SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Review
Article
Prophylaxis
with
nasal
decolonization
in
patients
submitted
to
total
knee
and
hip
arthroplasty:
systematic
review
and
meta-analysis
夽
David
Sadigursky
a,∗,
Henrique
Santos
Pires
a,
Saulo
Américo
Caldas
Rios
b,
Francisco
Luiz
Borja
Rodrigues
Filho
c,
Gustavo
Castro
de
Queiroz
c,
Mateus
Lemos
Azi
aaHospitalManoelVictorino,Salvador,BA,Brazil
bHospitalGeralErnestoSimõesFilho,Salvador,BA,Brazil cFaculdadedeTecnologiaeCiências(FTC),Salvador,BA,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received11August2016 Accepted28October2016 Availableonline27October2017
Keywords: Arthroplasty Prophylaxis Infection Decontamination
a
b
s
t
r
a
c
t
Despitetheevolutionofthetotalkneeandhiparthroplastysurgery,highpostoperative com-plicationratesintheshortandlongtermstillpersist.Infectionisoneofthemostchallenging complications;duetoitsgravityandtreatmentdifficulties,prophylaxisprotocolshavebeen createdtodecreaseitsincidence.Theobjectiveofthisstudywastoevaluatetheimpact oftheprophylaxisprotocolformethicillin-resistantStaphylococcusaureusdecolonizationof thenaresinpatientspreviouslyidentifiedbyswabcultures,whoweretobesubmittedtoa totaljointarthroplasty.Asystematicreviewwithmeta-analysiswasconducted,following thePRISMA-2015protocol,usingthedescriptors:“arthroplasty”and“nasaldecolonization,” or“jointarthroplasty”and“decolonization,”or“jointarthroplasty”and“nasal decoloniza-tion,”forfinalselectionoffourobservationalstudiesfrom79referencesidentified.This studyincludedatotalsampleof10,179patients,dividedintwogroups:thecontrolgroup (4788patients)andinterventiongroup(5391patients).Itwasobservedthattheintervention group,inwhichprophylaxiswithnasaldecolonizationwasused,59(1.09%)ofthepatients developedasurgicalsiteinfection,whileinthecontrolgrouptherewere86casesof sur-gicalsiteinfection(1.79%).Thistrendrepeateditselfinallarticles,showingnopublication biases,formingahomogeneoussample.Theuseofaprophylaxisprotocolfor decoloniza-tionofmethicillin-resistantStaphylococcusaureus,reducedsurgicalsiteinfectioncasesby approximately39%.
©2017SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
夽
StudyconductedattheHospitalManoelVictorino,DepartamentodeOrtopediaeTraumatologia,Salvador,BA,Brazil. ∗ Correspondingauthor.
E-mails:davidsad@gmail.com,dadav@hotmail.com(D.Sadigursky). http://dx.doi.org/10.1016/j.rboe.2016.10.018
Profilaxia
com
descolonizac¸ão
nasal
em
pacientes
submetidos
a
artroplastia
total
de
joelho
e
quadril:
revisão
sistemática
com
metanálise
Palavras-chave: Artroplastia Profilaxia Infecc¸ão
Descontaminac¸ão
r
e
s
u
m
o
Apesardaevoluc¸ãodosresultadosapósaartroplastiatotaldejoelhoequadril,ainfecc¸ão aindaéumadascausasmaisdesafiadorasparaocirurgião.Emvirtudedagravidadee dificuldadedotratamentodainfecc¸ãoarticularperiprotética,foramcriadosprotocolosde profilaxiaparaessetipodecomplicac¸ão.Oobjetivodesteestudofoiavaliaraprofilaxia infec-ciosacomadescolonizac¸ãonasalpréviacontraStaphylococcusaureusresistenteàmeticilina, identificadospormeiodacoletadematerialdanasofaringeporswabsempacientescom programac¸ãocirúrgicadeartroplastiatotaldejoelhoeartroplastiatotaldequadril.Foi elab-oradoumestudoderevisãosistemáticacommetanálisequeusouoprotocoloPRISMA-2015, noqualforamutilizadososdescritores:arthroplastyenasaldecolonizationoujointarthroplasty edecolonizationoujointarthroplastyenasaldecolonizationnalínguainglesa.Foram seleciona-dosquatroestudosobservacionaisdentreas79referênciasidentificadas.Aamostratotal foide10.179pacientes,divididosemdoisgrupos:controle(4.788pacientes)eintervenc¸ão (5.391pacientes).Foiobservadoque,nogrupodeintervenc¸ão,noquala profilaxiacom descolonizac¸ãonasalfoiaplicada,59(1,09%)dospacientesdesenvolveraminfecc¸ãodositio cirúrgico,enquantoainfecc¸ãodositiocirúrgicofoiobservadaem86(1,79%)dospacientes nogrupocontrole.Essatendênciaserepetiuemtodososartigosestudados, nãosendo observadorviésdepublicac¸ão,constituindoemumaamostrahomogênea.Aprofilaxia pré-operatóriacomdescolonizac¸ãonasalparaStaphylococcusaureusresistenteàmeticilina,reduz em39%oscasosdeinfecc¸ãopós-artroplastiasdojoelho,devendoserconsideradacomoum protocolocomplementarpeloscirurgiões.
©2017SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Totalknee(TKA)andhip(THA)arthroplastiesaresurgical
pro-ceduresthataimtoimprovequalityoflife,promotingpain
relief, functional gain,and correctionofdeformitiesofthe affectedjoint.1,2
Eachyear600,000TKAsareperformedintheUnitedStates;
by2030,a673%increaseindemandisexpectedworldwide.
InBrazil,thenumberofTKAsisestimatedtorangebetween
60,000and70,000peryear.3,4
Despitetheevolutionofarthroplastyresults,complications inthepostoperativeperiod,bothinshort-andlong-term,still persist.Postarthroplastyinfection isoneofthemost chal-lengingcausesofcomplicationforthesurgeon.5,6Therateof
post-TKAsurgicalsiteinfections(SSI)canvarybetween0.5% and23%,andhasanimpactofroughlyU$300millioninNorth Americancountries.7 SSIisoneofthemaininfectiontypes
associatedwithhealthcare,accountingfor17%ofthose in
theUnitedStatesand37%worldwide,accordingtotheWorld
HealthOrganization(WHO).7–10
Due to the seriousness and difficulty of treatment of
periprosthetic infections (PI), the development ofeffective
measurestominimizetheseratesisnecessary;prophylactic
measuresinthepreoperativeperiodofTKAhavebeen
demon-stratedintheliterature.2,10
Parvizi et al.2 have developed a protocol that
summa-rizesthemosteffectiveand provenprophylacticmeasures.
Thesemeasures includetheassessment ofnasal
coloniza-tion by Staphylococcus aureus and its methicillin-resistant
strain (MRSA).However,thereisstillno consensusfor
rec-ommending universal screening, despite the fact that the
decolonizationofMRSAcarriersdecreasestheSSIrate.10
Amongthepostoperativehospitalinfections,S.aureushas beenreportedasthemainpathogenisolatedincultureexams.
HighlevelsofnasalcolonizationbyMRSAstrainsmaybea
riskfactorforSSIonset.11Thenasalepithelium standsout
asthesiteofgreatestcolonization;itsprevalencereaches,on
average,40%intheadultpopulation.Aspartofthehuman
microbiota,saidbacteriumdoesnotconstituteariskandcan becarriedforalongperiodwithoutdamagetothehealthof individuals.12
Collectingsamplesfromthenostrilswiththeswab
tech-nique allows the identification of MRSA by culture or by
polymerasechainreaction(PCR)test;bothpresenthigh posi-tivepredictivevalueandspecificity.13Thismethodisindicated
forMRSAscreeningfromthenasalregionofpatientswhoare candidatesforTKAandTHA.14
Topicalantibiotics,whichactonS.aureusstrains,are indi-catedasaprophylacticmethod.Topicalmupirocinisthemost
frequentlyusedantibioticandrecommendedforpreoperative
nasaldecolonization(ND),andshouldbeconsideredasoneof thepillarsofanti-infectionprophylaxis.15
Thus, prophylaxis with ND forMRSA may be indicated
asanimportantprophylacticmethodforperiprostheticjoint infection.16,17However,studiesthatanalyzedthissubjectdid
notreachaconsensusinthevalidationofprophylaxisthrough
universalMRSAassessmentinTKAandTHAcandidates.2
Thisstudy isaimedatassessingwhether infection
Table1–InclusioncriteriaaccordingtoPICOstrategy. PICOinclusioncriteria
Indicators ResultsaccordingtoPICO
Project Cohortstudies
Population Patientsinsurgicalplanningforhipand kneearthroplasty
Intervention Prophylaxis:decolonizationforS.aureus
MRSAinidentifiedpatients Comparisons Noprophylaxis
Results Infectionrates(incidence)
identifiedthroughnasopharyngealswabcollection,isa risk-reducingfactorforSSI.
Methods
Thesystematicreviewstudy withmeta-analysiswas elabo-ratedaccordingtothePRISMAstatementprotocol(2015).18
Theliteraturewassearchedtoidentifystudiesthat evalu-atedprophylaxisasarisk-reducingfactorforSSIthroughND
forMRSAincolonizedpatients,identifiedthrough
nasopha-ryngealswabcollection.
Theinclusioncriteriafortheselectionofstudiesevaluating
prophylactictreatmentafterMRSAcolonizationassessment
inthepreoperativeperiodofpatientswhowouldundergoTKA
andTHAwerecohortstudiesinPortugueseandEnglish.
Studieswithaninadequatedescriptionandthoseinwhich theclinicaloutcomewasnottheoneproposedbytheauthors wereexcluded.Casereports,caseseriesstudies,ordescriptive reviewswerenotincluded.Incompletearticlesorthosethat didnotprovidedataregardingMRSAcolonizationinpatients
submittedtoTKAandTHAwerealsoexcluded.Articleswith
ascorelowerthan7intheNewcastle-OttawaQuality Assess-mentScale(NOS),19whichdeterminesthequalityofthestudy,
andthosethatdidnotfittherequiredLevelofScientific
Evi-dence byType ofStudy (OxfordCenter for Evidence-based
Medicine)todeterminethestudy’spublicationvaluewerealso excluded.20
Theinclusioncriteria,presentedinTable1,andthe exclu-sioncriteriaweredeterminedinaccordancewiththeobjective ofthisstudy,sothatonlyarticlesthatevaluatedtheefficacy
ofsurgicalprophylaxiswithNDforMRSAwere considered.
ThesecriteriaareshowninTable1andwerestratified accord-ingtothePICOstrategy(Patient,Intervention,Comparison, Objectives),21inordertoprovideinternalvaliditytothestudy.
ThedatabasesusedfortheresearchwereMEDLINE,SciELO, ScienceDirect,PubMed,Scopus,andGoogleScholar.
Thesearchwasperformedwiththefollowingdescriptors: “arthroplasty”and “nasaldecolonization,” or “joint
arthro-plasty” and “decolonization,” or “joint arthroplasty” and
“nasaldecolonization” inEnglish;“arthroplasty”and “nasal decolonization,”or“arthroplasty”and“decolonization,”“joint arthroplasty”and“nasaldecolonization”inPortuguese.
Theresultswerepresentedthroughanorganizationchart
forthe selection ofarticles; the dispersion datawas
com-piledintofunnelchartsandforestplotstobetterunderstand
the meta-analysis. The percentage of SSI in patients who
underwentarthroplastywasexpressedasarelativerisk(RR)
in 95% confidence interval (CI). The results from different
79 references retrieved in the electronic search
68 references excluded after analysis by title,
abstract, and language
11 references selected for
evaluation
7 references excluded (data not available
or inadequate study design) 4 studies selected,
including 10,179 individuals: 4,788 (47.03%) control group, 5,391 (52.96%) intervention
group
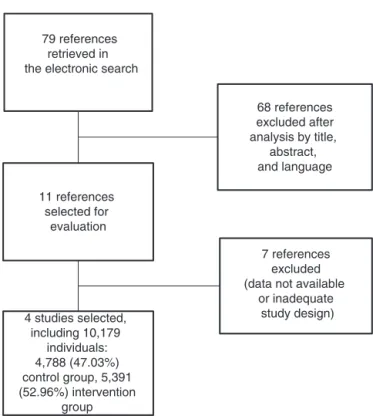
Fig.1–Organizationchartofarticleselection.PRISMA Protocol–2015.
studies were combined into a random effect model, since
notallstudiespresentedthesamemethodology.The
hetero-geneity wasanalyzedbythe chi-squared,I2, andtau2 tests
inordertoidentifydifferencesthatcouldcause biasinthe
study.Theseanalyzeswerecarriedoutwiththeappropriate
software:ReviewManager,version5.2(TheCochrane
Collab-oration,2012).
Results
Fig. 1shows the organization chartof article selection, in
which 79 references were identified aspotentially relevant
duringthesearch.Afteranalysisofthetitle,abstract,and
lan-guageofpublication,68studies didnotmeetthe inclusion
criteria.Ofthe11remainingreferences,sevenwerediscarded accordingtotheexclusioncriteria,basedonlackofdataor
inadequatestudydesign.
Aftertheselectionoffourstudies,22–25thetotalsampleof
10,179patientswasdividedintotwogroupsforstatistical anal-ysis:noprophylaxis,4788(47.03%)anduseofprophylaxis,5391 (52.96%;Fig.1).
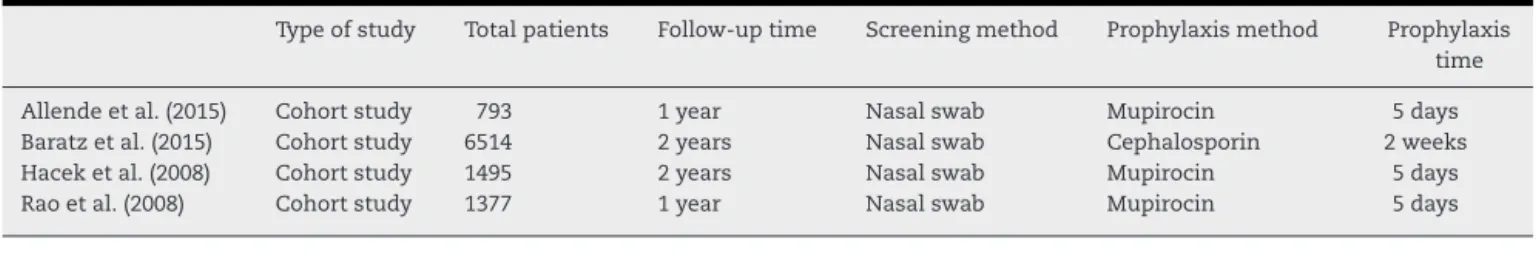
Table 2 shows the data collected that characterize the
four selected studies.22–25 All selected studies presented
cohortdesign,wereconsideredsuitableforsystematicreview
through meta-analysisbasedon theLevel ofScientific
Evi-dence by Type ofStudy(Oxford Centre forEvidence-based
Medicine),21andpresentedaminimumvalueof7intheNOS.20
Table2–Characteristicsofselectedstudies.
Typeofstudy Totalpatients Follow-uptime Screeningmethod Prophylaxismethod Prophylaxis time
Allendeetal.(2015) Cohortstudy 793 1year Nasalswab Mupirocin 5days
Baratzetal.(2015) Cohortstudy 6514 2years Nasalswab Cephalosporin 2weeks
Haceketal.(2008) Cohortstudy 1495 2years Nasalswab Mupirocin 5days
Raoetal.(2008) Cohortstudy 1377 1year Nasalswab Mupirocin 5days
RR M–H, Random, 95% CI
0,59 [0,29, 1,21] 0,73 [0,44, 1,22] 0,50 [0,23, 1,10] 0,52 [0,24, 1,14]
0,62 [0,44, 0,86]
0,2 0,5
Experimental Control
1 2 5
RR M–H, Random, 95% CI
Fig.2–ForestPlot.RR,riskratio;CI,confidenceinterval.
etal.,24whoevaluatedtheuseofcephalosporinfortwoweeks.
Patientswerefollowed-upfortheoutcomefortwoyearsin
thestudiesofBaratzetal.24andHaceketal.25;inthe
stud-iesbyBarberoAllendeetal.,23andRaoetal.,22patientswere
followed-upforoneyear.
InthegroupwhereMRSAprophylaxiswasperformed,59
(1.09%)ofthepatientsdevelopedSSI,whereaspostoperative
infectionwas observedin86 (1.79%)ofthe patients,which
reflectsareductionof39%inthecasesofthiscomplication (Table3).Thefollowingreductionswereobserved:40.7% in thestudybyBarberoAllendeetal.23;27.2%inthe studyby
Baratzetal.24;50%inthestudybyHaceketal.25;and47.6%in
thestudybyRaoetal.22
InthestudybyBaratzetal.,24inwhichthelowestinfection
rateswereobserved,theinterventiongrouppresented0.78%
casesandthecontrolgroup,1.07%(Table3).
Thefinal result ofthe weight attributedto each study,
reportedinTable3,wasbasedonthealgorithmofthe ran-domeffectmodel,whichtakesintoaccountthefactthatthere
areconsiderablemethodologicaldifferencesamongthe
stud-iesandthereforemakesadifferentiatedcalculationbasedon variance,andnotonlyonthenumberofpatients.
Table3showsthattheconfidenceintervaldidnotexceed1, whichindicatesthattheinterventiongroup,inwhich prophy-laxishadbeenperformed,presentedalowerriskofinfection. Thiswasconfirmed bythefinal statisticaltest, which pre-sentedp=0.004.
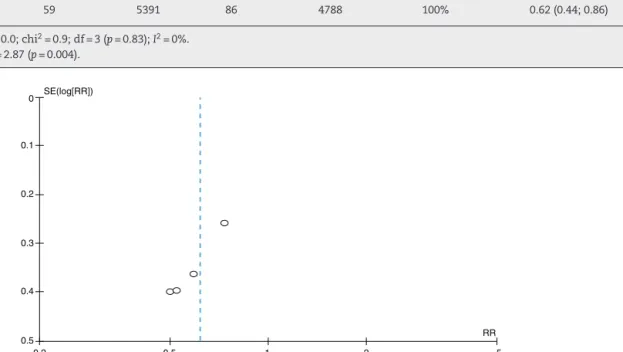
Regardingtheheterogeneitytests,whichseektoidentify
variations amongthe studies that may suggest conflicting
data, whether due to differences in design, methodology,
sampling,andbias,amongothers,thefirstparameter,tau2,
quantitatively evaluates the heterogeneity of the results
amongthestudies,anddemonstratedthattheyoverlappedin
averyorderlyway(Fig.2),converginginalowvalue.The chi-squaredtestwasthenapplied,withitsp-value,againseeking toidentifyevidenceofheterogeneity.Finally,theI2
parame-terwasusedtoexplainhowmuchofthevariabilityamong
theresultswasassociatedwithheterogeneity;thevalueof0
(zero)indicatedthatinconsistencyamongthestudiesshould notbeanimportantfactor(Table3).
Heterogeneity,representedbythefunnelplot(Fig.3),was non-significant(tau2=0.0;I2=0%)andtheoccasionalestimate
ofrelativeriskwas0.62(95%CI=0.44–0.86).Therefore,no sta-tistically significantdifferences were observedbetweenthe studies(Fig.2andTable3).
InFig.3,allstudiespresenteddatafavorableto
interven-tion, with a slight tendency toward a better result in the
smallergroups,ascanbeobservedinthecomparisonwith
thevalueobtainedinthecompilationoftheresults.
Discussion
Despite theprogressininfection controlafterTKAor THA,
especially in the short term, the treatment ofestablished
infectionsinprostheticjointsremainscomplexandcostlyin termsoftimeandresources.Therefore,carefulattentionto preventinfectionsisrequired.
In thiscontext,this meta-analysisevaluatedMRSA
pro-phylaxisasanSSIrisk-reducingfactorincolonizedpatients,
identifiedbynasopharyngealswabsinTKAandTHA
candi-datesinfourcohortstudies.
ThestudydemonstratedthatprophylaxiswithNDisa pro-tectivefactor.Thismodelaccountedfora39%reductioninthe incidenceofSSI;theratedecreasedfrom1.79%inthecontrol groupto1.09%inthegroupinwhichtheinterventionwas per-formed.Thistrendwasobservedinallfourstudies,arranged inanorderlymanner,presentingstatisticallyirrelevant differ-ences,whichsuggesttheabsenceofheterogeneity.
Theresultsobtainedarereflectedintherelativerisk(0.62) and its confidence interval (0.44–0.86), which indicate that MRSAprophylaxisisaprotectivefactor.Thisprobablyarises fromtheprevalenceofthesepathogensandtheirstrains, rec-ognizedasamajorcauseofSSIinthegeneralandin-hospital population.13,26 Infection in this group of patients may be
associatedwithcolonizationofthenostrils,whichjustifiesND withtopicalmuporicinoranantibioticdrugthatactsonthis pathogen.27,28
Theimportanceofpreoperativeprophylaxiswith
investi-gationofMRSAcolonizationisobservedinstudiessuchas
thosebyBarberoAllendeetal.,23whoperformedpreoperative
prophylaxisinTKAandTHApatientswithtopicalmupirocin,
appliedinthenostrils,andchlorhexidineskinwash. When
comparingthegroupsinwhichprophylaxiswasusedornot
used,asignificantdecreaseinSSIrateswasobserved,witha
reductionof40.7%;theincidencewas4.94%inthegroupin
Table3–Characteristicsandreviewofstudies.
Studyorsubgroup Prophylaxisused Prophylaxisnotused Weight Relativerisk
H-M,Random,95%CI
Events Total Events Total
Allendeetal.(2015) 12 409 19 384 21.7% 0.59(0.29;1.21)
Baratzetal.(2015) 27 3434 33 3080 42.6% 0.73(0.44,1.22)
Haceketal.(2008) 11 912 14 583 17.8% 0.50(0.23;1.10)
Raoetal.(2008) 9 636 20 741 18% 0.53(0.24;1.14)
Total(95%CI) 59 5391 86 4788 100% 0.62(0.44;0.86)
Heterogeneity:tau2=0.0;chi2=0.9;df=3(p=0.83);I2=0%.
Overalltesteffect:Z=2.87(p=0.004).
SE(log[RR]) 0
0.2
0.4 0.3
0.5
0.2 0.5 1 2 5
RR 0.1
Fig.3–Funnelplotofthefourindependentsamples,examiningtherelationshipbetweensurgicalsiteinfectionriskand intervention.
Baratzetal.24comparedtheincidenceofSSIinpatients
submittedto TKA and THA, consideringpatients who had
beentreatedwithNDforMRSAandmethicillin-sensitiveS.
aureus(MSSA)andthosewhodidnotreceiveprophylaxis.It
was observedthat the interventiongroup, treated prior to
surgerywithfirstgenerationcephalosporin,presentedan
inci-denceof 0.79%,a 27.3% reductionincomparison withthe
controlgroup,whichpresentedanincidenceof1.07%. Inthesamecontext,Haceketal.25demonstratedthat1.2%
ofthepatientstreatedwithNDdevelopedSSIvs.2.4%ofthose inthegroupthatwasnottreatedwithND,thatresultedina 50%reductioninSSIincidence.
Raoetal.22comparedtheresultsofpatientswhohadornot
undergoneNDwithnasalmupirocinandchlorhexidinebody
washinthepreoperativeperiod.TheSSIratewas1.41%inthe
prophylaxisgroupand2.69%inthecontrolgroup.Thisdata
suggestsanSSIreductionof47.6%.
ToevaluatethepercentageofpatientssubmittedtoTKA
whoremainedcolonizedbyS.aureusdespiteprophylacticND, Economedesetal.,29inapilotstudy,evaluated634patients
whounderwenttheprocedurebythesamesurgeonandwho
completedanNDprotocolbeforesurgery.Theauthors
demon-stratedthat33%(19of58)ofthepatientswhounderwentND continuedtopresentpositiveS.aureusculturedespite preop-erativedecolonization,inferringthatNDisnotabletoensure
thatpatientswillremaindecolonizedthroughoutthe postop-erativeperiod.TheeffectsofpersistentS.aureuscolonization inthepostoperativeperiodrequirefurtherstudiesinorderto assertthatthisgroupofpatientsisatgreaterriskofacquiring lateinfection.29
Inthesamelineofreasoning,theInternationalConsensus onPeriprostheticJointInfections,conductedbyParvizietal.,2
indicatedthatpatientscolonizedbyMRSA,especiallyinthe anteriorportionofthenostrils,haveapotentialsourceof hos-pitalandpostoperativeinfections,andthatNDwithtopical mupirocinappliedtothenostrilsforfivedayspriortosurgery wasaneffectivemeasureinreducingtheincidenceofSSI.
ThereductionofSSIrateafterMRSAscreeningand prophy-laxiscorroboratestheclinicalandpathologicalreasoning,in
whichthispathogenstandsoutasoneofthemaincausesof
infectionduetoitshighpresenceinthein-hospitaland gen-eralpopulations.TheconcernwiththeMRSAstrainishigher duetoits difficulttreatmentand control,sinceit doesnot respondtobeta-lactam antibiotics,including synthetics,as
inthe caseofmethicillin,which impliesthe needfor
ade-quate preoperativeprophylaxis.30 TopicalmupirocinforND
isthetreatmentofchoice.31Althoughsomefirst-generation
cephalosporins areefficientagainstS.aureus, thesearenot the first-choiceantimicrobial, eitherbecause theyhave
indiscriminateusecancontributetotheemergenceof drug-resistantbacteria.32
FailuretoperformprophylaxisagainstSSIinthe preoper-ativeperiodoffersevidencefortheclinicalandpathological
reasoningregardingthiscomplicationbydemonstratingthe
increaseintheriskfactorforitsoccurrence.33
In general, the following pathogens can also cause
periprosthetic infection: Coagulase-negative staphylococci,
Streptococcus,andGram-negativeandanaerobicbacilli.34
Inthestudies byBaratzet al.,24 Haceket al.,25 and Rao
etal.,22itwaspossibletoinferthat,inspiteofthesignificant
reductioninSSIduetotheS.aureusscreeningandprophylaxis protocol,infectionswerealsocausedbyotherpathogens,such asPseudomonas,Enterobacter,andStreptococcus,amongothers. ThevariationintheincidenceofS.aureusisrelatedtothe existenceofassociatedriskfactorsofinfection,suchas obe-sity,earlyage,anddiabetes.35Thus,populationswithdifferent
characteristicsmaypresentdifferentSSIincidencerates.35
Duetoitsinherentcharacteristicofgroupingseveral
stud-ies, combining the individual samples and results into a
synthesis, some factors could not be approached in the
presentstudy,suchasthequantitativeandqualitativeimpact oftheprofileofdifferentpopulations onthe rateofSSI in
patientssubmittedtheTKAandTHA,thelong-termefficacy
ofthesystematicuseofthesuggestedprophylacticmethod,
aswellasthespectrumofactionoftheantibioticusedand possibleassociations.Therefore,newstudiesarerequiredto performamultivariateanalysisofthesefactors.
This systematic review with meta-analysis, as others
retrieved in the literature, is based on secondary data
extractedfromoriginalcohortstudies.However,this charac-teristicisalimitationforthemodel,sinceitdoesnotallowthe assessmentofallthedatanecessaryformultivariateanalyses andissubjecttopossiblebiases.
Theinherentcharacteristicsofthestudyconferitalevel ofevidence2accordingtotheLevelofScientificEvidenceby
TypeofStudy(OxfordCentreforEvidence-based Medicine):
systematicreviewofhomogenouscohortstudies.18
Althoughthediagnosticpossibilitieshaveimprovedwith
thedevelopment ofnewimmunological andimaging
tech-niques,thedevastatingconsequencesofaninfection,even
when early diagnosed, remain a major challenge for the
orthopedic surgeon. Thus, the development of additional
prophylaxis techniques should be investigated in order to
achieveanevengreaterreductionofthisseriouscomplication.
Nonetheless,NDscreeningforS.aureusanditsMRSAstrain
throughnasopharyngealswabcollectioncanbepresentedas
aneffectivemeasureinthereductionofSSIinTKAandTHA
thatshouldbeimplemented.
Final
considerations
Theinvestigationofnasopharyngealswabmaterialtodetect
colonization by Staphylococcus aureus and its
methicillin-resistantvariantinpatientswithindicationforTKAandTHA,
followed by decolonization with topical antibiotic therapy
withmuporicin,presentsdatathatconfirmtheeffectiveness ofitsuseasaprophylacticmethodinordertoreducetherates ofpostoperativeinfection.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.LimaALLM,PécoraJR,AlbuquerqueRM,PaulaAP,D’EliaCO, SantosALG,etal.Infectionfollowingtotalkneejoint arthroplasty:considerationsandtreatment.ActaOrtopBras. 2004;12(4):236–41.
2.ParviziJ,GehrkeT.ConsensoInternacionalemInfecc¸ões ArticularesPeriprotéticas.Availablefrom:
http://www.rbo.org.br/pdf/consensos/consensosciiap.pdf [accessed11.01.16].
3.AlmeidaRF,QueirozAA,BellotiJC,CastroFilhoJM,CohenM, NavarroRD.Approachtowardstotalkneearthroplastyin Brazil:cross-sectionalstudy.SaoPauloMedJ.
2009;127(4):190–7.
4.D’EliaCO,SantosALG,LeonhardtMC,LimaALLM,PécoraJR, CamanhoGL.Treatmentofinfectionsfollowingtotalknee arthroplasty:2-yearfollow-upoutcomes.ActaOrtopédica Bras.2007;15(3):158–62.
5.CarvalhoJúniorLH,TemponiEF,BadetR.Infecc¸ãoem artroplastiatotaldejoelho:diagnósticoetratamento.Rev BrasOrtop.2013;48(5):389–96.
6.ChoiH-R,vonKnochF,ZurakowskiD,NelsonSB,MalchauH. Canimplantretentionberecommendedfortreatmentof infectedTKA?ClinOrthopRelatRes.2011;469(4):961–9. 7.PradellaJGDP,BovoM,SallesMJC,KlautauGB,CamargoOAP,
CuryRPL.Artroplastiaprimáriadejoelhoinfectada:fatores deriscoparafalhanaterapiacirúrgica.RevBrasOrtop. 2013;48(5):432–7.
8.Organizac¸ãoMundialdaSaúde.Segundodesafioglobalparaa seguranc¸adopaciente:Cirurgiassegurassalvamvidas (orientac¸õesparacirurgiaseguradaOMS).RiodeJaneiro: Organizac¸ãoPan-AmericanadaSaúde;MinistériodaSaúde; AgênciaNacionaldeVigilânciaSanitária;2009.Available form:http://bvsms.saude.gov.br/bvs/publicacoes/ segurancapacientecirurgiasalvamanual.pdf. 9.CentersforDiseasePreventionandControl(CDC).The
NationalHealthcareSafetyNetwork(NHSN)Manual. Healthcarepersonnelsafetycomponentprotocol.Atlanta, GA,USA:CDC;2009.Availablefrom:
http://www.cdc.gov/nhsn/pdfs/hspmanual/hpsmanual.pdf. 10.AndersonDJ,PodgornyK,Berríos-TorresSI,BratzlerDW,
DellingerEP,GreeneL,etal.Strategiestopreventsurgicalsite infectionsinacutecarehospitals:2014update.InfectControl HospEpidemiol.2014;35(6):605–27.
11.RezapoorM,ParviziJ.Preventionofperiprostheticjoint infection.JArthroplasty.2015;30(6):902–7.
12.EvangelistaSS,OliveiraAC,EvangelistaSS,OliveiraAC. Community-acquiredmethicillin-resistantStaphylococcus aureus:aglobalproblem.RevBrasEnferm.2015;68(1):136–43. 13.HombachM,PfyfferGE,RoosM,LuckeK.Detectionof
methicillin-resistantStaphylococcusaureus(MRSA)in specimensfromvariousbodysites:performance characteristicsoftheBDGeneOhmMRSAassay,theXpert MRSAassay,andbroth-enrichedcultureinanareawithalow prevalenceofMRSAinfections.JClinMicrobiol.
2010;48(11):3882–7.
14.ParviziJ,GhanemE,SharkeyP,AggarwalA,BurnettRSJ, BarrackRL.Diagnosisofinfectedtotalknee:findingsofa multicenterdatabase.ClinOrthop.2008;466(11):2628–33. 15.CoiaJE,DuckworthGJ,EdwardsDI,FarringtonM,FryC,
ofmeticillin-resistantStaphylococcusaureus(MRSA)in healthcarefacilities.JHospInfect.2006;63Suppl.1:S1–44. 16.DaSilvaPintoCZ,AlpendreFT,StierCJN,MazieroECS,de
AlencarPGC,deAlmeidaCruzED.Characterizationofhipand kneearthroplastiesandfactorsassociatedwithinfection.Rev BrasOrtop.2015;50(6):694–9.
17.LaudermilchDJ,FedorkaCJ,HeylA,RaoN,McGoughRL. Outcomesofrevisiontotalkneearthroplastyafter methicillin-resistantStaphylococcusaureusinfection.Clin Orthop.2010;468(8):2067–73.
18.MoherD,ShamseerL,ClarkeM,GhersiD,LiberatiA, PetticrewM,etal.Preferredreportingitemsforsystematic reviewandmeta-analysisprotocols(PRISMA-P)2015 statement.SystRev.2015;4:1.
19.OttawaHospitalResearchInstitute.Availablefrom:
http://www.ohri.ca/programs/clinicalepidemiology/oxford.asp [accessed11.08.16].
20.PhillipsB,BallC,SackettD,BadenochD,StrausS,HaynesB, etal.Oxfordcentreforevidence-basedmedicinelevelsof evidence;1998.Availablefrom:
http://www.cebm.net/levelsofevidence.asp.
21.BernardoWM,NobreMRC,JateneFB.Evidencebasedclinical practice:partII–searchingevidencedatabases.RevAssoc MédicaBras.2004;50(1):104–8.
22.RaoN,CannellaB,CrossettLS,YatesAJ,McGoughR.A preoperativedecolonizationprotocolforStaphylococcus aureuspreventsorthopaedicinfections.ClinOrthop. 2008;466(6):1343–8.
23.BarberoAllendeJM,RomanykCabreraJ,MonteroRuizE, VallésPurroyA,MelgarMoleroV,AgudoLópezR,etal. EradicationofStaphylococcusaureusincarrierpatients undergoingjointarthroplasty.EnfermInfecMicrobiolClin. 2015;33(2):95–100.
24.BaratzMD,HallmarkR,OdumSM,SpringerBD.Twenty percentofpatientsmayremaincolonizedwith methicillin-resistantStaphylococcusaureusdespitea decolonizationprotocolinpatientsundergoingelectivetotal jointarthroplasty.ClinOrthop.2015;473(7):2283–90.
25.HacekDM,PauleSM,ThomsonRB,RobicsekA,PetersonLR. Implementationofauniversaladmissionsurveillanceand decolonizationprogramformethicillin-resistant
Staphylococcusaureus(MRSA)reducesthenumberofMRSA andtotalnumberofS.aureusisolatesreportedbytheclinical laboratory.JClinMicrobiol.2009;47(11):3749–52.
26.LeventT,VandeveldeD,DelobelleJ-M,LabourdetteP, LétendardJ,LesageP,etal.Infectionriskpreventionfollowing totalkneearthroplasty.OrthopTraumatolSurgRes.
2010;96(1):49–56.
27.MatarWY.Preventinginfectionintotaljointarthroplasty.J BoneJtSurgAm.2010;92Suppl.2:36.
28.NasserS.Preventionandtreatmentofsepsisintotalhip replacementsurgery.OrthopClinNorthAm.
1992;23(2):265–77.
29.EconomedesDM,DeirmengianGK,DeirmengianCA. Staphylococcusaureuscolonizationamongarthroplasty patientspreviouslytreatedbyadecolonizationprotocol:a pilotstudy.ClinOrthop.2013;471(10):3128–32.
30.PatelH,KhouryH,GirgentiD,WelnerS,YuH.Burdenof surgicalsiteinfectionsassociatedwitharthroplastyandthe contributionofStaphylococcusaureus.SurgInfect.
2016;17(1):78–88.
31.ChandrananthJ,RabinovichA,KarahaliosA,GuyS,TranP. Impactofadherencetolocalantibioticprophylaxisguidelines oninfectionoutcomeaftertotalhiporkneearthroplasty.J HospInfect.2016;93(4):423–7.
32.DuplessisC,Crum-CianfloneNF.Ceftarolineanew cephalosporinwithactivityagainstmethicillin-resistant Staphylococcusaureus(MRSA).ClinMedRevTher.2011;3, pii:a2466.
33.WuCT,ChenIL,WangJW,KoJY,WangCJ,LeeCH.Surgical siteinfectionaftertotalkneearthroplasty:riskfactorsin patientswithtimelyadministrationofsystemicprophylactic antibiotics.JArthroplast.2016;31(7):1568–73.
34.RosenthalVD.Internationalnosocomialinfectioncontrol consortium(INICC)resources:INICCmultidimensional approachandINICCsurveillanceonlinesystem.AmJInfect Control.2016;44(6):e81–90.