Artigo Original
Adriana Ricarte1 Gisele Oliveira1 Mara Behlau1
Keywords
Voice Quality of life Validation studies Translation Dysphonia
Descritores
Voz Qualidade de Vida Estudos de validação Tradução Disfonia
Correspondence address:
Adriana Ricarte
R. Hélio Pradines, 737/602 , Ponta Verde, Maceió (AL), Brazil, CEP: 57035-220. E-mail: adriana_ricarte@hotmail.com
Received: 07/20/2011
Final paper of the specialization course in voice, Centro de Estudos da Voz – CEV – São Paulo (SP), Brazil. (1) Centro de Estudos da Voz – CEV – São Paulo (SP), Brasil.
Conlict of interest: nothing to declare.
Protocol in Brazil
Validação do protocolo Peril de Participação e Atividades
Vocais no Brasil
ABSTRACT
Purpose: The purpose of this study was to develop the Brazilian version of the Voice Activity and Participation Proile (VAPP) protocol and to demonstrate its measure properties so that it could be used as a self-evaluation instrument about the quality of life of Brazilian patients with vocal complaints. Methods: The translation and validation were performed following the guidelines of the Scientiic Advisory Committee of Medical Outcomes Trust. The instrument was administered to 50 patients, 25 with vocal complaint and 25 without it. The instrument was submitted to linguistic/cultural adaptation, validation, reliability, reproducibility, and responsiveness. The VAPP protocol is composed of 28 questions distributed into ive aspects: self-perception of the vocal problem intensity, effects at work, effects at daily communication, effects at social communication, and effects at emotion. Two additional scores are included: limitation in activities (LA) and participation restriction (PR). Results: The results showed that the Portuguese version of the VAPP protocol, called Peril de Participação e Atividades Vocais (PPAV), is valid and reliable, presenting an acceptable reproducibility level, considering p<0.05. Responsiveness to treatment was determined by signiicant changes between results before and after treatment (self-awareness of the vocal problem intensity: 5.33/0.35, effects at work: 12.40/1.93, effects at daily communication: 42.55/6.75, effects at social communication: 7.05/2.42, effects at emotion: 62.5/61.9; LA: 33.3/2.81; PR: 28.7/8.28). Conclusion: The Brazilian version of the VAPP protocol is valid, reliable, and responsive to changes. Therefore, it can be proposed as a useful instrument to evaluate quality of life of dysphonic patients and the treatment outcomes.
RESUMO
INTRODUCTION
According to the World Health Organization (WHO), health is a multidimensional concept that includes not only absence of disease, but also physical, mental, and social aspects(1). This concept was expanded incorporating the dei-nition of quality of life, which was deined as the perception that an individual has of his/her position in life, taking into consideration objectives; expectations; personal interests; and social, cultural, and economical patterns(1). The deini-tion of quality of life was introduced around two decades ago as an important issue in the clinical practice. Instruments that assess quality of life provide fast information about a person’s perception and the treatment outcomes(2).
Health evaluations are usually performed through clinical and/or laboratorial exams, although the WHO recommends the inclusion of a survey about the individual’s percep-tion of his/her health state in the clinical evaluapercep-tion(1). Therefore, instruments that assess treatment results and quality of life should be carefully developed and present proved psychometric measures of reliability, validity, and responsiveness(3,4). Most of the instruments about quality of life are developed in English, and in order that they are validated in other languages, they should be submitted to a cultural and linguistic adaptation, with a careful translation, following rules that were established in literature and, later, they should have their measure proprieties demonstrated in a speciic cultural context(5).
The quality of life of a subject can be affected due to con-ditions that interfere in his/her welfare, being both physical and psychological. Since dysphonia represents all and any dificulties or alterations in the vocal emission that hinders the natural production of voice, it can affect the quality of life of a subject with regard to personal, social, and profes-sional aspects. Ideally, the dysphonic patient exam should encompass detailed anamnesis and otorhinolaryngological and vocal evaluations(5). The accomplishment of such evalu-ations does not ensure the quantiication of the patient’s voice issue according to his/her perception(6). Frequently, the objective evaluations of a dysphonia may present results within the normality limits, while quality of life protocols and subjective analysis provide different information on the dificulty impact in the vocal production. Recently, re-search have showed the importance of including subjective parameters in the vocal assessment, not only focused on the perception of the professional evaluator but also on the patient’s self-perception as to the impact of vocal alteration in his/her life(7,8).
The Vocal Activity and Participation Proile (VAPP)(9) protocol was chosen based on the importance of using in Brazil an evaluation tool, which could approach the differ-ence between limitation of vocal issue and willingness of the subject to participate in daily activities in order to better conduct the treatment process. Although there are other protocols in Brazil that assess the impact of a dysphonia in the quality of life of a person with voice problem, this is the only one that includes an important issue proposed by
the International Classiication of Functionality, Incapacity, and Health (CIF) from the WHO, which is the participa-tion restricparticipa-tion (PR) and limitaparticipa-tion in activities (LA). Furthermore, the VAPP is one of the only instruments that approach aspects at work, in social and daily lives, and, when expressing emotions, offer therefore more details than the other validated instruments. This protocol has been used in studies that investigate the self-perception that people have of their own voices, mainly with those using them profes-sionally(10–12), and it has been validated in other languages(13). The objective of this study was to carry out the Brazilian version of VAPP protocol, concerning the self-evaluation impact of a dysphonia, which was developed in English, demonstrating its measure proprieties so that it can be used as an instrument to evaluate the quality of life of Brazilian patients with vocal complaints.
METHODS
This study was evaluated and approved by the Ethics Committee in Research of the Voice Study Centre (CEV), under report 4313/05. All participants were informed about the objectives of the study and agreed to participate by signing the Free Informed Consent. It is worth mention-ing that data collection was done at Hospital Beneicência Portuguesa de São Paulo.
The procedure for this research was performed in three stages: translation, cultural and linguistic adaptation, clini-cal and demographic characterization; and evaluation on the psychometric properties, which were developed according to the standards proposed by the Scientiic Advisory Committee of the Medical Outcomes Trust(14). The translation of the questionnaire was done by three bilingual speech therapists and the back-translation (to English) was developed by other two bilingual speech therapists who did not take part in the previous stage. The translators were informed about the objective and procedure of the research. A commission formed by three voice experts reviewed the stages and car-ried out consensual changes to produce the inal protocol.
For the accomplishment of the cultural and linguistic equivalence, 10 patients with vocal complaints that sought treatment in the Otorhinolaryngological Clinic of Hospital Beneicência de São Paulo were randomly chosen — six men and three women, with a mean age of 34 years. These partici-pants did not take part in the sample used to determine the protocol validation. To each question, the “non-applicable” option was added in order to identify the questions that were not understood or adequate for the population, which would be considered invalid for the culture at issue. There was no need to modify or eliminate any questions.
for treatment at Hospital Beneicência Portuguesa de São Paulo, in the Department of Otorhinolaryngology. They all took the otorhinolaryngological and speech therapy evalu-ations. None of them had undergone any previous treatment for voice, be it with medicine, surgery, or speech therapy. The group without vocal complaint was composed of 25 participants without vocal complaint who sought treatment at Hospital Beneicência Portuguesa de São Paulo, due to skin complaints (like acne and stains). The exclusion criteria adopted were age lower than 18 years and higher than 65 years old and presence of other communication disorders.
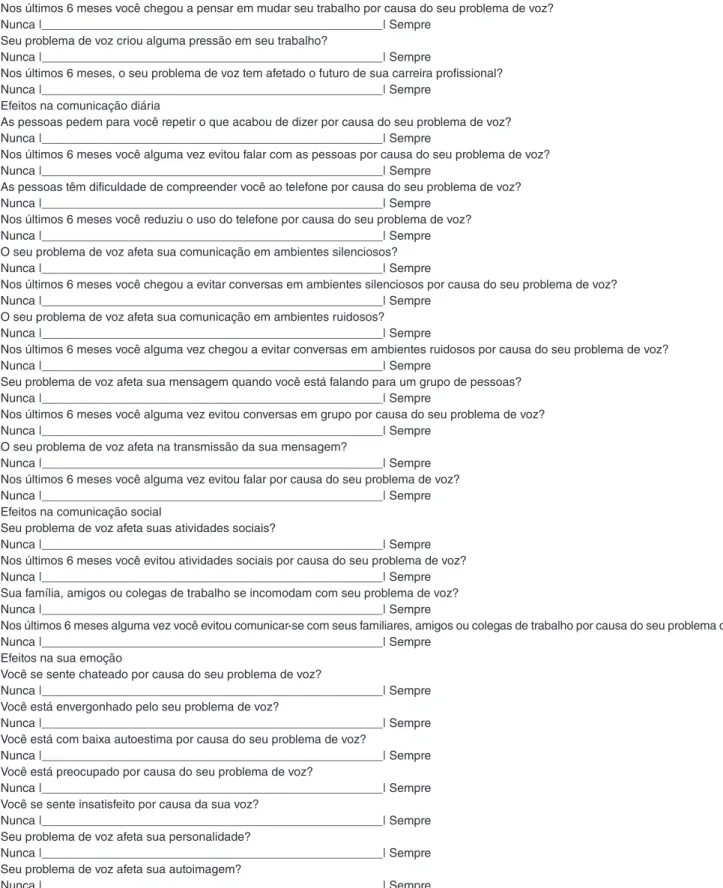
The VAPP protocol was named in Portuguese as “Peril de Participação e Atividades Vocais (PPAV)”(15). This is a questionnaire with 28 items developed speciically to evalu-ate the quality of life and the result of treatments of vocal disorders in dysphonic people. The items are distributed into ive aspects that produce a determined rank, which are self-perception of the vocal problem intensity with one question and maximum score of 10 points; effects at work, with four questions and maximum of 40 points; effects at daily com-munication, with 12 questions and maximum of 120 points; effects at social communication, with four questions and maximum score of 40 points; and effects at emotion, with seven questions and maximum score of 70 points. It also presents two additional scores, called limitation score in activities (LSA) and restriction score in participation (RSP), with maximum values of 100 points each. For LSA calcula-tion, the score of the 10 even questions must be summed involving the aspects “work”, “daily communication,” and “social communication” (questions 2, 4, 6, 8, 10, 12, 14, 16, 18, and 20); for the RSP calculation, the score of the 10 odd questions of the same previously mentioned aspects must be summed (questions 3, 5, 7, 9, 11, 13, 15, 17, 19, and 21). Higher the score, higher is the limitation in vocal activities (dificulties settled in the activities) and higher is the restriction in participation (participant decreases or avoids participating in activities that involve use of voice). The maximum score of this protocol, after summing all those of the questions, is 280 points.
The clinical and demographic characterization of the participants was done according to their ages, gender, occu-pations, type of dysphonia, and presence of vocal complaint. Participants were distributed into ive groups according to their occupation(16), associating the use of voice with de-mand and impact of an eventual dysphonia: level I — vocal elite, professionals whose careers can be severely affected due to a vocal alteration, such as singers and actors; level II — professional of the spoken voice for whom a vocal alteration of moderate grade could cause a professional impact, similar to what happens with most teachers; level III — nonprofessional voice user, whose occupational func-tions would be damaged only by a dysphonia with a very enhanced grade, like doctors and salespeople; and inally level IV — nonprofessional user, does not use voice and does not suffer limitations even in extreme conditions of vocal compromise, like drawers, computing programmers, among others. The introduction of another level, called level
V, for unemployed participants, retired people, students, and housewives was necessary.
Patients from the vocal complaint group were distrib-uted into three groups according to the dysphonia they presented: functional, organofunctional, and organic. This was done based on criteria used for classifying dysphonias, referring to another study(17). The functional dysphonia category includes patients with a deviation that has vocal compromising as the principle to develop vocal problem, with behavior changes, small structural changes, and psy-chogenic cases. The organofunctional category includes benign injuries, which are derived directly from vocal behavior, or which have an important role in causing such alteration, like nodules and polyps cases. Finally, the organic dysphonia category includes neurological and endocrine dysphonias, benign tumors, or larynx carcinoma, which are disorders caused by a series of processes that do not depend on voice use(17).
The psychometric propriety of reliability, which repre-sents the grade for which the protocol is free of presenting a random mistake(14), was analyzed based on the internal consistence by the Cronbach’s alfa correlation test and by the test-retest reproducibility. The validity, which is the grade for which the protocol assesses what is proposed(14), was determined by comparing VAPP scores of both groups with the represented self-vocal, obtained in three ways: related to content, to construct, and to criterion. The two irst ones are commonly done in the health ield, the third is hardly ever tested due to lack of widely accepted mea-sures. Responsiveness to treatment relects the ability of the protocol to identify important alterations in the directed problem(14); therefore there is a need to compare the groups before and after treatment. In our study, responsiveness was demonstrated approaching the irst aspect of the question-naire through Wilcoxon’s signed rank test. Reliability and reproducibility were determined by the test-retest and inter-nal consistence ainter-nalysis. The retest period varied from 2 to 14 days(7,18). Reproducibility was determined by Wilcoxon’s signed rank test and reliability by Cronbach’s alfa correlation coeficient test. Responsiveness to treatment was assessed through the comparison between scores before and after speech therapy, using Wilcoxon’s signed rank test.
For statistical analyses, the Statistical Package for Social Sciences program (SPSS), version 13.0, was used. The sig-niicance level was set at 5% (p<0.05).
RESULTS
The demographic characteristics were similar in both groups. The VAPP protocol scores were presented according to the type of dysphonia and professional voice use for the group with vocal complaint (Table 1).
Validity
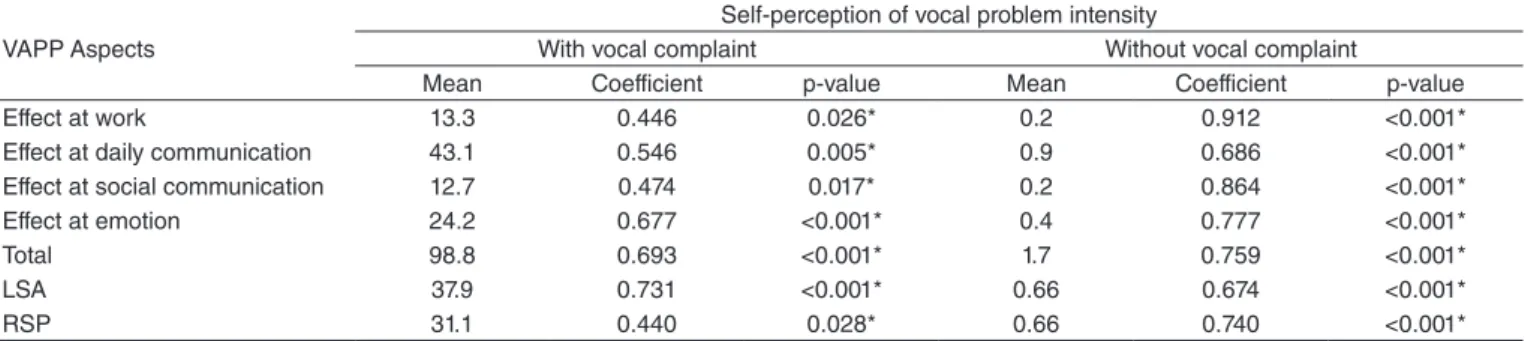
of people with and without vocal complaint. Therefore, the protocol validity calculation was carried out through Spearman’s correlation test (Table 2). The instrument showed a difference between both groups, because pa-tients with vocal complaint had higher scores than those without it.
Reliability
The instrument reliability was demonstrated by determin-ing the internal consistence (Table 3). The value from each test in every aspect was high, both in the total score and also in the additional ones. The correlation coeficients of each aspect and partial scores showed a positive correlation. The comparison of test-retest values presented an acceptable level of reproducibility (Table 4).
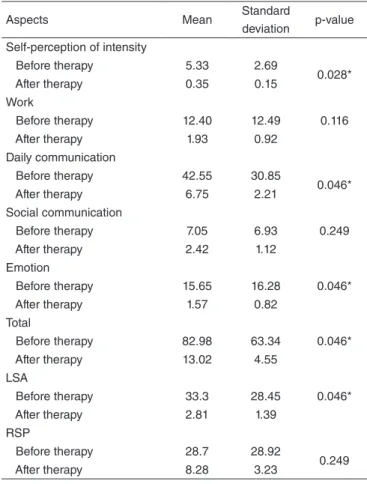
Responsiveness to treatment
The ability of evaluating the reaction to a treatment us-ing the protocol was tested, comparus-ing them to results from before and after speech therapy (Table 5). In the changes after treatment, there was a difference for the total score, for the self-perception of the vocal problem intensity, effects at social communication, effect at emotions, and rank of limita-tion of activities.
DISCUSSION
The development and validation of instruments that measure the quality of life have become an important focus on different areas in the health. Such instruments must be submitted to evaluation in different situations in order that their measure proprieties can be demonstrated(3,19,20). Most of the evaluation instruments concerning quality of life was developed in English(21). Therefore, it should be translated according to guidelines pre-established in literature for us-ing in other languages. The instruments should not only be
Table 1. Mean scores of the group including participants with vocal complaints according to the type of dysphonia and professional use of the voice
Variables Aspect 1 Aspect 2 Aspect 3 Aspect 4 Aspect 5 Total* LSA RSP
Dysphonia
Functional 5.41 15.10 27.59 12.26 19.59 79.94 31.68 23.25
Organic 6.13 6.50 47.20 6.17 7.23 73.23 25.93 33.93
Organofunctional 5.41 13.91 49.47 14.18 29.76 112.73 43.31 34.24
Occupation
Level I 6.73 24.07 41.40 9.57 34.30 116.07 19.80 6.50
Level II 4.34 13.39 41.83 13.06 17.60 90.21 48.53 39.46
Level III 1.64 4.52 12.91 3.92 8.46 31.45 36.76 30.58
Level IV 3.04 2.06 9.18 3.26 4.76 22.30 23.98 13.68
Level V 2.93 4.88 28.26 8.07 14.23 58.36 50.68 45.82
*Sum of the means of aspects.
Legend: Aspect 1 = self-perception of voice problem; Aspect 2 = effects at work; Aspect 3 = effects at daily communication; Aspect 4 = effects at social communication; Aspect 5 = effects at emotion; LSA = limitation score in activities; RSP = restriction score in participation
VAPP Aspects
Self-perception of vocal problem intensity
With vocal complaint Without vocal complaint
Mean Coefficient p-value Mean Coefficient p-value
Effect at work 13.3 0.446 0.026* 0.2 0.912 <0.001*
Effect at daily communication 43.1 0.546 0.005* 0.9 0.686 <0.001*
Effect at social communication 12.7 0.474 0.017* 0.2 0.864 <0.001*
Effect at emotion 24.2 0.677 <0.001* 0.4 0.777 <0.001*
Total 98.8 0.693 <0.001* 1.7 0.759 <0.001*
LSA 37.9 0.731 <0.001* 0.66 0.674 <0.001*
RSP 31.1 0.440 0.028* 0.66 0.740 <0.001*
*Significant values (p<0.05)—Spearman’s correlation test.
Legend: LSA = limitation score in activities; RSP = restriction score in participation
Table 3. Reliability calculation of VAPP: internal consistence of the total and additional aspects and scores
Aspectos Cronbach’s
alfa coefficient p-value Self-perception of the vocal problem
intensity 0.812 <0.001*
Effects at work 0.896 <0.001*
Effects at daily communication 0.920 <0.001* Effects at social communication 0.803 <0.001*
Effects at emotion 0.908 <0.001*
Total 0.754 <0.001*
LSA 0.920 <0.001*
RSP 0.812 <0.001*
*Significant values (p<0.05)—Cronbach’s alfa correlation coefficients. Legend: LSA = limitation score in activities; RSP = restriction score in participation
translated, but they should also present their psychometric measures tested in a speciic cultural context(3,14).
The quality of life evaluation is relevant not only to trace lines for medical acting but also to demonstrate eficiency and performance of the recent advances in Medicine, improv-ing the professional exercise in the health ield(22).
The results from this study showed that subjects with organofunctional dysphonias reported higher impact on their quality of life, presenting VAPP protocol scores su-perior to those people with other types of dysphonia. This result may happen due to an organofunctional change that is formed by the association of a behavioral problem with an injury in the vocal folds, which could limit these subjects’ vocal performance. Functional and organic dysphonias also presented high scores, reinforcing the negative impact of a dysphonia in several aspects of the speaker’s life. Level I occupations (singers and actors) had the highest total score means. It happened not only because they had great devia-tions, but also because dysphonia may be a limiting agent for the good professional return. Another hypothesis for the highest score between the other groups is that these people might consider any dysphonia symptom important, and therefore they look for professional help earlier, in order that such problem does not damage his/her professional and/or social lives(23) (Table 1).
Table 4. Reproducibility calculation for the VAPP: test–retest for repro-ducibility by aspects—total score and additional calculations
Aspects Mean Standard
deviation p-value Self-perception of intensity
Test 5.50 2.51
0.164
retest 5.56 2.36
Work
Test 13.36 11.81
0.246
retest 13.48 11.64
Daily communication
Test 43.07 29.67
0.345
Retest 43.38 29.25
Social communication
Test 12.68 10.84
0.618
Retest 12.56 11.11
Emotion
Test 24.21 17.73
0.367
Retest 23.06 18.13
Total
Test 98.81 60.63
0.545
Retest 98.04 59.08
LSA
Test 37.97 23.17
0.053
Retest 38.39 23.38
RSP
Test 31.13 25.23
0.957
Retest 25.23 24.52
Table 5. Calculation for responsiveness to VAPP treatment: difference of score mean of VAPP protocol in the group of participants with vocal complaint, before and after therapy
Aspects Mean Standard
deviation p-value
Self-perception of intensity
Before therapy 5.33 2.69
0.028*
After therapy 0.35 0.15
Work
Before therapy 12.40 12.49 0.116
After therapy 1.93 0.92
Daily communication
Before therapy 42.55 30.85
0.046*
After therapy 6.75 2.21
Social communication
Before therapy 7.05 6.93 0.249
After therapy 2.42 1.12
Emotion
Before therapy 15.65 16.28 0.046*
After therapy 1.57 0.82
Total
Before therapy 82.98 63.34 0.046*
After therapy 13.02 4.55
LSA
Before therapy 33.3 28.45 0.046*
After therapy 2.81 1.39
RSP
Before therapy 28.7 28.92
0.249
After therapy 8.28 3.23
The Brazilian version of VAPP had good performance as a vocal evaluation instrument in populations including dys-phonic patients. The instrument validity was demonstrated by a solid relation between self-perception of vocal problem intensity and mean scores of the aspects and additional cal-culations of VAPP protocol, as well as due to the signiicant differences between groups of people with and without vocal complaints (Table 2). Furthermore, results showed a positive correlation between vocal self-perception and VAPP protocol scores. If the vocal self-perception is worse, the rank in the protocol will be higher. Such correlation was also seen in the original study(9). The study data indicate that VAPP protocol is a responsive instrument to identify voice disorders. In the comparison between groups, the scores seen in individuals without complaints were lower than those in people with-out complaint. Similar results were also observed in other studies(15,24,25), in which dysphonic subjects presented higher scores than those from the Control Group.
The protocol reliability was demonstrated by determin-ing the internal consistence (Table 3) and the test–retest reproducibility (Table 4). The internal consistence of VAPP was measured by means of the Cronbach’s alfa statisti-cally high values. For the reproducibility, the protocol was
Wilcoxon’s signed rank test (p<0.05).
Legend: LSA = limitation score in activities; RSP = restriction score in participation
*Significant values (p<0.05) – Wilcoxon’s signed rank test.
Figure 1. Brazilian version of the VAPP(10).
Protocolo do perfil de participação e atividades vocais – PPAV Autopercepção do grau de seu problema vocal
O quanto o seu problema de voz é intenso?
Normal |___________________________________________________| Intenso Efeitos no trabalho
Seu trabalho é afetado pelo seu problema de voz?
Nunca |___________________________________________________| Sempre
Nos últimos 6 meses você chegou a pensar em mudar seu trabalho por causa do seu problema de voz? Nunca |___________________________________________________| Sempre
Seu problema de voz criou alguma pressão em seu trabalho?
Nunca |___________________________________________________| Sempre
Nos últimos 6 meses, o seu problema de voz tem afetado o futuro de sua carreira profissional? Nunca |___________________________________________________| Sempre
Efeitos na comunicação diária
As pessoas pedem para você repetir o que acabou de dizer por causa do seu problema de voz? Nunca |___________________________________________________| Sempre
Nos últimos 6 meses você alguma vez evitou falar com as pessoas por causa do seu problema de voz? Nunca |___________________________________________________| Sempre
As pessoas têm dificuldade de compreender você ao telefone por causa do seu problema de voz? Nunca |___________________________________________________| Sempre
Nos últimos 6 meses você reduziu o uso do telefone por causa do seu problema de voz? Nunca |___________________________________________________| Sempre O seu problema de voz afeta sua comunicação em ambientes silenciosos? Nunca |___________________________________________________| Sempre
Nos últimos 6 meses você chegou a evitar conversas em ambientes silenciosos por causa do seu problema de voz? Nunca |___________________________________________________| Sempre
O seu problema de voz afeta sua comunicação em ambientes ruidosos? Nunca |___________________________________________________| Sempre
Nos últimos 6 meses você alguma vez chegou a evitar conversas em ambientes ruidosos por causa do seu problema de voz? Nunca |___________________________________________________| Sempre
Seu problema de voz afeta sua mensagem quando você está falando para um grupo de pessoas? Nunca |___________________________________________________| Sempre
Nos últimos 6 meses você alguma vez evitou conversas em grupo por causa do seu problema de voz? Nunca |___________________________________________________| Sempre
O seu problema de voz afeta na transmissão da sua mensagem?
Nunca |___________________________________________________| Sempre Nos últimos 6 meses você alguma vez evitou falar por causa do seu problema de voz? Nunca |___________________________________________________| Sempre Efeitos na comunicação social
Seu problema de voz afeta suas atividades sociais?
Nunca |___________________________________________________| Sempre Nos últimos 6 meses você evitou atividades sociais por causa do seu problema de voz? Nunca |___________________________________________________| Sempre Sua família, amigos ou colegas de trabalho se incomodam com seu problema de voz? Nunca |___________________________________________________| Sempre
Nos últimos 6 meses alguma vez você evitou comunicar-se com seus familiares, amigos ou colegas de trabalho por causa do seu problema de voz? Nunca |___________________________________________________| Sempre
Efeitos na sua emoção
Você se sente chateado por causa do seu problema de voz?
Nunca |___________________________________________________| Sempre Você está envergonhado pelo seu problema de voz?
Nunca |___________________________________________________| Sempre Você está com baixa autoestima por causa do seu problema de voz?
Nunca |___________________________________________________| Sempre Você está preocupado por causa do seu problema de voz?
Nunca |___________________________________________________| Sempre Você se sente insatisfeito por causa da sua voz?
Nunca |___________________________________________________| Sempre Seu problema de voz afeta sua personalidade?
Nunca |___________________________________________________| Sempre Seu problema de voz afeta sua autoimagem?
applied twice, but the patient could not have undergone any treatment, once to obtain the test values and another for the retest amounts. The comparison of test–retest values, through Wilcoxon’s signed rank test, showed an accept-able level of reproducibility, because the results in both moments were similar (Table 4). Therefore, protocol reli-ability was determined by showing its internal consistence and reproducibility, as also seen in the validation study of the original questionnaire(9).
Voice changes after treatment are presented by the mean scores of VAPP protocol (Table 5). The present study showed that VAPP protocol is an instrument responsive to treatment. There were differences in most VAPP aspects, when the scores from before and after speech therapy treatment were compared. Likely, all scores may not have presented expressive differences due to the number of people who had undergone treatment, besides the fact that the tenth speech therapy session did not necessarily cor-respond to the speech therapy discharge. However, results were sufficient to demonstrate responsiveness to treatment, provided that the observed changes indicate an improve-ment of the voice pattern under the patient’s point of view and a reduction in the negative effects of a voice problem in the quality of life.
The protocol still presents two additional calculations, namely LSA and RSP. Results from these calculations create fundamental answers for the good performance in therapy, because from them a physician can know if the patient is not able to perform his/her activities or modifies his/her performance. Thus, it is possible to obtain data that can be approached in therapy directly. In this research, participants presenting vocal complaint showed higher limitations in performing professional activities, as well as other routine tasks due to the voice problem, than restricted directly to perform them. Other authors that applied VAPP have also seen this answer pattern(10,26).
The importance of development and validation of instru-ments that assess the effect of a vocal change in the quality of life of an individual is the main stage of an extensive and necessary process to establish self-perception measures. Such instruments are an important phase in the evaluation of a patient with vocal complaint, because they provide data concerning treatment evolution.
CONCLUSION
The Brazilian version of VAPP protocol is valid, reli-able, and responsive. It is an instrument directed specifi-cally to individuals with voice alterations and, thus, it is useful for evaluating the quality of life of dysphonic pa-tients and the results of their treatments.
*AR was in charge of data collection, tabulation, analysis and manuscript writing; GO was responsible for analysis and manuscript correction; MB was the advisor and responsible for scientific and final reviews
REFERENCES
1. World Health Organization. World Health Organization Quality: Measuring Quality of Life. Geneva: World Health Organization; 1997. WHO/MSA/MNH/PSF/97.4.
2. Ciconelli RM, Ferraz MB, Santos W, Meinão I, Quaresma MR. Tradução para a língua portuguesa e validação do questionário genérico de avaliação da qualidade de vida SF-36 (Brasil SF-36). Rev Bras Reumatol. 1999;39(3):143-50.
3. Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. 1993;46(12):1417-32. 4. Gill TM, Feinstein AR. A critical appraisal of the quality of
quality-of-life measurements. JAMA. 1994;272(8):619-26.
5. Gasparini G, Behlau M. Quality of life: validation of the Brazilian version of the voice-related quality of life (V-RQOL) measure. J Voice. 2009;23(1):76-81.
6. Benninger MS, Ahuja AS, Gardner G, Grywalski C. Assessing outcomes for dysphonic patients. J Voice. 1998 Dec;12(4):540-50. 7. Hogikyan ND, Sethuraman G. Validation of an instrument
to measure voice-related quality of life – V-RQOL. J Voice. 1999;13(4): 557-69.
8. Hogikyan ND. The voice-related quality of life (V-RQOL) measure: history and ongoing utility of a validated voice outcomes instrument. Voice Voice Dis. 2004;14(1):3-5.
9. Ma EP, Yiu EM. Voice activity and participation profile: assessing the impact of voice disorders on daily activities. J Speech Lang Hear Res. 2001;44(3):511-24.
10. Ricarte A, Bommarito S, Chiari B. Impacto vocal de professores. Rev CEFAC. 2011;13(4):719-27.
11. Ma EP, Yiu EM. Scaling voice activity limitation and participation restriction in dysphonic individuals. Folia Phoniatr Logop. 2007; 59(2):74-82.
12. Konnai RM, Jayaram M, Scherer RC. Developmente and validation of a voice disorder outcome profile for an Indian population. J Voice. 2010 Mar;24(2):206-20.
13. Sukanen O, Sihvo M, Rorarius E, Lehtihalmes M, Autio V, Kleemola L. Voice Activity and Participation Profile (VAPP) in assessing the effects of voice disorders on patients´ quality of life: validity and reliability of the Finnish version of VAPP. Logoped Phoniatr Vocol. 2007; 32(1):3-8.
14. Scientific Advisory Committee of Medical Outcomes Trust. Assessing health status and quality-of-life instruments: attributes and review criteria. Qual Life Res. 2002;11(3):193-205.
15. Behlau M, Santos LMA, Oliveira G. Cross-cultural adaptation and validation of the voice handicap index into Brazilian Portuguese. J Voice. 2011;25(3):354-9.
16. Koufman JA, Isaacson G. Voice disorders. Otolaryngol Clin North Am. 1991;24(5):989-98.
17. Behlau B, Madazio G, Feijó D, Pontes PAL. Avaliação da voz. In: Behlau, B. Voz: o livro do especialista. São Paulo: Revinter; 2001. p83-245.
18. Helidoni ME, Murry T, Moschandreas J, Lionis C, Printza A, Velegrakis GA. Cross-cultural adaptation and validation of the voice handicap index into Greek. J Voice. 2010;24(2):221-7.
19. Guyatt GH, Veldhuyzen Van Zanten SJ, Feeny DH, Patrick DL. Measuring quality of life in clinical trials: a taxonomy and review. CMAJ. 1989;140(12):1441-8.
20. Barbotte E, Guillemin F, Chau N, Lorhandicap Group. Prevalence of impairments, disabilities, handicaps and quality of life in the general population: a review of recent literature. Bull World Health Organ. 2001;79(11):1047-55.
22. Roper WL, Winkenwerder W, Hackbarth GM, Krakauer H. Effectiveness in health care: an initiative to evaluate and improve medical practice. N Engl J Med. 1988;319(18):1197-202.
23. Putnoki DS, Hara F, Oliveira G, Behlau M. Qualidade de vida em voz: o impacto de uma disfonia de acordo com o gênero, idade e uso vocal profissional. Rev Soc Bras Fonoaudiol. 2010; 15(4): 485-90.
24. Amir O, Ashkenazi O, Leibovitzh T, Michael O, Tavor Y, Wolf M. Applying the Voice Handicap Index (VHI) to dysphonic and nondysphonic Hebrew speakers. J Voice. 2006;20(2):318-24.
25. Guimarães I, Abberton E. An investigation of the Voice Handicap Index with speakers of Portuguese: preliminary data. J Voice. 2004;18(1):71-82. 26. Kasama ST, Brassolotto AG. Percepção vocal e qualidade de vida. Pro