BrazJOtorhinolaryngol.2015;81(4):439---446
www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
REVIEW
ARTICLE
Drug-induced
sleep
endoscopy
in
the
identification
of
obstruction
sites
in
patients
with
obstructive
sleep
apnea:
a
systematic
review
夽
,
夽夽
Alonc
¸o
da
Cunha
Viana
Jr.
a,b,∗,
Luiz
Claudio
Santos
Thuler
c,d,e,
Maria
Helena
de
Araújo-Melo
a,faPost-GraduatePrograminNeurology,UniversidadeFederaldoEstadodoRiodeJaneiro(UNIRIO),RiodeJaneiro,RJ,Brazil bHospitalNavalMarcílioDias(HNMD),RiodeJaneiro,RJ,Brazil
cInfectiousandParasiticDiseases,UniversidadeFederaldoRiodeJaneiro(UFRJ),RiodeJaneiro,RJ,Brazil dClinicalResearchandTechnologyIncorporation,InstitutoNacionaldeCâncer(INCA),RiodeJaneiro,RJ,Brazil eUniversidadeFederaldoEstadodoRiodeJaneiro(UNIRIO),RiodeJaneiro,RJ,Brazil
fClinicalResearchinInfectiousDiseases,Fundac¸ãoOswaldoCruz(FIOCRUZ),RiodeJaneiro,RJ,Brazil
Received5March2014;accepted11January2015
Availableonline9June2015
KEYWORDS Obstructivesleep apnea;
Sleepdisorders; Sleep;
Sleepmedicine specialty; Snoring; Endoscopy
Abstract
Introduction:Obstructivesleepapneasyndromehasmultifactorialcauses.Althoughindications forsurgeryareevaluatedbywell-knowndiagnostictestsintheawakestate,thesedonotalways correlatewithsatisfactorysurgicalresults.
Objective: Toundertakeasystematicreviewonendoscopyduringsleep,asoneelementofthe diagnosisroutine,aimingtoidentifyupperairwayobstructionsitesinadultpatientswithOSAS. Methods:Bymeansofelectronicdatabases,asystematicreviewwasperformedofstudiesusing drug-inducedsleependoscopytoidentifyobstructionsitesinpatientswithOSAS.
Results:Tenarticleswereselectedthatdemonstratedtheimportanceofidentifyingmultilevel obstruction,especiallyinrelationtoretrolingualandlaryngealcollapseinOSAS.
Conclusion: DISEisanadditionalmethodtorevealobstructionsitesthathavenotbeendetected inawakepatients.
© 2015Associac¸ãoBrasileira de Otorrinolaringologiae CirurgiaCérvico-Facial. Publishedby ElsevierEditoraLtda.Allrightsreserved.
夽 Pleasecitethisarticleas:VianaJr.AC,ThulerLCS,Araújo-MeloMH.Drug-inducedsleependoscopyintheidentificationofobstruction
sitesinpatientswithobstructivesleepapnea.BrazJOtorhinolaryngol.2015;81:439---46.
夽夽Institution:UniversidadeFederaldoEstadodoRiodeJaneiro(UNIRIO),RiodeJaneiro,RJ,Brazil.
∗Correspondingauthorat:RuaSenadorDantas,20/708,Centro,20031-204,RiodeJaneiro,RJ.
E-mail:aloncovianajr@gmail.com(A.C.VianaJr). http://dx.doi.org/10.1016/j.bjorl.2015.01.007
440 VianaJr.ACetal.
PALAVRAS-CHAVE Apneiadosonotipo obstrutiva;
Transtornosdosono; Endoscopia;
Medicinadosono; Sono;
Ronco
Endoscopiadosonoinduzidopordroganaidentificac¸ãodo(s)sítio(s)deobstruc¸ãoem pacientescomapneiaobstrutivadosono:revisãosistemática
Resumo
Introduc¸ão:A síndromedeapneiaobstrutivadosono(SAOS)apresentacausasmultifatoriais comindicac¸ãocirúrgicaavaliadapormeiodosexamesdiagnósticosconsagradosemvigília,que podem,porém,nãoassegurarresultadoscirúrgicossatisfatórios.
Objetivo:Realizarumarevisãosistemáticasobreaendoscopiadosono,comopartedarotina diagnóstica,empacientesadultoscomSAOSafimdeidentificarossítiosdeobstruc¸ãodavia aéreasuperior.
Método: Revisãosistemáticadaliteratura(RSL),apartirdebasesdedadoseletrônicas,dos estudosqueidentificaramossítiosdeobstruc¸ãoempacientescomSAOSapartirdaendoscopia dosonoinduzidopordroga(DISE).
Resultados: Foramselecionadosdezartigosquedemonstraramrelevâncianaidentificac¸ãodos multiníveis de obstruc¸ão,principalmente em relac¸ãoao colapsoretro-lingual e laríngeona SAOS.
Conclusão:DISEéummétodoadicionalnaidentificac¸ãodesítiosdeobstruc¸ãonãodetectáveis nopacienteemvigília.
©2015Associac¸ãoBrasileira deOtorrinolaringologiaeCirurgiaCérvico-Facial.Publicadopor ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
Obstructivesleepapnea syndrome(OSAS)ischaracterized byperiods of cessation(apnea) andreduction(hypopnea) of oronasal airflow during sleep accompanied by oxyhe-moglobindesaturation.Thisbreathingdisorderisaresultof abnormalanatomysuperimposedonphysiologicalor exces-sivereductionofmuscletoneduringsleep.1,2
Itaffectsapproximately2%offemalesand4%ofmales, withapeakincidence between40 and60 yearsofage in both sexes. It has high rates of morbidity and mortality, andis considered a publichealth problemdue to cardio-vascularoutcome,theriskofoccupationalandautomobile accidents,aswellasthepoorqualityoflife,with neurocog-nitiveimpairment.
Clinical symptoms are snoring, restless sleep,daytime fatigue, decreased intellectual capacity, and personality changes. Between 80% and 90% of individuals with OSAS areunawareoftheirdiagnosis,whichcanbeattainedmore accuratelyandeffectivelywiththeidentificationand indi-vidualizedanalysisofobstructionsites.3---6
Thediseasehasmultifactorialcauses,andpatientswith OSAS who receive recommendations for surgical inter-vention, by reputable diagnostic tests such as clinical examination, video examinations (nasal endoscopy, laryn-goscopy, nasofibrolaryngoscopy), cephalometry, computed tomography,andmagneticresonanceimaging,donot neces-sarilyobtainasatisfactoryanddefinitiveresultfromsurgery. Nasofibrolaryngoscopy(NFL)undersedation,alsoknownas drug-inducedsleependoscopy(DISE),maybeanimportant toolin locatingtheobstructionsiteinthesepatients,and thus allowing the best clinical and/or surgical approach, therebyimprovingthequalitative andquantitativeresults of treatment. Moreover,it could help prevent unrealistic expectations regarding the available treatment for each patient.
Therefore,theobjectiveofthisstudywastoperforma systematicliteraturereview(SLR)onsleependoscopyasa diagnostictoolinadultpatientswithOSAS,aimingto iden-tifyupperairwayobstructionsites.
Methods
BetweenOctober20thand30thof2013,articlesindexedin theelectronicdatabasesoftheMedicalLiteratureAnalysis and Retrieval System Online (MEDLINE), the Latin Ameri-canandCaribbeanHealthSciencesLiterature(LILACS),the Cochrane Central Registerof ControlledTrials (CENTRAL), and the Spanish Bibliographic Index of Health Sciences (IBECS)weresearchedat theRegionalLibraryofMedicine (BIREME). Additionally, a review of references from the selectedarticleswasperformedtoidentifyotherpotentially relevantstudies.
The descriptors used were: obstructive sleep apnea AND endoscopy ANDsleep, obtained fromthe descriptors in health sciences (DeCS). Other searches were also per-formed, includingthe descriptorsin English (MeSHterms: Sleep Apnea Syndromes, Sleep Disorders, Sleep Apnea, Obstructive,Endoscopy,Sleep)butitwasobservedthatthe abovesearchrepeatedallthestudiesthatwerepresentin thefirst.
Drug-inducedsleependoscopyinobstructivesleepapneapatients 441
174 identified titles
33 abstracts included for assessment
12 articles eligible for detailed analysis
8 articles included in the review
10 final articles
• 2 inclusions: references • 4 exclusions: outcome was not of interest
• 21 exclusions by the abstract • 141 exclusions by the title
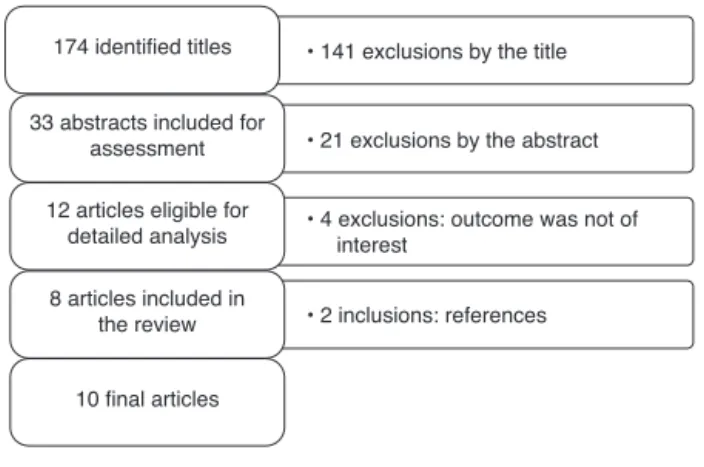
Figure1 Flowchartofarticleselection.
Epidemiology), an initiative of 2007, in the version translatedintoPortuguesein2010.7STROBEprovidesa
rec-ommendationonhowtoreportanobservationalstudymore adequatelywithoutanyreferencetothestudyquality.For thatpurpose,theauthorsusedthestrengthof recommen-dation and level of evidence of diagnostic studies based onthestudydesign, accordingtothe‘‘OxfordCenterFor Evidence-basedMedicine’’---lastupdatedin2011.8
A total of 174 titles were identified in the following databases: MEDLINE (160), LILACS (7), CENTRAL (4), and IBECS (3). Fig. 1 shows the flowchart of article selection includedinthisreview.Lookingforstudiesthathadas out-comeupperairwayobstructionsitesinpatientswithOSAS basedonsleependoscopyresults,usingmidazolamand/or propofol, the articleswere initially analyzed by title and thoseselectedwereevaluatedbasedontheabstractinthe nextphaseandsubsequently,thefulltexts.
Results
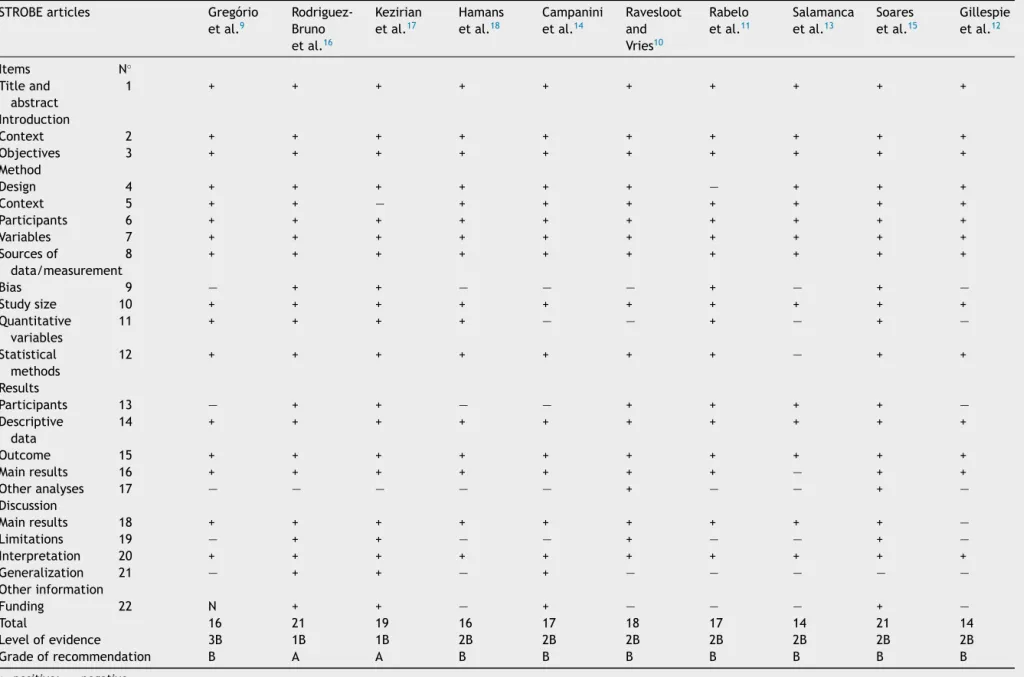
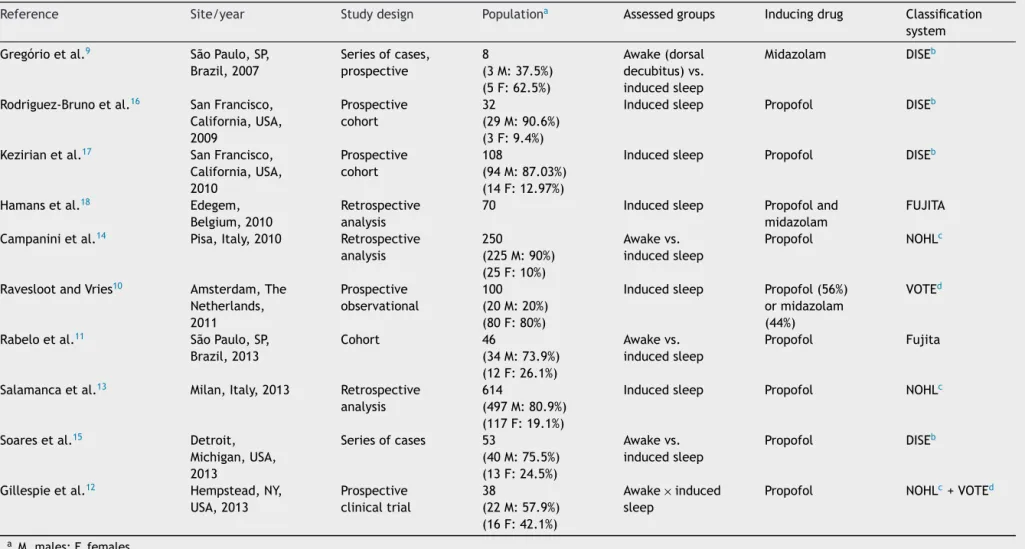
A total of ten articles were included in this systematic review,publishedbetween theyears 2007and 2013,with thenumber ofpatients ranging fromeightto614 individ-uals.Thenumberofessentialitemsidentifiedinthestudies, accordingtoSTROBE,rangedfrom14to21,withamedian of17,asshowninTable1.Thedegreeofrecommendations ofthestudiesrangedfromAtoB.Thisassignmentof qual-itative categoriestogradesof recommendationsindicates strongandmoderateevidence,respectively.
Thestudiesusedmidazolam9,10andpropofol10---17to
per-form sedation for nasofibrolaryngoscopy, either alone or associated.18Thetypesofclassificationsusedinthe
identifi-cationofobstructionsitesvariedamongstudiesandusedthe ownparametersofDISE,9,11,16,18theFujitaclassification,11,18
velumoropharynxtongue-baseepiglottis(VOTE),13 ornose
oropharynx hypopharynx larynx (NOHL).13,14 All selected
studieswerefavorabletotheDISEasan importanttoolin theassessmentofobstructionsitesinpatientswithOSAS.
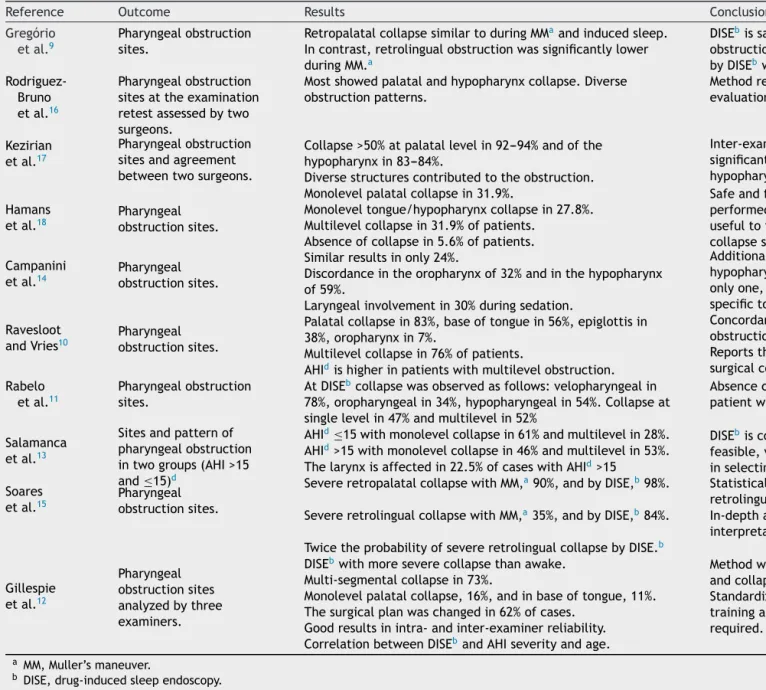
Rabelo et al., when analyzing a prospective cohort of 46 patients using the Fujita classification, found no concordance between the findings of patients assessedin wakefulnessandundersedation.Patientssubmittedtosleep endoscopyshowedinvolvementofthevelopharyngealregion in 78.26% of cases, oropharyngeal narrowing in 34.78%, and hypopharyngeal narrowing in 54.34%. Obstructions at
a single level were observed in 47.83%, while multilevel obstructions were observed in 52.17%.11 However, other
studiesevaluatingtheairwayduringwakefulnessandunder induced sleep did not differ significantly in the presence ofsevereretropalatalcollapse,butshowedsignificant dif-ference in the incidence of severe retrolingual collapse. Gregorio et al., when analyzing a small sample of eight patients, using midazolam to perform sedation, observed similarretropalatalobstructionduringtheMüllermaneuver (MM)andinducedsleep.Incontrast,retrolingualobstruction wassignificantlylowerduringMM.9
Hamans et al., in a retrospective analysis of 70 patients undergoing DISE with midazolam and propofol, found monolevel palatal collapse in 31.9%, monolevel tongue/hypopharynxcollapsein27.8%,andcollapseat sev-erallevelsin31.9%ofpatients.Nocollapsewasobservedin 5.6%ofpatients.Sleependoscopywasconsidered feasible andsafeindailypractice,whensedationisperformedbyan anesthesiologist,andishelpfulinlocatingthecollapsesite intheairway,whichmayinterferewithtreatmentchoices.18
RaveslootanddeVries,inaprospectiveanalysisof100 DISEsevaluatedusingtheVOTEclassification,foundseveral levelsof obstruction, present in 76 patients, statistically significantwhen associatedwithahigherapnea-hypopnea index(AHI),comparedtopatientswithobstructionata sin-glelevel.Theyfoundthatmostpatientshadobstructionat apalatallevel(83%),atthebaseofthetongue(56%),orat theepiglottis(38%).
Patientswith complete concentriccollapse of the soft palate were significantly more likely to have higher AHI andbodymassindex(BMI),while ananteroposteriorvelar collapse was significantly associated with a lower BMI. Moreover,theAHI wassignificantlyhigherinpatients with complete anterior-posterior collapse of the tongue. The observation of an obstruction at the base of the tongue orepiglottiswasmorecommoninpatientswithpositional OSAS;however,thisdifferencewasnotstatistically signif-icant(p=0.058).10 Gillespie etal., in aprospective study
with 38 patients, found multi-segmental airway collapse in73%of cases,uni-segmentalcollapse atpalatal levelin 16%,andat the base oftongue level in11%. The surgical planwaschangedafter sleependoscopyin 23cases(62%) andremainedunchangedin 14cases(38%).12Patientswith
complete concentriccollapse of thesoft palate were sig-nificantly more likely to have higher AHI and body mass index (BMI), while an anteroposterior velar collapse was significantly associated with a lower BMI. Moreover, the AHI was significantly higher in patients with complete anterior-posteriorcollapse ofthetongue.The observation of an obstruction at the base of the tongue or epiglottis wasmorecommonin patients withpositionalOSAS; how-ever, this difference was not statistically significant (p = 0.058).12 Gillespie et al., in a prospective study with 38 patients, also using the VOTE classification, found multi-segmentalairwaycollapsein 73%ofcases,uni-segmental collapseat palatallevelin16%,andatthebaseoftongue level in 11%. The surgical plan was changed after sleep endoscopy in 23 cases (62%) and remained unchanged in 14cases(38%).13
442
V
iana
Jr
.
AC
et
al.
Table1 AnalysisoftheselectedarticlesaccordingtotheSTROBEcriteria.7
STROBEarticles Gregório
etal.9
Rodriguez-Bruno
etal.16
Kezirian
etal.17
Hamans
etal.18
Campanini
etal.14
Ravesloot and
Vries10
Rabelo
etal.11
Salamanca
etal.13
Soares
etal.15
Gillespie
etal.12
Items N◦
Titleand
abstract
1 + + + + + + + + + +
Introduction
Context 2 + + + + + + + + + +
Objectives 3 + + + + + + + + + +
Method
Design 4 + + + + + + — + + +
Context 5 + + — + + + + + + +
Participants 6 + + + + + + + + + +
Variables 7 + + + + + + + + + +
Sourcesof
data/measurement
8 + + + + + + + + + +
Bias 9 — + + — — — + — + —
Studysize 10 + + + + + + + + + +
Quantitative variables
11 + + + + — — + — + —
Statistical methods
12 + + + + + + + — + +
Results
Participants 13 — + + — — + + + + —
Descriptive data
14 + + + + + + + + + +
Outcome 15 + + + + + + + + + +
Mainresults 16 + + + + + + + — + +
Otheranalyses 17 — — — — — + — — + —
Discussion
Mainresults 18 + + + + + + + + + —
Limitations 19 — + + — — + — — + —
Interpretation 20 + + + + + + + + + +
Generalization 21 — + + — + — — — — —
Otherinformation
Funding 22 N + + — + — — — + —
Total 16 21 19 16 17 18 17 14 21 14
Levelofevidence 3B 1B 1B 2B 2B 2B 2B 2B 2B 2B
Gradeofrecommendation B A A B B B B B B B
+,positive;—,negative.
STROBE2007:versiontranslatedintoPortuguesein2010.7
Drug-induced
sleep
endoscopy
in
obstructive
sleep
apnea
patients
443
Table2 Synthesisofthe10selectedarticles.
Reference Site/year Studydesign Populationa Assessedgroups Inducingdrug Classification
system
Gregórioetal.9 SãoPaulo,SP,
Brazil,2007
Seriesofcases,
prospective
8
(3M:37.5%)
(5F:62.5%)
Awake(dorsal
decubitus)vs.
inducedsleep
Midazolam DISEb
Rodriguez-Brunoetal.16 SanFrancisco,
California,USA,
2009
Prospective cohort
32
(29M:90.6%)
(3F:9.4%)
Inducedsleep Propofol DISEb
Kezirianetal.17 SanFrancisco,
California,USA,
2010
Prospective cohort
108
(94M:87.03%)
(14F:12.97%)
Inducedsleep Propofol DISEb
Hamansetal.18 Edegem,
Belgium,2010
Retrospective analysis
70 Inducedsleep Propofoland
midazolam
FUJITA
Campaninietal.14 Pisa,Italy,2010 Retrospective
analysis
250
(225M:90%)
(25F:10%)
Awakevs.
inducedsleep
Propofol NOHLc
RaveslootandVries10 Amsterdam,The
Netherlands, 2011
Prospective observational
100
(20M:20%)
(80F:80%)
Inducedsleep Propofol(56%)
ormidazolam
(44%)
VOTEd
Rabeloetal.11 SãoPaulo,SP,
Brazil,2013
Cohort 46
(34M:73.9%)
(12F:26.1%)
Awakevs.
inducedsleep
Propofol Fujita
Salamancaetal.13 Milan,Italy,2013 Retrospective
analysis
614
(497M:80.9%)
(117F:19.1%)
Inducedsleep Propofol NOHLc
Soaresetal.15 Detroit,
Michigan,USA,
2013
Seriesofcases 53
(40M:75.5%)
(13F:24.5%)
Awakevs.
inducedsleep
Propofol DISEb
Gillespieetal.12 Hempstead,NY,
USA,2013
Prospective
clinicaltrial
38
(22M:57.9%)
(16F:42.1%)
Awake×induced
sleep
Propofol NOHLc+VOTEd
a M,males;F,females.
444
V
iana
Jr
.
AC
et
al.
Table3 Synthesisofthetenselectedarticles(cont.).
Reference Outcome Results Conclusions
Gregório etal.9
Pharyngealobstruction
sites.
RetropalatalcollapsesimilartoduringMMaandinducedsleep.
Incontrast,retrolingualobstructionwassignificantlylower
duringMM.a
DISEbissafewithemphasisonretrolingual
obstruction.Theestimateoftheobstructionlevel
byDISEbwashigherthanMM.a
Rodriguez-Bruno
etal.16
Pharyngealobstruction
sitesattheexamination
retestassessedbytwo
surgeons.
Mostshowedpalatalandhypopharynxcollapse.Diverse
obstructionpatterns.
Methodreliabilityisgood,especiallyfor
evaluationofhypopharynxsites.
Kezirian
etal.17
Pharyngealobstruction
sitesandagreement
betweentwosurgeons.
Collapse>50%atpalatallevelin92---94%andofthe
hypopharynxin83---84%.
Inter-examinerreliabilityismoderateto
significant.Concordanceisgreaterinthe
hypopharynxassessment.
Diversestructurescontributedtotheobstruction.
Hamans
etal.18 Pharyngealobstructionsites.
Monolevelpalatalcollapsein31.9%. Safeandfeasiblemethodif
performedbyananesthesiologistand
usefultoidentifythepharyngeal
collapsesite.
Monoleveltongue/hypopharynxcollapsein27.8%.
Multilevelcollapsein31.9%ofpatients.
Absenceofcollapsein5.6%ofpatients.
Campanini
etal.14 Pharyngealobstructionsites.
Similarresultsinonly24%. Additionalusefulmethodfordetectingcollapseof
hypopharyngealandlaryngealsites.Itisnotthe
onlyone,butshouldbeconsideredanadditional
specifictoolinOSAS.c
Discordanceintheoropharynxof32%andinthehypopharynx
of59%.
Laryngealinvolvementin30%duringsedation.
Ravesloot
andVries10 Pharyngealobstructionsites.
Palatalcollapsein83%,baseoftonguein56%,epiglottisin
38%,oropharynxin7%.
Concordancebetweentheseverityofthe
obstructionsitesandtheseverityofAHI.d
ReportstheimportanceofDISEbinthe
surgicalconduct.
Multilevelcollapsein76%ofpatients.
AHIdishigherinpatientswithmultilevelobstruction.
Rabelo
etal.11
Pharyngealobstruction
sites.
AtDISEbcollapsewasobservedasfollows:velopharyngealin
78%,oropharyngealin34%,hypopharyngealin54%.Collapseat
singlelevelin47%andmultilevelin52%
Absenceconcordancebetweenthefindingsof
patientwhileawakeandundersedation.
Salamanca
etal.13
Sitesandpatternof
pharyngealobstruction
intwogroups(AHI>15
and≤15)d
AHId≤15withmonolevelcollapsein61%andmultilevelin28%. DISEbisconsideredsafe,easily
feasible,valid,reliable,andessential
inselectingtreatment.
AHId>15withmonolevelcollapsein46%andmultilevelin53%.
Thelarynxisaffectedin22.5%ofcaseswithAHId>15
Soares
etal.15 Pharyngealobstructionsites.
SevereretropalatalcollapsewithMM,a90%,andbyDISE,b98%. Statisticaldifferencesintheidentificationof
retrolingualcollapse.
SevereretrolingualcollapsewithMM,a35%,andbyDISE,b84%. In-depthanalysisoftechnique,training,and
interpretationisrequired.
TwicetheprobabilityofsevereretrolingualcollapsebyDISE.b
Gillespie
etal.12
Pharyngeal
obstructionsites
analyzedbythree
examiners.
DISEbwithmoreseverecollapsethanawake. Methodwithmoreinformationonpharyngealfunction
andcollapseassistinginthesurgicalconduct.
Multi-segmentalcollapsein73%.
Monolevelpalatalcollapse,16%,andinbaseoftongue,11%. Standardizationoftechnique,
trainingandinterpretationis
required.
Thesurgicalplanwaschangedin62%ofcases.
Goodresultsinintra-andinter-examinerreliability.
CorrelationbetweenDISEbandAHIseverityandage.
a MM,Muller’smaneuver.
Drug-inducedsleependoscopyinobstructivesleepapneapatients 445
EpworthSleepinessScale(ESS)orthequalityoflife assess-mentusingtheFunctionalOutcomesofSleepQuestionnaire (FOSQ). Thus,theincreasing DISEscoreseemstoindicate greaterseveritywhenmeasuredbyAHI.
Salamancaetal.usedtheNOHLclassificationsystemand reportedthe largest analyzed population of 614 patients, anddividedthe subjectsintothosewithAHI≤15andAHI
>15. They found in the first group, AHI ≤15 (32.4%), a
monolevelobstructionin61.3%(92.6%oropharynx)and mul-tilevelin28.2%(oro-andhypopharynx87.5%).Inthesecond group,AHI>15(67.6%),theyfoundonemonolevel obstruc-tion in 46.5% (95% oropharynx) and multilevel in 53.5% (obstruction of two levels in 91.5%, with oropharynx and hypopharynxobstructionin77%;obstructionofthreelevels in8.5%,withoropharynx,hypopharynx,andlarynx obstruc-tionin8.5%).Thelarynxparticipatedin12.5%ofcaseswith AHI>15.DISEwasconsideredasafe,easy-to-perform,valid, andreliableprocedure,inadditiontobeingconsideredby thegroupasanimportantclinicalassessmentthatmaybe essentialindeterminingtreatment.13
Campanini et al., with the second largest series (250 patients), also used the NOHL classification and demon-strated identicalobstruction sites identified at endoscopy during wakefulness and induced sleep in only 25% of patients.14 Soares etal., who retrospectively assessed 53
patients,showedthattheobservationsmadewhenawake and duringDISE were notsignificantly different regarding thepresence of severeretropalatal collapse,but differed significantly regarding the incidence of severe retrolin-gualcollapse (DISE84.9%;wakefulness 35.8%).Inpatients with Friedman I and II, regarding the tongue position, thedifferencewasevengreater (DISE88.9%; wakefulness 16.7%).15
Rodriguez-Brunoetal.prospectivelystudied32patients thatunderwenttwoseparate DISEassessments.The stud-ieswereevaluatedbyanon-blindedsurgeonandbyanother blindedsurgeon(whoonlyknewwhetherornotthepatient had undergone prior tonsillectomy). Almost all showed evidenceofobstructionatthepalatelevel;thevast major-ity also showed evidence at the hypopharynx level. The obstruction patterns were diverse. Test---retest reliability results were higher for the evaluations related to the hypopharynx. The two DISE studies were reviewed twice by each surgeon. They found good test---retest reliabil-ity (range 50---80%), mainly in airway assessment at the hypopharynxlevel.16 These findingswere similar tothose
found in the study of Gillespie et al., which assessed thetest---retestandinter-examinerreliabilityperformedby threeotorhinolaryngologistsqualifiedinDISEexaminations. The inter-examiner reliability,when blindlyand randomly assessed, demonstrated good results (K=0.65, K=0.62 betweenpairsofobservers).Test---retestreliabilitywasgood (K=0.61).12
Theinter-raterreliabilitywasalsoobservedbyKezirian etal.inaprospectivestudyof108patients,inwhichall sub-jectsexhibitedevidenceofpalatalobstructionandmostalso demonstratedhypopharyngealobstruction. Bothreviewers determinedthatmostindividualshadpalateand hypophar-ynxobstruction.Videoimagesweresubsequentlyreviewed by twosurgeons. The reliabilitybetween the presenceof obstructioninthepalateandthehypopharynx(K=0.76and
K=0.79, respectively) was higher than for the degree of
obstruction (weighted K-values=0.60 and 0.44). The reli-abilityoftheevaluationofthehypopharynxstructureswas greaterthanforthoseofthepalate.Ingeneral,DISE inter-observerreliabilityrangedfrommoderatetosubstantial.17
Thedetailedcharacteristicsofthestudiesaredescribed inTables2and3.
Discussion
Ananatomical,methodologicalapproach duringsleepcan be crucial to guide the surgeon during decision-making regardingtreatment. This review aimed to show therole of DISE as an additional method to identify the sites of obstructionthatwerenotdetectedbyothertests.Several authorshaveshownthat,whenincorrectlyorinsufficiently applied,the selection criteriausedfor surgical treatment may be responsible for the failure rates related to OSAS surgery.15,17,19
The number of articles found in the present review wassmall, indicating that there are few studies utilizing this approach. It is noteworthy that this review was sys-tematicallyperformedbyasingleresearcher. Studieswith differentdesigns were included and all of them included only individuals withOSAS. The assignment of qualitative categories tothe grades of recommendations of selected articles was strong and moderate evidence favored the practiceofsleependoscopyforobstructionsiteanalysisin thesepatients.
Results are still inconclusive regarding the type of obstruction, due to the difficulty with standardization amongthe studies.However,whenassessing thepatient’s obstruction sites while awake and under induced sleep, thestudies didnot differsignificantly regardingthe pres-ence of severe retro-palatal collapse, but did regarding theincidenceofsevereretrolingualcollapse.Furthermore, examinationsbyDISEhavedemonstratedasignificantrole oflaryngealobstructioninOSAS.
Sleependoscopyhasemergedasanimportanttechnique inidentifyingmultilevelcollapses,especiallyinthe position-ingofthebaseofthetongueandepiglottis.
There havebeen nostudiesthat assessed whetherthe findings obtained by DISE can predict success of surgical treatmentinpatientswithOSAS.Onlyonearticlereported that the findings changed the surgical indication12;
how-ever,itmadenoreferencetothesurgicalsuccessinthese patients. Sleependoscopy plays an important role in the identificationofmultilevelobstruction,withoutnecessarily ensuringtreatmentsuccesswhenthesesitesaresurgically addressed.
Although it was not the purpose of this review, it is pertinenttothefindingsdescribed inthe articlesthatwe findgoodtest---retestreliability, especiallyfor airwayand hypopharyngeal assessments, as well as good inter-rater reliability.
446 VianaJr.ACetal.
Conclusion
Despitethelackofstandardizationinclinicalexaminations, thetypeofdrugsusedforsedationandtheclassification sys-temused,theresultsobtainedtilldatefavortheinclusionof DISEintheinvestigationofobstructionsitesinpatientswith OSAS,particularlywithrespecttothelarynxand hypophar-ynx. The technique is valid, dynamic, safe, and easy to perform.TheVOTEclassificationsystemcurrentlyappears tobethemostused,asitiseasytoapply.Furthermore,the useofauniversalDISEscoringsystemcanfacilitatethe sci-entificassessmentofstudiesconductedinsinglecenters,as wellasmulticentricstudies,allowingcomparisonofresults.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Woodson BT, Wooten MR. Comparison of upper-airway evaluations during wakefulness and sleep. Laryngoscope. 1984;104:821---8.
2.StrohlKP,RedlineS.Recognitionofobstructivesleepapnea.Am JRespirCritCareMed.1996;154:279---89.
3.DykenME,SomersVK,YamadaT,RenZY,ZimmermanMB. Inves-tigatingtherelationshipbetweenstrokeandobstructivesleep apnea.Stroke.1996;27:401---7.
4.PhillipsonEA.Sleepapnea---amajorpublichealthproblem.N EnglJMed.1993;328:1271---3.
5.PeppardPE,YoungT,PaltaM,SkatrudJ.Prospectivestudyof theassociationbetweensleep-disorderedbreathingand hyper-tension.NEnglJMed.2000;342:1378---84.
6.ShaharE,WhitneyCW,RedlineS,LeeET,NewmanAB,NietoFJ, etal. Sleep-disorderedbreathingand cardiovasculardisease: cross-sectionalresultsoftheSleepHeartHealthstudy.AmJ RespirCritCareMed.2001;163:19---25.
7.MaltaM,CardosoLO,BastosFI,MagnaniniMMF,daSilvaCMFP. Iniciativa STROBE: subsídios para a comunicac¸ão de estudos observacionais.RevSaudePública.2010;44:559---65.
8.BallC,SackettD,PhillipsB,HaynesB,StrausS.Levelsof evi-denceandgradesofrecommendations.In:EBM(Websiteofthe OxfordCentreforEvidence-BasedMedicine)[cited12.06.14]. Availablefrom:www.cebm.net/levelsofevidence.asp 9.GregórioMG,JacomelliM,FigueiredoAC,CahaliMB,Pedreira
WL Jr, Lorenzi Filho G. Evaluation of airway obstruction by nasopharyngoscopy:comparisonoftheMüllermaneuverversus
inducedsleep.BrazJOtorhinolaryngol.2007;73:618---22. 10.RaveslootMJL,deVriesN.Onehundredconsecutivepatients
undergoingdrug-inducedsleependoscopy:resultsand evalua-tion.Laryngoscope.2011;121:2710---6.
11.RabeloFA,KüpperDS,SanderHH,SantosJúniorVD,ThulerE, FernandesRM,etal.AcomparisonoftheFujitaclassification ofawakeanddrug-induced sleependoscopypatients. BrazJ Otorhinolaryngol.2013;79:100---5.
12.Gillespie MB, Reddy RP, White DR, DiscoloCM, OverdykFJ, NguyenSA.Atrialofdrug-inducedsleependoscopyinthe surgi-calmanagementofsleep-disorderedbreathing.Laryngoscope. 2013;123:277---82.
13.SalamancaF, Costantini F,Bianchi A, Amaina T, ColomboE, Zibordi F.Identification of obstructive sites and patterns in obstructivesleepapneasyndrome bysleependoscopyin614 patients.ActaOtorhinolaryngolItal.2013;33:261---6.
14.CampaniniA,CanziP,DeVitoA,DallanI,MontevecchiF,Vicini C.Awakeversussleependoscopy:personalexperiencein250 OSAHSpatients.ActaOtorhinolaryngolItal.2010;30:73---7. 15.SoaresD,FolbeAJ,YooG,BadrMS,RowleyJA,LinHS.
Drug-inducedsleep endoscopyvs awakeMuller’s maneuver inthe diagnosisofsevereupperairwayobstruction.OtolaryngolHead NeckSurg.2013;148:151---6.
16.Rodriguez-Bruno K, Goldberg AN, McCulloch CE, Kezirian EJ. Test---retest reliability of drug-induced sleep endoscopy. OtolaryngolHeadNeckSurg.2009;140:646---51.
17.KezirianEJ,WhiteDP,MalhotraA,MaW,McCullochCE,Goldberg AN.Interraterreliabilityofdrug-inducedsleependoscopy.Arch OtolaryngolHeadNeckSurg.2010;136:393---7.
18.HamansE,MeeusO,BoudewynsA,SaldienV,VerbraeckenJ, VandeHeyningP.Outcomeofsleependoscopyinobstructive sleepapnea:theAntwerpexperience.B-ENT.2010;6:97---103. 19.denHerder C,vanTinteren H, de Vries N.Sleep endoscopy