Corresponding author: José Augusto Rodrigues Simões
University of Beira Interior CINTESIS – Centre for Research in Health Technologies and Service, Portugal Phone: +351924406127 E-mail: jars@ubi.pt 1Faculty of Health Sciences, University of Beira Interior; ARS Centro, USF Pulsar, Portugal
2 Faculty of Medicine, University of Coimbra; CEISUC – Centre for Health Studies and Research of the University of Coimbra, Portugal
3 University of Beira Interior; CINTESIS – Centre for Research in Health Technologies and Service, Portugal
Submitted: 2 December 2019 Accepted: 16 February 2020 Arch Med Sci
DOI: https://doi.org/10.5114/aoms.2020.93537 Copyright © 2020 Termedia & Banach
Prevalence of polypharmacy in the older adult
population within primary care in Portugal:
a nationwide cross-sectional study
Pedro Augusto Simões1, Luiz Miguel Santiago2, José Augusto Simões3
A b s t r a c t
Introduction: Polypharmacy is commonly defined as the simultaneous use of five or more medications; however, there is a lack of consensus regarding the most appropriate definition. It is a significant predictor of morbidity and mortality. The aim of this study was to determine the prevalence of polypharmacy in the population of older adults attending primary care in Portugal and to identify associated sociodemographic and clinical factors. Material and methods: We conducted a cross-sectional, analytical study in primary care centres from the five Portuguese healthcare administrative regions and the two autonomous regions. We used a random sample of 757 older adult patients provided by the information department of the ministry of health (SPMS) and family doctors from the autonomous regions. Data collection occurred in March 2018. The variables utilised were sociode-mographic characteristics, clinical profile and medication. For each patient, polypharmacy was measured either by the concurrent use of ≥ 5 drugs or by the median number of drugs at the time of data collection. Logistic regres-sion analyses were performed to determine associations between polyphar-macy and other variables.
Results: Polypharmacy (≥ 5 drugs) was present in 77% of the sample. A cut-off of over the median number of drugs was present in 55%. The likeli-hood of having polypharmacy increased significantly with age (OR = 1.05 (1.02–1.08)), number of chronic health problems (OR = 1.24 (1.07–1.45)) and number of prescribers (OR = 4.71 (3.42–6.48)). Cardiovascular, meta-bolic and musculoskeletal medications were the most commonly involved in polypharmacy.
Conclusions: Polypharmacy was a very common occurrence in Portugal. Fu-ture primary healthcare policies should address polypharmacy.
Key words: polypharmacy, aged, multimorbidity.
Introduction
Polypharmacy is commonly defined as the simultaneous use of five or more drugs [1]. But other definitions has been proposed: some au-thors propose a more detailed breakdown of the cut-off (“5 to 7” and
“8 and over”), allowing for the identification of those with an increased risk [2]; Steinman et al. [3] proposes a threshold of 8 medications justified by the fact that below this number, the risk of un-der-use is greater than the risk of polypharmacy or inappropriate prescription; and others consider polypharmacy as the use of inappropriate, ineffec-tive or duplicate medication [4].
Polypharmacy is estimated to affect 30–70% of older adults [5], and it has been associated with an increased risk of falls [6], inappropriate pre-scriptions, reduced patient adherence, drug inter-actions, hospital admissions [7] and mortality [8]. It is estimated that at least 75% of these adverse events are potentially preventable [9]. In some cas-es, an adverse drug reaction can be misinterpreted as a new medical condition and a new drug is pre-scribed, placing the patient at a higher risk of devel-oping additional adverse drug reactions; this prob-lem is known as the “prescribing cascade” [10].
According to Charlesworth et al. [11] the in-creased number of prescription medications seen in older adults in the USA between 1988 and 2010 was driven, in part, by higher use of cardioprotec-tive medications (statins, anti-hypertensives, and antidiabetics). Still the use of antidepressants, as well as the use of medication from other classes and subclasses (proton-pump inhibitors, thyroid hormones, bisphosphonate, among others), also increased.
In Portugal there are a few studies about the prevalence of polypharmacy in some of its regions, none on a national scale. A 2016 study in a pri-mary care health centre in the north of Portugal identified a prevalence of polypharmacy of 59.2%, higher in women (62%) than in men (54.8%) [12]. In the Portuguese public health system the pa-tients can only go to secondary care through re-ferral from primary care, but once in both levels of care both doctors can prescribe and renew all the patient’s medications. The medications’ prescrip-tion occurs through the mandatory naprescrip-tionwide electronic prescription platform (PEM).
The aim of this study was to identify the na-tionwide prevalence of polypharmacy in older adults in Portugal and its sociodemographic and clinical profiles. Although polypharmacy can be linked to drug-drug interactions (both pharmaco-kinetics and pharmacodynamics) and to adverse drug reactions, these results were presented in a previous paper [13]. Moreover, given the lack of consensus for the definition of polypharmacy and since multimorbidity and the use of multiple med-ications is common in older adults [14] we also intended to use a new definition of polypharmacy (equal to or greater than the median number of drugs taken by the population) and compare it to the most commonly used.
Material and methods Study design
A cross-sectional study whose details, defini-tions and methods were previously published [15].
The study was conducted in agreement with the principles of the Declaration of Helsinki and received ethical approval from the Institutional Ethics Committee of the University of Beira In-terior and Portuguese Healthcare Administrative Regions. The reporting of this study conforms to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.
Participants
Since there were 2.18 million older adults (≥ 65 years) in Portugal and the literature suggests that the range of polypharmacy is between 30% and 70%, we assumed the rate to be over 50% because of epidemiological concern for better ev-idence and larger sampling. We estimated a sam-ple of a minimum 742 patients for a 95% CI and a maximum precision error of 5%. In agreement with the geographical distribution of the pop-ulation of Portuguese aged 65 and older across the five mainland healthcare administrative re-gions and two autonomous rere-gions (Madeira and Azores), noted in PORDATA [16], a random sam-ple of 757 patients was provided by the informa-tion department of the ministry of health, SPMS (Serviços Partilhados do Ministério da Saúde), and invited family doctors from autonomous regions, due to lack of digital databases within these re-gions.
Data collection procedures
Data collection occurred in March 2018 (data extracted on March 30th). In brief, the SPMS pro-vided us with an electronic file with the variables of the study from the randomly selected (by pa-tient’s national health number) sample of the five healthcare administrative regions. This electron-ic file contained anonymised information stored in the patient’s electronic medical records. Since SPMS does not have access to electronic medical records from patients in the two autonomous re-gions, we invited two medical doctors, one from each autonomous region, to provide us with the needed information. The patients selected met the inclusion criteria and also had had an appoint-ment in six pre-randomized days of the month. We studied the prescribed medications using the mandatory nationwide PEM [17]. There is an un-known number of over-the-counter medications consumed by the Portuguese population and as they can be bought without prescription, there is no way to access this information. SPMS could not
provide us with information regarding level of ed-ucation, since in most cases it was missing from the medical records.
Outcome variable
For each patient, polypharmacy was measured either by the simultaneous taking of ≥ 5 drugs or by the median number of drugs at the time of data collection. The rationale for such a study re-sides in the lack of consensus regarding definition of polypharmacy [18]; also because of multimor-bidity older patients are consuming an increasing number of medications [19]. There is a study [2] that proposes a threshold of 8 medications, jus-tified by the fact that below this number, there is a big risk of under-use. Prescribed medication (from April 2017 to March 2018) was encoded following the Portuguese pharmacotherapeutic classification using the most discriminative level possible. The Portuguese pharmacotherapeutic classification has similarities with the ATC (Ana-tomical Therapeutic Chemical) classification and was adapted by INFARMED (National Authority of Medicines and Health Problems) [20]. We defined chronic medication as medication prescribed for more than three months.
Independent variables
These were sociodemographic characteristics such as age, gender (male/female), area of resi-dence (in terms of health administrative region) and clinical profile (chronic health problems ac-cording to International Classification of Primary Care, second edition – ICPC-2).
Compliance with ethical standards
Ethical approval was obtained from Institution-al Ethics Committee at the University of Beira In-terior and Portuguese Healthcare Administrative Regions.
Statistical analysis
In addition to the descriptive analysis, we also performed the χ2 test for nominal qualitative char-acteristics. Lastly, we performed a logistic regres-sion with all the statistically significant variables. All testswere two-sided using a significance level of 0.05. Statistical analysis was conducted using SPSS V.24.0.
Results
Characteristics of participants
The sample consisted of 757 people, mean age was 75.5 ±7.9 years (75.1 ±7.9 years for men and 75.8 ±7.8 years for women) and median number
of drugs was 8. Table I shows the characteristics of the sample.
Prevalence of polypharmacy
More than 9 out of 10 older patients (93.4%) were on at least 1 medication, with an overall av-erage of 8.2 (95% CI: 7.9–8.6), 7.5 (95% CI: 7–8) in men and 8.8 (95% CI: 8.3–9.3) in women.
The rate of polypharmacy, use of 5 or more drugs simultaneously, was 77% (95% CI: 74–80%). With a cut-off of equal to or more than the medi-an number of drugs (equal to 8), medi-an importmedi-ant per-centage of polypharmacy 55% (95% CI: 51–58%) remained present.
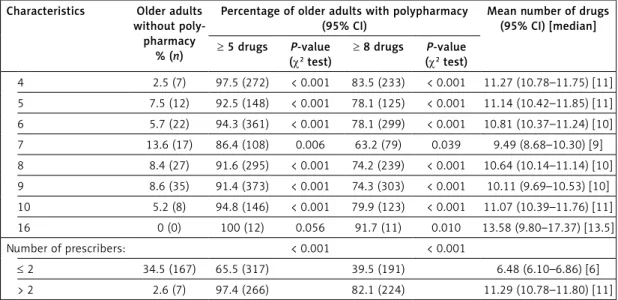
According to Table II there was a significant relationship between health administrative re-gion, age, number of chronic health problems and number of prescribers and both definitions for polypharmacy (≥ 5 drugs and ≥ median number of drugs). Gender was only significant in our new definition of polypharmacy.
After adjustments, Table III shows that the likelihood of having polypharmacy (as ≥ 5 drugs) increased significantly with age (OR = 1.05 (1.02– 1.08)), number of chronic health problems (OR = 1.24 (1.07–1.45)) and number of prescribers (OR = 4.71 (3.42–6.48)).
The likelihood of having polypharmacy with our new definition (as ≥ median of drugs taken by the sample) increased significantly in females (OR = 1.86 (1.24–2.80)), with number of chronic health problems (OR = 1.11 (1.02–1.20)) and number of prescribers (OR = 2.32 (1.97–2.73)).
Pharmacological subclasses and patterns of polypharmacy
Table III shows the odds ratio measured im-pact of having each specific chronic health prob-lem (according to ICPC2). For patients suffering from chronic health problems related to the car-diovascular system there were 3.8 times and 2.4 times greater probability of having polypharmacy (as ≥ 5 drugs and ≥ median number of drugs tak-en, respectively) compared to those not suffer-ing from health problems related to that specific system.
Table IV shows the most used pharmacological subclasses in this random sample. Three pharma-cological subclasses were present in more than half of the sample: ACE inhibitor/ARBs (56.8%), statins (52%) and analgesics and antipyretics (50.6%).
Comparation between both definitions of polypharmacy in detecting potentially inappropriate medication
The common definition (≥ 5 drugs taken) had a sensitivity of 91.3%, specificity of 54.2%,
posi-tive predicposi-tive value of 81.3% and negaposi-tive pre-dictive value of 74.1%.
Our definition (≥ median number of drugs tak-en) had a sensitivity of 72.6%, specificity of 84.0%, positive predictive value of 90.8% and negative predictive value of 58.5%.
The mean number of PIM in older adults with polypharmacy according to the common definition was 2.19 (95% CI: 2.03–2.34) compared to 0.34
(95% CI: 0.24–0.44) in those without polypharma-cy. According to our definition (≥ median number of drugs taken) we found a prevalence of 2.64 PIMs (95% CI: 2.46–2.83) in those with polyphar-macy compared to 0.69 PIMs (95% CI: 0.58–0.80).
Discussion
As described in the project protocol [15], the objectives for its phase I were to identify the
prev-Table I. Characteristics of the sample
Characteristics % (n)
Gender:
Women 56.8 (430)
Men 43.2 (327)
Health administrative region:
North 32.2 (244) Centre 25.1 (190) Lisbon-Tejo Valley 27.7 (210) Alentejo 8.7 (66) Algarve 4.5 (34) Madeira 0.9 (7) Azores 0.8 (6) Age [years]: < 75 51.5 (390) ≥ 75 48.2 (365)
Number of chronic health problems:
0–2 17.3 (131) 3–4 19.3 (146) 5–6 17.6 (133) 7–8 16.8 (127) 9–10 11.9 (90) ≥ 11 17.2 (130)
Chronic health problems (ICPC2)*:
A 11.2 (85) B 7.5 (57) D 36.5 (276) F 20.5 (155) H 11.5 (87) K 77.5 (587) Characteristics % (n) L 51.8 (392) N 15.7 (119) P 34.3 (260) R 23.4 (177) S 19.3 (146) T 68.6 (519) U 21.5 (163) X 9.5 (72) Y 15.2 (115) Z 3.6 (27) Number of drugs: 0–4 23.1 (175) 5–9 39.0 (295) ≥ 10 37.9 (287)
Pharmacological classes (INFARMED):
2 74.5 (564) 3 81.8 (619) 4 36.9 (279) 5 21.1 (160) 6 50.6 (383) 7 16.5 (125) 8 42.5 (322) 9 53.9 (408) 10 20.3 (154) 16 1.6 (12) Number of prescribers: ≤ 2 63.9 (484) > 2 36.1 (273)
A – general and unspecified, B – blood, blood forming organs, lymphatics, spleen, D – digestive, F – eye, H – ear, K – circulatory, L – musculoskeletal, N – neurological, P – psychological, R – respiratory, S – skin, T – endocrine, metabolic and nutritional, U – urology, X – female genital system and breast, Y – male genital system, Z – social problems, 2 – central nervous system, 3 – cardiovascular system, 4 – blood, 5 – respiratory system, 6 – digestive system, 7 – genitourinary system, 8 – hormones and medications used to treat endocrine diseases, 9 – locomotive system, 10 – antiallergic medication, 16 – antineoplastic and immunomodulatory drugs.
Table II. Prevalence of polypharmacy according to characteristics Characteristics Older adults
without poly-pharmacy
% (n)
Percentage of older adults with polypharmacy (95% CI)
Mean number of drugs (95% CI) [median] ≥ 5 drugs P-value (χ2 test) ≥ 8 drugs P-value (χ2 test) Gender: 0.059 < 0.001 Women 20.5 (88) 79.5 (342) 60.5 (260) 8.78 (8.30–9.25) [8] Men 26.3 (86) 73.7 (342) 47.4 (155) 7.47 (6.98–7.96) [7] Health administrative region: 0.022 0.017 North 26.6 (65) 73.4 (179) 49.6 (121) 7.77 (7.18–8.36) [7] Centre 17.9 (34) 82.1 (156) 58.9 (112) 8.62 (7.96–9.28) [8] Lisbon-Tejo Valley 20.0 (42) 80.0 (168) 59.5 (125) 8.69 (8.02–9.36) [8] Alentejo 27.3 (18) 72.7 (48) 53.0 (35) 7.48 (6.33–8.64) [8] Algarve 41.2 (14) 58.8 (20) 41.2 (14) 6.29 (4.49–8.10) [6] Madeira 14.3 (1) 85.7 (6) 28.6 (2) 9.43 (5.13–13.73) [6] Azores 0 (0) 100 (6) 100 (6) 14.17 (9.50–18.83) [13] Age [years]: < 0.001 0.001 < 75 28.2 (110) 71.8 (280) 49.2 (192) 7.73 (7.25–8.22) [7] ≥ 75 17.4 (64) 82.6 (303) 60.8 (223) 8.72 (8.24–9.21) [9] Number of chronic health problems < 0.001 < 0.001 0-2 48.1 (63) 51.9 (68) 35.9 (47) 5.44 (4.67–6.21) [5] 3-4 35.6 (52) 64.4 (94) 41.1 (60) 6.97 (6.17–7.78) [6] 5-6 23.3 (31) 76.7 (102) 48.1 (64) 7.80 (7.06–8.55) [7] 7-8 12.6 (16) 87.4 (111) 63.8 (81) 9.22 (8.50–9.94) [9] 9-10 7.8 (7) 92.2 (83) 64.4 (58) 9.21 (8.36–10.06) [9] ≥ 11 3.8 (5) 96.2 (125) 80.8 (105) 11.15 (10.34–11.95) [10] Chronic health problems (ICPC2): A 10.6 (9) 89.4 (76) 0.004 62.4 (53) 0.139 9.40 (8.42–10.38) [9] B 15.8 (9) 84.2 (48) 0.179 66.7 (38) 0.062 9.25 (7.98–10.52) [9] D 13.0 (36) 87.0 (240) < 0.001 60.1 (166) 0.026 8.93 (8.38–9.49) [8,5] F 17.4 (27) 82.6 (128) 0.065 63.9 (99) 0.011 9.25 (8.43–10.08) [9] H 12.6 (11) 87.4 (76) 0.015 63.2 (55) 0.094 9.70 (8.58–10.82) [9] K 16.9 (99) 83.1 (488) < 0.001 61.2 (359) < 0.001 8.98 (8.60–9.37) [9] L 17.6 (69) 82.4 (323) < 0.001 62.0 (243) < 0.001 8.95 (8.49–9.42) [8] N 16.0 (19) 84.0 (100) 0.047 67.2 (80) 0.003 10.06 (9.13–10.99) [10] P 16.5 (43) 83.5 (217) 0.002 60.4 (157) 0.026 9.01 (8.43–9.59) [8] R 10.7 (19) 89.3 (158) < 0.001 67.2 (119) < 0.001 9.72 (9.03–10.41) [9] S 19.2 (28) 80.8 (118) 0.224 56.2 (82) 0.717 8.66 (7.87–9.44) [8] T 17.3 (90) 82.7 (429) < 0.001 60.5 (314) < 0.001 8.97 (8.56–9.38) [9] U 16.0 (26) 84.0 (137) 0.016 65.0 (106) 0.003 9.09 (8.35–9.83) [9] X* 10.9 (7) 89.1 (57) 0.041 67.2 (43) 0.233 9.72 (8.45–10.99) [10] Y** 19.1 (22) 80.9 (93) 0.030 58.3 (67) 0.004 8.63 (7.78–9.47) [8] Z 18.5 (5) 81.5 (22) 0.574 63.0 (17) 0.387 9.44 (7.65–11.24) [10] Pharmacological classes (INFARMED): 2 9.2 (52) 90.8 (512) < 0.001 68.8 (388) < 0.001 9.77 (9.42–10.12) [9] 3 11.8 (73) 88.2 (546) < 0.001 63.8 (395) < 0.001 9.35 (9.01–9.69) [9]
alence and its characteristics of polypharmacy and PIMs in the elderly Portuguese population. The results related to the PIMs have already been published [13], but they are not necessarily relat-ed to the polypharmacy.
Strengths of the study
This was the first study to report the prevalence and patterns of polypharmacy in older adults at-tending primary care consultations on a national scale in Portugal.
We performed a cross-sectional study, which is the most frequent design to assess prevalence and its characteristics.
We used the most discriminative chemical sub-group of the Portuguese pharmacotherapeutic classification, to assess polypharmacy; this can minimize the bias of medical changes.
We assessed the number of medications taken by older adults using doctor’s prescription records to minimise memory bias.
Since the data were mainly obtained by SPMS from national records (which allowed for a more representative sample of the population) and by sampling according to the patient’s national health number in most health regions, we avoided over-representation of frequent users of primary care services (normally the ones with a higher number of morbidities and medication).
Statement of overall findings
The study results show a high prevalence of polypharmacy in the Portuguese older population
(77%), exceeding the reported prevalence of oth-er studies (30–70%) [5]. One of the explanations can be the period of time we used in this study (12-months), which can increase polypharmacy [21], making this high prevalence misrepresenta-tive of reality, since medication could have been ceased. We used a more prolonged period of time because we believed it would allow differentiation between chronic and acute medication, done by evaluating the number of times each medication was prescribed in order to obtain a more accu-rate value [22]. Further research is needed to bet-ter assess which methodology is more suitable, a 12-month or a 6-month period.
Another possible explanation is that we as-sessed the prescribed drugs and not the ones that were dispensed or consumed by the patient (ther-apeutic adhesion). This may be misrepresentative of reality; patients could have stopped taking their medication (due to adverse effects, financial prob-lems, etc.) and not have informed their doctor. On the other hand, we did not consider over-the-counter medications and the medications pre-scribed without the use of the electronic program PEM (e.g. manually), which may have a residual effect.
It is likely that differences in the rate of poly-pharmacy can be found at the prescriber level [14]. This variation could be explained by practi-tioners single-handedly treating diseases and ill-nesses and the lack of guidelines regarding poly-pharmacy or its prescription [23]. However, efforts to address polypharmacy within evidence-based deprescribing guidelines are being pursued [24].
Characteristics Older adults without poly-pharmacy
% (n)
Percentage of older adults with polypharmacy (95% CI)
Mean number of drugs (95% CI) [median] ≥ 5 drugs P-value (χ2 test) ≥ 8 drugs P-value (χ2 test) 4 2.5 (7) 97.5 (272) < 0.001 83.5 (233) < 0.001 11.27 (10.78–11.75) [11] 5 7.5 (12) 92.5 (148) < 0.001 78.1 (125) < 0.001 11.14 (10.42–11.85) [11] 6 5.7 (22) 94.3 (361) < 0.001 78.1 (299) < 0.001 10.81 (10.37–11.24) [10] 7 13.6 (17) 86.4 (108) 0.006 63.2 (79) 0.039 9.49 (8.68–10.30) [9] 8 8.4 (27) 91.6 (295) < 0.001 74.2 (239) < 0.001 10.64 (10.14–11.14) [10] 9 8.6 (35) 91.4 (373) < 0.001 74.3 (303) < 0.001 10.11 (9.69–10.53) [10] 10 5.2 (8) 94.8 (146) < 0.001 79.9 (123) < 0.001 11.07 (10.39–11.76) [11] 16 0 (0) 100 (12) 0.056 91.7 (11) 0.010 13.58 (9.80–17.37) [13.5] Number of prescribers: < 0.001 < 0.001 ≤ 2 34.5 (167) 65.5 (317) 39.5 (191) 6.48 (6.10–6.86) [6] > 2 2.6 (7) 97.4 (266) 82.1 (224) 11.29 (10.78–11.80) [11]
*Considering only women, **considering only men. A – general and unspecified, B – blood, blood forming organs, lymphatics, spleen, D – digestive, F – eye, H – ear, K – circulatory, L – musculoskeletal, N – neurological, P – psychological, R – respiratory, S – skin, T – endocrine, metabolic and nutritional, U – urology, X – female genital system and breast, Y – male genital system, Z – social problems, 2 – central nervous system, 3 – cardiovascular system, 4 – blood, 5 – respiratory system, 6 – digestive system, 7 – genitourinary system, 8 – hormones and medications used to treat endocrine diseases, 9 – locomotive system, 10 – antiallergic medication, 16 – antineoplastic and immunomodulatory drugs.
Table III. Logistic regression model for polypharmacy Characteristics Polypharmacy ≥ 5 drugs ≥ 8 drugs OR 95% CI P-value OR 95% CI P-value Gender: Women – – – 1.86 1.24–2.80 0.003 Men – – – Base – – Age 1.05 1.02–1.08 0.002 1.02 1.00–1.04 0.109 Number of chronic health problems: 1.24 1.07–1.45 0.005 1.11 1.02–1.20 0.016 A 1.17 0.47–3.00 0.735 – – – D 1.55 0.88–2.75 0.131 0.77 0.51–1.16 0.204 F – – – 0.91 0.56–1.47 0.696 H 1.20 0.49–2.91 0.688 – – – K 2.43 1.37–4.30 0.002 2.53 1.56–4.11 < 0.001 L 0.66 0.39–1.13 0.130 0.99 0.67–1.48 0.974 N 0.62 0.31–1.27 0.195 1.13 0.68–1.87 0.644 P 0.98 0.55–1.75 0.953 0.96 0.64–1.46 0.851 R 1.19 0.61–2.33 0.619 1.06 0.68–1.67 0.788 T 1.49 0.86–2.61 0.159 1.32 0.87–2.01 0.192 U 0.67 0.35–1.26 0.214 1.03 0.64–1.65 0.909 X 1.24 0.45–3.38 0.678 – – – Y 0-77 0.39–1.53 0.451 1.33 0.75–2.33 0.329 Number of prescribers 4.71 3.42–6.48 < 0.001 2.32 1.97–2.73 < 0.001
OR – odds ratio, A – general and unspecified, D – digestive, F – eye, H – ear, K – circulatory, L – musculoskeletal, N – neurological, P – psychological, R – respiratory, S – skin, T – endocrine, metabolic and nutritional, U – urology, X – female genital system and breast, Y – male genital system.
Table IV. Fifteen most used pharmacological subclasses and common chronic health problems INFARMED pharmacotherapeutic
classification
% (n) ICPC-2 chronic health problems % (n)
3.4.2 ACE inhibitor/ARBs 56.8 (430) K86 Hypertension uncomplicated 54.7 (414)
3.7.1 Statins 52.0 (394) T93 Lipid disorder 48.1 (364)
2.10 Analgesics and antipyretics 50.6 (383) T90 Diabetes non-insulin dependent 24.0 (182)
6.2.2.3 PPIs 38.2 (289) L86 Back syndrome with radiating pain 17.7 (134)
3.4.1.1 Thiazide 37.5 (284) L90 Osteoarthrosis of knee 16.2 (123)
2.9.1.3 Benzodiazepines 33.6 (254) T82 Obesity 14.8 (112)
3.4.3 Calcium channel blockers 26.7 (202) K87 Hypertension complicated 14.1 (107)
2.9.3 Antidepressants 24.7 (187) P76 Depressive disorder 13.2 (100)
4.3.1.3 Antiplatelet agents 23.6 (179) Y85 Benign prostatic hypertrophy 12.9 (98) 9.1.3 NSAIDs – propionic acid
derivatives
22.3 (169) T83 Overweight 12.2 (92)
3.4.4.2 β-Blockers 21.9 (166) L91 Osteoarthrosis other 10.8 (82)
8.4.2.1 Biguanide 21.4 (162) K95 Varicose veins of leg 10.0 (76)
8.2 Corticosteroids 18.1 (137) F92 Cataract 9.4 (71)
10.1.2 H1 non-sedative antihistamines 17.7 (134) P74 Anxiety disorder/anxiety state 9.4 (71) 2.12 Narcotic analgesics 15.3 (116) L87 Bursitis/tendinitis/synovitis NOS 8.6 (65)
In line with previous reports [11, 25, 26], we found a significant association between increased age and prevalence of polypharmacy. This could be due to the increase in the prevalence of age-re-lated chronic diseases, which are accompanied by an increase in medications and possibly also because of prescribing for social problems [27]. However, in our new definition (≥ median number of drugs taken) there was not a significant asso-ciation between increased age and prevalence of polypharmacy. This could be due to the increase of the threshold of polypharmacy that can pre-vent labelling older adults with polypharmacy just because of the increase of comorbidities and drugs that may be necessary for them, commonly referred to as appropriate polypharmacy, as sug-gested by Steinman et al. [3].
There was no difference in risk of polypharmacy between genders with the common definition of polypharmacy. Our findings were in line with those of other studies [11, 28]. However, there are stud-ies that found an increased risk of polypharmacy in men [26] and women [14, 25]. A higher prev-alence of polypharmacy was also present in our study when we considered polypharmacy as a val-ue equal to or greater than the median number of drugs (≥ 8) taken by the population. One explana-tion can be that women tend to live longer than men, hence having more chronic health problems and needing more drugs. However, more studies are needed to assess whether there is a difference in risk of polypharmacy between genders.
As expected, the number of chronic health problems affects the number of medications tak-en by the patitak-ent and this association has betak-en well described in the literature [11, 14, 25, 28]. However, in our study there were some chronic health problems with a stronger impact on the risk of polypharmacy, for example group classifi-cation D (digestive problems) for polypharmacy as ≥ 5 drugs and K (cardiovascular) for our definition (≥ the median number of drugs taken).
A higher number of prescribers per patient was associated with higher risk of polypharmacy, namely for the common definition (≥ 5). One ex-planation is that having multiple prescribers may unknowingly duplicate or induce contraindicated medication regimens due to lack of information available, which increases the risk of serious ad-verse drug events [29]. On the other hand, more complex patients (with multimorbidity) need to be assisted by more doctors and take more drugs. To our knowledge, this is one of the first studies to assess the impact of having multiple prescribers on polypharmacy.
In agreement with previous reports [14, 26], car-diovascular, metabolic and musculoskeletal medi-cations were the most common in our study sam-ple. This is in line with the most common chronic
health problems described in Portugal [19], which are cardiovascular (such as lipid disorder and hy-pertension), metabolic (such as diabetes and obe-sity) and musculoskeletal (such as back pain syn-drome, osteoarthritis and osteoarthrosis) problems [30]. This highlights the importance of prescribing the best drug option for the patient.
Our proposed definition had better specific-ity in detecting PIM than the common defini-tion, which means a much lower number of false positive “results”. This occurred at the cost of diminished sensitivity. However, we found a sim-ilar mean number of PIMs in both groups (with polypharmacy and without) according to both definitions. These results are in line with those of Steinman et al. [3], which raises the question of whether we should raise the threshold to avoid the risk of under-use as there does not seem to be a greater risk of inappropriate prescription. The advantage of our definition compared to others that propose a higher threshold is that it is not a rigid definition and can be adapted to a specific population morbidity burden, since different pop-ulations have different needs. Therefore, it would be like standardizing the risk of inappropriate pre-scription according to the population’s morbidity burden to help us compare the impact of different health systems and policies on this problem.
There are some limitations in this study. Firstly, we used a 12-month period to assess the chronic prescribed medication, which can in-crease the prevalence of polypharmacy, since med-ication could have been ceased or not purchased (non-compliance). Therefore, the number of medi-cations per older adult may be overestimated.
Secondly, since the SPMS could not provide us with data from both autonomous regions (Madei-ra and Azores), representing 1.7% of the sample, data were collected by local GPs, making the sam-ple and data processes in these two regions dif-ferent from the rest. Nevertheless, randomisation was performed for these data.
Thirdly, we intended to evaluate the effects of level of education on polypharmacy. This was not possible due to lack of information in the patients’ electronic records.
Fourthly, the sample size was chosen to achieve a sufficiently precise overall proportion estimate of polypharmacy in the Portuguese older adults’ population, but not to find differences among dif-ferent population strata.
Fifthly, we could not find any study using an approach like ours (polypharmacy as ≥ median number of drugs taken by the population) and had great difficulty making comparisons between different studies.
Sixthly, we could not have data on over-the-counter medications, so the prevalence of poly-pharmacy may be underestimated.
Finally, this was a cross-sectional study and so no causal relationship could be proven, and we could not study the health consequences of polypharmacy, namely drug-drug interactions and adverse drug reactions. Therefore, longitu-dinal studies are needed to understand whether these factors are responsible for the prevalence of polypharmacy. However, we intended to study prevalence and raise questions and not determine causality, so other studies are required to study causality, frequency and outcomes.
In conclusion, this study found a high preva-lence of polypharmacy in the studied sample; the most important factors were number of chronic health problems and number of prescribers in both used definitions and age in the most common definition and being female in our new definition.
Polypharmacy should consider medical con-straints, pathological needs and patients’ feelings and fears, implying future studies on the accurate-ness of prescription and the need of deprescrip-tion.
We think that our new definition of polyphar-macy is of relevance for practitioners since it will identify patients with higher risks. However, fur-ther studies are needed to increase its reliability and usefulness.
Acknowledgments
The authors thank the SPMS, Nivalda Pereira and Tânia Bairos for their participation in the data collection.
Conflict of interest
The authors declare no conflict of interest. R e f e r e n c e s
1. Gnjidic D, Hilmer SN, Blyth FM, et al. Polypharmacy cut-off and outcomes: five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J Clin Epidemiol 2012; 65: 989-95.
2. Preskorn SH, Silkey B, Shah R, et al. Complexity of med-ication use in the veterans affairs healthcare system. Part I: Outpatient use in relation to age and number of prescribers. J Psychiatr Pract 2005; 11: 5-15.
3. Steinman MA, Seth Landefeld C, Rosenthal GE, Berthen-thal D, Sen S, Kaboli PJ. Polypharmacy and prescribing qual-ity in older people. J Am Geriatr Soc 2006; 54: 1516-23. 4. Maher RL, Hanlon J, Hajjar ER. Clinical consequences of
polypharmacy in elderly. Expert Opin Drug Saf 2014; 13: 57-65.
5. Machado-Alba JE, Gaviria-Mendoza A, Machado-Du- que ME, Chica L. Deprescribing: a new goal focused on the patient. Expert Opin Drug Saf 2017; 16: 111-2. 6. Ziere G, Dieleman JP, Hofman A, Pols HAP, Van Der
Cam-men TJM, Stricker BHC. Polypharmacy and falls in the middle age and elderly population. Br J Clin Pharmacol 2006; 61: 218-23.
7. Bourgeois FT, Shannon MW, Valim C, Mandl KD. Adverse drug events in the outpatient setting: an 11-year na-tional analysis. Pharmacoepidemiol Drug Saf 2010; 19: 901-10.
8. Jyrkkä J, Enlund H, Korhonen MJ, Sulkava R, Hartikai- nen S. Polypharmacy status as an indicator of mortality in an elderly population. Drugs Aging 2009; 26: 1039-48. 9. Scott IA, Anderson K, Freeman CR, Stowasser DA. First do no harm: a real need to deprescribe in older patients. Med J Aust 2014; 201: 390-2.
10. Rochon PA, Gurwitz JH. Optimising drug treatment for elderly people: the prescribing cascade. Br Med J 1997; 315: 1096-9.
11. Charlesworth CJ, Smit E, Lee DSH, Alramadhan F, Od- den MC. Polypharmacy among adults aged 65 years and older in the United States: 1988–2010. J Gerontol Ser A Biol Sci Med Sci 2015; 70: 989-95.
12. Eiras A, Teixeira MA, Gonzalez-Montalvo JI, Castell MV, Queipo R, Otero A. Consumption of drugs in over 65 in Porto (Portugal) and risk of potentially inappropri-ate medication prescribing. Aten Primaria 2016; 48: 110-20.
13. Simões PA, Santiago LM, Maurício K, Simões JA. Prev-alence of potentially inappropriate medication in the older adult population within primary care in Portugal: a nationwide cross-sectional study. Patient Prefer Ad-herence 2019; 13: 1569-76.
14. Ong SM, Lim YMF, Sivasampu S, Khoo EM. Variation of polypharmacy in older primary care attenders occurs at prescriber level. BMC Geriatr 2018; 18: 59.
15. Simões PA, Santiago LM, Simões JA. Deprescribing in primary care in Portugal (DePil17-20): a three-phase observational and experimental study protocol. BMJ Open 2018; 8: 1-6.
16. PORDATA – Contemporary Portugal Database [homep-age on the Internet]. Lisbon: Fundação Francisco Man-uel dos Santos; 2009. Available from: https://www.por-data.pt/en/Home. Accessed February 19 2018. 17. Patrao L, Deveza R, Martins H. PEM – a new patient
cen-tred electronic prescription platform. Procedia Technol 2013; 9: 1313-9.
18. Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr 2017; 17: 230.
19. Prazeres F, Santiago L. Prevalence of multimorbidity in the adult population attending primary care in Portugal: a cross-sectional study. BMJ Open 2015; 5: e009287. 20. Vademecum: DCI em Português [homepage on the
in-ternet]. Lisbon:INFARMED; 2005. Available from: http:// www.infarmed.pt/documents/15786/17838/vademe-cum.pdf/f85294bb-db17-4d18-aaab-f394fbbb963e. Acessed February 19 2018.
21. Hovstadius B, Åstrand B, Petersson G. Dispensed drugs and multiple medications in the Swedish population: an individual-based register study. BMC Clin Pharmacol 2009; 9: 11.
22. Fincke BG, Snyder K, Cantillon C, et al. Three complemen-tary definitions of polypharmacy: methods, application and comparison of findings in a large prescription da-tabase. Pharmacoepidemiol Drug Saf 2005; 14: 121-8. 23. Molokhia M, Majeed A. Current and future perspectives
on the management of polypharmacy. BMC Fam Pract 2017; 18: 70.
24. Developing an evidence-based deprescribing guideline: instruction manual for guideline coordinators (work-ing document) [homepage on the internet]. WONCA EUROPE: Thompson W, Pizzola L, Hogel M, Black C,
Far-rell B; 2018. Available from: https://deprescribing.org/ wp-content/uploads/2016/03/Preprescribing_Docu-ment_2018_inhouse.pdf.
25. Morin L, Johnell K, Laroche ML, Fastbom J, Wastes- son JW. The epidemiology of polypharmacy in older adults: register-based prospective cohort study. Clin Ep-idemiol 2018; 10: 289-98.
26. Slabaugh SL, Maio V, Templin M, Abouzaid S. Preva-lence and risk of polypharmacy among the elderly in an outpatient setting: a retrospective cohort study in the Emilia-Romagna region, Italy. Drugs Aging 2010; 27: 1019-28.
27. Monégat M, Sermet C, Perronnin M, Rococo E. Polyphar-macy: definitions, measurement and stakes involved. review of the literature and measurement tests. Inst Rech Doc En Économie La Santé 2014; 204: 1-8. 28. Prithviraj GK, Koroukian S, Margevicius S, Berger NA,
Bagai R, Owusu C. Patient characteristics associated with polypharmacy and inappropriate prescribing of medications among older adults with cancer. J Geriatr Oncol 2012; 3: 228-37.
29. Groysberg B, Polzer JT, Elfenbein HA. Too many cooks spoil the broth: how high-status individuals decrease group effectiveness. Organ Sci 2011; 22: 722-37. 30. Bromfield SG, Ngameni CA, Colantonio LD, et al. Blood
pressure, antihypertensive polypharmacy, frailty, and risk for serious fall injuries among older treated adults with hypertension. Hypertension 2017; 70: 259-66.