www.jped.com.br
ORIGINAL
ARTICLE
Psychopathology,
quality
of
life,
and
related
factors
in
children
with
celiac
disease
夽
Eylem
Sevinc
¸
a,∗,
Fatih
Hilmi
C
¸etin
b,
Banu
Demet
Cos
¸kun
caEmelMehmetTarmanChildren’sHospital,DepartmentofPediatricGastroenterology,Kayseri,Turkey
bEmelMehmetTarmanChildren’sHospital,DepartmentofChildandAdolescentPsychiatry,Kayseri,Turkey cKayseriTrainingandResearchHospital,DepartmentofGastroenterology,Kayseri,Turkey
Received28April2016;accepted28June2016 Availableonline23November2016
KEYWORDS Celiacdisease; Qualityoflife; Child;
Psychiatricdiagnosis
Abstract
Objective: Thisstudyaimedtosurveychildrenwithceliacdisease(CD)forpsychiatricdisorders,
determinethepossiblefactorsthatpredictpsychopathology,andanalyzehealth-relatedquality oflifeandpossiblefactorsthatcouldaffectthequalityoflife.
Methods: In this study, all children completed the Schedule for Affective Disorders and
Schizophrenia for SchoolAge Children---Present and LifetimeVersion ---TurkishVersion (K-SADS-PL-T),aswellasthePediatricQualityofLifeInventory(PedsQL)forthe8---12agegroup, andasentencecompletiontest.Aface-to-faceinterviewwasperformedwiththeparentsof theparticipantstoinformthemaboutthestudy.
Results: Thisstudyincluded52childrenwithceliacdiseaseintheagerangeof8---12years,and
40healthychildren.Themeanageofthestudygroupwas10.36±0.36years,and31(59%)of themwerefemales.Themeanageofthecontrolgroupwas10.35±0.46yearsand24(60%)of themwerefemales.ThemeansubscalescoresofthePediatricQualityofLifeInventorywere significantlylowerinchildrenwithceliacdiseasewhencomparedtothecontrolgroup(p<0.05). Therewasatleastonepsychiatricdisorderinthe26(50%)childrenwithceliacdisease.
Conclusions: Thisstudyhasshownoncemorethatceliacdiseaseisassociatedwithsome
psy-chiatricsigns/diagnoses,andthatitdecreasedqualityoflife.Furtherstudiesareneededto determinethefactorsthatcouldreducethepsychiatricsigns.Itisapparentthatthosestudies wouldcontributenewapproachestoimprovediagnosis,treatment,andqualityoflife. ©2016SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/ 4.0/).
夽
Pleasecitethisarticleas:Sevinc¸E,C¸etinFH,Cos¸kunBD.Psychopathology,qualityoflife,andrelatedfactorsinchildrenwithceliac disease.JPediatr(RioJ).2017;93:267---73.
∗Correspondingauthor.
E-mail:dr.eylemsevinc@gmail.com(E.Sevinc¸).
http://dx.doi.org/10.1016/j.jped.2016.06.012
PALAVRAS-CHAVE Doenc¸acelíaca; Qualidadedevida; Crianc¸a;
Diagnóstico psiquiátrico
Psicopatologia,qualidadedevidaefatoresrelacionadosemcrianc¸ascomdoenc¸a celíaca
Resumo
Objetivo: Neste estudo,foramavaliadas crianc¸as comdoenc¸acelíaca (DC) para verificara
existênciadetranstornos psiquiátricos,determinarospossíveisfatores quepredizem psico-patologiaeanalisar aqualidadedevidarelacionada àsaúdeepossíveisfatores quepodem afetá-la.
Métodos: Nesteestudo,todasascrianc¸asresponderamàEntrevistaparaTranstornosAfetivos
eEsquizofreniaemCrianc¸asemIdadeEscolar---VersãoPresenteeaoLongodaVida---Versão Turca(K-SADS-PL-T),bemcomoaoInventárioPediátricodeQualidadedeVida(PedsQL)dafaixa etáriade8-12anoseaotestedecompletarsentenc¸as.Umaentrevistapresencialfoirealizada comospaisdosparticipantesparainformá-lossobreoestudo.
Resultados: Esteestudoincluiu52crianc¸ascomDCentreasidadesde8a12anose40crianc¸as
saudáveis.Aidademédiadogrupodeestudoerade10,36±0,36anos,e31deles(59%)eramdo sexofeminino.Aidademédiadogrupodecontroleerade10,35±0,46anos,e24deles(60%) eramdosexofeminino.OsescoresmédiosdassubescalasdoPedsQLforamsignificativamente menoresem crianc¸ascomDCquandocomparadoscomogrupodecontrole(p<0,05).Havia pelomenosumtranstornopsiquiátricoem26(50%)crianc¸ascomDC.
Conclusões: Este estudo mostrou mais uma vez que a DC está associada a alguns
sin-tomas/diagnósticos psiquiátricos e reduziu a qualidade de vida. São necessários estudos adicionaisparadeterminarosfatoresquepodemreduzirossintomaspsiquiátricos.Estáclaro queessesestudoscontribuiriamcomnovasabordagensparamelhorarodiagnóstico,o trata-mentoeaqualidadedevida.
©2016SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Este ´eumartigo OpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4. 0/).
Introduction
Celiac disease (CD) is a chronic, inflammatory, immune-mediated disease characterized by persistent intolerance ofthesmallintestinestogliadin.1Itsprevalenceis
approxi-mately1%inmostcountriesoftheworld.Themanifestations of CD can be divided into gastrointestinal symptoms and extraintestinalsymptoms.Thediagnosisdependson gluten-dependent symptoms, CD-specific antibody levels, the presence of human leukocyte antigen (HLA-DQ2) and/or HLA-DQ8,andcharacteristichistologicalchangesinthe duo-denalbiopsy. In thepresence of highantibody levels,the diagnosisofCDmaybebasedonacombinationofsymptoms, antibodies, and HLA, thus omitting the duodenal biopsy. Compliancewitha gluten-freediet(GFD) is monitoredby endomysiumantibody(EMA)status.2Thetreatmentconsists
ofremovingglutenfromthedietthroughoutlife.3Justlike
other chronic diseases, CD affects physical, mental, and sociallife, aswell asthe health-relatedquality oflife of children.4
Anumberofstudieshave investigatedtheeffectofCD onqualityoflifeandpsychopathology.Althoughthe preva-lenceofmajordepressivedisorder,dysthymicdisorders,and adjustmentdisordersvariesbetween10and80%,theyare themost commonpsychiatricdisorders(PD)inadultsand childrenwithCD.5Thebasicfactorfocusedoninthose
stud-ieswasthequalityanddegreeofadherencetotheGFD.Itis knownthatlifelongGFDincreasesperceptionofwell-being andpositivefeelingsinsomedomains,anddecreasesthose perceptionsinsomeotherdomains.6Inconclusion,children
withCD trying toadapt GFD are at risk for psychological disorders.
Mostofthestudiesintheliteraturethatinvestigated psy-chopathologyandqualityoflifewereconductedonadults, and the data on children are scarce.7 The present study
aimedtoscreenchildrenwithCDforPD,determinepossible factors that predict psychopathology,and analyze health-relatedqualityoflifeandthepossiblefactorsthataffected thequalityoflifeinthosechildren.
Methods
Samples
This cross-sectional study was carried out with fifty-two patients who were formerly diagnosed with CD recruited fromtheDepartmentofPediatricGastroenterology, Emel-Mehmet Tarman Children Hospital in Kayseri, Turkey, betweenJanuaryandMarch2016.ThediagnosisofCDwas based on the criteria outlined by the European Society forPediatricGastroenterology,Hepatology,andNutrition.8
those on GFD for less than six months. The study sam-plewaschosenamongchildren betweentheagesof8---12 years, which represented the period that children begin schoolandleavetheOedipalstage.Thus,theyexperience and try to handle social and academic stresses. In order todetermine theeffectof compliancetoGFD, theceliac groupwassubdividedintoadietarycompliantgroupanda dietarynoncompliantgroupaccordingtoserumEMAlevels. Forty age- andsex-matched healthychildren whodid not haveanygastrointestinaldisorderorPDandadmittedtothe Emel-MehmetTarmanChildrenHospitalforvariousreasons were included as controls. All of controls had a negative serumEMAtest. Allcharacteristics includingage, gender, symptoms, weight,height, body mass index(BMI), serum EMAlevel,andfamilycharacteristics(numberofhousehold members, socioeconomic status, PD in the history) were evaluated.
Inthesecondstepofthestudy,allpatientsincludedin thestudywereexaminedbythechildpsychiatrist.All parti-cipantsweregiventheScheduleforAffectiveDisordersand SchizophreniaforSchoolAgeChildren---PresentandLifetime Version--- Turkish Version(K-SADS-PL-T),asemi-structured diagnostictool.TheywerealsogiventhePediatricQuality ofLifeInventory(PedsQL)8---12 agegroupanda sentence completiontest,andtheparentswereinterviewedtoobtain informationabout their children. In addition,the authors completedthesociodemographicdataform.Thestudywas approved by the Ethics Committee for Non-invasive Clin-ical Research of Kayseri Training and Education Hospital, underNo.2016/49. Allparticipants providedtheirwritten informedconsent,andparticipatedinthestudyvoluntarily.
Datacollectiontools
K-SADS-PL
This is a semi-structured scale developed by Kauffman etal.toscreenpsychopathologyinchildrenandadolescents between the ages of 6 and 18 years.9 In this scale,
psy-chopathologyisinvestigatedbycombiningthedataobtained from the parents and the child. The psychopathologies includedinthescaleincludemood,psychosis,anxiety, dis-ruptivebehaviordisorder,eliminationdisorders,eatingand ticdisorders,andalcohol andsubstanceabuse.Reliability andvalidityoftheK-SADS-PLinTurkishwasverifiedby Gök-leretal.10
PedsQL
This is a general quality of life tool used in 2---18 year-oldchildrenandadolescents.11Emotionalfunctioningscore
(EFS), social functioning score (SoFS), school functioning score(ScFS),totalphysicalhealthscore(TPhHS),total psy-chosocialhealthscore(TPsHS),andtotalscalescore(TSS) areusedinthescale.A5-point,Likert-typescoringscaleis usedinthescale(0=never,1=almostnever,2=sometimes, 3=often,4=almostalways).The scoresobtainedfromthe itemsarelinearlytransformedintoavaluebetween0and 100(0=100,1=75,2=50,3=25,4=0).Thequalityoflife increasesasthescoresincreasesfrom0to100.12The
relia-bilityandvalidityofthePedsQLforages8---12andforages 13---18inTurkishwasstudiedbyCakinMemiketal.,and8---12 year-oldformwasusedinthisstudy.13
Beiersentencecompletiontest
Being one of the projection techniques, this test has a wideusagearea.Ithas twoforms; FormA,which is suit-able for children, can be applied to ages 8---16. Via this testtheindividualsprojecttheirinterests,feelings, behav-iors,wishes, sadness,andthe otherimportantpersonality featuresagainstanunclearstimulant.Thus,consciousand unconsciousemotionsandideascanbeobtainedfromthe individual.Withthistest,problemsseenfrequentlyin envi-ronmentslikeschoolandthehomecanbedetected.
Sociodemographicdataform
Via this data form, prepared by the authors, the name (optional), age, sex, and the number and the identity of householdmembers wereidentified byasking the partici-pantortheirfamily.Inthisform,thesocioeconomiclevel wasdeterminedinaccordancetoincomeofthefamily.An incomethree-fold or more of minimumwage was consid-ered as a good, an income between minimum wage and three-foldofminimumwagewasconsideredasamoderate, andan incomeat thelevel of minimumwage or less was considered as low socioeconomic level. Their history was assessedregardinganyprevious diagnosisof PD,the pres-enceofPDinfamily,andanyinformationrelatedCDsuch asdateofdiagnosis,bodyweight,height,primary gastroin-testinalsymptoms,andthecompliancewiththeGFD.
Statisticalanalysis
Thedata wereanalyzed withSPSSversion 16.0(SPSSInc. Released 2007. SPSS for Windows, version 16.0. IL, USA). Descriptive statistics were presented as mean, standard deviation, and percent. Student’s t-test for independent sampleswasusedtodeterminethesignificanceofthe inter-group differences for quantitative variables with normal distributions.Qualitativevariableswerecomparedwiththe chi-squaredandFisher’sexacttests.The normalityofthe distribution of data was analyzed with the Shapiro---Wilk test.ItwasdeterminedthatthesubscalescoresofPedsQL werenotdistributednormally,andSpearman’scorrelation analysis, Mann---Whitney, chi-squared, and Kruskal---Wallis tests were used to compared the data without normal distributions. A p-value of less than 0.05 was considered significant.
Results
Table1 Sociodemographic-cliniccharacteristicsofthestudyandthecontrolgroups.
Studygroup(n=52) Controlgroup(n=40) p
Age(years)(mean±SD,amin---max) 10.36±0.36(8---12) 10.35±0.46(8---12) 0.700
Gender(Female/male,%) 31/21(59%/41%) 24/16(60%/40%) 0.650
Householdmembers(mean±SD) 4.66±1.22 4.46±0.97 0.088
Height(cm;mean±SD) 129.50±8.67 134.42±7.89 0.176
Weight(kg;mean±SD) 27.05±8.85 33.57±8.22 0.491
BMI(kg/m2;mean±SD) 16.02±1.07 16.95±1.14 0.627
Ageatfirstdiagnosis(years;mean±SD) 6.4±2.2
Durationoffollowup(years;mean±SD) 3.94±1.10
Adherencetogluten-freediet(n,%)b
Goodadherence 16(30%)
---Pooradherence 36(70%)
Socioeconomiclevel(n,%)
Low 10(19%) 8(20%) 0.79
Moderate 37(82%) 28(70%)
High 5(9%) 4(10%)
Parenteducation(maternal---paternal,n,%)
Elementaryschool 8(16%)---7(13%) 6(15%)---6(15%) 0.842c
Middleschool 35(67%)---28(53%) 25(62%)---24(60%) 0.322d
Highschool 9(17%)---17(34%) 9(23%)---10(25%)
aStandarddeviation.
b Goodadherencetodiet:thepatientswithaserumendomysiumantibody(EMA)level<20RU/mL.
c Therewerenosignificantdifferencesbetweentheceliacgroupandcontrolsformaternaleducationstatus. d Therewerenosignificantdifferencesbetweentheceliacgroupandcontrolsforpaternaleducationstatus.
witha GFD(non-strictdietor somegluten),whostill suf-feredchronic gastrointestinalsymptoms.The meanserum EMAlevelwas140RU/mL(0---760)inchildrenwithCD,and 16(30%)ofthemadheredtoGFDwell;ontheotherhand,all ofthecontrolshadanegativeserumEMAtest.PDwere iden-tifiedinsix(11%)familiesinceliacgroupandinthree(7%) familiesinthecontrolgroup,andtherewasnosignificant differencebetweentheceliacandcontrolgroups(p>0.05). The meannumber of household members(4.66±1.22 vs. 4.46±0.97,p>0.05)wasnotsignificantlydifferentbetween celiacgroupandcontrols. Asfor parents,fatherswerean averageof36.6yearsandthemothersof32.3years,andit wasalsoobserved that35(67%) ofthechildren’smothers and28(53%)oftheirfathershadgraduatedmiddleschoolin theceliacgroup.Table1showsthattherewereno signifi-cantdifferencesbetweenceliacgroupandcontrolsforage, gender,height,BMI,andfamilycharacteristics(p>0.05).
When the meansubscalescores of PEDSQL weretaken intoconsiderationinchildrenwithCD,itwasobservedthat TPhHSwas79.68,EFSwas82.50,SoFSwas97.50,ScFSwas 90,TPsHS was90, andTSS was87.50,while thosescores were100,90,90,100,90,and92.30inthecontrolgroup, respectively.ThePedsQLsubscalescores(Table2)were sig-nificantlylowerinchildrenwithCD(p<0.05).
The effects of sociodemographic variables on subscale scoresofPedsQLwereanalyzed.MeanTPhHSandEFSscores weresignificantlyloweringirls withCDcomparedtoboys withCD;however,therewerenodifferencesformeanSoFS, ScFS, TPsHS, or TSS scores. The children with CD were dividedintothreegroups accordingtotheirincomelevels (low---medium---high),andtheydidnotshowany signifi-cantdifferencesfor PedsQLsubscalescores(p>0.05).The
Table2 MeanPediatricQualityofLifeInventory(PedsQL) subscalescoresforthestudyandcontrolgroups.
Studygroup (n=52)
Controlgroup (n=40)
p
EFS 82.5(0---100)a 90(0---100)a 0.003
SoFS 97.5(50---100)a 90(70---100)a 0.024
ScFS 90(45---100)a 100(80---100)a 0.000
TPhHS 79.68(34.37---100)a 100(75---100)a 0.005
TPsHS 90(41.65---100)a 90(76.66---100)a 0.039
TSS 87.50(44.56---100)a 92.30(84.78---100)a 0.000
EFS,emotionalfunctioningscore;SoFS,socialfunctioningscore; ScFS, school functioning score; TPhHS, total physical health score;TPsHS,totalpsychosocialhealthscore;TSS,totalscale score.
a Median(min---max).
Table3 Effectsofsociodemographic-clinicalvariablesonthePediatricQualityofLifeInventory(PedsQL)subscalescoresin childrendiagnosedwithceliacdisease.
EFS SoFS ScFS TPhHS TPsHS TSS
Psychiatricdiagnosis
Present 85 100 90 75 90.8 85.4
Absent 75 95 87.50 84.30 86.81 84.7
p 0.519 0.206 0.514 0.755 0.433 0.219
Gender
Male 85 100 95 87.5 90 90.12
Female 75 95 90 75 88.3 83.69
p 0.040a 0.897 0.488 0.032a 0.167 0.107
Adherencetogluten-freedietb
Goodadherence 72.5 95 87.5 70.3 85 80.43 Pooradherence 85 100 90 84.3 90.8 85.80
p 0.414 0.464 0.425 0.052 0.433 0.219
Socioeconomiclevel
Low 87.5 100 92.5 78.12 92.49 84.85
Moderate 80 95 90 83.5 90 84.7
High 70 100 90 84.37 85 83.69
p 0.650 0.137 0.951 0.703 0.763 0.979
Durationofdiseasec
r −0.249 0.036 −0.300 −0.362 −0.240 −0.313
p 0.755 0.798 0.031a 0.008a 0.875 0.025a
EFS,emotionalfunctioningscore;SoFS,socialfunctioningscore;ScFS,schoolfunctioningscore;TPhHS,totalphysicalhealthscore; TPsHS,totalpsychosocialhealthscore;TSS,totalscalescore.
a p<0.05.
b Goodadherencetodiet:patientswithaserumendomysiumantibody(EMA)level<20RU/mL. c Spearman’scorrelationanalysis.
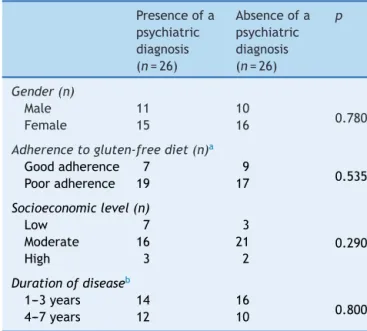
TherewerenoPDin26(50%)ofthechildrenwithCD.On theotherhand,ten(19%)haddepression,sixhad(12%) anxi-etydisorder,fivehad(9%)adjustmentdisorder,two(4%)had concomitantdepressionandanxietydisorder,andthree(6%) hadconcomitantadjustmentdisorderandanxietydisorder. The effects ofsociodemographic variablesonpresence of psychopathologywereanalyzed inTable 4.There were no significant differences for sociodemographic variables between patients with a psychiatric diagnosis and those withoutapsychiatricdiagnosis(p>0.05).
Discussion
Inthis study,theauthorsinvestigatedqualityof life, psy-chopathology,andtheprobablefactorsassociatedwithboth concepts,andfoundthatallsubscalescoresofPedsQLwe significantlylowerinthestudygroup.Inthisregard,itwas concluded that CD impaired quality of life by decreasing functionalityin social relations,emotional life,and phys-icalhealth. Itwasalsofound thatatleastonepsychiatric diagnosiswaspresentinhalfofthecases.
Interestingresultswerereportedintheliterature regard-ingqualityoflifeandpsychopathologyinchildrenwithCD. Petersetal. reportedthatexposure toglutenresulted in depressivesymptomseventhoughit didnotresultin gas-trointestinal symptoms in patients with non-celiac gluten sensitivity,whichmightexplainwhythepatientswith non-celiacgluten sensitivity feltbetter witha GFD.14 Astudy
followedupnineadolescentswithCDbetweentheagesof 12 and 16 years for six months on a monthly basis with theK-SADS-PLand achild behaviorcontrol list,and mea-suredserumaminoacidandantibodylevelsbeforeandafter GFD.The authorsdiagnosedthreeadolescentswithmajor depressivedisorder,twoadolescentswithdisruptive behav-iordisorder,andoneadolescentwithalearningdifficulty; however,theydidnotfindanyPDinfour(44%)patients.In thesamestudy,itwasreportedthatthetryptophanlevelsof theadolescentswerelowbeforeGFD,andpsychiatric symp-tomsdecreasedandserumtryptophanlevelsincreasedthree monthsafterstartingthediet.15ThoseresultsbyPynnönen
etal.indicatethatthemostimportantfactorforthehigh psychiatricdiagnosisprevalenceinthepresentstudywasthe lowadherenceratetoGFD.Wagneretal.performedastudy toinvestigatetheeffectsofadherencetoGFDonqualityof life on283 adolescentswith CD and 82 healthy controls. Theauthors didnotfindanydifferencebetweenthe ado-lescentsthatadheredtothedietandthehealthycontrols forqualityoflifeandwell-being;however,theadolescents whodidnotadherediethadworsequalityoflife;theyfelt sick,hadmore psychiatricproblems, and hadmore prob-lemsinschool.Inthesamestudy,itwasemphasizedthat adherencetothedietwasthemain factor foran optimal qualityof life, andthose withlow adherence tothe diet shouldhave psychologicalsupport.16 Thosedata showthe
Table4 Effectsofsociodemographic-clinicalvariableson thepresenceofpsychopathologyinchildrendiagnosedwith celiacdisease.
Presenceofa psychiatric diagnosis (n=26)
Absenceofa psychiatric diagnosis (n=26)
p
Gender(n)
Male 11 10
0.780
Female 15 16
Adherencetogluten-freediet(n)a
Goodadherence 7 9
0.535 Pooradherence 19 17
Socioeconomiclevel(n)
Low 7 3
0.290 Moderate 16 21
High 3 2
Durationofdiseaseb
1---3years 14 16
0.800 4---7years 12 10
aGoodadherencetodiet:patientswithaserumendomysium
antibody(EMA)level<20RU/mL.
b Spearman’scorrelationanalysis.
withGFDandthehighprevalenceofpsychiatricdiagnoses arenotableinthepresentstudy,thedegreeofthe compli-ancewithGFDwasnotdirectlycorrelatedwiththepresence or absenceof apsychiatricdiagnosis. Even when possible variants(sex,durationofdisease)wereexamined,adirect correlationcouldnotbeshown.Therefore,toevaluatethe potentialeffectoflowGFDcomplianceontheappearance ofpsychopathology,alargerstudysamplemaybeneeded.
The most frequently diagnosed disease wasdepression (23%) in this study; however, the rates of anxiety (22%) and adjustment (15%) disorders were also high when the comorbid diagnoses were taken into consideration. From anotherpointof view, lowrate ofadherence toGFDmay meanmoreexposuretogluten,andhencemorepsychiatric signs/diagnoses.Although the etiopathogenesis of psychi-atricsigns/diagnosesobservedinCDisnotclear,tryptophan deficiencyduetomalabsorptioninpatientswithpoor adher-ence to diet may cause a hyposerotonergic state in the centralnervoussystem.17---20Anotherimportantfactoris
psy-chosocialstressrelatedtoCDandGFD.21---23 Notbeingable
todineout,difficultytofindgluten-freefoods,and incon-venience in school and social life result in isolation and stigmatization.Thosemaycauselowself-esteem,and con-stituterisk factorsfor psychopathology.24,25 In accordance
withtheliteratureandinconjunctionwiththehigh preva-lence of psychopathology seen in the present study, the statementsthatindicatedlowself-esteeminsentence com-pletion test were as follows: ‘‘unfortunately I am a sick person,’’‘‘IwishIwasnotsick,’’‘‘Idon’tunderstandwhy Iamsick,’’and‘‘IneverforgetthatIamsick.’’
An interesting point in this study is that emotional functionality and physical health were affected more in girls. Supporting those data, all patients diagnosed with depression were girls in the study that investigated nine
adolescentswithCD.15Variousstudieshavereportedhigher
anxiety levelsin women diagnosedwithCD26---28 and some
others indicated that emotional well-being significantly improvedwithGFDinwomen.22Studiesconductedonadults
showed that duration of disease was another factor that couldaffectthequalityoflife.Barrattetal.didnotshow a correlation between duration of disease and quality of life.29 On theother hand,Roosetal.didnotfindany
dif-ferencebetweenpatientswithCDwhohadbeentreatedfor tenyearsandthecontrolgroup.30Contradictoryresultsmay
beexplainedbythedifferencesinadherencetoGFD. Itis clearthatpatientswithlowadherencetoGFDwillbecome worse,bothregardingphysicalandpsychologicalwell-being. Inthepresentstudy,therateofadherencetodietwaslow, andphysicalhealth,schoollife,andemotionalfunctionality scoresdecreasedasthedurationofthediseaseincreased.
This study has some limitations. First, it was cross-sectional, and there was no prospective follow-up. Therefore, there are no data concerning how the ther-apeutic interventions of the child psychiatrist affected adherence todiet, quality of life, and frequency of psy-chopathology.Inaddition,thesmallnumberofthepatients includedpreventsgeneralizationoftheresults.Norelation wasfoundbetweenhighdiagnosisprevalenceandthe inves-tigatedvariants,andthismaybeduetothesmallsizeofthe studysample.
Inconclusion,thisstudyshowedimpairedqualityoflife andincreasedrateofpsychopathologyinchildrenwithCD. When the possible factors that cause these results were investigated,itwasfoundthattheseoutcomesarerelated withbeingfemaleandthedecreaseinsomepartsofquality oflifeduetothedurationofthedisease.Ontheotherhand, accordingtothesefindings,bothimpairedqualityoflifeand increased psychopathologies werenot related with worse compliancewitha GFD. Fromthispoint, further prospec-tivestudieswithlargersamplesizeareneededtodetermine the factors that affect quality of life and high frequency ofpsychopathologyinpatientswithCD.Thepresent study indicatesthatchildren andadolescentsdiagnosedwithCD shouldbefollowedupbyachildpsychiatristforasuccessful adherencetodiet,andhenceanoptimalqualityoflifeand mentalhealth.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Rubio-Tapia A, Hill ID, Kelly CP,Calderwood AH, Murray JA. AmericanCollegeofGastroenterology.ACGclinicalguidelines: diagnosisandmanagementofceliacdisease.AmJ Gastroen-terol.2013;108:656---76.
2.HusbyS,KoletzkoS,Korponay-SzabóIR,MearinML,PhillipsA, ShamirR,etal.EuropeanSocietyforPediatric Gastroenterol-ogy,Hepatology,andNutritionguidelinesforthediagnosisof coeliacdisease.JPediatrGastroenterolNutr.2012;54:136---60.
4.CastilhosAC,Gonc¸alvesBC,SilvaMM,LanzoniLA,MetzgerLR, KotzeLM,etal.Qualityoflifeevaluationinceliacpatientsfrom SouthernBrazil.ArqGastroenterol.2015;52:171---5.
5.van Hees NJ, Van der Does W, Giltay EJ. Coeliac disease, diet adherence and depressive symptoms. JPsychosom Res. 2013;74:155---60.
6.ZingoneF,Swift GL,CardTR, SandersDS, LudvigssonJF,Bai JC.Psychologicalmorbidityofceliacdisease:areviewofthe literature.UnitedEurGastroenterolJ.2015;3:136---45.
7.FidanT, Ertekin V,Karaba˘g K. Depression-anxiety levelsand thequalityoflifeamongchildrenandadolescentswithcoeliac disease.Düs¸ünenAdam.2013;26:232---8.
8.HillID,DirksMH,LiptakGS,CollettiRB,FasanoA,GuandaliniS, etal.Guidelineforthediagnosisandtreatmentofceliacdisease inchildren:recommendationsoftheNorthAmericanSocietyfor PediatricGastroenterology,HepatologyandNutrition.JPediatr GastroenterolNutr.2005;40:1---19.
9.KaufmanJ,BirmaherB,BrentD,RaoU,FlynnC,MoreciP,etal. ScheduleforAffectiveDisordersandSchizophreniafor School-AgeChildren-PresentandLifetimeVersion(K-SADS-PL):initial reliabilityandvaliditydata.JAmAcadChildAdolescPsychiatry. 1997;36:980---8.
10.Gökler B, Ünal F, Pehlivantürk B, C¸engel Kültür E, Devrim AkdemirD,TanerY.Reliabilityandvalidityofschedulefor affec-tivedisordersandschizophreniaforschoolagechildren-present andlifetimeversion-Turkishversion(K-SADS-PL-T).TurkJChild AdolescMentHealth.2004;11:109---16.
11.Varni JW, Seid M, Rode CA. The PedsQL: measurement modelfor thepediatric quality of life inventory. Med Care. 1999;37:126---39.
12.VarniJW,SeidM,KurtinPS.PedsQL4.0:reliabilityandvalidity ofthePediatricQuality ofLifeInventory version4.0generic core scales in healthy and patient populations. Med Care. 2001;39:800---12.
13.CakinMemikN,A˘gao˘gluB,Cos¸kunA,UneriOS,KarakayaI.The validityandreliabilityoftheTurkishPediatricQuality ofLife Inventory for children13---18 years old.Turk Psikiyatri Derg. 2007;18:353---63.
14.PetersSL,BiesiekierskiJR,YellandGW,MuirJG,GibsonPR. Ran-domisedclinicaltrial:glutenmaycausedepressioninsubjects withnon-coeliac gluten sensitivity --- an exploratory clinical study.AlimentPharmacolTher.2014;39:1104---12.
15.PynnönenPA,IsometsäET,VerkasaloMA,KähkönenSA,Sipilä I,SavilahtiE,etal.Gluten-freedietmayalleviatedepressive and behavioural symptoms in adolescents with coeliac dis-ease:aprospectivefollow-upcase-seriesstudy.BMCPsychiatry. 2005;5:14.
16.WagnerG, BergerG, SinnreichU, GrylliV,SchoberE,Huber WD,etal.Quality oflifeinadolescentswithtreatedcoeliac
disease:influenceofcomplianceandageatdiagnosis.JPediatr GastroenterolNutr.2008;47:555---61.
17.CartaMG,HardoyMC,BoiMF,MariottiS,CarpinielloB,UsaiP. Associationbetweenpanicdisorder,majordepressivedisorder andceliacdisease:apossibleroleofthyroidautoimmunity.J PsychosomRes.2002;53:789---93.
18.HernanzA,PolancoI.Plasmaprecursoraminoacidsofcentral nervoussystemmonoaminesinchildrenwithcoeliacdisease. Gut.1991;32:1478---81.
19.PotockiP,HozyaszK.Psychiatricsymptomsandcoeliacdisease. PsychiatrPol.2002;36:567---78.
20.HallertC,SvenssonM,TholstrupJ,HultbergB.Clinicaltrial:B vitaminsimprove health inpatientswithcoeliac disease liv-ing ona gluten-free diet.Aliment PharmacolTher. 2009;29: 811---6.
21.LeeAR,NgDL,DiamondB,CiaccioEJ,GreenPH.Livingwith coeliacdisease:surveyresultsfromtheU.S.A.JHumNutrDiet. 2012;25:233---8.
22.ZarkadasM,DuboisS,MacIsaacK,CantinI,RashidM,Roberts KC,etal.Livingwithcoeliacdiseaseandagluten-freediet:a Canadianperspective.JHumNutrDiet.2013;26:10---23.
23.Sainsbury K, Mullan B, Sharpe L. Reduced quality of life in coeliac disease is more strongly associated with depression than gastrointestinal symptoms. J Psychosom Res. 2013;75: 135---41.
24.ByströmIM,HollénE,Fälth-MagnussonK,JohanssonA. Health-relatedqualityoflifeinchildrenandadolescentswithceliac disease: fromtheperspectivesofchildrenand parents. Gas-troenterolResPract.2012;2012:986475.
25.ZarkadasM,CranneyA,CaseS,MolloyM,SwitzerC,Graham ID, et al. The impact of a gluten-free diet on adults with coeliacdisease:resultsofanationalsurvey.JHumNutrDiet. 2006;19:41---9.
26.HäuserW,JankeKH,KlumpB,GregorM,HinzA.Anxietyand depressioninadultpatientswithceliacdiseaseonagluten-free diet.WorldJGastroenterol.2010;16:2780---7.
27.HallertC,GrännöC,HulténS,MidhagenG,StrömM,Svensson H,et al.Livingwithcoeliacdisease: controlledstudyofthe burdenofillness.ScandJGastroenterol.2002;37:39---42.
28.TaylorE,Dickson-SwiftV,AndersonK.Coeliacdisease:thepath todiagnosisandtherealityoflivingwiththedisease. JHum NutrDiet.2013;26:340---8.
29.BarrattSM,LeedsJS,SandersDS.QualityoflifeinCoeliac Dis-easeisdeterminedbyperceiveddegreeofdifficultyadheringto agluten-freediet,notthelevelofdietaryadherenceultimately achieved.JGastrointestinLiverDis.2011;20:241---5.