REVISTA
PAULISTA
DE
PEDIATRIA
www.rpped.com.br
CASE
REPORT
Septic
arthritis
by
Sphingobacterium
multivorum
in
immunocompromised
pediatric
patient
Maiana
Darwich
Mendes
∗,
Rafael
Ruiz
Cavallo,
Cecilia
Helena
Vieira
Franco
Godoy
Carvalhães,
Maria
Aparecida
Gadiani
Ferrarini
EscolaPaulistadeMedicinadaUniversidadeFederaldeSãoPaulo(Unifesp),SãoPaulo,SP,Brazil
Received13August2015;accepted1December2015 Availableonline3April2016
KEYWORDS
Arthritis;
Sphingobacterium; Bacteria
Abstract
Objective: Toreportacasesepticarthritiswithararepathogeninaimmunosuppressedchild.
Casedescription: Malepatient,6yearsold,hadlivertransplantfiveandhalfyearsagodueto biliaryatresia.Patientwasusingtacrolimus1mgq.12h.Thispatientstartedtohavepaininleft footandankleandhadoneepisodeoffever3daysbeforehospitaladmission.Physical exam-inationshowedweight17kg,height109cm,temperature36.4◦C,withpain,swellingandheat
intheleftankle, withoutotherclinicalsigns.Initialtests:hemoglobin11.7g/dL hematocrit 36.4%, leukocytecount 17,600L−1 (7%bandedneutrophils, 70%segmentedneutrophils,2%
eosinophils, basophils 1%, 13%lymphocytes, 7%monocytes) C-reactive protein 170.88mg/L. Joint ultrasound showed moderate effusion in the site. Patient was submitted to surgical procedureandSphingobacteriummultivorumwasisolatedfromtheeffusion. Thegermwas susceptibletobroadspectrumcephalosporins(ceftriaxoneandcefepime)andfluoroquinolones (ciprofloxacinandlevofloxacin),anditwasresistanttocarbapenemicantibioticsand amino-glycosides.Hewastreatedintravenouslywithoxacillinfor15daysandceftriaxonefor13days, andorallywithciprofloxacinfor15days,withgoodoutcome.
Comments: TheS.multivorumisagramnegativebacillusthatbelongstoFlavobacteriaceae familyanditisconsiderednon-pathogenic.Ithasrarelybeendescribedasacauseofinfections inhumans,especially inhospitalenvironmentandinimmunosuppressedpatients.Thiscase reportisrelevantforitsunusualetiologyandforthesiteaffected,whichmaybethefirstcase ofsepticarthritisdescribed.
©2016SociedadedePediatriadeS˜aoPaulo.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBYlicense(http://creativecommons.org/licenses/by/4.0/).
∗Correspondingauthor.
E-mail:maianamendes@msn.com(M.D.Mendes).
http://dx.doi.org/10.1016/j.rppede.2016.03.014
PALAVRAS-CHAVE
Artrite;
Sphingobacterium; Bactérias
ArtritesépticaporSphingobacteriummultivorumempacientepediátrico imunossuprimido
Resumo
Objetivo: Relatarumcasodeartritesépticadeetiologiararaemumacrianc¸aimunossuprimida.
Descric¸ãodocaso: Pacientemasculino,seisanos,transplantadohepáticohaviacincoanose meiodevidoàatresiadeviasbiliares,emusodetacrolimus1mgde12/12horas,inicioudorem péetornozeloesquerdoeumepisódiodefebretrêsdiasantesdainternac¸ão.Aoexamefísico, peso17 kg,estatura 109cm, temperaturade36,4◦C,comdor,edemaecalor notornozelo
esquerdoesemoutrasalterac¸ões.Exames daentrada:hemoglobina 11,7g/dL,hematócrito 36,4%,leucócitos,17.600/uL(7%bastões,70%segmentados,2%eosinófilos,1%basófilo,13% linfócitos,7%monócitos),proteínaCreativa170,88mg/L.Ultrassonografiaarticularevidenciou moderado derrameno recessotíbio talar anterior esquerdo. Feitalimpeza cirúrgicacomo isolamentodoS.multivorumnaculturadolíquidoarticular,suscetívelaumamploespectro decefalosporinas(cefepimeeceftriaxone)efluoroquinolonas(ciprofloxacinoelevofloxacino), esistenteacarbapenêmicoseaminoglicosídeos.Tratadocomoxacilinapor15diaseceftriaxone 13diasintravenosoeciprofloxacinaviaoralpormais15diascomboaevoluc¸ão.
Comentários: O Sphingobacterium multivorum é um bacilo gram negativo, pertencente à famíliaFlavobacteriaceae,considerado não patogênico, tem sidoraramente descrito como etiologia de infecc¸ões em seres humanos principalmente em ambientes hospitalares e em imunossuprimidos. Orelato deste caso é relevante por sua etiologia incomume pelo sítio acometido,podeseresteoprimeirocasodeartritesépticadescrito.
©2016SociedadedePediatriadeS˜aoPaulo.PublicadoporElsevierEditoraLtda.Esteéumartigo OpenAccesssobalicençaCCBY(https://creativecommons.org/licenses/by/4.0/deed.pt).
Introduction
Septicarthritisis causedby thepresence ofa pathogenic microorganisminthejointspaceandrepresentsa diagnos-tic and therapeutic challenge. It affects mainly children and Staphylococcus aureus is the most common etiologi-cal agent. The implementation of early and appropriate treatment is essential for a favorable evolution without sequelae.1
Unusualetiologiesofsepticarthritishavebeenreported, alsoinimmunocompetentchildren,asinthecasedescribed in India, from which Achromobacter xylosoxidans was isolated,2 but immunosuppression is a determining factor
regarding the presence of other etiological agents rather thanS.aureusandunfavorableevolution.
Immunocompromisedpatientsaremorelikelytodevelop infections with unusual etiologies, such as Mycoplasma hominis, which has been associated with septic arthri-tis in the immunosuppressed pediatric population.3 In
thesepatients, the diagnosis is often delayed, which can determine the evolution to erosive arthritis, joint space destructionandsepsis.4
Sphingobacteriummultivorumisagram-negative, sapro-phytic bacillus of the Flavobacteriaceae family, naturally foundinsoil,plantsandwater,5firstdescribedin1981.6It
wasconsiderednonpathogenicforalongtime,butforsome yearsnow it has been described as a cause of infectious processesinhumanbeings.7
The objectiveof this study is toreportthe case of an immunosuppressedpediatricpatientwhodevelopedseptic arthritisbyS.multivorum.
Case
description
Asix year-oldmalepatientwasadmittedtothePediatric EmergencyRoomwithahistoryofpainintheleftfootand ankle,togetherwithdifficultyinambulationfor fivedays, with reports of an isolated fever peak (39◦C) three days
beforeadmission.
Atadmission,hisweightwas17kg,height109cm,body mass indexof14.3,heart rateof 120bpm,blood pressure of95×62mmHg,temperatureof36.4◦C,withswellingand
warmthintheleftankleandmildpainatmobilization.The remainingphysicalexaminationwasuneventful.
Thepatientwasbornat39weeks,bycesareansection. Themotherreportedanuneventfulprenatalperiod.Onthe seconddayoflifethepatienthadjaundiceandwas submit-ted tophototherapy for eightdays.It progressedwithout improvementandhewasreferredforoutpatienttreatment. Atthreemonthsofage,hewasdiagnosedwithbiliaryatresia andatsixmonthshewassubmittedtolivertransplantation. Hehasreceivedimmunosuppressivemedicationsincethen (currently receiving tacrolimus, 1mg q.12hs). Due to the presence ofsome phenotypicdeviations andsinglekidney ontheright,heisalsofollowedbythegeneticsdisciplineof thesameinstitution,butstillwithoutadiagnosis.Hehasa normalkaryotype.HeisbeingfollowedattheChild Devel-opment Outpatient Clinicof the same service and all his vaccinesareup-to-dateforhisage.
Laboratory tests at admission: hemoglobin 11.7g/dL, hematocrit36.4%,whitebloodcellcountof17,600L−1(7%
170.88mg/L. The ultrasonography showed moderate joint effusionintheleftanteriortibiotalarrecess.
Thepatientwasadmittedandintravenoustherapywith oxacillin200mg/kg/daywasstarted.Twodaysafter admis-sion,the patientunderwentsurgical cleaning ofthe joint
together with drainage of secretions, which were sent
to culture without other joint fluid analysis. After two days, the partial result showed growth of gram-negative bacilli andceftriaxone (100mg/kg/day) wasassociated to oxacillin.
Thejointfluidcultureshowedbacterialgrowthonblood agar, in which they appeared as non-hemolytic colonies
of 1mm in diameter, convex, smooth, opaque after
48h-incubationat37◦
C.Bacterialidentificationwascarriedout withthePhoenix®automatedsystem,whichidentified
Sph-ingobacterium multivorum(90% certainty),with negative resultsforthel-glutamicacidtest.Additionaltests,suchas
thepositive responsetotheoxidase andureasetests and morphological characteristics and sensitivity profile con-firmedtheidentificationofthebacterium.
Antimicrobial susceptibility was tested using the
Phoenix® automatedsystem andinterpretedwiththeCLSI
document(M100S25).8 The isolatedbacteria were
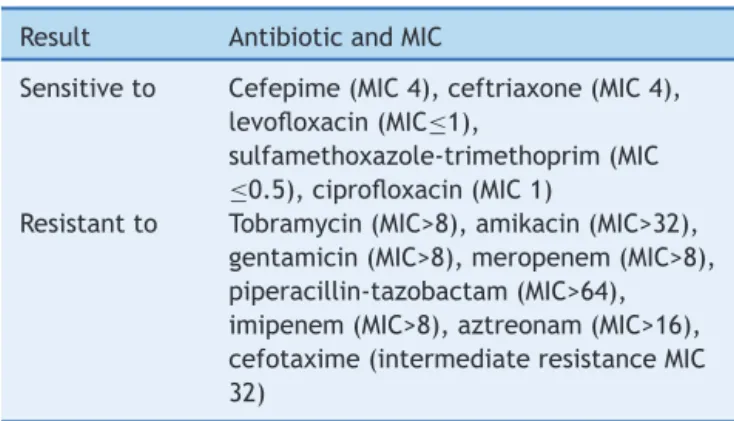
suscep-tible to a broad spectrum of cephalosporins (ceftriaxone and cefepime) and fluoroquinolones (ciprofloxacin and levofloxacin). Nevertheless, it showed a resistant pheno-typetocarbapenems(imipenemandmeropenem;minimum inhibitoryconcentration(MIC)>8mg/L)andaminoglycosides (Table1).
Treatment wasmaintained, asthepatientwasin good overall status, with no fever, no signs of inflammation in thejointandimprovementininflammatorytestsandwhite bloodcellcount.Onthe13thdayofoxacillinand11thday ofceftriaxoneuse,heshowedincreasedlivertransaminase levels (aspartate transaminase (AST) 115U/L and alanine transaminase (ALT) 114U/L, respectively) and pulse ther-apywasstarted(10mg/kgmethylprednisolone)fortwodays withdecreaseinliverenzymeslevels(AST:43U/LandALT: 79U/L).
He was dischargedafter 15 daysof amoxicillin and 13 days of ceftriaxone, with maintenance of oral treatment withciprofloxacinfor15days,accordingtotheantibiogram.
Table1 Sensitivityprofileoftheisolatedstraininthecase report.
Result AntibioticandMIC
Sensitiveto Cefepime(MIC4),ceftriaxone(MIC4), levofloxacin(MIC≤1),
sulfamethoxazole-trimethoprim(MIC
≤0.5),ciprofloxacin(MIC1)
Resistantto Tobramycin(MIC>8),amikacin(MIC>32), gentamicin(MIC>8),meropenem(MIC>8), piperacillin-tazobactam(MIC>64), imipenem(MIC>8),aztreonam(MIC>16), cefotaxime(intermediateresistanceMIC 32)
CentralLaboratoryofthehospitalwherethestudywascarried out.MIC(minimuminhibitoryconcentration):inmg/mL.
At discharge, he showed no signs of inflammation in the affectedjointandCRPwas2.8mg/L.
He returned to outpatient care 12 days after
dis-charge, stillreceiving ciprofloxacin 250mg q.12hs. At the
time, he was asymptomatic and had no complaints. The
antibiotic was maintained for three more days. At the
following consultation, 15 days later, he was clinically well and a new measurement of CRP was<0.6mg/L, one week afterthe end of treatment. At the monthly follow-up,the patient remainedasymptomatic, with nosigns of inflammation in the affected joint. He remains in outpa-tient treatment, with a follow-up schedule for at least oneyear.
Discussion
Thisisapatientwithsepticarthritiscausedbyabacterium thatrarelycausesinfectionsinhumansandtherehasbeen nodescriptionofpyoarthritiswiththisetiologytodate.The
Sphingobacteriummultivoruminitiallywasnotconsidered pathogenic,butinrecentyearsithasbeenrelatedto infec-tions,especiallyin-hospitalonesandinimmunosuppressed patients.7
Therehasbeenadescriptionofthisagentnotonlyin hos-pitalsbutalsoasacontaminantofpublictransportobjects inthecityofSãoPaulo,withresistancetocephalexinand cefazolin.9 The presence of this bacterium in the
envi-ronmenthas alreadyallowed itsinoculation in a prostate biopsyprocedure.10ThatdemonstratesthatS.multivorumis
presentintheenvironmentandmaybeaninfectiousagent, mainlyinimmunosuppressedindividuals.
In 1999, this bacterium was primarily related to opportunisticinfectionin patients withthe human immu-nodeficiency virus (HIV)7 and was later described as the
triggeringfactorofsepsisanddeathinapatientwiththis virus.11 S. multivorum has also been associated to
sep-sis under other circumstances, such as the duration of chemotherapy,12 hemodialysis13 and in an elderly patient
withchronic obstructive pulmonary disease, hypertension anddiabetes14;and inthe airwaycolonizationof patients
withcysticfibrosis,15,16butcasereportsofarthritiscaused
by this bacterium were not found in the literature. The patient’s age range is also noteworthy, as most infection reports by this microorganism describes the involvement ofadults andelderly patientswith comorbidities.8,11---16 In
2006, the first case of sepsis caused by S. multivorum
wasdescribed in Turkey,in apreviously healthy pediatric patient,who was treated withampicillin and cefotaxime andprogressedwithfullrecoverywithoutcomplications.17
Asummaryofthe17casesreportedintheliteratureisshown inTable2.
Another point to be emphasized is the importance of adequateantimicrobialtherapytobeimplementedinsuch cases.The susceptibilityprofile of thestrain described in thiscaseisinaccordancewithastudybyLambiaseetal., withacarbapenemandaminoglycosideresistanceprofile15;
however there is an account of respiratory infection by
S. multivorum in which a strain sensitive to Imipenem was demonstrated.18 The present study showed
Table2 SummaryofreportsofinfectionscausedbyS.multivorum. Authorandreference Patient’sage/siteof
infection/comorbidity
Treatment Evolution
Areekul11 47years/sepsis/HIVanddiabetes Gentamicinandampicillin. Subsequently,ceftriaxoneand sulfamethoxazole-trimethoprim
Death
Freney12 57years/sepsis/non-Hodgkin’s lymphoma
Pefloxacinand
sulfamethoxazole-trimethoprim
Full recovery Lambiase15 3positivesamplesin332patients
withcysticfibrosisandchronic pulmonaryinfection
Nodata Nodata
Aydo˘gan17 2months/sepsis/healthy Ampicillinandcefotaximefull recovery
Full recovery Ramírez18 74years/pneumonia/chronic
obstructivepulmonarydisease
Ceftazidime,cefuroxime. Full recovery Grimaldi5 64years/septicshock/obesityand
coronarydisease
Amoxicillinandclavulanate Full recovery Nielsen10 Studywith3patientsafterprostate
biopsy.
Patient1:79years/cystitis Patient2:59years/cystitis Patient3:69years/cystitis
1-Piperacilina-tazobactamand ciprofloxacin
2-Noantibiotics
3-Sulfamethoxazole-trimethoprim
Full recovery
Potvliege13 43years/sepsis/onhemodialysis Ampicillin Full
recovery Reina16 1yearand8months/cysticfibrosis Ceftazidimeandamikacin Full
recovery Barahona14 67years/sepsis/obesity,arterial
hypertensionandchronicobstructive pulmonarydisease
Cefepimeandvancomycin, ciprofloxacina
Full recovery
a study that showed the capacity of the bacterium to
cause hydrolysis of third-generation cephalosporins and carbapenems.19
In this case, both ciprofloxacin and sulfamethoxazole-trimethoprim could be used. However, the choice of ciprofloxacinfor oral therapyafterhospitaldischarge was duetothefactthattheetiologicalagenthadnotyetbeen described as the cause of septic arthritis in our country, due toits morphological similarity toPseudomonas,20 for
which this antibiotic would be a good choice, as well as thepatient’simmunosuppression.Studieshaveshownthat ciprofloxacin may beused in pediatric patients according totheanalysisof risksandbenefitsin each situation.21---23
Oneof theindications by theAmericanAcademy of Pedi-atricsandthe WorldHealthOrganizationwouldbeitsuse inbacterial infectionby gram negativemicroorganismsin immunosuppressedchildren.21,24
Itis noteworthythe relevanceofthe culturematerial, asit indicated thebroader spectrum of theantimicrobial therapy,whichallowedafavorableevolutionofthepatient’s condition.Earlydiagnosisofarthritisalsocontributedtothe absenceofcomplicationsandsequelae.
Infections by S. multivorum have been studied more frequently in recent years, but studies in the literature involving this pathogen are still scarce. No articles were found onseptic arthritisrelatedtothis bacterium, which makes it essential to report on the case of the studied patient.
Funding
Thisstudydidnotreceivefunding.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.ChenWL,Chang WN, ChenYS, HsiehKS,ChenCK, PengNJ, etal. Acutecommunity-acquired osteoarticular infectionsin children:highincidenceofconcomitantboneandjoint involve-ment.JMicrobiolImmunolInfect.2010;43:332---8.
2.SuryavanshiKT,LalwaniSK.Uncommonpathogen:serious man-ifestation:a rarecase ofachromobacterxylosoxidans septic arthritisinimmunocompetetantpatient.IndianJPathol Micro-biol.2015;58:395---7.
3.MianAN,Farney AC,MendleySR.Mycoplasma hominisseptic arthritisinapediatricrenaltransplantrecipient:casereport andreviewoftheliterature.AmJTransplant.2005;5:183---8. 4.Bloom KA, Chung D, Cunningham-Rundles C. Osteoarticular
infectiouscomplicationsinpatientswithprimary immunode-ficiencies.CurrOpinRheumatol.2008;20:480---5.
6.HolmesB,OwenRJ,WeaverRE.Flavobacteriummultivorum,a newspeciesisolatedfromhumanclinicalspecimensand pre-viously known as group IIk, biotype 2. Int JSyst Bacteriol. 1981;31:21---34.
7.Manfredi R, Nanetti A, Ferri M, Mastroianni A, Coronado OV,Chiodo F. Flavobacterium spp.organisms as opportunis-ticbacterialpathogensduringadvancedHIVdisease.JInfect. 1999;39:146---52.
8.ClinicalLaboratoryStandardsInstitute.Performancestandards forantimicrobialsusceptibilitytesting;twenty-second informa-tionalsupplement.Wayne:ClinicalandLaboratoryStandards; 2015.
9.Mendonc¸a RG,OlivalGS,Mímica LM,NavariniA,Paschoalotti MA,ChieffiPP. Potencialinfecciosodo transportepúblicode passageirosdacidadede SãoPaulo.ArqMedHospFacCienc MedSantaCasaSãoPaulo.2008;53:53---7.
10.Nielsen TK, Pinholt M, Nørgaard N, Mikines KJ. Inoculation ofSphingobacteriummultivorum in theprostate byprostate biopsy.ScandJUrol.2014;48:116---8.
11.Areekul S, Vongsthongsri U, Mookto T, Chettanadee S, WilairatanaP.Sphingobacteriummultivorumsepticemia:acase report.JMedAssocThail.1996;79:395---8.
12.FreneyJ,HansenW,PlotonC,MeugnierH,MadierS,Bornstein N,etal.SepticemiacausedbySphingobacteriummultivorum. JClinMicrobiol.1987;25:1126---8.
13.PotvliegeC,Dejaegher-BauduinC,HansenW,DratwaM,Collart F,TielemansC,etal.Flavobacteriummultivorumsepticemiain ahemodialyzedpatient.JClinMicrobiol.1984;19:568---9. 14.BarahonaF,SlimJ.Sphingobacteriummultivorum:casereport
andliteraturereview.NewMicrobesNewInfect.2015;16:33---6.
15.LambiaseA,RossanoF,DelPezzoM,RaiaV,SepeA,deGregorio F,etal.Sphingobacteriumrespiratorytractinfectioninpatients withcysticfibrosis.BMCResNotes.2009;2:262.
16.ReinaJ,BorrellN,FiguerolaJ.Sphingobacteriummultivorum isolatedfromapatientwithcysticfibrosis.EurJClinMicrobiol InfectDis.1992;11:81---2.
17.Aydo˘ganM,YumukZ,DündarV,ArisoyES.Sphingobacterium multivorumsepticemiainaninfant:reportofacaseandreview oftheliterature.TürkMikrobiyolCemiyDerg.2006;36:44---8. 18.Ramírez JC, Rodríguez AS. Infección respiratoria por
Sphin-gobacterium multivorum. Ann Med Interna (Madr). 2001;18: 655---6.
19.BlahováJ,KrálikováK,KrcméryVSr,KubonováK.Hydrolysis ofimipenem,meropenem,ceftazidime,andcefepimeby mul-tiresistantnosocomialstrainsofSphingobacteriummultivorum. EurJClinMicrobiolInfectDis.1997;16:178---80.
20.Public Health England. UKstandards for microbiology inves-tigations. Identification of Pseudomonas species and other nonglucosefermenters.Issueno.3;2015.p.1---41.
21.Committee on Infectious Diseases. The use of systemic flu-oroquinolones committee on infectious diseases. Pediatrics. 2006;118:1287---92.
22.ChoiSH,Kim EY,KimYJ.Systemic useoffluoroquinolonein children.KoreanJPediatr.2013;56:196---201.
23.VelissariouIM.Theuseoffluoroquinolonesinchildren:recent advances.ExpertRevAntiInfectTher.2006;4:853---60. 24.Switzerland---WHO. Fluoroquinolonesinchildren.In:Second