weight, preventing LGA newborns. However, one consequence is the increase in the number of SGA newborns.18Suchdisordersarealsorelatedtoearlyneonatal complicationsanddiseasesinadulthood.18,19
Inthisstudy,theincidenceofSGAinfantswas7.2%,while intheliteratureitrangedfrom3%to10.5%.19,20Thechance ofhavinganSGAnewbornwaslowerinthegroupofwomen treatedwithmetformin.ThestudybyGohetal.showedno differencefortheSGA outcomeaccordingtothedifferent treatments.6
BeingSGAisasunfavorableasbeingLGA,sincebothare associatedwithhighermorbidityandmortalityinthe short-andlong-term.Therefore,preventingtheoccurrenceofSGA isasimportantaspreventingthatofLGA.20Inaselectgroup ofpregnantwomen,whenthereisindirectevidenceoffetal hyperinsulinizationattheultrasound,thedrugdosecouldbe reduced.
Forthatpurpose,itmightbenecessarytoconsiderthe fetalweightestimated bytheultrasoundinthe therapeu-ticoptionofpatientstreatedwithmetformin,astherewas
a higher risk of SGA. Thus, an approach based on ultra-soundparameterscanprovide amoreflexibletherapeutic modelforthosepatientswhosenewbornweightestimated bytheultrasoundisreducedandtherefore,thedosecanbe decreased.20
The quality of the treatment provided to diabetic pregnantwomenhasadirecteffectonthenewbornweight classification.ConsideringthatAGAis thetreatmentgoal, treatmentsuccesscanbeassessedbythisparameter.Inthe presentstudy,theincidenceofAGAinfantswas76.6%.The literaturereports thatAGArates arearound86.6%.20 Met-forminwasshowntobeverysatisfactoryinthisregard,as itsusewasassociatedwithatwo-foldhigherchanceofAGA newborns.
Spontaneous and medically indicated preterm birth occursmoreoftenindiabeticpregnantwomenthanintheir non-diabeticpeers.5 Pretermnewborns haveahigherrate ofinfantmortalityandmorbiditywhencomparedwith chil-drenbornatterm.Short-termcomplicationsofprematurity arerelatedtothecardiovascularandrespiratorysystems21; disorderssuchascerebral palsymayoccurasalong-term neurodevelopmentalcomplication.22 Pretermnewbornsare morelikelytodevelophypertension,obesity,and cardiovas-culardiseaseinadulthood.23
Thepercentageofpreterminfantsinthisstudywas7.1%. Inotherstudies,thepercentageofpreterminfantsranged from4%to16%.5,6Thepresent studyshowedthatpreterm infantsare morecommonly born tomothers treated with insulin or the combination of metformin and insulin than tothose under diet therapy. These data corroborate the resultsofasimilarstudy.6Furthermore,thecomparisonof theprematurityoutcomebetweenthedietandmetformin therapiesshowednosignificantdifference,6similarlytothe presentstudy.
Giventhevariouscomplications towhichthechildofa motherwithGDMispredisposed,sometimesamore inten-sivetherapyisnecessary.ReasonsforNICUadmissioninclude congenitalabnormalities(suchascardiovascular malforma-tions),prematurity,perinatalasphyxia,respiratorydistress, andmetaboliccomplications(hypoglycemia,hypocalcemia, polycythemia,andhyperbilirubinemia), amongothers.5 In thepresentstudy,theNICUadmissionratewas5.1%.This value corroborates other values found in the literature (2%---6%),1,20butisdissimilarfromothers,inwhichtheneed forNICUadmissionrangedfrom15%6to23.5%.5
Inthepresentstudy,thetypeoftreatmentdidnotaffect theneedforNICUadmission,whileotherauthorsfoundthat infantsborntowomentreatedwithinsulinhadhigherrates of NICU admission when compared with pregnant women whoreceivedtreatmentwithmetforminordiettherapy.6
Sincepregnantdiabeticwomenhaveahigherriskof hav-ingLGAchildren,theindicationforcesareandeliveriesmay increase.Thepurposeofthistypeofdeliveryistoprevent trauma during thebirth of infants withestimated weight
≥4500g.17
thecesareansectionwasmoreprevalentinwomentreated withinsulin.6
TheApgarscoreisusedasanevaluationmethodofthe newborn’sbirthqualitybetweenthefirstandfifthminutes oflife.27Itassessestheimmediateadjustmentofthe new-born to extrauterine life, analyzing the baby’s vitality. It consists of the evaluation of five items of the newborn’s physicalexamination:heartrate,respiratoryeffort,muscle tone,reflexirritability,andskincolor.27
The Apgar score at the first minute is considered a diagnosis ofthe present situation, an indexthat can rep-resentasignofasphyxiation andtheneedfor mechanical ventilation.27 AsfortheApgar scoreatthefifthminute,it isconsideredtobemoreaccurate,leadingtothe progno-sisofneurologicalhealthandoutcomessuchasneurological sequelaeordeath.27
Inthepresent population,similarlytootherstudies,5,26 therewasnoincreasedriskoflowApgar,eitheratthefirst orthefifthminute,accordingtothetherapyused.Thismay demonstratethesuccessinthecareprovidedtonewborns ofdiabeticmothers.28
Theoutcomesofcesarean deliveryandApgar scoresat thefirstandfifthminutesandneedforNICUadmissionwere notdifferentbetweenthetreatments.
Due to the methodology used in the study, there weresome limitations tothecomparisonof results, since few studies used the same method. Another point to be highlightedistheheterogeneityofparticipantsineach ther-apeuticmodalitygroup,becauseeachtreatmentwasaimed atadistinctprofileofpregnantwomen.
Itcanbeconcludedthatthepediatricianinthedelivery roomcan expect different outcomes for children born to diabeticmothersbasedonthetreatmentthatshereceived duringpregnancy.Womentreated withmetforminareless likelytohaveSGAchildrenandmorelikelytohaveanAGA child.Apregnantwomanwhowastreatedwithinsulinhas alowerchanceofhavingapretermchild.IftheGDM treat-mentofwasacombinationofinsulinandmetformin,there isahigherchanceofthechildbeingbornLGAandalower chanceofbeingpreterm.
Fortheotherassessedoutcomes(typeofdelivery,Apgar score,andneedforNICUadmission),therewereno differ-encesbetweentreatmentmodalities.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgment
ToDarcyVargasMaternityHospital.
References
1.Grandi C, Tapia JL, Cardoso VC. Impact of maternal dia-betes mellitus on mortalityand morbidityof very lowbirth weightinfants: amulticenterLatin Americastudy.JPediatr. 2015;91:234---41.
2.Ruholamin S, Eshaghian S, Allame Z. Neonatal outcomes in women with gestational diabetes mellitus treated with
metforminincomparewithinsulin:arandomizedclinicaltrial. JResMedSci.2014;19:970---5.
3.RibeiroMC,NakamuraMU,AbdoCH,TorloniMR,ScanavinoMde T,MattarR.Pregnancyandgestationaldiabetes:aprejudicial combinationtofemalesexualfunction?RevBrasGinecolObstet. 2011;33:219---24.
4.Hartling L, DrydenDM, Guthrie A, Muise M, Vandermeer B, DonovanL.Benefitsandharmsoftreatinggestationaldiabetes mellitus:a systematicreviewand meta-analysis forthe U.S. PreventiveServicesTaskForceand theNationalInstitutesof HealthOfficeofMedicalApplicationsofResearch.AnnIntern Med.2013;159:123---9.
5.MesdaghiniaE,Samimi M,Homaei Z,Saberi F,Moosavi SGA, YaribakhtM.Comparisonofnewbornoutcomesinwomenwith gestationaldiabetesmellitustreatedwithmetforminorinsulin: arandomisedblindedtrial.IntJPrevMed.2013;4:327---33.
6.GohJE,SadlerL,RowanJ.Metforminforgestationaldiabetes inroutineclinicalpractice.DiabetMed.2011;28:1082---7.
7.Poolsup N, Suksomboon N, Amin M. Efficacy and safety of oral antidiabetic drugs in comparison to insulin in treat-inggestationaldiabetesmellitus:ameta-analysis.PLoSONE. 2014;9:e109985.
8.BalaniJ,HyerSL,Rodin DA,ShehataH.Pregnancyoutcomes inwomenwithgestationaldiabetestreatedwithmetforminor insulin:acase---controlstudy.DiabetMed.2009;26:798---802.
9.RaiL,MeenakshiD,KamathA.Metformin---aconvenient alter-nativetoinsulinforIndianwomenwithdiabetesinpregnancy. IndianJMedSci.2009;63:491---7.
10.AmericanDiabetesAssociation.Classificationanddiagnosisof diabetesmellitus.DiabetesCare.2015;38:S8---16.
11.CoustanDR,LoweLP,MetzgerBE,DyerAR,TheHyperglycemia. AdversePregnancyOutcome(HAPO)study:pavingthewayfor newdiagnosticcriteriaforgestationaldiabetesmellitus.AmJ ObstetGynecol.2010;202:e1---6.
12.BerggrenEK,StuebeAM,BoggessKA.Excessmaternalweight gainandlargeforgestationalageriskamongwomenwith ges-tationaldiabetes.AmJPerinatol.2015;32:251---6.
13.Silva JC, Bertini AM, Ribeiro TE, de Carvalho LS, Melo MM, Barreto Neto L. Factors related to the presence of large for gestational age newborns in pregnant women with ges-tationaldiabetesmellitus.RevBrasGinecol Obstet.2009;31: 5---9.
14.BarnesRA,EdghillN,MackenzieJ,HoltersG,RossGP,Jalaludin BB,etal.Predictorsoflargeandsmallforgestationalage birth-weightinoffspringofwomenwithgestationaldiabetesmellitus. DiabetMed.2013;30:1040---6.
15.DaponteA,GuidozziF,MoisucD,MarineanuA.Managementof diabeticpregnantpatientsinatertiarycenterinthedeveloping world.IntJGynaecolObstet.1999;64:141---6.
16.RehderPM,PereiraBG,SilvaJLP.Gestationalandneonatal out-comesinwomenwithpositivescreeningfordiabetesmellitus and100goralglucosechallengetestnormal.RevBrasGinecol Obstet.2011;33:81---6.
17.BerntorpK,AnderbergE,ClaessonR,Ignell C,Källén K.The relativeimportanceofmaternalbodymassindexandglucose levelsfor prediction oflarge-for-gestational-age births.BMC PregnancyChildbirth.2015;15:280.
18.Bonomo M, Cetin I, Pisoni MP, Faden D, Mion E, Taricco E, et al. Flexible treatment of gestational diabetes modulated onultrasoundevaluationofintrauterinegrowth:acontrolled randomizedclinicaltrial.DiabetesMetab.2004;30:237---44.
19.LeguizamónG,vonStecherF.Thirdtrimesterglycemicprofiles andfetalgrowth.CurrDiabRep.2003;3:323---6.
20.AktünHL,UyanD,YorgunlarB,AcetM.Gestationaldiabetes mellitusscreeningandoutcomes.JTurkishGerGynecolAssoc. 2015;16:25---9.
case of maternal gestational diabetes? World J Diabetes. 2015;6:734---43.
22.MosterD,LieRT,Markestad T. Long-termmedical andsocial consequencesofpretermbirth.NEnglJMed.2008;359:262---73.
23.EvensenKA, Steinshamn S,Tjønna AE,Stølen T,Høydal MA, WisløffU,etal.Effectsofpretermbirthandfetalgrowth retar-dationoncardiovascularriskfactorsinyoungadulthood.Early HumDev.2009;85:239---45.
24.ÁRogviR,FormanJL,GreisenG.Prematurity, smallness-for-gestationalage and later hospital admissions:a nation-wide registrystudy.EarlyHumDev.2015;91:299---306.
25.InocêncioG,BragaA,LimaT,VieiraB,ZulmiraR,CarinhasM, etal.Whichfactorsinfluencethetypeofdeliveryandcesarean
sectionrateinwomenwithgestationaldiabetes?JReprodMed. 2015;60:529---34.
26.IjäsH,VääräsmäkiM,Morin-PapunenL,KeravuoR,EbelingT, SaarelaT,etal.Metforminshouldbeconsideredinthe treat-mentofgestationaldiabetes:aprospectiverandomisedstudy. BJOG.2011;118:880---5.
27.CaseyBM,McIntireDD,LevenoKJ.Thecontinuingvalueofthe Apgarscorefor theassessmentofnewborninfants.NEnglJ Med.2001;344:467---71.