www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
Comparison
of
turbinoplasty
surgery
efficacy
in
patients
with
and
without
allergic
rhinitis
夽
,
夽夽
Rodrigo
Hamerschmidt
a,f,∗,
Rogério
Hamerschmidt
a,b,f,
Ana
Tereza
Ramos
Moreira
b,c,
Sérgio
Bernardo
Tenório
b,d,
Jorge
Rufno
Ribas
Timi
b,eaDepartmentofOtorhinolaryngology,UniversidadeFederaldoParaná(UFPR),Curitiba,PR,Brazil bHospitaldeClínicas,UniversidadeFederaldoParaná(UFPR),Curitiba,PR,Brazil
cDepartmentofOphthalmology,UniversidadeFederaldoParaná(UFPR),Curitiba,PR,Brazil dDepartmentofAnesthesiology,UniversidadeFederaldoParaná(UFPR),Curitiba,PR,Brazil eVascularSurgery,UniversidadeFederaldoParaná(UFPR),Curitiba,PR,Brazil
fClinicalSurgery,UniversidadeFederaldoParaná(UFPR),Curitiba,PR,Brazil
Received26July2014;accepted23January2015 Availableonline6November2015
KEYWORDS
Turbinates; Rhinitis;
Olfactiondisorders; Smell;
Snoring;
Nasalobstruction
Abstract
Introduction:Turbinoplastyisaprocedurethataimstoreducethesizeoftheinferiorturbinate through exuberant boneremoval with highmucosal preservation. The procedure is recom-mendedforpatientswithorwithoutallergicrhinitisandthoseshowingirreversiblehypertrophy ofinferiorturbinates.
Objective: Toevaluatetheefficacyofinferiorturbinoplastyforobstructiveandnon-obstructive symptomsinpatientswithorwithoutallergicrhinitis.
Methods:Prospectivestudywith57patientswhounderwentinferiorturbinoplasty.Theywere evaluated for nasal obstruction, snoring, facialpressure, smell alterations, sneezing,nasal itchingandrunnynosesymptoms,surgerytime,andintraoperativebleeding.Thelastevaluation tookplacethreemonthsaftersurgery.
Results:Thirty-ninepatientswithallergicrhinitisand18withoutwereassessed.Ninetydays after surgery,94.7% ofpatients showeddegrees IV andV ofbreathingimprovement; 89.5% showed moderate orcomplete improvementinsnoring; allpatients showed smell improve-ment(only oneshowedmoderateimprovement;alltheothershadfullimprovement);95.5% experiencedcompletefacialpressureimprovement;and89.7%showedmoderatetocomplete improvementinnasalitchingandrunnynosesymptoms,aswellasinsneezing.
夽 Pleasecitethisarticleas:HamerschmidtR,HamerschmidtR,MoreiraATR,TenórioSB,TimiJRR.Comparisonofturbinoplastysurgery
efficacyinpatientswithandwithoutallergicrhinitis.BrazJOtorhinolaryngol.2016;82:131---9.
夽夽Institution:UniversidadeFederaldoParaná(UFPR),Curitiba,PR,Brazil.
∗Correspondingauthor.
E-mail:rodrigohsch@hotmail.com(R.Hamerschmidt). http://dx.doi.org/10.1016/j.bjorl.2015.10.010
Conclusion:Theefficacyofinferiorturbinoplastywasconfirmednotonlyforobstructive symp-toms,butalsofornon-obstructivesymptomsinpatientswithandwithoutallergicrhinitis. © 2015 Associac¸ão Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial. Published by Elsevier Editora Ltda. This is an open access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/).
PALAVRASCHAVE
Conchasnasais; Rinite;
Durac¸ãodacirurgia; Olfato;
Ronco;
Obstruc¸ãonasal
Comparac¸ãodaeficáciadaturbinoplastiaempacientescomesemrinitealérgica
Resumo
Introduc¸ão:Aturbinoplastiaéprocedimentoquevisaareduc¸ãodaconchainferior,àcustada remoc¸ãoósseaexuberanteemaiorpreservac¸ãodamucosa.Éindicadaparapacientescome semrinitealérgica,comhipertrofiairreversíveldasconchasinferiores.
Objetivo:Avaliaraeficáciadacirurgiadeturbinoplastiainferiornossintomasobstrutivosenão obstrutivosempacientescomesemrinitealérgica.
Método: Estudoprospectivocom57pacientessubmetidosaturbinoplastiainferior.Foram avali-adosquantoàobstruc¸ãonasal,roncos,pressãofacial,alterac¸õesnoolfato,espirros,prurido nasalecoriza,tempodecirurgiaesangramentointraoperatório.Aúltimaavaliac¸ãofoicom3 mesesdeoperac¸ão.
Resultados: 39pacientescomrinitealérgicae18sem.Com90diasdeoperac¸ão,94,7%dos pacientesapresentaramgrausIVeVdemelhoranarespirac¸ão;89,5%apresentarammelhora moderadaoutotaldosroncos;todosospacientestiverammelhoranoolfato(apenas1 mod-erada, osdemais melhoratotal); 95,5% obtiverammelhora total dapressão faciale 89,7% obtiverammelhoramoderadaoutotalempruridonasal,espirrosecoriza.
Conclusão:Comprovou-seaeficáciadacirurgiadeturbinoplastiainferiornãosónossintomas obstrutivos,mastambémnossintomasnãoobstrutivostantoempacientescomousemrinite alérgica.
© 2015 Associac¸ão Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial. Publi-cado por Elsevier Editora Ltda. Este é um artigo Open Access sob a licença CC BY (https://creativecommons.org/licenses/by/4.0/deed.pt).
Introduction
Nasal obstruction affects approximately 25% of the population.1 It is a symptom that can affect people of
all ages and ethnicities. It has some degree of morbid-ity, which varies with the severity and cause of nasal obstruction. The main causes are: septal deviation, infe-rior and medial turbinate hypertrophy, nasal polyps, and pharyngealtonsilhypertrophy.1Ofallofthesealterations,
inferiorturbinatehypertrophyisthemostcommoncauseof nasalobstruction.2Theleadingcausesofinferiorturbinate
hypertrophy are allergic rhinitis, vasomotor rhinitis, and septal deviation (compensatory hypertrophy).3 Bilateral
nasalobstructionusuallyoccurswithmucosaldisease.When associatedwithwateryrhinorrhea,sneezing,andnasal itch-ing,itischaracteristicofnasalmucosainflammatoryedema, especiallyofallergicnature.4
Rhinitisistheinflammationofthenasalmucosallining, characterized by the presence of one or more symp-toms:nasalcongestion, rhinorrhea,sneezing,itching,and hyposmia.5 Nasal obstruction is one of the most
inconve-nientsymptomsfor thepatient.4 Thediagnosis ofallergic
rhinitisincludespersonalandfamilyhistoryofatopy, physi-calexamination,andcomplementaryexams.Thediagnosis isessentiallyclinical,takingintoaccounttheassociationof theseveralsymptoms.5Themostimportantcomplementary
exams inthe diagnosis of allergicrhinitis, for both speci-ficity and sensitivity, are immediate hypersensitivity skin pricktest(SPT)usingthepuncturetechniqueandevaluation ofserumlevelsofallergen-specificIgE.5
ThedeterminationofspecificIgEinvitromaybe accom-plishedbyseveralenzymeimmunoassaymethods,andmore recently,byimmunofluorescence.SpecificIgEassayinvitro
forindividualallergens,whenperformedwithstandardized antigens and adequate technique, has operational char-acteristics (sensitivity and specificity) that are similar to those of the skin prick test: sensitivity of 89% and speci-ficityof91%.5Treatmentincludesbothnon-pharmacological
---environmental control---andpharmacologicalmeasures. Thelatterarebasedonantihistamines,decongestants, top-ical and systemic corticoids, and other medications such asipratropiumbromide,chromoglycatedisodium,and anti-leukotrienes.
Immunotherapyandtheuseof salinesolutionfor nasal irrigation are other choices. Modern pharmacology offers many options for clinical treatment of inferior turbinate hypertrophy,whateverthesourceis.However,althoughstill a controversial issue, most authors agreethat when clin-icaltreatment is not sufficient toprovide adequate nasal airways,surgicaltreatmentshouldbeindicated.6,7
aims to increase the nasal cavity without altering nasal physiology.5Thesearchforeffectivenasalturbinate
treat-menthasstimulatedthesurgicalskillofrhinologistsforover 100years.8
Surgical procedures that aim to reduce mucosal or boneyhypertrophyoftheinferiornasalturbinate,orboth, include: corticosteroid infiltration, lateral dislocation of the nasal turbinate, partial turbinectomy, lower turbino-plasty,cryosurgery,laservaporization,andradiofrequency. Turbinoplasty is a procedure aimed at reducing the size of theinferior turbinate throughexuberant bone removal and meatalsurface removalwithgreater mucosal preser-vation. Itallowsreductionofthe turbinatevolume,while maintainingthe physiological functions ofthe mucosa.4 It
is performed through an incision along the border of the turbinates,detachmentandexposureofthebonesurface, followed by bone and redundant mucosa removal, cover-ing the remaining bone with the excess mucosa.4 Nasal
turbinatesurgeryisoneofthemostfrequentlyperformed procedures in otorhinolaryngologists’ daily practice, rec-ognized as an effective treatment for nasal obstruction secondarytohypertrophicrhinitis.9
Serrano et al. followed 71 patients submitted to infe-riorturbinate surgery for at leastone year, andover 80% attainedimprovementwiththeoperation.9 In2009,Batra
etal.carriedoutaliteraturereviewof514studiesto ver-ifywhethertheinferiorturbinatesurgeryimprovesquality oflife, symptoms,and objectiveparameterswithatleast six months of follow-up. It was concluded that there is level4and5evidenceoftheoperation’sefficacyinadults withsymptomatichypertrophyofinferiorturbinates.10
Put-ermanetal.haveperformedturbinoplastiessince2002with excellentresults andminimal adverse effects.The proce-dureremoved thelateralmucosaandboneof theinferior turbinate.11Theinferiorturbinatereductionprocedurehad
apositiveimpactinpatientswithpersistentallergicrhinitis withclinicaltreatment.12
Morietal.studied,inasampleof45patients,theefficacy ofturbinectomyonrhinitissymptomsafterfiveyears,and concludedthattheoperationisausefulstrategytocontrol allergicrhinitissymptomsandhelpstoimprovethequality oflife,withsignificant improvementinsymptomsofnasal obstruction(70%)andsneezing(50%).13Muccietal.intheir
sampleof55patients,emphasizedtheimprovementinnasal obstructionin90%ofpatientssubmittedtoinferiorturbinate surgery, aswellasimprovement in symptomssuchas rhi-norrhea,headache,andsnoring.14Brandarkaretal.stated
thattheinferiorturbinatesurgerywaseffectiveandremains thebesttreatmentforhypertrophyunresponsivetomedical therapy.15
Thereareseveralstudiesintheliteraturethatassessed the improvement in nasal obstruction after the inferior turbinate operation. However, the literature is poor in assessingtheimpactofturbinatesurgeryonsymptomssuch as rhinorrhea, sneezing, and nasal itching.16,17 It is also
poorin assessing symptomssuchasanosmia,snoring, and headache.Fewstudieshavecomparedpostoperative symp-toms in patients with and without allergic rhinitis (AR) submittedtoinferiorturbinateoperation.
Theaimofthisstudyistoassesstheefficacyofinferior turbinoplasty surgery on obstructive and non-obstructive symptomsinpatientswithandwithoutallergicrhinitis.
Methods
This longitudinal contemporary cohort study involved 57 patientstreatedonanoutpatientbasis,prospectively eval-uatedandsubmittedtoinferiorturbinoplastysurgeryfrom JanuarytoDecember2013,allperformedinthesame hos-pital, after approval by the Research Ethics Committee underNo.0005/2012-05.Allpatientshadinferiorturbinate hypertrophy and nasal obstruction refractory to medical treatmentwithat leasttwomonthsof topicalnasal corti-costeroidandsystemicantihistamineuse,andnoothernasal conditions,suchasseptaldeviation,middleconchabullosa, orhypertrophicmiddleturbinate.
Patientsweredividedintotwogroups:groupI---patients withnasalobstructionandsymptomsofrhinorrhea, sneez-ing, and itchy nose --- were considered as having allergic rhinitis; and group II --- patients with nasal obstruction withoutthe other described symptoms---were considered withoutallergicrhinitis.
Specific IgEassays wereperformed on theblood of all patientstoaeroallergens,carriedoutpreoperativelyinvitro
fordetectionofallergicrhinitis;thetestedallergens,which are common in the local environment, are grasses, dust mites,pollen,fungi,anddogandcatepithelium.
Allpatientswereoperatedonbythesamesurgeon,under localanesthesiaandsedation.
The following inclusion criteria were used: patients withchronicnasalobstruction,withoutimprovementafter standardmedications(systemicandtopicalcorticosteroids and systemic antihistamines) for at least two months; aged between 14 and 70 years; willing to participate in thestudy andtoanswer theprotocol questions;available to return for reassessment seven, 30, and 90 days after surgery;patientswithirreversiblehypertrophyofthe infe-riorturbinate;patientsdividedintogroupswithandwithout allergicrhinitis,basedonthesymptomsofitching,sneezing andrhinorrhea,inadditiontonasalobstruction.
Patients with any significant anatomical alterations (apartfrominferiorturbinatehypertrophy)thatgenerated nasalobstruction(septaldeviation,middleconchabullosa, nasalvalvealterations,nasaltumorsofanynasal-sinus ori-gin,retro-nasalorparanasalmasses,choanalimperforation, septal perforation, unciform process abnormalities, nasal polyps,adenoidhypertrophy);thosewhoshowed improve-mentafterclinicaltreatment;pregnantwomen;thosewho couldnotundergotheturbinoplastyduetoclinicalstatus; andthosenotwillingtoparticipateandanswertheprotocol questionswereexcluded.
Patients were evaluatedpreoperatively regarding gen-der; age; intensity of nasal obstruction (mild, moderate, severe); presence or absence of snoring; presence or absenceof facialpressure; presence or absence of smell alterations;presenceor absenceofsneezing,itching,and rhinorrhea.Timeofoperationwasassessedtransoperatively afterturbinateinfiltrationandplacingofcottonoidpatties withvasoconstrictorsolutionuntiltheendoftheprocedure (0---5min,5---10min,10---15min,15---20min,over20min)and intraoperativebleeding(+/IV;++/IV;+++/IV;++++/IV).
Figure1 Incisionlineontheinferiorturbinate (endoscopic view).
grade was assessed, as well as olfaction improvement grade (no improvement, moderate improvement, total improvement); facial pressure improvement grade (no improvement,moderateimprovement,totalimprovement); snoring improvement grade (no improvement, moderate improvement, total improvement) and sneezing, itching, andrhinorrheaimprovementgrade(noimprovement, mod-erateimprovement,andtotalimprovement).
The turbinoplasty surgery technique consisted of the following: incision in the center of the inferior turbinate in its horizontal extension (Fig. 1); detachment of the entiremucosaabovetheincision,creatingamucosalflap; next, the turbinate was incised in the anterior---posterior directionusing turbinectomyscissors andthen oneof the scissorsbladeswasdirectedtothemucosadetachedfrom the bone in the upper part of the turbinate, while the otherwasdirectedtotheinferiormeatus(Fig.2),thereby removingmostof theboneandall itslateralmucosa;the medial mucosa was removed only below the incision, as the mucosa above was used to cover the bony remnant, therebyremoving50%ofthemedialmucosa(septalsurface), 100% of the lateral mucosa (meatal surface), and 70% of
Figure2 Directionoftheturbinectomyscissorsblades.
Figure3 Removalofresectedturbinate.
thebonyturbinate(Fig.3).Subsequently,thebonespicules were removed with achisel toreduce thebulging of the remainingturbinate (Fig.4),and thenelectrocauterywas usedtocauterizeoccasionalbleedingspots,particularlyin theturbinatetail.
Afterthat,thepatientsweretransferredtotherecovery roomanddischargedinapproximately4hafterthesurgery, withoutnasalpacking.Theywereinstructedtoavoidefforts orblowingthenoseonthefirstpostoperativedaysandwere warned that a small amount of bleeding is common. On theseconddayaftersurgery,theystartedtoperformnasal irrigation with 0.9% saline solution toremove the crusts. Salinesolutionnasalspraycouldalsobeusedforthis pur-pose.Nasalwashingisanimportantoperationstepforrapid improvementofnasalobstructionandcleaning.
Statistical analysis of pre-, trans- and postoperative parameters was carried out, comparing the differences
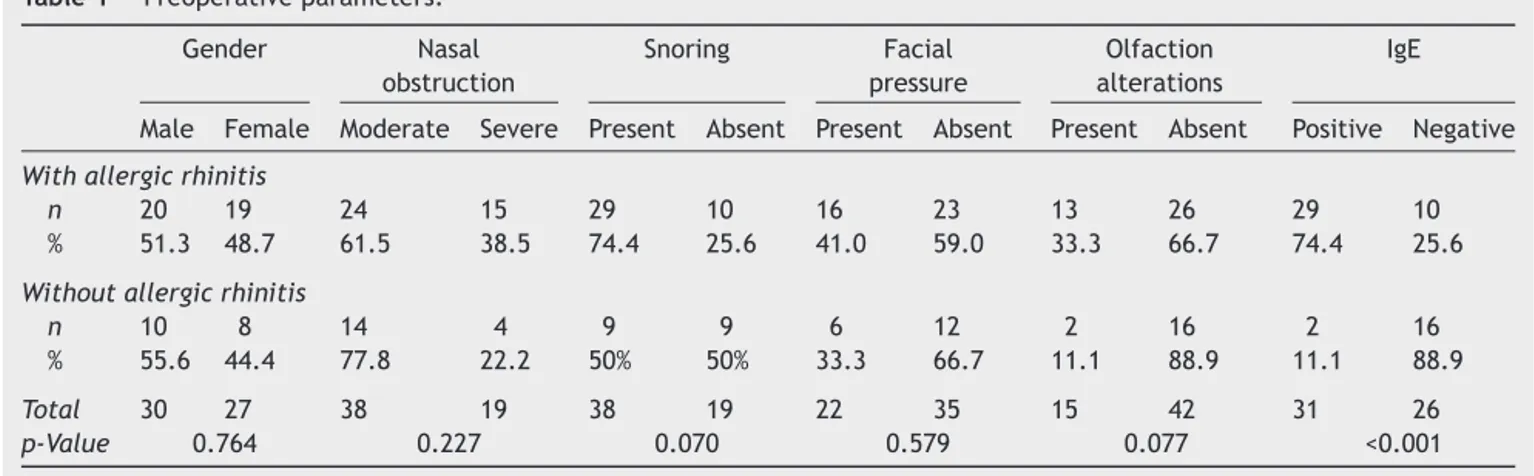
Table1 Preoperativeparameters.
Gender Nasal
obstruction
Snoring Facial
pressure
Olfaction alterations
IgE
Male Female Moderate Severe Present Absent Present Absent Present Absent Positive Negative
Withallergicrhinitis
n 20 19 24 15 29 10 16 23 13 26 29 10
% 51.3 48.7 61.5 38.5 74.4 25.6 41.0 59.0 33.3 66.7 74.4 25.6
Withoutallergicrhinitis
n 10 8 14 4 9 9 6 12 2 16 2 16
% 55.6 44.4 77.8 22.2 50% 50% 33.3 66.7 11.1 88.9 11.1 88.9
Total 30 27 38 19 38 19 22 35 15 42 31 26
p-Value 0.764 0.227 0.070 0.579 0.077 <0.001
between groupsI andII. The significancelevel wassetat
p<0.05,usingthechi-squaredandFisher’sexacttests.
Results
Atotalof57patientswereincludedinthisstudy,ofwhom39 werediagnosedwithallergicrhinitis(groupI)and18 with-out(groupII).PreoperativedataareshowninTable1.The sampleincluded30maleindividuals,20ingroupIandten ingroupII;and27females,with19ingroupIandeightin groupII.
Agerangedfrom14to70years,andtherewereno sta-tisticallysignificantdifferencesbetweenpatientswithand withoutallergicrhinitis(p=0.642).
Nasalobstructionintensitywasevaluatedinbothgroups. Most of the patients had moderate to severe complaints in the groups, withno statistically significant differences betweenthem.
Asforthepresenceofpreoperativesnoring,itwasfound thatmostofgroupIpatientssnored(29[74.4%]),whereas ninepatientsingroupII (50%)snored,withnostatistically significantdifferences(p=0.07).
Regarding the presence of facialpressure, 22 patients had the symptom, 16 in group I (41%) and six in group II (33.3%).Thesenumbersdidnotshowstatisticallysignificant differences.
Thepresenceofsmellalterationswasalsoassessed.Most patients with anosmia/hyposmia (13) were from group I. OnlytwopatientsingroupIIhadthisalteration.However, theseresultsshowednostatisticallysignificantdifferences. Operating time was assessed in both groups during surgery(Fig.5).There werestatisticallysignificant differ-encesbetweenthegroups,asgroupIhadalongeroperation time,onaverage(p=0.001).
Bleeding was also evaluated intraoperatively, which tendedtobehigheringroupI(mostdegrees+and+++/IV) thaningroupII(mostdegrees+and++/IV)withstatistically significantdifferences(p<0.001),asshowninFig.6.
Allpatientswereassessedpostoperativelyondaysseven, 30,and90.
On the seventh day after the surgery, patients were assessed in relation to breathing. There were no statis-tically significant differences between groups (p=0.079).
25
20
15
10
5
0
0 to 5 minutes 5 to 10 minutes More than 10 minutes
Allergic rhinitis + (group I) Allergic rhinitis - (group II)
Figure5 Operativetime.
30
25
20
15
10
5
0
(+/IV) (++/IV) (+++/IV) (++++/IV)
Allergic rhinitis + (group I) Allergic rhinitis - (group II)
Allergic rhinitis + (group I) Allergic rhinitis - (group II)
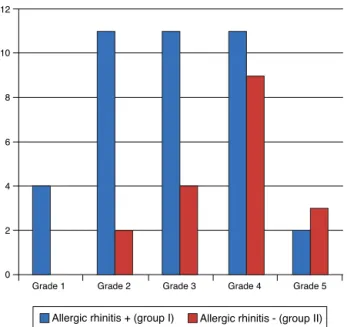
12
10
8
6
4
2
0
Grade 1 Grade 2 Grade 3 Grade 4 Grade 5
Figure7 Degree ofbreathing improvement--- seventh day postoperatively.
TheprevalencewashigheratgradesII,III,andIV(Fig.7). Improvementwasnotexpectedinallpatientsatthisphase, duetoswellingandpresenceofcrusts, butmanypatients alreadymentionedimprovement.
Onthe30thdayaftersurgery,thedegreeofimprovement inbreathingwasevaluatedagainandtherewerestillno sta-tisticallysignificantdifferencesbetweengroups(p=0.271), asshowninFig.8.Mostpatientsreportedimprovementsat gradesIVandV.
Onthe90thday,thedegreeofimprovementinbreathing wasreassessed(Fig.9).This evaluation showed consider-ableimprovementofresults,asusuallytherearenomore crustsandedema.18 Therewerenostatisticallysignificant
differencesbetweenthegroups(p=0.808).
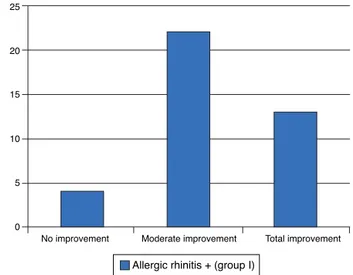
Regardingtheimprovementinthesmellalteration symp-tom,allpatientsshowedimprovementaftertheoperation.
Allergic rhinitis + (group I) Allergic rhinitis - (group II)
18
16
14
12
10
8
6
4
2
0
Grade 1 Grade 2 Grade 3 Grade 4 Grade 5
Figure8 Degreeofbreathingimprovement---30thday post-operatively.
25
20
15
10
5
0
Allergic rhinitis + (group I) Allergic rhinitis - (group II)
Grade 1 Grade 2 Grade 3 Grade 4 Grade 5
Figure9 Degreeofbreathingimprovement---90thday post-operatively.
Only two patients in group I showed mild improve-ment,whereasallothersachievedcomplete improvement (Fig.10).Therewerenostatisticallysignificantdifferences (p=1.000---Fisher’sexacttest).
Regarding the facial pressure variable, most patients achieved complete improvement with surgery. Only one patient did not achieve any improvement, as shown in
Fig.11. Therewere nostatisticallysignificant differences (p=1.000---Fisher’sexacttest).
Regarding the snoring, of the 38 patients who snored, mostshowedmoderateorcompleteimprovement,asshown inFig.12.Therewerenostatisticallysignificantdifferences betweengroups(p=0.588).
Finally,onthe90thdaypostoperatively,improvementin symptomsofsneezing,itching,andrhinorrheawasassessed
Allergic rhinitis + (group I) Allergic rhinitis - (group II)
14
12
10
8
6
4
2
0
No improvement Moderate improvement Total improvement
Allergic rhinitis + (group I) Allergic rhinitis - (group II)
16
14
12
10
8
6
4
2
0
No improvement Moderate improvement Total improvement
Figure11 Degreeoffacialpressureimprovement.
ingroup I.Ofthe39patients, onlyfourdidnotshow any improvement,asshowninFig.13.
Discussion
Theincidenceofrhinitisinadultsfromtheallergygroupof theDepartmentofOtorhinolaryngologyofHospitalde Clíni-casofFaculdadedeMedicinaofUniversidadedeSãoPaulo was56% for allergic rhinitis and 44% of nonallergic rhini-tis.Thisstudyonlyenrolledpatientswithnasalobstruction. Thus,theincidenceofrhinitisinpatientswithnasal obstruc-tionwas muchhigher.Of the 57patients, 39 (68.4%) had allergicrhinitisand18(31.58%)didnot.
Patientswithobstructivesymptomswhodidnotachieve anyimprovementwithclinicaltherapymaybenefitfrom sur-gicaltreatment.9,19---21Eventoday,clinicalexperienceshows
thatthesuccessofthenasalfunctionaloperationdepends,
20
18
16
14
12
10
8
6
4
2
0
Allergic rhinitis + (group I) Allergic rhinitis - (group II)
No improvement Moderate improvement Total improvement
Figure12 Degreeofsnoringimprovement.
Allergic rhinitis + (group I)
No improvement Moderate improvement Total improvement 25
20
15
10
5
0
Figure13 Degreeofimprovementinsneezing,pruritus,and rhinorrhea.
in many cases, onhow thesurgeon approaches the nasal turbinates.21,22 Thereareseveraltechniquestoreducethe
turbinates,andaccordingtoMabryetal.,thesurgeonmust knowalltheavailabletechniquesandusethemineachcase, asrequired.22
According to the authors’ literature review, the most widely used current procedures are lateral fracture, electrocautery, partial turbinectomy turbinoplasty, and resectionwithmicrodebrider.Patientssubmitted tolower turbinoplasty in the present study had inferior turbinate hypertrophy as the only finding. None of the cases had concomitant septal deviation or another finding, which made it possible for this study to assess the impact of surgeryexclusively onthe inferiorturbinate. None of the postoperativeparametersassessedbetweengroupsIandII showedstatisticallysignificantdifferences,butall parame-tersshowedimprovementinbothgroups.
Ophiretal.assessed186 patientsat 10---15yearsafter theyhadbeen submittedtoinferiorturbinatesurgeryand observed that 88% of patients showed nasal obstruction improvement.23 Thepresentstudyshowedsimilarfindings.
Onthe90thpostoperativeday,21ofthe57patients(36.8%) reportedgradeIVimprovementinbreathing,and33(57.9%), grade V. Together, 56 (94.7%) of the patients had good improvementinbreathing,eithergradesIVorV.Other rhini-tissymptoms than nasal obstruction also show the effect of thenasal surgery. The benefits of surgeryon the infe-rior turbinate are not limited to improvement in nasal obstructionandencompassotherrhinitissymptoms,mainly inrelation tosneezing.16 The present studydemonstrated
fromlowerturbinoplastyarenotlimitedtonasal obstruc-tion,and patients also can expect improvement in other rhinitissymptoms.
This study also showed an improvement in snoring. Of the38patientswhosnored,24(63.16%)reportedcomplete improvementthreemonthsafter surgery.It isnoteworthy thatofthe39patientsingroupI,29(74.4%)snored.Allergic rhinitisiscloselyrelatedtosleepdisorders,andphysicians shouldbeawareofthisfact,asitrepresentsanunexplored area.24 In 2008, Montovani et al. found that sleep
disor-ders were very common in patients with allergic rhinitis (over90%),25whichisinaccordancewiththefindingsofthe
presentstudy.
Facialpressurealsoshowed significant improvementin thisstudy,asofthe22patientswhoreportedthissymptom, 21(95.5%) showed totalimprovement, andonly one indi-vidual(4.55%)fromthegroupwithallergicrhinitisshowed none. There were no statistical differences between the groups;however,mostofthemshowedimprovement.There arenostudiesonthisparameter.
Noneofthepreoperativesymptomsshowedstatistically significant differencesbetween patientswithand without allergicrhinitis.
Theonlyfindingwithstatisticallysignificantdifferences in the preoperative period was the measurement of IgE
invitro,inwhich29patients(74.4%)hadapositiveresult inthegroupwithallergicrhinitisandten(25.6%)didnot.In thegroupwithoutrhinitis,thetestwaspositiveintwocases (11.1%).IgEmeasurementdeterminesthatthepatienthas anallergy,butnotnecessarilyallergicrhinitis.
Therearenostudies comparingthe degree ofanosmia improvementwiththeturbinateoperation,butafew stud-ieshavereportedthattheprevalenceofanosmiainallergic patientsishigh.In2008,Haroetal.emphasizedthatsmell alterationsarecommoninpatientswithallergicrhinitis.26
Olfaction should be investigated in patients withallergic rhinitisthroughclinical trials, dueto thehigh prevalence of alterations.27 Higoetal. investigatedsmell alterations
inpatientswithallergicrhinitisandspeculated that rhini-tiscauses alterationsintheolfactory mucosa,resultingin olfactorytransductionimpairment.28 In thepresent study,
smellalterationsingroupIwerefoundin33.3%ofindividuals (13patients),andingroupII,11.1% (twopatients).Three monthspostoperatively,onlytwopatientsdidnotachieve overallsymptomimprovement,withnodifferencebetween thetwogroups.
The assessed transoperative parameters were time of operationandtransoperative bleeding. Theauthors found nostudiesintheliteraturethatevaluatedtheseparameters intheinferiorturbinatesurgerybetweenpatientswithand withoutallergicrhinitis.Theseparametersshowed statisti-caldifferencesinthepresentstudy.PatientsingroupIhad alongerdurationofsurgery(p=0.001)andhigher transop-erativebleeding(p<0.001).Onefactorcouldhavebeenthe resultoftheother,consideringthatwhenbleedingishigher, theoperatingtimewillbelonger.Thismaybeimportantfor theschedulingofthesesurgicalpatients.
Regardingimprovementinbreathing,atsevendays post-operatively,40patients(70.18%)werealreadyinthegroup withimproved gradeIII,IV,andV.At30days,47patients (82.5%) reported grades IV and V of improvement, and afterthree months,this numberincreased to54 patients
(94.73%). This is consistentwiththe evolution inthe first weekspostoperatively,whenedemaandcrustsmayobstruct breathing.
Conclusion
This study demonstrated the efficacy of inferior turbino-plasty three months after the surgery regarding non-obstructivesymptomsofsnoring,anosmia,facialpressure, itching,sneezing,andrhinorrhea,inadditiontoobstructive symptomsinpatientswithandwithoutallergicrhinitis.
Funding
This study was supported by Coordenac¸ão de Aperfeic¸oamentodePessoaldeNívelSuperior(CAPES).
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.PassaliD,PassaliFM,DamianiV,PassaliGC,BellussiL. Treat-mentof inferior turbinatehypertrofy: a randomizedclinical trial.AnnOtolRhinolLaryngol.2003;112:683---8.
2.LaiVWS,CoreyJP.Theobjectiveassessmentofnasalpatency. EarNoseThroatJ.1993;72:395---400.
3.Jackson LE, Koch RJ. Controversies in the management of inferiorturbinatehypertrophy:acomprehensivereview.Plast ReconstrSurg.1999;103:300---12.
4.MelloJuniorJFD,MionO.Rinitealérgica.In:CamposCh,Olival Ho,editors.Tratadodeotorrinolaringologia,vol.III,2nded.São Paulo:Roca;2011.
5.SoléD,MelloJúniorJF,WeckxLLM,RosárioFilhoNA.IIIConsenso sobrerinites.BrazJOtorhinolaryngol.2012;75.
6.Mabry RL. Surgery of the inferior turbinate: how much and when.OtolaryngolHeadNeckSurg.1984;92:571---6.
7.Schmeizer B, Katz S, Vidts G. Long-term efficacy of our surgical approach to turbinate hypertrophy. Am J Rhinol. 1999;13:199---201.
8.JonesTC.Turbinectomy.Lancet.1895;2:496.
9.SerranoE,PercodaniJ,WoisardV,BraunF,ClémentO,FloresP, etal.Efficacyofpartialinferiorturbinectomyinthetreatment ofnasalobstruction.Retrospectivestudyaproposof71patients. AnnOtolaryngolChirCerevicofac.1996;117:175---8.
10.Batra PS, Seiden AM, Smith TL. Surgical management of adult inferior turbinate hypertrophy. Laryngoscope. 2009;119:1819---27.
11.Puterman MM, Segal N, Joshua BZ. Endoscopic, assisted, modified turbinoplasty with mucosal flap. J Laryngol Otol. 2012;126:525---8.
12.El Henawi D, Ahmer MR, Madian YT. Comparison between power-assistedturbinoplastyandsubmucosalresectioninthe treatmentofinferiorturbinate hypertrophy.ORLJ Otorhino-laryngolRelatSpec.2011;73:151---5.
13.MoriS,FugiedaS,YamadaT,KimuraY,TakahashiN,SaitoH. Longtermeffectofsubmucousturbinectomyinpatientswith perennialallergicrhinitis.Laryngoscope.2002;112:865---9. 14.MucciS,SismaniA.Inferiorpartialturbinectomy,aneffective
16.BarbosaAA,CaldasN,MoraisAX,CamposAJC,CaldasS,LessaF. Avaliac¸ãodasintomatologiapréepós-operatóriadepacientes submetidosaturbinectomiainferior.RevBrasOtorrinolaringol. 2005;71.
17.MelloJuniorJFD,MionO.Rinitesnão-alérgicas.In:CamposCh, OlivalHo,editors.TratadodeOtorrinolaringologia.1sted.São Paulo:Roca;2003.
18.GrymerLF,IllumP,HilbergO.Septoplastyand compensatory inferiorturbinatehypertrophy:arandomizedstudyevaluated byacousticrhinometry.JLaryngolOtol.1993;107:413---7. 19.CastroFFM. RiniteAlérgica: modernasabordagenspara uma
clássicaquestão.3rded.SãoPaulo:Vivali;2003.
20.LippertBM, Werner JA. Treatmentof hypertrophied inferior turbinate.HNO.2000;48:267---74.
21.HolMK, Huizing EH.Treatment ofinferior turbinate pathol-ogy:areviewand criticalevaluationofdifferenttechniques. Rhinology.2000;38:157---66.
22.MabryR. Inferiorturbinoplasty:patientselection,technique, and long-term consequences. Otolaryngol Head Neck Surg. 1988;98:60---6.
23.Ophir D, Schindel D. Long term follow up of the effective-nessand safetyofinferiorturbinectomy.PlastReconstrSurg. 1992;90:980---7.
24.LégerD,Annesi-MaesanoI,CaratF,RuginaM,ChanalI,PribilC, etal.Allergicrhinitisanditsconsequencesonqualityofsleep: anunexploredarea.ArchInternMed.2006;166:1744---8. 25.MontovaniJC,GomesMA,BalbaniAPS.Sintomasdedistúrbios
dosonoempacientescomrinite.RevBrasAlergiaImunopatol. 2008;31:249---52.
26.HaroJ,BenítezP,AlobidI,GonzálezJA,PascualB,MullolJ. Alteracionesolfativasenlasrinitisalérgicasapólenesyácaros. ActaOtorrinolaringolEsp.2008;59:47---51.
27.GuilemanyJM,Garcia-Pi˜neroA,AlobidI,CardelúsS,Centellas S,Bartra J,et al.Persistentallergicrhinitishasamoderate impactinthesenseofsmell,dependingonbothnasal conges-tionandinflammation.Laryngoscope.2009;119:233---8. 28.HigoR,IchimuraK,OtaY,IshizukaT,ShimazokiY.Investigation