RevPaulPediatr.2016;34(1):132---135
www.rpped.com.br
REVISTA
PAULISTA
DE
PEDIATRIA
CASE
REPORT
Neonatal
atrial
flutter
after
insertion
of
an
intracardiac
umbilical
venous
catheter
Marcos
Moura
de
Almeida
∗,
Wládia
Gislaynne
de
Sousa
Tavares,
Maria
Mônica
Alencar
Araripe
Furtado,
Maria
Marcia
Farias
Trajano
Fontenele
MaternidadeEscolaAssisChateaubriand,UniversidadeFederaldoCeará(UFC),Fortaleza,Ceará,Brazil
Received28January2015;accepted15May2015 Availableonline19October2015
KEYWORDS
Atrialflutter; Catheters; Newborn
Abstract
Objective: Todescribeacaseofneonatalatrialflutteraftertheinsertionofanintracardiac umbilicalvenouscatheter,reportingtheclinicalpresentationandreviewingtheliteratureon thissubject.
Casedescription: Alate-pretermnewborn,bornat35weeksofgestationalagetoadiabetic motherandlargeforgestationalage,withrespiratorydistressandrule-outsepsis,requiredan umbilicalvenousaccess.Aftertheinsertionoftheumbilicalvenouscatheter,thepatient pre-sentedwithtachycardia.Chestradiographyshowedthatthecatheterwasplacedintheposition thatcorrespondstotheleftatrium,andtractionwasapplied.Thepatientpersistedwith tachy-cardia,andanelectrocardiogramshowed atrialflutter.Asthepatientwashemodynamically unstable,electriccardioversionwassuccessfullyapplied.
Comments: Theassociationbetweenatrialarrhythmiasandmisplacedumbilicalcathetershas beendescribedintheliterature,butinthiscase,itisnoteworthythatthepatientwasaninfant borntoadiabeticmother,whichconsistsinanotherriskfactorforheartarrhythmias.Isolated atrialflutterisararetachyarrhythmiaintheneonatalperiodanditsidentificationisessential toestablishearlytreatmentandpreventsystemiccomplicationsandevendeath.
©2015SociedadedePediatriadeSãoPaulo.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBYlicense(https://creativecommons.org/licenses/by/4.0/).
PALAVRAS-CHAVE
Flutteratrial; Cateteres; Recém-nascido
Flutteratrialneonatalapósinserc¸ãodecateterumbilicalintracardíaco
Resumo
Objetivo: Descreverumcasodeflutteratrialneonatalapósainserc¸ãodeumcatetervenoso umbilical intracardíaco,relatando suaevoluc¸ão clínica,erealizaruma revisão bibliográfica sobreotema.
∗Correspondingauthor.
E-mails:marcosmalmeida@yahoo.com.br,marcosmouradealmeida@gmail.com(M.M.Almeida).
http://dx.doi.org/10.1016/j.rppede.2015.10.002
Neonatalatrialflutterafterinsertionofanintracardiacumbilicalvenouscatheter 133
Descric¸ãodocaso: Recém-nascidopré-termotardiode35 semanasdeidadegestacional,filho de mãe diabética, grande para a idade gestacional, com desconfortorespiratório precoce e risco para infecc¸ão neonatal, que necessitou de cateterizac¸ão venosa umbilical. Após o procedimento,opaciente apresentoutaquicardia. A radiografiatorácicaevidenciou posic¸ão intracardíaca inadequadadocateterumbilical,quefoitracionado,eoneonatopermaneceu taquicárdico.Oeletrocardiogramapermitiuodiagnósticodeflutteratrial.Porcontada insta-bilidadehemodinâmicafoirealizadacardioversãoelétrica,comsucesso.
Comentários: A relac¸ãoentre arritmiasatriaise cateteresumbilicais malposicionados tem sidodescritanaliteratura,mas,nestecaso,valeressaltarofatodeopacienteserfilhodemãe diabética,oqueconsisteemoutrofatorderiscoparaasarritmiascardíacas.Oflutteratrial isoladoéumataquiarritmiararanoperíodoneonatal,sendooseureconhecimentofundamental paraumtratamentoprecoceeparaevitarcomplicac¸õessistêmicaseatémesmofatais. ©2015SociedadedePediatriadeSãoPaulo.PublicadoporElsevierEditoraLtda.Esteéumartigo OpenAccesssobalicençaCCBY(https://creativecommons.org/licenses/by/4.0/deed.pt).
Introduction
Atrial flutteris arare arrhythmia in the neonatalperiod. Itslowincidencemakesitdifficulttocarryoutstudiesand justifies the smallnumber of publications about the best treatmentandlong-termprognosis.1,2
Umbilical catheterization is commonly used in neona-tal management for the administration of parenteral nutrition,hypertonicsolutions,bloodproducts,blood pres-sure monitoring andmedication infusion. This procedure, although easy to perform, has potential risks, including catheter-related infection, thrombosis, myocardial perfo-ration,pleuralandpericardial effusionsandarrhythmias.3
Catheters should ideally be positioned between the infe-rior vena cava and the right atrium. Catheters that go beyondtherightatriumcangetlodgedinthesuperiorvena cava,rightventricle,butusuallypassthroughtheforamen ovaleandbecomelodgedintheleftatrium,whichcanlead toendocardial injury.4 The association between umbilical
venous catheterizationand cardiac arrhythmias is mainly reportedwhenthecatheterismisplaced,inanintracardiac position.4---8
Abnormalities in the fetal heart rate occur in 2% of pregnancies.9 Fetuses of diabetic mothers require special
care, both in the prenatal and early neonatal periods. Thesenewbornsareusuallylargeforgestationalage(LGA), havehigheradmissionratesatneonatalintensivecareunits (NICUs)andhighermortalityratesthannewbornswhoare adequateforgestationalage,aswellasahigherfrequency ofatrialarrhythmia.9,10
TheaimofthisarticleistoreportacaseofanLGA new-born,borntoadiabeticmother,whodevelopedatrialflutter after the placement of an intracardiac umbilical venous catheter,reportingtheclinical outcomeand performinga briefliteraturereviewonthetopic.
Case
description
Thepatientwasaninfantborntoadiabeticmotherwith ges-tationalhypertensionandurinarytractinfection,ofwhich treatment wasstartedduring labor.The patientwasborn bycesareansectionduetoobstetricindicationat35weeks ofgestationalage,accordingtothelastmenstrualperiod,
withApgarscoresof3and8inthefirstandfifthminutesof life,respectively,andbirthweightof3755gbeingclassified asLGAaccordingtoAlexander’scurveof referencevalues ofneonatalweight.11
Thepatienthadearlymildrespiratorydistress,withno other alterations in the physical examination and asymp-tomatichypoglycemiainthefirsthouroflife,resolvedafter formulaadministration. The newborn wasreferred tothe medium-riskneonatalunitusingoxygenwithinspiratory oxy-gen fraction of 40%. Ten hours after birth, the newborn showedworsenedrespiratorydistressandwasadmittedat the neonatal ICU for ventilatory support with continuous positiveairway pressure (CPAP) and early antibiotic ther-apy for rule-out sepsis. Umbilical venous catheterization wasperformed approximately12h after birth due tothe difficultyinobtainingperipheralvenousaccess.
Soon after the procedure, the patient showed persis-tenttachycardia(190---230beatsperminute)andworsening ofrespiratorypattern,requiringtrachealintubation.Chest radiography showed normal cardiac area,clear lungs and intracardiac umbilical catheter in the left atrium region (Fig. 1), which was repositioned. The patient, however, persistedwithtachycardia.Anelectrocardiogramwasthen performed,whichconfirmedthesupraventricular tachycar-dia,suggestiveofatrialflutter.
134 AlmeidaMMetal.
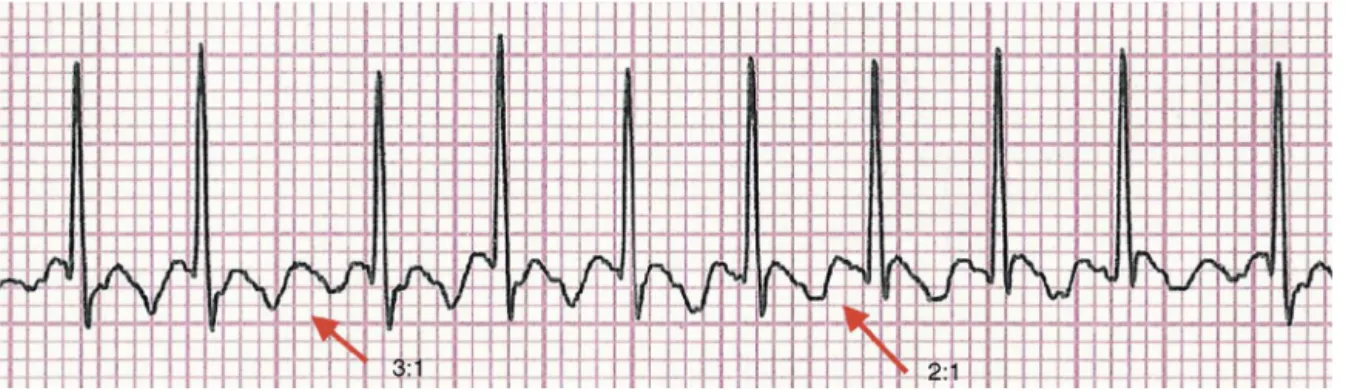
Figure2 Electrocardiogramshowingthe‘‘sawtooth’’or‘‘picketfence’’patternofatrialflutter,with3:1and2:1atrioventricular conductionintheD2lead.
The diagnosis was confirmed after adenosine adminis-tration(50mcg/kg/dose),whenthetypical‘‘sawtooth’’or ‘‘picketfence’’patternwasobservedinthePwave, char-acteristicof atrialflutter,with460atrialcontractionsper minute(Fig.2).Theinfantdevelopedhemodynamic insta-bility, weak pulses and slowed peripheral perfusion, thus beingsubmittedtoelectricalcardioversion(0.5J/kg),with sinusrhythmreturn.Administrationofamiodarone(5mg/kg) was initiated, and the newborn progressed with no new tachyarrhythmias,maintaininghemodynamic stability.The echocardiographyperformedonthedayaftercardioversion showedmildpulmonaryhypertensionanda2.6-mmpatent foramenovale.
Thepatientremainedstable,withprogressive improve-mentofrespiratorydistress, andwasextubatedafterfour days,beingdischargedfromtheneonatalICUateightdays old,asymptomatic.
Discussion
Atrialflutteristhemostcommonlyreported tachyarrhyth-miainthefetalperiod,beingrareinitsisolatedforminthe neonatalperiod.12 Itsetiologyisuncertain,butthereisan
associationwithstructuralheartdiseases,whichshouldbe promptlyruled out byechocardiography. The presence of structuralalterationsiscorrelatedwithworseprognosis.2
Thediagnosisisoftensimple,withtheelectrocardiogram showingthetypical‘‘sawtooth’’or‘‘picketfence’’pattern, betterobservedinleadsII,IIIandaVF.Theclinical presen-tationofatrialflutterdependsontheventricularresponse toatrialtachyarrhythmia.Innewborns,theatrialrateis400 beatsperminute(bpm),withanatrioventricularconduction ratioof2:1,resultinginaventricularrateofapproximately 200bpm.12 Thepatientdescribedhadaventricularrateof
around190---230bpmandatrialrateof380---460bpm. Complicationsrelatedtotheumbilicalvenous catheter-izationarereportedregardingitsinadequatepositioning.4---8
Therearemethodstodeterminethecorrectinsertionlength ofumbilicalvenouscatheters.13,14Oneapproachuses
equa-tionsbasedonthenewborn’sweight,asdescribedbyShukla etal.13 Dunn’smethod, the most commonly used one, is
basedonthemeasurementoftheshoulder-naveldistance. Thismethodishinderedbynumerousimportantlimitations, includinginterpersonalvariations.14Itisnotknownwhether
theestimated insertion lengthbased onthesemethods is
accurate.15 Once thepatientis catheterized,thelocation
isroutinelyverifiedbyachestX-ray.InchestX-raysinthe anteroposteriorview,theidealpositionforthecathetertip is located between the T8 and T9 thoracic vertebrae. In thisposition,90%ofthecatheterswillhavetheirdistalend placedbetweentherightatriumandtheinferiorvenacava. Itisnoteworthythat56%ofumbilicalvenouscatheters, when radiography was used to verify the location of the catheter tip, had to be repositioned because they were placed in an unsatisfactory site.16,17 When comparing the
methods to identify the correct position of catheters, ultrasound is a more accurate complementary method of examination than chestX-ray todetermine the route and thepositionofvenousumbilicalcatheters.16,17Thefirst
diffi-cultyistocrosstheductusvenosusandthenreachitscenter position.Thisdifficultyjustifiesthecomplicationsrelatedto poor positioning.16 In thepatientdescribedin thisreport,
the Dunn method was used as a reference for catheter positioning,withitspositionbeingassessedbychestX-ray, accordingtotheserviceroutine.
Theassociationbetweendiabeticmothersandnewborns withatrialarrhythmiashasbeenreportedintheliterature. Some studies have shown that fetuses and neonates with atrial tachyarrhythmiasare mostcommonly large for ges-tational age or the offspring of diabetic mothers, as the patientshownhere.Theyhavecardiacfunctionalterations, regardlessofthepresenceofventricularhypertrophy.There isthehypothesisthatdiastolicdysfunction,withsubsequent atrial dilation,maypredisposeinfants ofdiabeticmothers toatrialarrhythmias.9
Themanagementofnewbornswithcardiacarrhythmias secondarytoumbilicalvenouscatheterizationhasnotbeen systematically studied.As arrhythmiasoften occur dueto poor positioningof the catheter, the first step should be to pullit back or even remove the catheter.However, in ourcase,catheterpullbackwasnoteffective.Treatmentto bringtheheartbacktosinusrhythmcanbepharmacological (antiarrhythmics such asadenosine, digoxin, amiodarone, etc.) or electric (cardioversion or transesophageal atrial stimulation). Adenosine administration may be effective, butitdoesnotalwaystreattachycardiaofatrialorigin,such asatrialflutter,asseeninthepatientdescribedhere.18---20
Neonatalatrialflutterafterinsertionofanintracardiacumbilicalvenouscatheter 135
inadultsandchildren,arebeingstudied,suchasibutilide and propafenone, and there have been reports of their use in newborns.21,22 When there is no response to
phar-macologicaltreatment, therapy mayrequiresynchronized cardioversion or transesophageal atrial pacing, with high probabilityofsinus rhythmconversion.1,21---24 Incaseswith
hemodynamicinstability,electricalcardioversionshouldbe preferablyused,asinthecasereportedhere.
Leroyetal.5describedasimilarcase,inwhichafull-term
newborndevelopedatrial flutterafteranumbilicalvenous catheterwasplacedintheleftatrium.Treatmentconsisted inrepositioningthecatheterandtransesophagealatrial pac-ing,withgoodevolution.Sinhaetal.7alsoreportedapatient
withhemodynamicinstabilityduetoatrialflutterafter cath-eterization,resolvedaftersynchronizedcardioversion.
Fetalandneonatalatrialflutterisassociatedwith signif-icantmorbidity.However,mortalityseemstobemoreoften relatedtothepresenceofassociatedmedicalconditions.25
Pharmacologicalorelectricalcardioversiontonormalsinus rhythmmaybeeffectiveand,oncesuchreversalisachieved, thepatientdoes notseemtohavea riskof recurrenceof atrialflutter,exceptwhenthereisanaccessorypathway;in thiscase,supraventriculartachycardiaepisodesmayoccur. Inpatientswithout anaccessorypathway,it isnotusually necessarytomaintainthelong-termmedication.25
Considering the small amount of data available in the nationalandinternational literature,mainlyfromthe iso-lated case reports, thereis scarce informationabout the preciseassociation betweenneonatalarrhythmiasandthe umbilicalcatheterization,includingtheactualincidenceof atrialflutterandtheindicationofa‘‘universal’’therapeutic approachfor it.The association betweencardiac arrhyth-mias and maternal diabetes is a research field yet to be developed,whichcan contributetothepreventionof this disease,supportedbyabetterunderstandingofthe physio-pathologicalmechanismsoftheseentities.
Funding
Thisstudydidnotreceivefunding.
Conflicts
of
interest
Theauthorshavenoconflictsofinteresttodeclare.
References
1.TexterKM,KerteszNJ,FriedmanRA,FenrichALJr.Atrialflutter ininfants.JAmCollCardiol.2006;48:1040---6.
2.LisowskiLA, Verheijen PM, BenatarAA, Soyeur DJ, Stouten-beekP,Brenner JI, et al. Atrialflutter in the perinatalage group:diagnosis,managementandoutcome.JAmCollCardiol. 2000;35:771---7.
3.RamasethuJ.Complicationsofvascularcathetersinthe Neona-talIntensiveCareunit.ClinPerinatol.2008;35:199---222. 4.Hermansen MC, Hermansen MG. Intravascular catheter
complications in the neonatal intensive care unit. Clin Perinatol.2005;32:141---56.
5.LeroyV, BelinV, FarnouxC,Magnier S, Auburtin B, Gondon E,etal.Uneobservationdeflutterauriculaireaprèsposede cathéterveineuxombilical.ArchPediatr.2002;9:147---50. 6.Verheij G, Smits-Wintiens V, Rozendaal L, Bolm N, Walther
F,Lopriore E.Cardiac arrhythmiasassociated withumbilical venouscatheterisationinneonates.BMJCaseRep.2009:2009. 7.SinhaA,FernandesCJ,KimJJ,FenrichALJr,EncisoJ.Atrial flutterfollowingplacementofanumbilicalvenouscatheter.Am JPerinatol.2005;22:275---7.
8.HoganMJ.Neonatalvascularcathetersandtheircomplications. RadiolClinNorthAm.1999;37:1109---25.
9.Pike JI, Krishman A, Kaltman J, Donofrio MT. Fetal and neonatal atrial arrhythmias: an association with maternal diabetes and neonatal macrosomia. Prenat Diagn. 2013;33: 1152---7.
10.CorderoL,LandonMB.Infantofthediabeticmother.Clin Peri-natol.1993;20:635---48.
11.AlexanderGR,HimesJH,KaufmanRB,MorJ,KoganM.AUnited States national reference for fetal growth. Obstet Gynecol. 1996;87:163---8.
12.MendelsohnA,DickM2nd,SerwerGA.Naturalhistoryof iso-latedatrialflutterininfancy.JPediatr.1991;119:386---91. 13.Shukla H, Ferrara A. Rapid estimation of insertional length
of umbilical catheters in newborns. Am J Dis Child. 1986;140:786---8.
14.DunnPM.Localizationoftheumbilicalcatheterbypost-mortem measurement.ArchDisChild.1966;41:69---75.
15.VerheijGH,TePasAB,WitloxRS,Smitis-WintejensVE,Walther FJ, Lopriore E. Pooraccuracy of methods currently usedto determine umbilical catheter insertionlength. Int JPediatr. 2010;33:78---83.
16.GreenbergM,MovahedH,PetersonB,BejarR.Placementof umbilicalvenouscatheterswithuseofbedsidereal-time ultra-sonography.JPediatr.1995;126:633---5.
17.MichelF,Brevaut-MalatyV,PasqualiR,ThomachotL,VialetR, HassidS,etal.ComparisonofultrasoundandX-rayin determin-ingthepositionofumbilicalvenouscatheters.Resuscitation. 2012;83:705---9.
18.ClarkeB,TillJ,RowlandE,WardDE,BarnesPJ,Shinebourne EA.Rapidandsafeterminationofsupraventriculartachycardia inchildrenbyadenosine.Lancet.1987;1:299---301.
19.Till J, Shinebourne EA, Rigby ML, Clarke B, Ward DE, Row-landE.Efficacyand safetyofadenosinein thetreatmentof supraventriculartachycardiaininfantsandchildren.BrHeart J.1989;62:204---11.
20.Dixon J, Foster K, Wyllie J, Wren C.Guidelines and adeno-sine dosing in supraventricular tachycardia. Arch Dis Child. 2005;90:1190---1.
21.Konak M, Alp H, Tarakc¸ı N, Baysal T, Örs R. Successful treatment of atrial flutter with propafenone and synchro-nizedcardioversionin a newborn.IndianJPediatr. 2014;81: 413---4.
22.Prasad D, Snyder C, Ashwath R. Ibutilide therapy in atrial flutter conversion in neonates. Heart Rhythm. 2013;10: 1231---3.
23.BarclayRP,BarrDG.Directcurrentcardioversioninacaseof congenitalatrialflutter.ArchDisChild.1972;47:833---4. 24.KerrCR,GallagherJJ,SmithWM,SterbaR,GermanLD,Cook
L,etal.Theinductionofatrialflutterandfibrillationandthe terminationofatrialflutterbyesophagealpacing.PacingClin Electrophysiol.1983;6:60---72.