Braz. J. of Develop., Curitiba, v. 5, n. 11, p. 23751-23767 nov. 2019 ISSN 2525-8761 Adherence to non-pharmacological treatment for hypertension: impact of two
educational strategies on health and nutrition
Adesão ao tratamento não medicamentoso da hipertensão arterial: impacto de duas estratégias de educação em saúde e nutrição
DOI:10.34117/bjdv5n11-077
Recebimento dos originais: 14/10/2019 Aceitação para publicação: 07/11/2019
Aline Aparecida de Oliveira Campos 1
Doutora em Ciência da Nutrição - Universidade Federal do Sul e Sudeste do Pará (Unifesspa) - Instituto de Estudos em Saúde e Biológicas - Faculdade de Saúde Coletiva. Endereço: Avenida dos Ipês s/n - Marabá - Pará - Brasil. Contato: +55 (94) 2101-7116.
E-mail: aline.campos@unifesspa.edu.br Carla de Oliveira Barbosa Rosa
Doutora em Bioquímica Agrícola – Universidade Federal de Viçosa Departamento de Nutrição e Saúde
E-mail: carla.rosa@ufv.br Glauce Dias da Costa
Doutora em Ciência da Nutrição - Universidade Federal de Viçosa Departamento de Nutrição e Saúde.
E-mail: glauce.costa@ufv.br Flávia Mara de Oliveira Campos
Pós Graduada em Centro Cirúrgico e Central de Material pela Faculdade Unyleya E-mail: flamaracampos@yahoo.com.br
Tiago Ricardo Moreira
Doutor em Saúde Pública - Universidade Federal de Viçosa Departamento de Medicina e Enfermagem
E-mail: tiagoricardomoreira@gmail.com Rosângela Minardi Mitre Cotta
Doutora em Saúde Coletiva - Universidade Federal de Viçosa Departamento de Nutrição e Saúde
E-mail: rmmitre@ufv.br ABSTRACT
Objective: To compare the effect of two strategies of education in health and nutrition about adherence to non-pharmacological treatment of hypertension. Methods: a longitudinal intervention study, comparative test type community. The sample was composed of 84 individuals with hypertension, divided into two groups (group 1: educational workshops; Group 2: educational workshops and visits), accompanied by 5 consecutive months in 2016 in Viçosa, Brazil. Were evaluated anthropometric, biochemical, clinical and dietary requirements. For the analyzes were performed the Kolmogorov-Smirnov test, the Chi-square
Braz. J. of Develop., Curitiba, v. 5, n. 11, p. 23751-23767 nov. 2019 ISSN 2525-8761 test, Wilcoxon test, paired t-test, Mann Whitney test. Results: group 2 presented more satisfactory results when compared to group 1. To analyze the results before and after the activities carried out independent of the types of intervention, of the 17 variables analyzed, 12 were statistically significant. Conclusion: The educational workshops and visits were essential for the improvement of the quality of life of patients with arterial hypertension. However, it reinforces that visits is a privileged locus for the practice of nutritional counseling, because it contributed to the change of behavior patterns and increase the quality of life of patients with arterial hypertension.
Key words: hypertension, nutrition, health education, home visit, treatment adherence. RESUMO
Objetivo: comparar o efeito de duas estratégias educativas em nutrição acerca da adesão ao tratamento não medicamentoso da hipertensão arterial. Métodos: estudo de intervenção longitudinal, comparativo, do tipo ensaio comunitário, constituído por 84 indivíduos com hipertensão arterial, divididos em dois grupos (grupo 1: oficinas educativas; grupo 2: oficinas educativas e visitas domiciliares), acompanhados por 5 meses, em 2016 em Viçosa, Brasil. Foram avaliadas variáveis antropométricas, bioquímicas, dietéticas e clínicas. Foram realizados os testes Kolmogorov-Smirnov, Qui–Quadrado, Teste de Wilcoxon, Teste T pareado, Mann Whitney. Resultados: o grupo 2 apresentou resultados mais satisfatórios em relação ao ao grupo 1. Ao analisar os resultados antes e após as atividades realizadas independente do tipo de intervenção, das 17 variáveis analisadas, 12 foram estatisticamente significantes. Conclusão: as oficinas educativas e as visitas domiciliares foram essenciais para a melhora da qualidade de vida dos portadores de hipertensão arterial. Porém, reforça-se que a visita domiciliar é um lócus privilegiado para a prática do aconselhamento nutricional, pois contribuiu para a mudança de padrões de comportamento e aumento da qualidade de vida dos portadores de hipertensão arterial.
Palavras chave: hipertensão, nutrição, educação em saúde, visita domiciliar, adesão ao tratamento.
1 INTRODUCTION
Chronic non-communicable diseases, such as cardiovascular diseases, account for 17.9 million deaths per year worldwide. Arterial hypertension is a chronic disease of high prevalence, low control rates and is a risk factor for cardiovascular, cerebrovascular and renal diseases 1. However, its negative effects on the health of arterial hypertension carriers can be reduced when patients adhere to both pharmacological treatment and treatments related to changing lifestyle habits, the so called non-pharmacological treatments2.
Adherence means patients fulfilling therapeutic measures indicated by health professionals, whether related to medication intake, the adoption of a specific diet indicated for the carrier’s health status or lifestyle changes 3. Due to the many factors associated with hypertension treatment it is important that health actions are directed not only with drug treatment of this disease, but also with non- pharmacological therapy. Non- pharmacological
Braz. J. of Develop., Curitiba, v. 5, n. 11, p. 23751-23767 nov. 2019 ISSN 2525-8761 therapy is essential for control of arterial hypertension and other risk factors of cardiovascular diseases, such as obesity and dyslipidemia.
Among lifestyle habits, diet has a prominent place in changing the lives of individuals with arterial hypertension. Nutrition and health education must be developed to achieve healthier strategies that can improve quality of life4,5. In this sense, health education is of fundamental importance in relation to the promotion of healthier habits, as it promotes access to crucial knowledge of the disease which helps increase the capacity for better care and control.
However, scientific evidence shows that education activities on health and nutrition directed to arterial hypertension carriers are strictly guided by a biologicist and hygienist discourse, focused on the disease – on prescriptive and vertical information – which keeps arterial hypertension carriers ill-informed about their health status and unable to cope in their everyday life to minimize the complications of this disease 6,7 .
In this sense, the objective of this study was to compare the effects of two educational strategies in health and nutrition, regarding the adherence of arterial hypertension patients to non-pharmacological treatment, through anthropometric, clinical, biochemical and dietary parameters.
2 METHODS
This is a longitudinal intervention study, comparative and community based, that was randomized by lottery and not blind, having a quantitative approach and conducted with 84 arterial hypertension carriers from a Viçosa, municipality of Brazil in 2016.
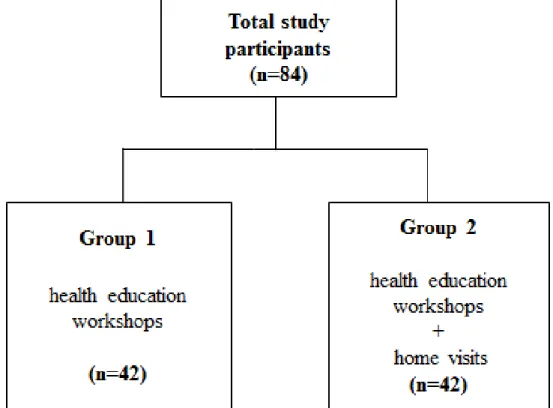
The participants were randomly divided into 2 groups (Figure 1), in order to compare two different types of nutritional intervention. The intervention lasted five months and consisted of the following strategies according to each group:
-Group 1: composed of individuals who were instructed to use the dietary treatment for arterial hypertension, given through monthly health education workshops (n = 42). These activities were carried out in a dialogic and participatory manner, through dynamic and interactive lectures with the help of posters, figures, household items, videos and practical demonstrations of the per capita amount recommended for the consumption of sodium, fat and sugar.
-Group 2: composed of individuals who, in addition to participating in the monthly health education workshops described above, received further nutritional counseling
Braz. J. of Develop., Curitiba, v. 5, n. 11, p. 23751-23767 nov. 2019 ISSN 2525-8761 guidelines through monthly periodic home visits (n = 42) over 5 months. Each home visit had the approximate duration of 1 hour, held at the time of preparation of the participant’s main meal (lunch).
Figure 1: Formation of groups according to the types of intervention, 2016.
The subjects discussed in the health education workshops and home visits are described in Table 1.
Table 1: Content of health education workshops and home visits, 2016. The health education workshops Home visits
1- Arterial hypertension: general aspects, dietary measures and lifestyle habits for non-pharmaceutical treatment;
1.1- Identification of foodstuffs purchased for the home and implementation of guidelines in accordance with the food habits of the family 1.2- Identification of foodstuffs purchased for the home and implementation of guidelines in accordance with the food habits of the family
Braz. J. of Develop., Curitiba, v. 5, n. 11, p. 23751-23767 nov. 2019 ISSN 2525-8761 2- Lipid, sugar and sodium consumption:
recommendations, comorbidities and cardiovascular risk factors related to arterial hypertension;
2- Identification of foodstuffs purchased for the home and implementation of guidelines in accordance with the food habits of the family
3- Fruits and vegetables: importance and food recommendations;
3- Strengthening of guidelines carried out and introduction of necessary adjustments according to the specific needs of each family; 4- Types of fats and adequate
consumption;
4- Strengthening of guidelines carried out and introduction of necessary adjustments according to the specific needs of each family; 5- Reduction/maintenance of body weight:
the importance of physical activity.
5- Strengthening performed guidelines and making necessary adjustments according to the specific needs of each family.
Data on lifestyle habits and socioeconomic status was collected through individual interviews before the intervention. Anthropometric, biochemical and blood pressure (BP) variables, as well as dietary data were collected before and after the interventions.
Weight was obtained by using an electronic scale with capacity of 150 kg, with 50 gram divisions. Height was measured using a portable anthropometer according to techniques proposed by Jellife8 . Body mass index (BMI) was calculated using the relationship between weight and height squared (W/H2) and rated according to criteria of the World Health Organization (WHO)9 for adults, and Lipischitz 10 for the elderly. Waist circumference (WC) was measured using an inextensible tape at the midpoint between the iliac crest and the outer face of the last rib at the moment of expiration and classified according to the cutoff points proposed by the WHO 11.
For clinical and laboratory evaluation the results of serum tests for fasting glucose, triglycerides, sodium and total cholesterol were utilized, as well as the fractions (LDL, HDL, VLDL). The BP was measured in days of biochemical collections. The classification was carried out according to standard procedures and parameters.
The food consumption evaluation was carried out through a questionnaire of food consumption frequency. The per capita values/day were obtained by estimating the monthly consumption of these foods in the participant's residence, divided by the number of days in the month and the number of household members 13. Individual consumption scores were
Braz. J. of Develop., Curitiba, v. 5, n. 11, p. 23751-23767 nov. 2019 ISSN 2525-8761 calculated according to the method proposed by Fornés et al. 14.The foods were divided into two groups: group of foods considered of risk for cardiovascular diseases (whole milk and dairy products, fried foods, foods high in animal fat, sugar and sodium) and group of protective or neutral foods (rice, beans, whole grains, fish, olive oil, low fat milk and dairy products, fruits and vegetables).
With regards to the physical activity evaluation the study used the short version of the International Physical Activity Questionnaire proposed by the World Health Organization 15.
For data analysis the SPSS for Windows (Version 20.0; SPSS Inc., Chicago) was used 16. To evaluate the similarity between the groups, the Chi-Square test was used in socioeconomic and health characteristics. The Kolmogorov-Smirnov, Chi-Square, Wilcoxon test, Paired T-test, Mann Whitney tests were used for the analyzes, considering the level of statistical significance of p <0.05.
The study was approved by the Ethics Committee of Research with Human Beings under report number 1146817/2015 and the participants signed the Free and Clarified Consent Term.
3 RESULTS
Table 2 shows the socioeconomic and health characteristics of the participants, according to the intervention groups, in addition to presenting the characteristics of the total sample. There is a higher proportion of adults aged ≤ 64 years, female and with low level of educational, most having 1-4 years of study. Regarding smoking and alcohol use most declared being non-smokers or drinkers (Table 2).
Table 2. Socioeconomic and health characteristics of arterial hypertension carriers who participated in the two types of intervention (groups 1 and 2), 2016.
Variable
Group 1 Group 2 Total
N % N % N % p-value* Gender Female 36 85.7% 28 66.7% 64 76.2% 0.040a Male 6 14.3% 14 33.3% 20 23.8% Age ≤ 52 20 47.6% 9 21.4% 29 34.5% 53 - 64 11 26.2% 16 38.1% 27 32.1% 0.041a ≥ 65 11 26.2% 17 40.5% 28 33.3%
Braz. J. of Develop., Curitiba, v. 5, n. 11, p. 23751-23767 nov. 2019 ISSN 2525-8761 Education (years of study) Illiterate 4 9.5% 4 9.5% 8 9.5% 1-4 years 29 69.0% 30 71.4% 59 70.2% 0.963 5 years or more 9 21.4% 8 19.0% 17 20.2% Alcohol Yes 14 33.3% 7 16.7% 21 25.0% 0.078 No 28 66.7% 35 83.3% 63 75.0% Tobacco Smoker 6 14.3% 6 14.3% 12 14.3% Former smoker 11 26.2% 10 23.8% 21 25.0% 0.967 Non-smoker 25 59.5% 26 61.9% 51 60.7% Physical activity Inactive 21 50.0% 19 45.2% 40 47.6% 0.662 Active 21 50.0% 23 54.8% 44 52.4%
Table 3 shows the initial and final means of the anthropometric, clinical, biochemical, dietary and physical activity variables, comparing the differences among the independent means of the intervention group, but taking into account the intervention of the educational activities as a whole.
Of the 17 variables studied, 12 showed statistically significant differences. The participants of the study had improvements in the anthropometric, biochemical, clinical and dietary parameters. Among the anthropometric variables, all had a value of p<0.001 (weight, WC and BMI). The risk score for food consumption showed an average reduction of 2.57, while there was an average increase of 1.08 in the intake of protection or neutral food (p <0.001). Statistically significant results were also observed in systolic blood pressure, biochemical variables (fasting glucose, VLDL cholesterol and triglycerides) and the dietary variables (per capita/day of oil, salt and sugar). All of the above mentioned variables showed a value of p <0.001.
Braz. J. of Develop., Curitiba, v. 5, n. 11, p. 23751-23767 nov. 2019 ISSN 2525-8761 *Paired t-test; **Wilcoxon test; standard deviation (SD); interquartile range (IR); a p<0.05
Table 4 shows the initial and final means of the anthropometric, clinical, biochemical and dietary variables, in order to statistically compare the mean differences between the two intervention groups. There was a statistically significant difference for triglycerides, weight, BMI and per capitas of oil and salt. It is noteworthy that, although the other variables did not show statistically significant results, all showed improvements in their respective evaluated parameters when compared to the moment before the intervention (except for total cholesterol in group 1 - health education workshops - and HDL cholesterol in both groups). Also noteworthy is the fact that although both groups showed improvements in all parameters, Table 3. Biochemical, anthropometric, clinical and dietary variables before (initial) and after (final) the health education strategies, 2016.
Variables
Before After
Difference
Mean (SD) Mean (SD) p - value*
Total cholesterol (mg/dL) 184.45 (37.27) 180.50 (33.36) 3.95 (24.10) 0.137 HDL cholesterol (mg/dL) 47.84 (7.70) 47.09 (7.37) 0.75 (5.59) 0.222 LDL cholesterol (mg/dL) 104.29 (33.49) 104.32 (31.50) -0.03 (20.47) 0.987 Sodium (mEq/L) 139.62 (2.21) 139.39 (2.30) 0.22 (2.18) 0.345 Weight (Kg) 68.91 (13.80) 67.73 (13.14) 1.18 (1.91) <0.001a BMI (Kg/m2) 28.66 (5.52) 28.18 (5.32) 0.48 (0.77) <0.001a WC (cm) 92.41 (11.62) 90.82 (11.63) 1.58 (4.23) <0.001a Risk score for food
consumption 9.05(2.16)
6.47 (1.60)
2.57 (1.75) <0.001 a
Protection score for food
intake 5.76 (1.84) 6.84 (1.64) -1.08 (1.18) <0.001 a Variables Before After Difference
Median (IR) Median (IR) p -
value** Glucose (mg/dL) 102 (88-134.50) 93.50 (85-117) 6 (-0.50-17.50) <0.001a VLDL cholesterol (mg/dL) 26.80 (19.30-39) 24.70 (18.20-32) 2.80 (-2-8) <0.001a Triglycerides (mg/dL) 136 (102.50-198) 122.50 (89-159) 18 (-4.50-47) <0.001a Systolic BP (mmHg) 130 (120-150) 130 (115-140) 10 (0-20) <0.001a Diastolic BP (mmHg) 80 (70-90) 80 (80 -90) 0 (-10-10) 0.569 Per capita/day of oil (g) 52.78 (37-83) 30 (23.25-40) 7.50
(1.88-15)
<0.001a
Per capita/day of salt (g) 11.11 (8.33-16) 8.33
(6.67-11.11) 0 (0-24.41)
<0.001a
Per capita/day of sugar(g) 66.67 (44-83.33)
52.78
(37-83.33) 0 (0-5.56)
Braz. J. of Develop., Curitiba, v. 5, n. 11, p. 23751-23767 nov. 2019 ISSN 2525-8761 group 2 (educational workshops on health and home visits) presented better results when compared to group 1 (only health education workshops).
4 DISCUSSION
This study showed important findings about the positive influence of educational interventions on the adherence of individuals with arterial hypertension to non- pharmacological treatment, as can be seen in the statistically significant results on the modifiable risk factors of: glucose, triglycerides, VLDL cholesterol, systolic blood pressure, weight, WC, BMI, risk and protection food scores and reduction in per capitas of oil, salt and sugar. In this context, the importance of prioritizing strategies to promote the health of arterial hypertension carriers becomes evident, and health education plays a crucial role in this regard. Studies investigating the prevalence of cardiovascular risk factors showed arterial hypertension associated to other risk factors for cardiovascular diseases, some of which have metabolic and behavioral determinants. Among the most investigated factors are the following: BMI, diabetes mellitus, dyslipidemia, alcohol consumption, smoking and sedentary lifestyles17-19. The high prevalence and co-occurrence of risk factors are concerning because they substantially increase the degree of cardiovascular risk 12,18.
Regarding anthropometric (weight, BMI and WC) and clinical (BP) risk factors, the interventions carried out with arterial hypertension carriers in this study have provided
Braz. J. of Develop., Curitiba, v. 5, n. 11, p. 23751-23767 nov. 2019 ISSN 2525-8761 statistically significant results (Tables 3 and 4); group 2 (health education workshops and home visits) having more satisfactory results compared with group 1 (health education workshops only). The anthropometric profile affects BP behavior. It is estimated that 79% of cases of hypertension in men and 65% in women are a direct result of excess weight. The reduction of 10 kg in body weight can decrease systolic blood pressure (SBP) in 5-20 mmHG 20. In the present study, there was an average reduction of 1.98 kg of body weight and 10 mmHg. An intervention study conducted by Ribeiro et al.13 observed the importance of changes in lifestyle, particularly in diet to reduce weight and BP. After interventions to change individuals’ lifestyles, there was statistical difference in weight, BMI, WC and SBP parameters. As for anthropometric parameters, weight had a mean reduction of 1.7 kg (p = 0.018); BMI had a mean reduction of 0.7 kg/m² (p = 0.019); and WC had a mean reduction of 4.2 cm (p = 0.001). SBP showed a mean decrease of 13mmHg (p = 0.004). These findings corroborate with the results obtained in this present study, showing therefore the relevance of introducing food and nutrition education when expecting results which permit a better quality of life of patients with arterial hypertension 13,19,21.
Treatment success depends mainly on behavioral change and adherence to a healthy eating plan18,22. A longitudinal study by Forman et al. 23, identified that maintaining the BMI below 25 kg/m2 prevents by 40% the development of hypertension in women. Similarly, loss of weight and WC correlate with reductions in BP and improvements in associated metabolic disorders 23, 24.
Another factor that influences BP behavior is body fat distribution. Central or visceral obesity has greater impact on BP than peripheral obesity. It is estimated that a WC increase of 2.5% in men and 4.5% in women raises 1 mmHg in the systolic BP 20. In the present study, there was a statistically significant reduction (p <0.001) in the WC measurements of the participants in both groups, those of group 2 being more pronounced. This result is an important finding regarding the health of participants, considering that the increased WC is a risk factor for metabolic and cardiovascular diseases, even when the BMI is adequate 25,26.
Similarly to the anthropometric factors, the biochemical parameters are of fundamental importance for the prevention of cardiovascular diseases. A comparative longitudinal study carried out on arterial hypertension patients found that health education workshops and home visits had positive effects on the adherence to non-pharmacological treatment, and that home visits had significant effects on biochemical, anthropometric and dietary parameters, corroborating with the findings of this present study 13.
Braz. J. of Develop., Curitiba, v. 5, n. 11, p. 23751-23767 nov. 2019 ISSN 2525-8761 The biochemical, fasting glucose, VLDL cholesterol and triglycerides variables showed a statistically significant reduction at the end of the intervention (p <0.001), without taking into account the type of educational intervention performed (Table 3). Regarding the difference between the intervention groups, the triglycerides showed statistically significant results in group 2 (Table 4). A study which compared two intervention strategies found that only fasting glucose improved among subjects who received home visits 13.
As for dietary variables, the study found that the interventions were able to promote positive and statistically significant changes in the average per capita consumption of oil, sugar and salt in this general population (Table 3) (p <0.001). When comparing the types of interventions carried out, group 2 stood out with statistically significant results in the consumption of oil and salt compared to group 1 (p <0.001). Moreover, an increase in the consumption of foods considered protective and a reduction in the consumption of foods considered of risk was found, pointing to an improvement in diet quality. Food and nutrition education can favorably modify several conditions related to additional risk factors for hypertension, such as dyslipidemia and glucose intolerance 19, 24.
Other non-pharmacological measures associated with the treatment of arterial hypertension can also be found in the scientific literature, such as quitting smoking and reducing alcohol consumption 12. Smoking is one of the most important factors of modifiable environmental cardiovascular risk. It is estimated that smokers have three times higher risk of acute myocardial infarction than non-smokers, and all kinds of tobacco use, including different types of cigarettes and the inhaling of smoke by passive smokers should be discouraged. Furthermore, there is evidence that cardiovascular changes such as increased arterial stiffness, caused by smoking, can be reversed with the inhibition of smoking 28,29. As for alcohol, there is an association between its intake and BP changes, depending on the amount ingested. Evidence of the correlation between a small intake of alcohol and the consequent reduction in BP is still fragile and needs further research. In individuals with arterial hypertension, alcohol intake, acutely and depending on the dose, reduces BP, however, it increases a few hours after 18, 30.
In relation to physical activity (Table 2), group 2 had the highest proportion of active individuals compared to group 1, contributing thus to a better quality of life for the arterial hypertension patients in this group, since the regular practice of physical activity is an important modifiable risk factor for arterial hypertension. Studies report that a sedentary lifestyle is common in the elderly and in patients with arterial hypertension. Thus, the WHO
Braz. J. of Develop., Curitiba, v. 5, n. 11, p. 23751-23767 nov. 2019 ISSN 2525-8761 recommends that for specific groups such as arterial hypertension carriers, participatory health education worked in the environment where they live adds benefits to the pharmacological treatments 4, 21.
Health education strategies, such as the community interventions carried out in this present study, have been implemented in several developed and developing countries as a way of coping with non-transmissible chronic diseases, from a risk-based approach21,31-33. Community strategies are based on the premise that public health actions have a greater potential impact than proposals at an individual level, as they are based on prevention of risk factors and the promotion of health 21, 31. These findings corroborate the results of this present study, since education activities in health and nutrition conducted in a dialogic and participatory manner, were essential for the adherence to the non-pharmacological treatment of arterial hypertension, reflecting on the anthropometric, clinical, biochemical and food standard parameters of the study’s population.
The scientific evidence also points out that the attendance of patients to educational activities, the more frequent meetings with the health care team, and family support are predictor factors that are favorable to the adhesion to non-pharmacological treatment for arterial hypertension 13,21,33-35. In addition, reconciling educational activities with a greater number of home visits allows for a better application of the necessary therapeutic adjustments, and encourages more effective changes in lifestyle 13,21,34,36.Similar results were found in this present study. Although the two types of intervention significantly favored the anthropometric, clinical, biochemical and dietary changes in the groups studied, more satisfactory results were found in the intervention group which received monthly home visits in addition to the health education workshops.
5 CONCLUSION
This study showed that the educational interventions carried out were effective for the improvement of 12 of the 17 parameters evaluated, which highlights the relevance of the strategies used (health education workshops and home visits) for the improvement of the quality of life of arterial hypertension patients.
When comparing the types of interventions between the groups, group 2 (health education workshops and home visits) provided the best results with respect to the adherence to non-pharmacological treatment for arterial hypertension in relation to group 1 (health education workshop only). This finding reinforces the fact that the patient’s home is a
Braz. J. of Develop., Curitiba, v. 5, n. 11, p. 23751-23767 nov. 2019 ISSN 2525-8761 privileged place for the practice of nutritional counseling, since the practice of visiting the home contributed to changing behavior patterns and consequently to an increase in the quality of life of these patients through the promotion of health and prevention.
Making individuals more aware of their blood pressure levels and the strategies they can use to control it, increases their understanding of the asymptomatic and chronic nature of the disease, and can be used as a motivational factor to stimulate changes in inappropriate lifestyle habits.
A limitation found in this present study was the fact that even with a random drawing for inclusion of participants in each group, there was a higher frequency of males and older age in group 2. However, these aspects did not influence the results since statistically significant differences were not found in the stratified analysis for either sex or age.
REFERENCE
1. World Health Organization - Noncommunicable diseases. 2018. Available <https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases>
Acess 12 de Junho de 2019.
2 . Souza ACC, Borges JW, Moreira TMM. Qualidade de vida e adesão ao tratamento em hipertensão: revisão sistemática com metanálise. Rev Saude Publica. 2016; 50:1-14.
3.World Health Organization. Adherence to long term therapies: evidence for action. Geneva: 2003.
4. Pan American Health Organization. Plan of Action for the Prevention and Control of Noncommunicable Diseases in the Americas 2013-2019. PAHO. 2014.
5. Gouveia Neto JR, Alves KKAF, Souza ANA et al. Adesão terapêutica e qualidade de vida de hipertensos assistidos na atenção primária de saúde/Therapeutic adhesion and quality of living of hypertensions assisted in primary health care. Nursing. 2019; 22(249):2600-2603. 6. Lauziére TA, Chevarle N, Poirier M et al. Effects of an interdisciplinary education program on hypertension:a pilot study. Can J Cardiovasc Nurs. 2013; 23(1):12-18.
7. Malta DC, Bernal RT, de Souza MF et al. Social inequalities in the prevalence of self-reported chronic non-communicable diseases in Brazil: national health survey 2013. Int J Equity Health. 2016;15(153): 1-11.
Braz. J. of Develop., Curitiba, v. 5, n. 11, p. 23751-23767 nov. 2019 ISSN 2525-8761 8.Jellife DBI. Evaluacíon del estado de nutricíon de la comunidade. Genebra: World Health Organization; 1968.
9.World Health Organization. Physical Status: The Use and Interpretation of Anthropometry - Report of a WHO Expert Committee. WHO Technical Report Series. Geneva: 1995. 10.Lipschitz DA. Screening for nutritional status in the elderly. Primecare. 1994; 21(1):56-67.
11.World Health Organization. Obesity: Preventing and managing the global epidemic. Report of a WHO Consulation on Obesity. Geneva: 1998.
12. Whelton PK, Carey RM, Aronow WS et al.
ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA-Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017.
13. Ribeiro AG, Ribeiro SMR, Dias CMGC et al. Non-pharmacological treatment of hypertension in primary health care: A comparative clinical trial of two education strategies in health and nutrition. BMC Public Health. 2011;11: 637-647.
14. Fornés NS, Martins IS, Velásquez-Meléndez G et al. Escores de consumo alimentar e níveis lipêmicos em população de São Paulo, Brasil. Rev Saude Publica. 2002; 36(1):12-18. 15.Matsudo SM, Matsuo VR, Araújo T et al. Questionário Internacional de Atividade Física (IPAQ): estudo de validade e reprodutibilidade no Brasil. Rev Bras Ativ Saude. 2001; 6(2):5-18.
16. IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp. 2011.
17. Meng-Ping W, Shu-Fang VW, Tsu-Chi W et al. Effectiveness of a community-based health promotion program targeting people with hypertension and high cholesterol. Nurs Health Sci. 2012;14(2):173-181.
18. Sebo P, Pechère-bertschi A, Herrmann FR et al. Blood pressure measurements are unreliable to diagnose hypertension in primary care. J Hypertens. 2014; 32(3):509-517.
Braz. J. of Develop., Curitiba, v. 5, n. 11, p. 23751-23767 nov. 2019 ISSN 2525-8761 19.Machado JC, Cotta RMM, Moreira TR et al. Análise de três estratégias de educação em saúde para portadores de hipertensão arterial. Cien Saude Colet. 2016; 21(2):611-620.
20. Oliveira EA, Bubach S, Flegeler DS. Perfil de Hipertensos em uma Unidade de Saúde da Família. Rev Enferm. 2009;17(3):383-387.
21. Ribeiro AG, Cotta RMM, Silva LS et al. Hipertensão arterial e orientação domiciliar: o papel estratégico da saúde da família. Rev Nutr. 2012; 25(2):271-282.
22. Lau KK, Wong YK, Chan YH et al. Mediterranean-style diet is associated with reduced blood pressure variability and subsequent stroke risk in patients with coronary artery disease. Am J Hypertens. 2015; 28(4):501–507.
23. Forman JP, Stampfer MJ, Curhan GC. Diet and lifestyle risk factors associated with incident hypertension in women. JAMA.2009; 302(4):401-411.
24. Bricarello LP, Retondario A, Poltronieri F et al. Dieta DASH (Dietary Approach to Stop Hypertension): Reflexões sobre adesão e possíveis impactos para a saúde coletiva. Cien Saude Colet [periódico na internet] (2018/Ago). [Citado em 17/06/2019]. Está disponível em:
http://www.cienciaesaudecoletiva.com.br/artigos/dieta-dash-dietary-approach-to-stop- hypertension-reflexoes-sobre-adesao-e-possiveis-impactos-para-a-saude-coletiva/16925?id=16925
25.Veloso HJF, Silva AMM. Prevalência e fatores associados à obesidade abdominal e ao excesso de peso em adultos maranhenses. Rev Bras Epidemiol. 2010;13(3):400-412.
26. Drehmer M, Odegaard AO, Schmidt MI et al. Brazilian dietary patterns and the dietary approaches to stop hypertension (DASH) diet?relationship with metabolic syndrome and newly diagnosed diabetes in the ELSA? Brasil study. Diabetol Metab Syndr. 2017; 13(9):13-24.
27. Dong GH, Wang D, Liu MM et al. Sex difference of the prevalence and risk factors associated with prehypertension among urban Chinese adults from 33 communities of China: the CHPSNE study. J Hypertens. 2012; 30(3):485-491.
28. Li N, Li Z, Chen S. Effects of passive smoking on hypertension in rural Chinese nonsmoking women. J Hypertens. 2015; 33(11):2210-2214.
Braz. J. of Develop., Curitiba, v. 5, n. 11, p. 23751-23767 nov. 2019 ISSN 2525-8761 29. Yun M, Li S, Sun D et al. Tobacco smoking strengthens the association of elevated blood pressure with arterial stiffness: the Bogalusa Heart Study. J Hypertens. 2015; 33(11):266-274. 30. Zatu MC, Van-Rooyen JM, Loots DT et al. Self-reported alcohol intake is a better estimate of 5-year change in blood pressure than biochemical markers in low resource settings: the PURE study. J Hypertens. 2014; 32(4):749-755.
31. Tobe SW, Von SS, Kandukur K et al. Hypertension management initiative prospective cohort study: comparison between immediate and delayed intervention groups. J Hum Hypertens. 2014; 28(1):44-50.
32. Lu CH, Tang ST, Yi-Xiong YX et al. Community-based interventions in hypertensive patients: a comparison of three health education strategies. BMC Public Health. 2015; 15:1-9. 33. Machado JC, Cotta RMM, Moreira TR et al. Adherence to non-pharmacological treatment: Analysis of the impact of three health educational and nutritional strategies in hypertensive patients. Rev Nutr. 2016; 29(1):11-22.
34. Pearson TA, Palaniappan LP, Artinian NT et al. American Heart Association Council on Epidemiology and Prevention. American Heart Association guide for improving cardiovascular health at the community level, 2013 update: a scientific statement for public health practitioners, healthcare providers, and health policy makers. Circulation. 2013;127(16):1730-175.
35. World Health Organization. Action Plan for the Prevention and Control of Noncommunicable Diseases in the WHO European Region. 2016.
36. Zangirolani LTO, Assumpção D, Medeiros MAT et al. Hipertensão arterial autorreferida em adultos residentes em Campinas, São Paulo, Brasil: prevalência, fatores associados e práticas de controle em estudo de base populacional. Cien Saude Colet. 2018; 23(4):1221-1232.
Contributors
AAOC: draft the article, conception and design; acquisition of data, analysis and interpretation of data and final approval of the version to be published.
Braz. J. of Develop., Curitiba, v. 5, n. 11, p. 23751-23767 nov. 2019 ISSN 2525-8761 COBR and GDC: critical revision of the manuscript to improve intellectual content and final approval of the version to be published.
FMOC: acquisition of data and final approval of the version to be published.
TRM: analysis and interpretation of data and final approval of the version to be published. RMMC: orientation and supervision of the research, revising it critically and final approval of the version to be published.