ww w . e l s e v i e r . c o m / l o c a t e / b j i d
The
Brazilian
Journal
of
INFECTIOUS
DISEASES
Original
article
Ratio
of
monocytes
to
lymphocytes
in
peripheral
blood
in
patients
diagnosed
with
active
tuberculosis
Jun
Wang
a,∗,1,
Yongmei
Yin
b,1,
Xuedong
Wang
a,1,
Hao
Pei
a,
Shougang
Kuai
a,
Lan
Gu
b,
Huiqin
,
Yu
Zhang
c,
Qiusheng
Huang
d,
Bin
Guan
eaCenterofClinicalLaboratory,TheFifthPeople’sHospitalofWuxi,AffiliatedtoJiangnanUniversity,Wuxi,Jiangsu,China
bRadiologyDepartment,TheFifthPeople’sHospitalofWuxi,AffiliatedtoJiangnanUniversity,Wuxi,Jiangsu,China
cDepartmentofBasicMedicalScience,MedicalCollege,XiamenUniversity,Xiamen,Fujian,China
dDepartmentofRespiratoryMedicine,TheFifthPeople’sHospitalofWuxi,AffiliatedtoJiangnanUniversity,Wuxi,Jiangsu,China
eDepartmentofPharmacy,TheFifthPeople’sHospitalofWuxi,AffiliatedtoJiangnanUniversity,Wuxi,Jiangsu,China
a
r
t
i
c
l
e
i
n
f
o
Articlehistory: Received12June2014 Accepted6October2014
Availableonline18December2014
Keywords:
Activetuberculosis Monocytes Lymphocytes MLratio
a
b
s
t
r
a
c
t
Objective:Theratioofmonocytestolymphocytesinperipheralbloodcouldreflectan indi-vidual’simmunitytoMycobacteriumtuberculosis.Theobjectiveofthisstudywastoevaluate therelationshipbetweenratioofmonocytestolymphocytesandclinicalstatusofpatients withactivetuberculosis.
Methods:Thiswasaretrospectivereviewofdatacollectedfromtheclinicaldatabaseof TheFifthPeople’sHospitalofWuxi,MedicalCollegeofJiangnanUniversity.Atotalof419 patientswhohadnewlydiagnosedactivetuberculosisand108casesfrom419patientswith tuberculosistherapyeithernearcompletionorcompletedwereselected.Controlswere327 healthydonors.
Results:Median ratioofmonocytesto lymphocyteswas0.36(IQR,0.22–0.54)inpatients beforetreatment, and0.16(IQR,0.12–0.20)incontrols(p<0.001).Ratio ofmonocytesto lymphocytes <9%or>25%wassignificantpredictorsforactivetuberculosis(OR=114.73, 95%CI,39.80–330.71;OR=89.81,95%CI,53.18–151.68,respectively).Aftertreatment,the medianratioofmonocytestolymphocytesrecoveredtobenearlynormal.Comparedto otherpatients,patientswithextrapulmonarytuberculosisandofage>60yearsweremore likelytohaveextremeratioofmonocytestolymphocytes(AOR=2.57,95%CI,1.08–6.09; AOR=4.36,95%CI,1.43–13.29,respectively).
Conclusions: Ratioofmonocytestolymphocytes<9%or>25%ispredictiveofactive tubercu-losis.
©2014ElsevierEditoraLtda.Allrightsreserved.
∗ Correspondingauthor.
E-mailaddress:j.wang1988@hotmail.com(J.Wang). 1 Theseauthorscontributedequallytothisarticle. http://dx.doi.org/10.1016/j.bjid.2014.10.008
Introduction
Globallythere were an estimated8.6million new casesof tuberculosis(TB)in2013and1.3milliondeaths.1Chinaand Indiahavethe greatestburdenofdisease.Indiaand China aloneaccountedfor26%and12%oftotalcases,respectively.1 InthemostWesternEuropeancountriesandUnitedStates, the majority of cases occur in foreign-born residents and recentimmigrantsfromcountriesinwhichTBisendemic.2–4 TB is presenting new challenges as a global health prob-lem, especially with new threats of HIV coinfection and drug-resistantstrainsofMycobacteriumtuberculosis(Mtb).5The knowledgeabout the hematological manifestations of Mtb infectioniscriticallyimportanttoprovideinsightinto patho-genesis.Fordecades,myeloid-specificcellshavebeenknown toserveashostcellsforMtbgrowthandlymphoidcellsare thoughttobethemajoreffectorcellsinTBimmunity.Given thecentralroleofmonocytesandlymphocytesinthe induc-tionofimmuneresponses,theirlevels(hereaftertermed“ML ratio”)in peripheralbloodmight beexpectedtoreflectthe stateofanindividual’simmunitytoinfection.
In a recent clinical analysis of peripheral blood mono-nuclearcellsfromacohortofSouthAfricaninfantstherelative ratioofmonocytestolymphocytesatthestartofmonitoring wasshowntopredictriskofdevelopingtuberculosisdisease duringfollow-up.6
Othersreportedthattheratiooflymphocytestomonocytes inperipheralbloodcorrelatedwiththeextentof tuberculo-sisinbothrabbits7and humans,8 butthenumbers studied weresmallandthestrengthoftheconclusionsthatcouldbe reachedinhumanswasdeemedtobemodest.Thedirect char-acterizationofMLratiotodatehasbeensurprisinglylimited. TherewasnostrongevidencethatMLratiowasaffectedby Mtbinfectioninhumans.
Tostartwiththis,usingfulldifferentialbloodcountdata frompatientswithactivetuberculosisandhealthydonors,we soughttodeterminewhether MLratio couldbeaffectedby tuberculosisorongoinganti-TBtreatmentandprovideinsight intoitspathogenesis.
Method
Studypopulationandethicsstatement
Data from all subjects in the present retrospective review werecollectedfromtheclinicaldatabaseofTheFifthPeople’s HospitalofWuxi,AffiliatedtoJiangnanUniversity,between December2010andJune2013.Thisstudywasapprovedbythe InstitutionalEthicsCommitteeofTheFifthPeople’sHospital ofWuxi,AffiliatedtoJiangnanUniversity(QD-2013-0016),and wasincompliancewiththenationallegislationandthe Dec-larationofHelsinkiguidelines.Writtenpatientconsentwas obtainedaccordingtotheinstitutionalguidelines.
Participantsclinicaldiagnosisandtreatment
Healthydonorswere from thephysicalexaminationcenter ofourhospitalandmetthefollowingcriteria:nohistoryof
Exclusion 1068 cases diagnosed
with active TB
25 cases with acquired immune deficiency syndrome 638 new diagnosis
419 patients included in analysis
94 cases with viral hepatitis, such as viral hepatitis type A , B or C
55 with diabetes
26 patients with other diseases 13 disagree with this research 6 pregnant patients
327 return-visiting
103 cases without before treatment data of full blood counts 965 cases with before
treatment data of full blood counts
464 patients
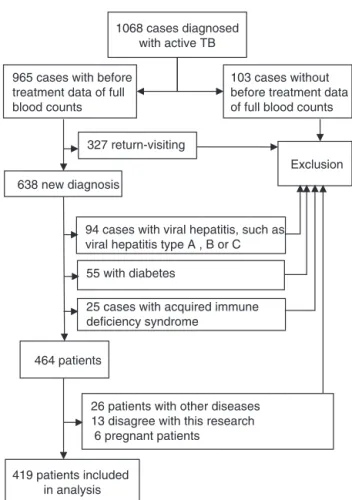
Fig.1–Patientselectioncriteriausedinthisstudy.
previous activeTBor TBtreatment, noevidenceofcurrent activeTB(absence ofcough,intermittent fever,and exces-sive night sweating inthe past twoweeks and absenceof unexplainedweightlossinthepastmonth).Tuberculosiswas diagnosedwhensubjectswithclinicaland/orimagingfeatures compatiblewithtuberculosishadatleastoneofthe follow-ingcriteria:positivesputumsmearforacid-fastbacilli(AFB); positivecultureforM.tuberculosis;biopsysuggestiveof tuber-culosis,and/orfullresponsetoanti-tuberculosistreatment. PatientswithextrapulmonaryTBaccompanyingpulmonary TBinvolvementwere included inthe categoryof extrapul-monary TB. Treatment ofnew cases, both pulmonary and extrapulmonarytuberculosis,receivedtwomonthsof isoni-azid(H),rifampicin(R),pyrazinamide(Z)andethambutol(E) duringanintensivephaseandfourmonthsofHRinthe con-tinuationphase.Thedurationoftreatmentwassixmonths. Severalkindsofextrapulmonarytuberculosisweremore dif-ficulttocure.Treatmentforanextendedperiodoftimewas requiredtoensurediseasecontrol.Suchas,prolongedtherapy hadbeenadoptedinTBmeningitis(9–12months)andbone andjointTB(9months;Fig.1).9
Fulldifferentialbloodcounts
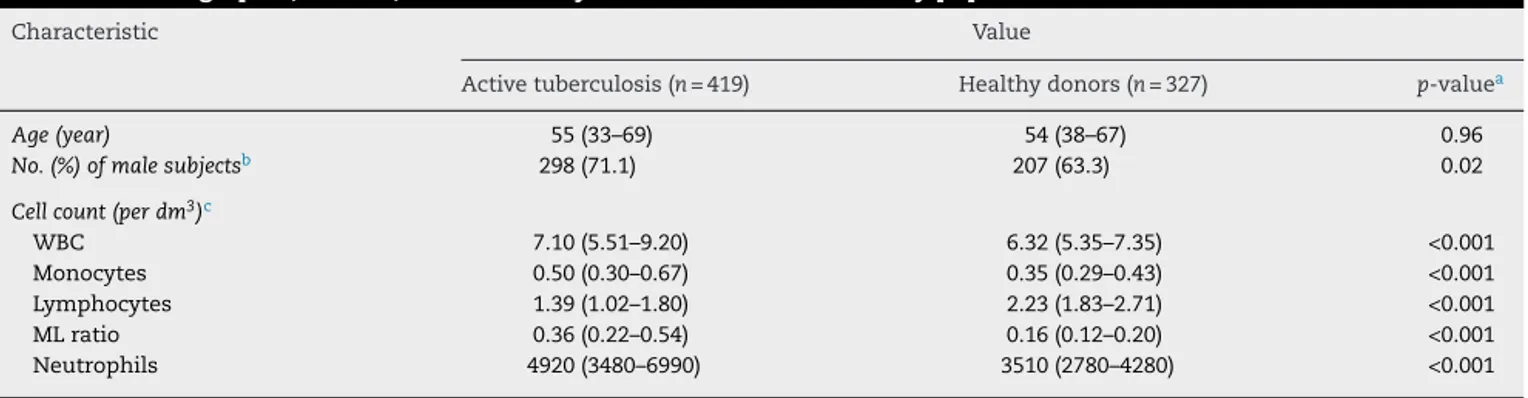
Table1–Demographic,clinical,andlaboratorycharacteristicsofthestudypopulation.
Characteristic Value
Activetuberculosis(n=419) Healthydonors(n=327) p-valuea
Age(year) 55(33–69) 54(38–67) 0.96
No.(%)ofmalesubjectsb 298(71.1) 207(63.3) 0.02
Cellcount(perdm3)c
WBC 7.10(5.51–9.20) 6.32(5.35–7.35) <0.001
Monocytes 0.50(0.30–0.67) 0.35(0.29–0.43) <0.001
Lymphocytes 1.39(1.02–1.80) 2.23(1.83–2.71) <0.001
MLratio 0.36(0.22–0.54) 0.16(0.12–0.20) <0.001
Neutrophils 4920(3480–6990) 3510(2780–4280) <0.001
a ByMann–WhitneyorPearson’schi-squaretest.
b Dataarepresentedasnumbers(%)ofindividualsexceptindicated. c Dataarepresentedasmediannumbers(interquartilerange).
(SysmexModelXS,Hamburg,Germany).Fullbloodcount mea-surementwassubjecttostrictqualityassuranceprocedures includingtwice-dailyhigh andlowinternalqualitycontrol, fortnightlyqualitycontrolsdone bytheWuxiclinical labo-ratoryQCscheme(Wuxi,Jiangsu,China)andannualquality assuranceaspartofJiangsuclinical laboratoryQCscheme. BothlaboratoriesareaccreditedbytheChinaNational Accred-itationSysteminaccordancewithinternationalstandardsISO 17025/2005andISO15189/2007.
Statisticalmethods
Statisticalanalysis wasconductedusing SPSSversion 17.0. Pearson’schi-squaretestandMann–WhitneyUtestwereused toidentifysignificantdifferencesacrosspatientsandhealthy donors,patientsbeforetreatmentandaftertreatment.p<0.05 (two-sided)wasconsideredasstatisticallysignificant differ-ence.Theoddsratios(OR)wereestimatedwith95%confidence intervals(CIs)fromtheunivariateanalysistoinvestigatethe relationshipbetweenactivetuberculosisandthedifferentML ratios.Adjustedoddsratios(AOR)with95%CIswerealso esti-matedfromthemultivariateanalysistodeterminethefactors associatedwiththedifferentMLratiosofpatients.
Results
Characteristicsofthestudypopulation
A total of1068 patients were diagnosed with activeTB in the database of The Fifth People’s Hospital of Wuxi from December2010toJune 2013.Availabilityoffulldifferential blood countswhennewly diagnosedwithactiveTB (previ-ouslyuntreatedforTBandneverreceivedanti-TBdrugsfor<1 month)wasrequiredtocomparewithhealthydonors.Patients withoutpre-treatmentdatawereexcludedand965patients remained.Wefurtherexcludedreturn-visitingpatients,who experiencedtreatmentfailureorreinfectionduringthecourse oftherapy,638patients remained.Afterexcludingpatients with viral hepatitis(viral hepatitis type A, B and C), AIDS (acquiredimmune deficiency syndrome),and diabetes, 464 patientsremained.Individualswhowere pregnant, didnot agreetoparticipateinourstudy,orhadotherdiseases,such
as,lungcancer,measles,syphilis,leucopenia,systemiclupus erythematosus,orrheumatoidarthritis,whichwerelikelyto influencefullbloodcounts,werealsoexcluded.Finally,data offullbloodcountsfrom419patientswereincludedinthe analysis, with a median age of 55 years, and 71.1% were men.Furthermore,inordertoassesstheinfluenceofanti-TB therapy, weexcludedpatientswho didnotreceive the rec-ommendedtherapy,suchasirregulartreatment,intermittent treatment, and undertreated patients. Finally, 108 patients whohadanti-TBtherapyeithernearcompletionorcompleted remained.Atotalof327healthyvolunteerswereincluded,207 maleand120femalesubjects.
Demographic,clinical,andlaboratorycharacteristicsof thestudysample
Therewere746individualsenrolledinthestudy:419patients withnewlytreatedactivetuberculosis,and327healthydonors without Mtbinfection.Demographicandclinical character-isticsandlaboratorydataaresummarizedinTable1.There wasnodifferenceinmedianageorsexbetweenpatientsand healthydonors.Patientswithactivetuberculosishad signif-icantlyhigher medianabsolutenumberofwhite blood cell (WBC),monocytesandneutrophilsthanhealthydonors.The medianabsolutenumberoflymphocytesofpatientswas sig-nificantly lower than thatof healthy donors.Patients with activetuberculosishad a significantlydifferentMLratio to healthydonors.
AssociationbetweenMLratioandactivetuberculosis,by percentilerankingoftheratioofmonocytestolymphocytes
Table2–Percentilerankingoftheratioofmonocytestolymphocytes.
Explanatoryvariable Value Activetuberculosis
(n=419)
Healthydonors (n=327)
p-valuea ORa 95.0%CIforOR Lower Upper
MLratiobetween9thand25thpercentile 43(10.3) 299(91.4) 1
MLratio<9thpercentile 66(15.8) 4(1.2) <0.001 114.733 39.803 330.716 MLratio>25thpercentile 310(73.9) 24(7.4) <0.001 89.816 53.181 151.687
p-valueb <0.001
a Logisticregressionanalysis,abbreviations:OR,oddsratio;CI,confidenceinterval. b Pearson’schi-squaretest.
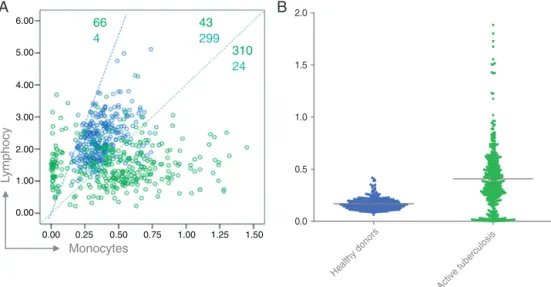
ofhealthydonors(bluecircle)centralizedmostlybetweenthe blueandgreenlines(91.4%);MLratioofpatients(green cir-cle)distributedmainlyout ofthe lines(89.7%)(Fig.2A).ML ratioofhealthy donorswasthemostcentralized data(IQR 0.08),andgatheredmainlyintheareawherethedatafrom patients distributed rarely (Fig. 2B).Compared to ML ratio betweenthe 9th and 25th percentile,participantswith ML ratio<the9thpercentileor>the25thpercentilehadahigher likelihoodtobepatientswithactivetuberculosis(OR=114.73, 95%CI,39.80–330.71;OR=89.81,95%CI,53.18–151.68, respec-tively)(Table2).ItindicatedthatMLratio lessthanthe9th percentileorgreaterthanthe25thpercentileweresignificant predictorsforactivetuberculosis.
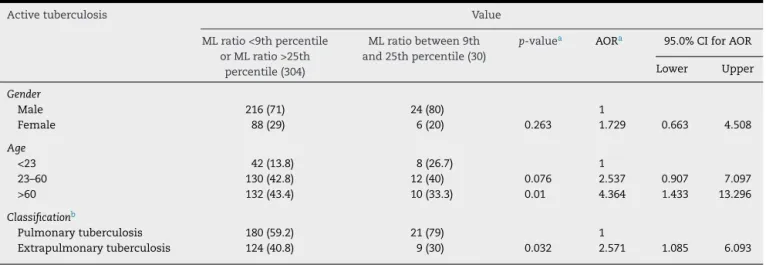
FactorsassociatedwithdifferentMLratiodistributionin 334patients
Amultivariateanalysiswasconductedusingvariablesof gen-der,ageanddiseaseclassification.AsshowninTable3,our studycomparedthecharacteristicsof334from419patients
who had clear information of disease classification. Male patientshadahigherprobabilitytobeinthegroupofMLratio <9%orMLratio>25%thanfemalepatients,buttheresulthad nostatisticalsignificance.Comparedtopatientslessthan23 years ofage, patientsolder than 60years were over 4-fold morelikelytobeinthe groupofMLratio<9%or MLratio >25%.Patientswithextrapulmonarytuberculosiswerenearly 2.5-foldmorelikelytobeintheextremegroups(Table3).
MLratioofpatientsrecoveredtobenearlynormalwith treatment
Inordertofurtherevaluatetheimpactofanti-TBtherapyon the MLratio,weexcludedpatientswhodidnotreceive the recommendedtherapy,suchasirregulartreatment, intermit-tenttreatment,andundertreatedtherapy.Atotalof108from 419patientswhohadFBCwiththerapyeithernear comple-tionorcompletedwereremainingandwasalsostratifiedinto thesamethreecategorieswithMLratio:lessthanthe9th per-centile,betweenthe9thand25thpercentile,andgreaterthan
Hea lthy donors
Activ e tuber
culo sis
0.0 0.5 1.0 1.5 2.0
Ly
m
p
h
o
c
y
Monocytes
A
B
66 4
43 299
310 24
0.00 0.00 1.00 2.00 3.00 4.00 5.00 6.00
0.25 0.50 0.75 1.00 1.25 1.50
Fig.2–Distributionofparticipants(patientsandhealthydonors)withratioofmonocytestolymphocytes(MLratio).(A) Monocytesandlymphocytescountareplottedonthex-andy-axes,respectively.MLratioofhealthydonors(bluecircle)
Table3–FactorsassociatedwithdifferentMLratiosdistributionofpatientsdiagnosedwithactivetuberculosis.
Activetuberculosis Value MLratio<9thpercentile
orMLratio>25th percentile(304)
MLratiobetween9th and25thpercentile(30)
p-valuea AORa 95.0%CIforAOR Lower Upper
Gender
Male 216(71) 24(80) 1
Female 88(29) 6(20) 0.263 1.729 0.663 4.508
Age
<23 42(13.8) 8(26.7) 1
23–60 130(42.8) 12(40) 0.076 2.537 0.907 7.097
>60 132(43.4) 10(33.3) 0.01 4.364 1.433 13.296
Classificationb
Pulmonarytuberculosis 180(59.2) 21(79) 1
Extrapulmonarytuberculosis 124(40.8) 9(30) 0.032 2.571 1.085 6.093
a Logisticregressionanalysis,abbreviations:AOR,adjustedoddsratio;CI,confidenceinterval. b 85caseslackclearinformationofdiseaseclassification.
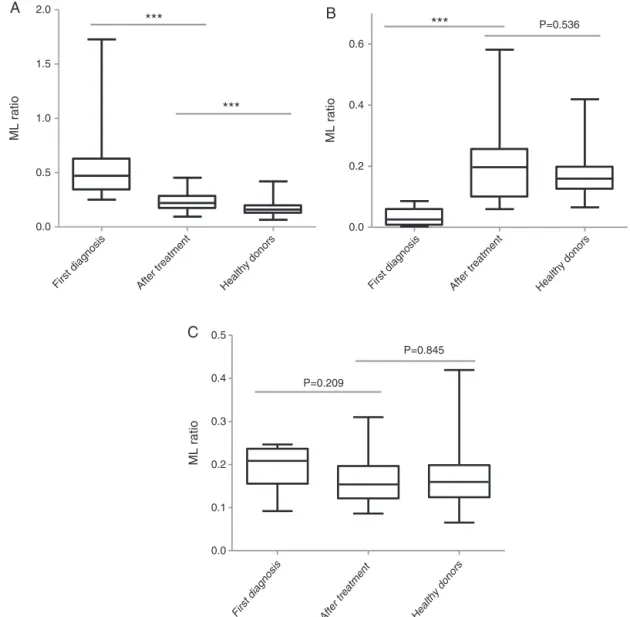
the25thpercentile.Anti-TBtherapysignificantlyreducedML ratiowithMLratiogreaterthan25thpercentile(medianML ratio,0.472(IQR,0.33–0.62) beforetreatmentvs 0.2199(IQR, 0.16–0.28)aftertreatment,p<0.001).MLratioelevated signif-icantly withML ratio less than 9th percentile(median ML ratio,0.026(IQR,0.006–0.059)beforetreatmentvs0.197(IQR, 0.09–0.25)aftertreatment,p<0.001).InpatientswithMLratio between the 9th and 25th percentile, there was no differ-ence betweenMLratio beforetreatment (median MLratio, 0.20 [IQR0.15–0.23]) and aftertreatment (median MLratio, 0.15[IQR,0.12–0.19],p=0.166).Beforeanti-TBtherapy,9.3%of individuals(10/108)hadMLratiobetweenthe9thand25th percentile,comparedwith75%(81/108)followinganti-TB ther-apy(p<0.001). ThemedianMLratio ofhealthydonorswas 0.15(IQR,0.12–0.19).TheresultsindicatedthathigherMLratio decreased,andlowerMLratioincreasedtobeclosetotheML ratioofhealthydonors.MLratioofpatientsrecoveredtobe nearlynormalwithtreatment.
Discussion
Monocytesareanessentialcomponentoftheinnateimmune responsethatactsasalinktotheadaptiveimmunesystem throughantigenpresentationtolymphocytes.Thusany fac-torthat perturbsthefunctionorrelativenumbersofeither celltypecouldpotentiallyaffectanindividual’sresponseto infection.
TheMLratioinperipheralcirculationmayreflectan indi-vidual’s capacity to mount an effective immune response. ML ratio has been shown to correlate with inhibition of mycobacterialgrowthinvitro10,11andtheriskishigheramong individualswitheitherloworhighMLratio.12Theseresults addtoevidencesupportingthat extremesofimmunityare associated with TB. This ratio could herald a previously unknownpathophysiologicchangeofTB.Asdemonstratedby ourstudy,patientswithactivetuberculosishad ahigheror lowerMLratiocomparedtohealthydonors.Westratified par-ticipantsintothreecategorieswithdifferentMLratios,and
healthydonorsweremostlyinthegroupofMLratiobetween the9thand25thpercentile,butpatientsweremainlyinthe groupofMLratiogreaterthanthe25thpercentileandinthe groupofMLratio lessthan the9thpercentile(Table2).ML ratiosinextremepercentileswere significantpredictorsfor activetuberculosis.
ThenormalMLratioisdisruptedbyMtbinfection.Ithas beenreportedrecentlythatMtbinfectionmayaltersubsets ofhematopoieticstemcells13ordirectlyinfectbonemarrow mesenchymalstemcells.14Studiesinmice15andhumans16 have shownthat subsetsofhematopoietic stemcells have distinctbiasesintheratioofmyeloidtolymphoidcellsthey
giveriseto.17,18Thedifferentproportionofmyeloidbiasedor
lymphoid-biasedhematopoieticstemcellsmayunderliethe peripheraldifferenceofMLratio.Therefore,itisreasonable thatMtbinfectionmayalterhematopoieticstemcellssuch thattheMLratioisaltered.Thechangeofmonocytesand lym-phocytes,reflectedintheirratio,mayaffectpatients’abilityto respondtomycobacterialinfection.Furtherworktoexplore thepathophysiologicalinvolvementoftheMLratioinTBmay yieldnewpathwaystomodifyorpreventthedisease.
MLratioofpatientsagedmorethan60yearsand extrapul-monarytuberculosisaredisruptedmoreseriouslythanothers. Themultivariateanalysisindicatedthat,amongpatients diag-nosedwithactivetuberculosis,tobeagedmorethan60years and to have extrapulmonary tuberculosis were associated withdifferentMLratiosofpatients.
In order to further evaluatewhether ML ratio could be affected byanti-TB therapy, the difference between before treatmentandaftertherapywasanalyzed(Fig.3).Theresults indicated that high ML ratio decreased, and low ML ratio increasedtobeclosetotheMLratioofhealthydonors.It sug-gestedthatMLratioofpatientsmaybechangedwithanti-TB therapy andthe alterationofMLratio mayalsoreflect the effectivenessandphaseoftherapy.
First diagnosis After treatment Healthy donors
0.0 0.5 1.0 1.5 2.0
ML ratio
***
***
A
First diagnosis After treatment
Healthy donors
0.0 0.2 0.4 0.6
ML ratio
***
P=0.536B
First di agnosis
After treatment Healthy donors
0.0 0.1 0.2 0.3 0.4 0.5
ML ratio
P=0.209
P=0.845
C
Fig.3–Ratioofmonocytestolymphocytes(MLratio)ofpatients,beforetreatment,aftertreatmentandhealthydonors.(A) MLratioofpatientswithMLratiogreaterthan25thpercentile;(B)MLratioofpatientswithMLratiolessthanthe9th percentile;(C)MLratioofpatientswithMLratiobetweenthe9thand25thpercentile.Dataarepresentedwithboxplot reportingthemedianvaluesandtheinterquartilerange(***p<0.001).MedianMLratioofpatientschangedtobecloseto
healthydonorswithanti-tuberculosistreatment.
excluded.Whetherthe exclusionofthesepatientsaffected theoutcomeisunknown.Asaretrospectivestudy,collecting informationfrommedicalrecordsfilledinbyother profession-alsisunavoidablebuttendstobelessaccurate.Fortunately,at thetimeofclinicalassessment,althoughclinicianswerenot blindedtothefullbloodcount,theywerenotawareofthis hypothesis,thusdiminishingdiagnosticbias.
Despitetheselimitations,ourresultssupportthatMLratios aredisruptedwithtuberculosis;MLratiosintheextreme per-centilesareassociatedwithactiveTB.Thisobservationneeds tobeconfirmedinothergeographicsettings.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgments
Wethankthe allpatientsfortheir supportinthisresearch andcolleaguesofTheFifthPeople’sHospitalofWuxifortheir assistanceincollectionofresearchdata.
r
e
f
e
r
e
n
c
e
s
1.WHO.Globaltuberculosisreport2013.Geneva,Switzerland:
WorldHealthOrganization;2013.
2.HillAN,BecerraJ,CastroKG.Modellingtuberculosistrendsin
theUSA.EpidemiolInfect.2012;140:1862–72.
3.Surveillancereport:tuberculosissurveillanceandmonitoring inEurope2013.Geneva,Switzerland:WorldHealth
4. PublicHealthEngland.TuberculosisintheUK2013report.
London,England:PublicHealthEngland;2013.
5. ZumlaA,RaviglioneM,HafnerR,vonReynCF.Tuberculosis.N
EnglJMed.2013;368:745–55.
6. NaranbhaiV,HillAV,AbdoolKarimSS,etal.Ratioof
monocytestolymphocytesinperipheralbloodidentifies
adultsatriskofincidenttuberculosisamongHIV-infected
adultsinitiatingantiretroviraltherapy.JInfectDis.
2014;209:500–9.
7. SabinFR,DoanCA,CunninghamRS.Studiesofthebloodin
experimentaltuberculosis:themonocyte-lymphocyteratio;
theanemia-leucopeniaphase.Trans22ndAnnuMeetingNatl
TubercAssoc.1926;22:252–6.
8. RogersPM.Astudyofthebloodmonocytesinchildrenwith
tuberculosis.NEnglJMed.1928;198:740–9.
9. WHO.Treatmentoftuberculosis:guidelines.4thed.Geneva,
Switzerland:WorldHealthOrganization;2010.
10.CarpenterE,FrayL,GormleyE.Cellularresponsesand
MycobacteriumbovisBCGgrowthinhibitionbybovine
lymphocytes.ImmunolCellBiol.1997;75:554–60.
11.DenisM,WedlockDN,BuddleBM.AbilityofTcellsubsetsand
theirsolublemediatorstomodulatethereplicationof
Mycobacteriumbovisinbovinemacrophages.CellImmunol. 2004;232:1–8.
12.TobinDM,RocaFJ,OhSF,etal.Hostgenotype-specific
therapiescanoptimizetheinflammatoryresponseto
mycobacterialinfections.Cell.2012;148:434–46.
13.BaldridgeMT,KingKY,BolesNC,WeksbergDC,GoodellMA.
Quiescenthaematopoieticstemcellsareactivatedby
IFN-gammainresponsetochronicinfection.Nature.
2010;465:793–7.
14.DasB,KashinoSS,PuluI,etal.CD271+bonemarrow
mesenchymalstemcellsmayprovideanichefordormant
Mycobacteriumtuberculosis.SciTranslMed. 2013;5:170ra13–213ra.
15.Muller-SieburgCE,ChoRH,ThomanM,AdkinsB,SieburgHB.
Deterministicregulationofhematopoieticstemcell
self-renewalanddifferentiation.Blood.2002;100:1302–9.
16.PangWW,PriceEA,SahooD,etal.Humanbonemarrow
hematopoieticstemcellsareincreasedinfrequencyand
myeloid-biasedwithage.ProcNatlAcadSciUSA.
2011;108:20012–7.
17.SchroederT.Hematopoieticstemcellheterogeneity:
subtypes,notun-predictablebehavior.CellStemCell.
2010;6:203–7.
18.Muller-SieburgCE,SieburgHB,BernitzJM,CattarossiG.Stem
cellheterogeneity:implicationsforagingandregenerative