w w w . r b o . o r g . b r
Original
Article
Reconstruction
of
the
medial
patellofemoral
ligament
using
autologous
graft
from
quadriceps
tendon
to
treat
recurrent
patellar
dislocation
夽
Constantino
Jorge
Calapodopulos
a,b,
Marcelo
Corvino
Nogueira
c,∗,
José
Martins
Juliano
Eustáquio
b,
Constantino
Jorge
Calapodopulos
Júnior
b,
Oreston
Alves
Rodrigues
aaDepartmentofOrthopedicsandTraumatology,UniversidadeFederaldoTriânguloMineiro(UFTM),Uberaba,MG,Brazil
bDepartmentofOrthopedicsandTraumatology,UniversidadedeUberaba(UNIUBE),Uberaba,MG,Brazil
cHospitalRegionaldeSobradinho,Brasília,DF,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received17February2014 Accepted29May2015
Availableonline6February2016
Keywords:
Patellofemoralligament Quadricepstendon Patellardislocation
a
b
s
t
r
a
c
t
Objective:Theobjectiveofthisstudywastoevaluatetheefficacyofthesurgicaltechnique usingthequadricepstendonasagraftinstaticreconstructionofthemedialpatellofemoral ligament.
Methods:Thiswasaprospectivecaseseriesstudyinwhichtheparticipantswere22patients withadiagnosisofrecurrentpatellardislocationwithoutanyotheranatomicalalterations thatrequiredsurgicaltreatment.Thefunctionalresultsfromthetechniquewereevaluated usingclinicaldataandtheLysholmquestionnaire,oneyearaftertheoperation.
Results:Itwasobservedthatthepatientswerepredominantlyfemale(86%)andunder21 yearsofage(73%),justlikeintheliterature.Atthefirstannualreturnafterthesurgery, therewasnosignificantpainonmediumefforts,nolossofrangeofmotionandapositive apprehensiontest.Accordingtothequestionnaireused,theresultsweregradedasgood.The patientswhoreportedhavingseverepainongreatereffortwereinvolvedin employment-relatedlegaldisputes.
Conclusion: Thistechniqueshowedlowmorbidityandgoodfunctionalresultsovertheshort term.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
夽
WorkperformedattheUniversidadeFederaldoTriânguloMineiro(UFTM),Uberaba,MG,Brazil.
∗ Correspondingauthor.
E-mail:mcorvino.ort@gmail.com(M.C.Nogueira).
http://dx.doi.org/10.1016/j.rboe.2016.01.012
188
rev bras ortop.2016;51(2):187–193Reconstruc¸ão
do
ligamento
patelofemoral
medial
com
enxerto
autólogo
do
tendão
quadricipital
no
tratamento
da
luxac¸ão
recidivante
da
patela
Palavraschave:
Ligamentopatelofemoral Tendãoquadricipital Luxac¸ãopatelar
r
e
s
u
m
o
Objetivo:Avaliaraeficáciadetécnicacirúrgicaqueusaotendãodoquadrícepscomoenxerto nareconstruc¸ãoestáticadoLPFM.
Métodos: Estudode sériedecasos,prospectivo,doqualparticiparam22 pacientescom odiagnósticodeluxac¸ãorecidivantedapatela,quenãoapresentavamoutrasalterac¸ões anatômicasquenecessitassemdetratamentocirúrgico.Osresultadosfuncionaisdatécnica foramavaliadospormeiodedadosclínicosedoquestionáriodeLysholm,comumanode pós-operatório.
Resultados: Observou-sepredomíniodepacientesdosexofeminino(86%)emenoresde 21 anos(73%),aexemplo doobservadonaliteratura.Noprimeiroretornoanualapósa cirurgia,nãohouvedorsignificativaaosmédiosesforc¸os,perdadeamplitudedemovimento epositividadedostestesdeapreensão.Segundooquestionárioempregado,osresultados foramgraduadoscomobons.Aquelesqueinformaramdorintensaaosmaioresesforc¸os apresentavampendênciastrabalhistas.
Conclusão: Atécnicaapresentadamostrou,emcurtoprazo,baixamorbidadeebons result-adosfuncionais.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Todososdireitosreservados.
Introduction
Acute dislocationof the patella isa common event, espe-ciallyamongadolescentsandyoungadults,withhigherrates among females.1 It can be triggered bytraumatic or non-traumaticevents. In the lattercases, it is associated with significantanatomicalalterationsofthekneeextensor mech-anism.Thereisnoconsensusregardingtheidealtreatment afterthefirstoccurrenceofdislocation,mainlybecauseonly 30%ofthepatientspresentanewepisode.2However,incases ofrecurrentdislocation(twoormoreepisodes),thetreatment isessentiallysurgicalandhastheaimofcorrectingthe pre-disposingfactors.Amongthese,reconstructionofthemedial patellofemoralligament(MPFL)isconsideredtobethemost importantprocedure,3especiallyafterkneeinjury.
TheMPFLactsasthemainligamentrestrictinglateral dis-placementofthepatellaatknee flexionofbetween0◦ and
30◦.4Becauseofitsbiomechanicalproperties,itisessentialfor controllingthenormalkinematicsofthepatellofemoraljoint.5 Duringthefirstepisodeoftraumaticpatellardislocation,this anatomicalstructurebecomespartiallyortotally torn.This injuryisconsideredtobeanessentialfactorenabling devel-opmentofrecurrentdislocation.6
Thefirstreportsofthisreconstructionweremadeby Sug-amunaetal.,7 in1990,whousedtendonautografts,andby ElleraGomes,whousedsyntheticgrafts.8Intheliterature, dif-ferentsurgicaltechniqueshavebeendescribed,withoptions forstaticanddynamicreconstruction,but noneofthem is consideredtobethegoldstandard.9
Surgicalproceduresusingaportionoftheextensor mech-anismasagraftinstaticreconstructionoftheMPFL,through tendontransfer,asdescribedbyCamanhoetal.10forthe patel-lartendon,andbySteensenetal.11forthequadricepstendon, areeasilyreproducibleandhavelowmorbidity.
Theobjectiveofthisstudywastoevaluatetheshort-term resultsfromMPFLreconstructioninpatientswithrecurrent patellardislocation,bymeansofatechniqueusingafragment fromthequadricepstendonasagraft.
Materials
and
methods
This was a prospective case series. Theparticipants were 22 patientsofbothsexeswho hadadiagnosis ofrecurrent patellar dislocation.Theyunderwentsurgicaltreatmentfor MPFLreconstructionatHospitaldeClínicas,Federal Univer-sityoftheTriânguloMineiro(UFTM),inUberaba,MinasGerais, betweenJanuary2008andSeptember2013.Theparticipants signedafreeandinformedconsentstatement.
Table1–Lysholmquestionnaire.Translationvalidated forthePortugueselanguage.
Claudication(5points) Pain(25points)
Never=5
Mildorperiodic=3 Severeandconstant=0
None=25
Mildorperiodicduringphysical effort=20
Greaterpainduringorafter walking>2km=10 Graterpainduringorafter walking<2km=5 Constant=0
Weight-bearing(5points) Edema(10points)
None=5
Withstickorcrutch=2 Impossible=0
None=10
Withheavyexercise=6 Withordinaryexercise=3 Constant=0
Locking(15points) Goingupstairs(10points)
Nolockingorfeelingof this=15
Feelingbutwithout locking=10 Occasional=6 Frequent=2 Jointlockedduring examination=0
Noproblem=10 Slightlyimpaired=6 Onestepatatime=3 Impossible=0
Instability(25points) Squatting(5points)
Never=25
Rarelyduringphysical effort=20
Frequentlyduring effort=15
Occasionallyduring dailyactivities=10 Frequentlyduringdaily activities=5
Ateachstep=0
Noproblem=5 Slightlyimpaired=4
Notpossiblebeyond90degrees=2 Impossible=0
Totalscore:
Scoring:excellent:95–100;good:84–94;fair:65–83;poor≤64.
Theexclusioncriteriaforthestudyweredefinedafter clini-calevaluation,radiologicalevaluation(radiography,computed
tomography and magneticresonance imaging) and
arthro-scopicevaluation.Thefollowingpatientswereexcluded:those withgenuvalgum,previoussurgeryinthesameknee, abnor-malityofjointrangeofmotion(ROM),Qanglegreaterthan 20◦,trochlearanglegreaterthan145◦,TT-TGdistancegreater
than20mm,highpatella(greaterthan1.2,asassessedusing theInsall-Salvatiindex),patellardysplasiaofgradeIV orV
accordingtotheWibergclassification,12cartilaginousinjuryof gradeIIIorIVaccordingtotheOuterbridgeclassification13and meniscaland/orligamentinjurieswithindicationsforrepair orreconstruction.
Oneyearaftertheoperation,thepatientswereevaluatedby meansofclinicalparameters(pain,ROMandpatellar instabil-itytest)andthroughapplicationoftheLysholmquestionnaire, asvalidated forthe Portuguese language14 (Table 1). Their intensityofpainwasinvestigatedbymeansofavisualanalog scaleandwasgradedasmild(scoresfrom0to3),moderate(3 to7)orsevere(7to10).15ROMwasinvestigatedusingamanual goniometerandinstability,bymeansoftheapprehensiontest. Assessmentsmadebypatientswhowereoffworkbecauseof thesurgicalprocedurewereusedascomplementarydatafor thisstudy.
Fig.1–Surgicalincisiononthesuperomedialfaceofthe patella,ofapproximately50mm.
Thedatagatheredweresubsequentlyplaceinan inven-toryinanelectronicdatabase,throughvalidationbymeansof doubledataentry(typing).Toanalyzetheresults,descriptive statisticalprocedureswereused.
This study was approved by the Ethics Committee for HumanResearchofUFTM(protocol2567/13).
Surgical
technique
The patientswere positioned on a standardsurgical table, in dorsal decubitus, and underwent spinal anesthesia. A pneumatictourniquetwasusedroutinelyinthissurgical pro-cedure. Firstly,aninventory ofthe jointwas performedby meansofarthroscopy,inordertodiagnoseandtreatany pos-siblecartilagelesions.
Asurgicalincisionwasmadeatthelevelofthemedialedge ofthepatella,50mmproximallytoitsupperedge,andthiswas continueddistallyuntilreachingthepatellarlevel. Layer-by-layerdissectionwasperformeddowntotheperitendon,which wasincisedvertically(Fig.1).
The segment corresponding to the medial third of the quadricepstendon,withawidthofapproximately10mmand lengthof50mm,wassectionedwithpreservationofthe dis-talportioninsertedinthepatella(Fig.2).Thetendonsegment
190
rev bras ortop.2016;51(2):187–193Fig.3–Incisiononthemedialfaceoftheknee,of approximately20mm(arrow).
waspreparedwithsuturingusingabsorbablethread(Vycril® 1.0mm)inanchoredrunningstitchesatitsfreeend.
After graft preparation, the second stage of the proce-durebegan.Averticalincision wasmadeintheskinofthe medialfaceoftheknee,betweenthemedialepicondyleand the tubercle of the adductor, of around 20mm in length (Fig.3).
Sincetheintentionwasthatthegraftshouldpassalong thenormalanatomicalpath,fromits origintothepointof fixationinthedistalfemur(Nomura’spoint),16throughthe secondlayerofWarrenandMarshall,17anincisionwasmade inthemedialretinaculumandthislayerwasexploredasfar asthesuperomedialedgeofthepatella(Fig.4).
Thegraftwaspassedintoplacemediallyandthenneeded tobefixedtothefemur,atthepointcorrespondingtoits orig-inalinsertion(Nomura’spoint).Thiswaslocatedwiththeaid ofanimageintensifyingdevice(Fig.5).
Ananchorwasinsertedatthislocation(Fig.6)andthegraft wasfixedwhilethekneewasflexedat30◦,withthepatella
centeredatthetrochlea.Afterdefinitivefixation,thejointROM andpatellarstabilityoverthekneeflexionrangeof0–30◦were
tested.
Fig.4–Transferofthegrafttoitsfixationpointonthe distalfemur,underthevastusmedialismuscle.
Fig.5–*Nomura’spoint:fixationofthemedial
patellofemoralligamentinthedistalfemur(ME=medial epicondyle,AM=insertionoftheadductormagnus).
Results
Twenty-twopatientswithaconditionofcurrentdislocationof thepatellaparticipatedinthisstudy.Theywereagedbetween 15and48yearsand73%wereundertheageof21years.Female patients predominated (86%)and the left legwas affected morefrequently (59%).Theworst scoresfrom the Lysholm questionnairewereamongtheolderparticipants(Table2).The meanlengthofpostoperativefollow-upwas30months,with arangefrom12to52months.Therewerenocomplications relatingtothesurgicalwound.
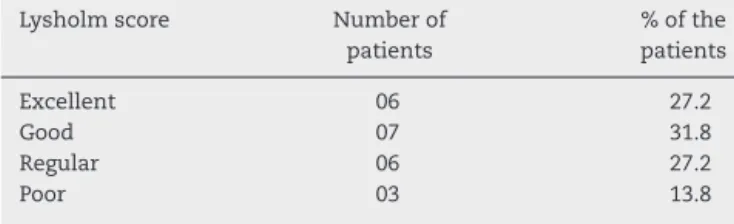
Basedonthequestionnaireused,59%ofthepatients pre-sentedgoodorexcellentresults,27.2%fairresultsand13.8%
r
e
v
b
r
a
s
o
r
t
o
p
.
2
0
1
6;
5
1(2)
:187–193
191
Patient Sex Age Side Employment-law
issues
Limping Weight-bearing Locking Instability Pain Swelling Goingup stairs
Squatting TOTAL SCORE
1 F 16 L N 5 5 10 25 20 10 10 4 89
2 F 18 R N 3 5 15 25 20 10 10 4 92
3 F 15 R N 5 5 10 20 20 6 6 2 74
4 F 21 R N 3 5 15 20 20 6 10 4 83
5 M 21 L N 5 5 15 25 20 10 10 5 95
6 F 20 L N 5 5 20 20 25 6 4 5 80
7 F 21 L N 5 5 15 20 25 10 10 5 95
8 F 18 R N 5 5 10 25 20 10 3 4 82
9 F 19 L N 5 5 10 20 20 10 10 4 84
10 F 39 L Y 5 5 10 15 10 3 6 2 56
11 F 19 R N 5 5 15 25 25 10 10 4 99
12 F 40 L Y 5 5 6 25 10 0 3 2 56
13 M 19 L N 5 5 10 25 20 10 10 5 90
14 F 28 R N 5 5 15 25 25 10 10 5 100
15 F 18 L N 5 5 15 25 25 10 10 2 97
16 F 26 R N 3 5 15 25 20 10 10 5 93
17 F 18 R N 5 5 10 25 20 10 3 2 80
18 F 28 L N 3 5 15 20 20 6 10 4 83
19 F 48 L Y 5 5 10 15 10 3 6 4 58
20 F 20 R N 5 5 15 25 25 10 10 2 97
21 M 19 L N 5 5 15 20 20 10 10 4 89
192
rev bras ortop.2016;51(2):187–193Table3–Resultsfrompatient’sscoresintheLysholm questionnaire.
Lysholmscore Numberof
patients
%ofthe patients
Excellent 06 27.2
Good 07 31.8
Regular 06 27.2
Poor 03 13.8
poorresults(Table3).Alltheparticipantswhoclassifiedtheir resultsaspoorreportedthattheyexperiencedseverepainin thepatellofemoraljointonmakingmajoreffort.However,they hademployment-lawissuesduringtheperiodevaluated.The finalmeanscoreforthequestionnairewas84.6,whichwas gradedasagoodresult.
Intheclinicalevaluationoneyearaftertheoperation,none ofthepatientssaidthattheyhadanymoderateorseverepain uponmakingmediumeffortinvolvingthepatellofemoraljoint orthelocationofinsertionoftheanchorinthedistalfemur,as shownbythevisualanalogscale.Therewasnodeficitofjoint ROMandallthepatientshadnegativeresultsfromthe appre-hensiontest.In16casesinwhichanevaluationatleast30 monthsaftertheoperationwaspossible,theclinicalresults, theclinicalresultsremainedsimilar.
Discussion
Independentofthe etiology ofrecurrent dislocationofthe patella, this isapathological condition that mostlyaffects youngadultsandwomen,1 asalsoobservedinthepresent study.Bothinpost-traumaticandinnon-traumaticcasesin whichconservativetreatmentischosen,instabilitygenerally becomesrecurrentandinmostcases,anatomicalalterations associatedwithtearingoftheMPFLareseen.Aprevious ran-domizedprospectivestudyinwhichpatientswithtraumatic dislocation ofthe patella were evaluated showed that the resultswerebetteraftersurgicaltreatmentthanafter conser-vativetreatment.18
Theparticipantsinthepresentstudydidnotpresentany anatomicalalterations withindicationsforcomplementary orthopedicproceduresthathavebeendevelopedfortreating recurrentdislocationofthepatella.19Mostofthesetechniques havetheaimofrealigningtheextensormechanismand reduc-ingthe lateralizationofthepatella whenthequadricepsis putintoaction.Distalrealignmentprocedures(forcaseswith TT-TGdistancesgreaterthan20mmorcasesofhighpatella) consistofmedializationand/ordistalizationoftheanterior tibialtuberosity.Proximalrealignmentproceduresdependon quadricepscontraction tokeepthe patella inthetrochlear groove. Both of these have shown limited clinical results. However,intactpassivestabilizerssuchastheMPFLhavean importantroleindependentofthemisalignment,withresults thatare more effectivethan those from proximalor distal realignmentprocedures.20
TheMPFLcontributesapproximately50–70%ofthe restric-tiononlateraltranslationofthepatella.Thus,itisthemost importantstabilizerofthe patellaand itsreconstruction is theprimaryprocedureincasesofrecurrentluxation.20Several surgicaltechniqueshavebeendescribed,withdifferenttypes
ofgrafts(artificialligament,patellartendon,quadriceps ten-donorflexortendons)andfixationmethods(bonetunnelin thepatellaandscrewinthefemur;suturinginthepatellaand Endobuttoninthefemur;andanchorinthepatellaandscrew inthefemur,amongothers).21Recentsystematicreviewshave shownthatreconstructionoftheMPFLisaneffective proce-durewithalowrateofrecurrenceofpatellarinstabilityand good functional and subjectiveresults, independent ofthe surgicaltechnique.22
Themethodusingthequadricepstendonasthegraftis commonamongsurgicalproceduresontheknee.Itpresents theadvantagesthatthegraftiseasilyobtainedgraft,nobone tunnelsareneededand,becausethepatellarboneinsertionis maintained,thereismoreeconomicaluseofsurgicalfixation materials.However,italsopresentsvariationsregardingthe thicknessofthegraft(partial ortotal),thetendonsegment usedandthepathfollowedbetweenthesuperomedialsurface ofthepatellaandthemedialfemoralcondyle(subcutaneous orbelowthevastusmedialismuscle).11,23
Thetechniquedescribedhere,inwhichagraftfromthefull thicknessofthemiddlethirdofthequadricepstendonwas used, presentedsatisfactoryefficacy,witharesultthatwas classified asgood accordingtothescorefrom the Lysholm questionnaire. Asdescribed here, it enables the surgeryto belessaggressiveand,becauseoftheanatomicalpathused andbecauseonlyoneextremityiskeptfree,adequate func-tionality for performing routine activities is ensured. This questionnairewaschosenbecauseofitsreliabilityforknee lig-amentinjuriesandbecauseitcontainstheitem“instability”, whichisimportantforevaluatingtheresultsfromasurgical techniqueforligamentreconstruction.
Inrelationtotheclinicalresultsoneyearafterthe oper-ation, no diminution of joint range of motion or positive apprehensiontestswasobserved.Noneofthepatientssaid that they had any moderate or severe pain in the region ofthepatellofemoraljointatrestoruponmakingmedium effort. Among the patients who continued to be followed up,thegoodresultsweremaintained.In13.8%ofthecases, thepatientsreportedexperiencinggreaterpainduringmore intensiveeffort(suchaswalkingformorethan2km). How-ever,theseparticipants,whoweretheoldestparticipantsin thestudy,hademployment-lawissuesandthereforeprobably wishedtoobtainsomeformofsecondaryadvantagethrough thedisease.
The homogenous population obtained for this study, without the presenceofsevere femoropatellar dysplasiaor associatedlesions,makestheresultsmorereliable.Thereisa needforlongfollow-upofthesepatients,sincesome compli-cationsmayonlyhaveemergedaftertheperiodstudied.Pain consequenttojointdegenerationcanbehighlightedamong these,causedbyincreasedmedialretropatellarforce.Given thelowmorbidityandtheresultsthatwereobservedoverthe shortterm,thistechniquecanbequalifiedasagoodoption forMPFLreconstructionsurgery.
Conclusion
reproducibletechnique,withlowmorbidity,whichpresents goodshort-termresultsfortreatingrecurrentdislocationof thepatella.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. FithianDC,PaxtonEW,StoneML,SilvaP,DavisDK,EliasDA,
etal.Epidemiologyandnaturalhistoryofacutepatellar
dislocation.AmJSportsMed.2004;32(5):1114–21.
2. StefancinJJ,ParkerRD.First-timetraumaticpatellar
dislocation:asystematicreview.ClinOrthopRelatRes.
2007;455:93–101.
3. SmithTO,WalkerJ,RussellN.Outcomesofmedial
patellofemoralligamentreconstructionforpatellar
instability:asystematicreview.KneeSurgSportsTraumatol
Arthrosc.2007;15(11):1301–14.
4. ZaffagniniS,ColleF,LopomoN,SharmaB,BignozziS,Dejour
D,etal.Theinfluenceofmedialpatellofemoralligamenton
patellofemoraljointkinematicsandpatellarstability.Knee
SurgSportsTraumatolArthrosc.2013;21(9):2164–71.
5. SmirkC,MorrisH.Theanatomyandreconstructionofthe
medialpatellofemoralligament.Knee.2003;10(3):221–7.
6. EliasDA,WhiteLM,FithianDC.Acutelateralpatellar
dislocationatMRimaging:injurypatternsofmedialpatellar
soft-tissuerestraintsandosteochondralinjuriesofthe
inferomedialpatella.Radiology.2002;225(3):736–43.
7. SugamunaJ,MitaniT,SuzukiN,TezukaM,IsekiF,FujikawaK,
etal.Reconstructionofthemedialpatellofemoralligament.J
TokyoKneeSoc.1990;10:137–48.
8. ElleraGomesJL.Medialpatellofemoralligament
reconstructionforrecurrentdislocationofthepatella:a
preliminaryreport.Arthroscopy.1992;8(3):335–40.
9. ShahJN,HowardJS,FlaniganDC,BrophyRH,CareyJL,
LattermannC.Asystematicreviewofcomplicationsand
failuresassociatedwithmedialpatellofemoralligament
reconstructionforrecurrentpatellardislocation.AmJSports
Med.2012;40(8):1916–23.
10.CamanhoGL,BitarAC,HernandezAJ,OliviR.Medial
patellofemoralligamentreconstruction:anoveltechnique
usingthepatellarligament.Arthroscopy.2007;23(1),
108.e1-4.
11.SteensenRN,DopirakRM,MaurusPB.Asimpletechniquefor
reconstructionofthemedialpatellofemoralligamentusinga
quadricepstendongraft.Arthroscopy.2005;21(3):
365–70.
12.WibergG.Roentgenographicandanatomicstudiesonthe
patellofemoraljointwithspecialreferencetochondromalacia
patellar.AtaOrthopScand.1941;12:319–410.
13.OuterbridgeRE.Theetiologyofchondromalaciapatellae.J
BoneJointSurgBr.1961;43:752–7.
14.PeccinMS,CiconelliR,CohenM.Questionárioespecíficopara
sintomasdojoelhoLysholmKneeScoringScale–traduc¸ãoe
validac¸ãoparaalínguaportuguesa.ActaOrtopBras.
2006;14(5):268–72.
15.AnandKJ,CraigKD.Newperspectivesonthedefinitionof
pain.Pain.1996;67(1):3–6.
16.NomuraE,InoueM,OsadaN.Anatomicalanalysisofthe
medialpatellofemoralligamentoftheknee,especiallythe
femoralattachment.KneeSurgSportsTraumatolArthrosc.
2005;13(7):510–5.
17.WarrenLF,MarshallJL.Thesupportingstructuresandlayers
onthemedialsideoftheknee:ananatomicalanalysis.JBone
JointSurgAm.1979;61(1):56–62.
18.BitarAC,D’EliaCO,DemangeMK,ViegasAC,CamanhoGL.
Estudoprospectivorandomizadosobrealuxac¸ãotraumática
depatela:tratamentoconservadorversusreconstruc¸ãodo
ligamentofemoropatelarmedialcomtendãopatelar–
mínimodedoisanosdeseguimento.RevBrasOrtop.
2011;46(6):675–83.
19.AgliettiP,BuzziR,DeBiaseP,GironF.Surgicaltreatmentof
recurrentdislocationofthepatella.ClinOrthopRelatRes.
1994;308:8–17.
20.SchöttlePB,FucenteseSF,RomeroJ.Clinicalandradiological
outcomeofmedialpatellofemoralligamentreconstruction
withasemitendinosusautograftforpatellainstability.Knee
SurgSportsTraumatolArthrosc.2005;13(7):
516–21.
21.Gonc¸alvesMBJ,CarvalhoJúniorLH,SoaresLFM,Gonc¸alvesTJ,
SantosRL,PereiraML.Reconstruc¸ãodoligamento
patelofemoralmedialparatratamentodaluxac¸ãorecidivante
dapatela.RevBrasOrtop.2011;46(2):160–4.
22.FisherB,NylandJ,BrandE,CurtinB.Medialpatellofemoral
ligamentreconstructionforrecurrentpatellardislocation:a
systematicreviewincludingrehabilitationand
return-to-sportsefficacy.Arthroscopy.2010;26(10):
1384–94.
23.NoyesFR,AlbrightJC.Reconstructionofthemedial
patellofemoralligamentwithautologousquadricepstendon.