2011 Jan-Feb;19(1):11-7 www.eerp.usp.br/rlae
Corresponding Author:
Fernanda Raphael Escobar Gimenes
Universidade de São Paulo. Escola de Enfermagem de Ribeirão Preto. Departamento de Enfermagem Geral e Especializada.
Av. Bandeirantes, 3.900 Bairro Monte Alegre
CEP: 14040-902 Ribeirão Preto, SP, Brasil
E-mail: fer_gimenes@yahoo.com.br / fergimenes@usp.br
Medication Wrong-Route Administrations in Relation
to Medical Prescriptions
Fernanda Raphael Escobar Gimenes
1Tatiane Cristina Marques
2Thalyta Cardoso Alux Teixeira
3Maria Lurdemiler Sabóia Mota
4Ana Elisa Bauer de Camargo Silva
5Silvia Helena De Bortoli Cassiani
6This study analyzes the influence of medical prescriptions’ writing on the occurrence of medication
errors in the medical wards of five Brazilian hospitals. This descriptive study used data obtained
from a multicenter study conducted in 2005. The population was composed of 1,425 medication
errors and the sample included 92 routes through which medication was wrongly administered.
The pharmacological classes most frequently involved in errors were cardiovascular agents
(31.5%), medication that acts on the nervous system (23.9%), and on the digestive system
and metabolism (13.0%). In relation to the prescription items that may have contributed to
such errors, we verified that 91.3% of prescriptions contained acronyms and abbreviations;
patient information was missing in 22.8%, and 4.3% did not include the date and were effaced.
Medication wrong-route administrations are common in Brazilian hospitals and around the world.
It is well established that these situations may result in severe adverse events for patients,
including death.
Descriptors: Medication Errors; Drug Prescriptions; Safety Management; Drug Administration
Routes.
1 RN, Doctoral Student of Nursing, Escola de Enfermagem de Ribeirão Preto, Universidade de São Paulo, WHO Collaborating Centre for Nursing
Research Development, SP, Brazil. Professor, Universidade Camilo Castelo Branco, São Paulo, SP, Brazil. Email: fer_gimenes@yahoo.com.br.
2 Pharmacy-Biochemistry, M.Sc. in Nursing, Hospital São Lucas, Ribeirão Preto, SP, Brazil. E-mail: tatianecm@hotmail.com.
3 RN, Hospital Vera Cruz, Campinas, SP, Brazil. Doctoral Student in Nursing, Escola de Enfermagem de Ribeirão Preto, Universidade de São Paulo,
WHO Collaborating Centre for Nursing Research Development, SP, Brazil. E-mal: thalytacat@yahoo.com.br. 4 RN, Ph.D. in Pharmacology, Assistant Professor, Universidade de Fortaleza, CE, Brazil. Email: mila269@terra.com.br.
5 RN, Ph.D. in Nursing, Adjunct Professor, Universidade Federal de Goiás, GO, Brazil. E-mail: anaelisa@terra.com.br.
6 RN, Ph.D. in Nursing, Full Professor, Escola de Enfermagem de Ribeirão Preto, Universidade de São Paulo, WHO Collaborating Centre for
Administração de medicamentos, em vias diferentes das prescritas, relacionada à prescrição médica
O objetivo foi analisar a inluência da redação da prescrição médica nos erros de via de administração, ocorridos em enfermaria de clínica médica de cinco hospitais brasileiros. Estudo descritivo que utilizou dados de pesquisa multicêntrica, realizada em 2005. A população foi composta por 1.425 erros de medicação e a amostra por 92 erros de
via. As classes farmacológicas mais envolvidas no erro foram as cardiovasculares
(31,5%), drogas que atuam no sistema nervoso (23,9%) e no sistema digestório e
metabolismo (13,0%). No que diz respeito aos itens da prescrição médica, que poderiam ter contribuído com os erros de via, veriicou-se que 91,3% das prescrições continham
siglas/abreviaturas, 22,8% não continham dados do paciente e 4,3% não apresentavam
data e continham rasuras. Erros de via são frequentes nos hospitais brasileiros e ao
redor do mundo, e se sabe que essas situações podem resultar em eventos adversos
severos aos pacientes, incluindo morte.
Descritores: Erros de Medicação; Prescrições de Medicamentos; Gerenciamento de Segurança; Vias de Administração de Medicamentos.
Administración de medicamentos en vías diferentes de las indicadas en la prescripción médica
El objetivo fue analizar la inluencia de la redacción de la prescripción médica en los errores de vía de administración ocurridos en la enfermería de clínica médica de cinco
hospitales brasileños. Se trata de un estudio descriptivo que utilizó datos de investigación
multicéntrica realizada en 2005. La población fue compuesta por 1.425 errores de medicación y la muestra por 92 errores de vía. Las clases farmacológicas más envueltas
en el error fueron: 1) las cardiovasculares (31,5%), 2) las drogas que actúan en el
sistema nervioso (23,9%), y 3) las que actúan en el sistema digestivo y metabolismo
(13,0%). En lo que se reiere a los ítems de la prescripción médica que podrían haber contribuido con los errores de vía, se veriicó que 91,3% de las prescripciones contenían siglas/abreviaturas; 22,8% no contenían datos del paciente, y 4,3% no presentaban fecha y contenían raspados. Errores de vía son frecuentes en los hospitales brasileños
y alrededor del mundo y se sabe que estas situaciones pueden resultar en eventos
adversos severos en los pacientes, incluyendo la muerte.
Descriptores: Errores de Medicación; Prescripciones de Medicamentos; Administración
de La Seguridad; Vías de Administración de Medicamentos.
Introduction
Errors in healthcare result from a non-intentional
action caused by some problem or failure during care
delivered to patients(1), and can be committed by any
member of the health team at any point of the care
process such as when administering medication to
patients. Medication errors can occur at any stage of
medication therapy, from writing the prescription to the
administration of medication to patients, and represents
about 65% to 87% of all adverse events(2).
Physicians traditionally decide on the medication to
be used and then prescribe it so that pharmacists and
the nursing staff implement their decisions. Hence, the
medical prescription is the document that guides and
inluences the other stages of the medication process.
Medical prescriptions have an important role in the
prevention and occurrence of errors. It is known that
ambiguous, illegible or incomplete prescriptions, the
a standardized medication nomenclature (brand name
or generic) are factors that can contribute to medication
errors(3).
In relation to medication errors that may occur in
the administration stage, we can highlight dosage errors
(overdosing or underdosing, including omissions),
dosage form, and route of administration, in addition
to administering the wrong medication, to the wrong
patient, with the wrong frequency and/or at the wrong
time.
An account of error reporting from the United
States Pharmacopeia (USP) stated that one of the most
frequent errors harming patients is related to the route
of administration(4). Studies presented frequencies
of 19%(5) and 18%(6) of errors related to the route of
administration among all medication errors.
Since errors in the route of administration are
common in care delivery, this study analyzes the inluence
of a prescription’s writing on the administration of
medication resulting in wrong-route administration that
occurred in the medical units of ive Brazilian hospitals.
Methods
This descriptive study used secondary data
obtained from a multicenter study carried out in 2005
in ive Brazilian university hospitals(7), named A, B, C, D, and E, all belonging to the ANVISA network of
Sentinel Hospitals. The study was authorized by the
studied hospitals and approved by the Research Ethics
Committee.
The study’s population was composed of 1,425
situations in which the administered medication was
in disagreement with the medical prescription; the
sample also included 92 situations in which the route of
administration used was different from that speciied in
the medical prescription. For that information, data from
the databases EPIDATA version 3.1 of the ive studied
hospitals, obtained through a data collection instrument
of the multicenter study and which addressed the
prescription of medication dosages, was used.
The variables were determined based on items
contained or lacking in medical prescriptions: absence
of patient’ data (name, bed number, and registration
number); absence of data; absence of medication
data (route of administration); acronyms and/or
abbreviations; changes and/or discontinuation of
medication; and obscure writing.
This information was passed through the SPSS
version 11.5 (SPSS Inc., Chicago, II, USA). The results
obtained in this analysis were distributed in tables and
expressed as absolute frequencies and percentages.
The pharmacological classiication of medication
involved in errors was performed according to the
Anatomical Therapeutic Chemical (ATC) classiication
system by WHO Collaborating Centre for Drug Statistics
Methodology.
Results
With respect to medication wrong-route
administrations, discrepancies were observed in 92
(6.5%) cases of the total of the 1,425 medication
errors and hospital A accounted for the majority of such
events, with a frequency of 34 (37.0%). Hospital B was
responsible for 22 (23.9%); C for ive (5.4%); D for 26 (28.3%); and ive (5.4%) drugs were administered via
routes different from those prescribed in hospital E.
Some examples wrong-route administrations are
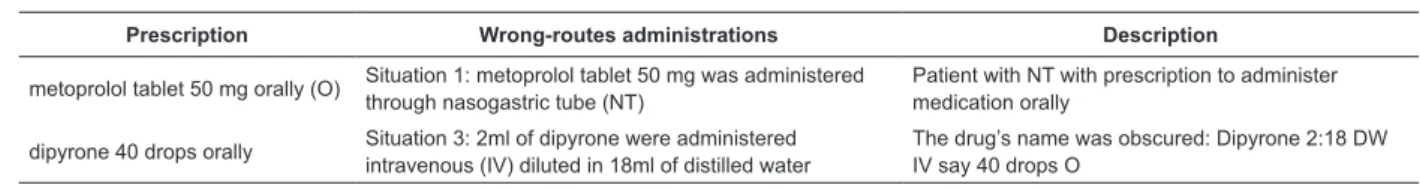
presented in Table 1.
Table 1 –Examples of situations in which discrepancies between prescribed and administered routes were observed.
Ribeirão Preto, SP, Brazil 2006
Prescription Wrong-routes administrations Description
metoprolol tablet 50 mg orally (O) Situation 1: metoprolol tablet 50 mg was administered through nasogastric tube (NT)
Patient with NT with prescription to administer medication orally
dipyrone 40 drops orally Situation 3: 2ml of dipyrone were administered intravenous (IV) diluted in 18ml of distilled water
The drug’s name was obscured: Dipyrone 2:18 DW IV say 40 drops O
In relation to the pharmacological classes involved
in wrong-route administrations, according to the ATC
system, 31.5% of the medication belonged to group
C (cardiovascular system), while captopril was the
most frequent drug, representing 16.3% of the total of
cases; 23.9% of the medication administered in wrong
routes belonged to group N (nervous system). Of these,
dipyrone and tramadol hydrochloride were the most
frequent, each representing 3.3% of the total of events
Rev. Latino-Am. Enfermagem 2011 Jan-Feb;19(1):11-7.
Then the medications of group A (digestive system
and metabolism) were present in 13.0% of the
wrong-route administrations, while ranitidine was the most
common (6.5%) in this group. Group H (hormones used
for systemic therapy, except sexual hormones) was also
administered in wrong routes in 9.8% of the total cases
(Table 2).
Table 2 – Distribution of the frequency with which
medication wrong-route administrations occurred in the
medical wards of ive Brazilian hospitals according to the
WHO’s ATC system. Ribeirão Preto, SP, Brazil. 2006
ATC Class – Level 1 N %
Group C – Cardiovascular system 29 31.5
Group N – Nervous system 22 23.9
Group A – Digestive system and metabolism 12 13.0
Group H – Hormones for systemic use, with
exception of sex hormones 9 9.8
Group M – Musculoskeletal system 4 4.3
Group J – Anti-infectives for systemic use 3 3.3
Group B – Blood, organs and derivatives 3 3.3
Others 10 10.9
Total 92 100.0
Analyzing the items of the medical prescriptions
that could be related to discrepancies in the routes
of administration, we observed that 84 (91.3%)
prescriptions had acronyms and/or abbreviations (e.g.
clindamycin 600mg GTT; dipyrone 1 ampoule IV PRN;
Predifort 1 drop O); the patient’s registration number
was not recorded in 21 (22.8%) prescriptions; two
(2.2%) omitted the date and had erasures. The route of
the medication administration was not speciied in one
(1.1%) prescription (Table 3). The patients’ name and
bed, though, were speciied in all situations in which
wrong-administrations occurred.
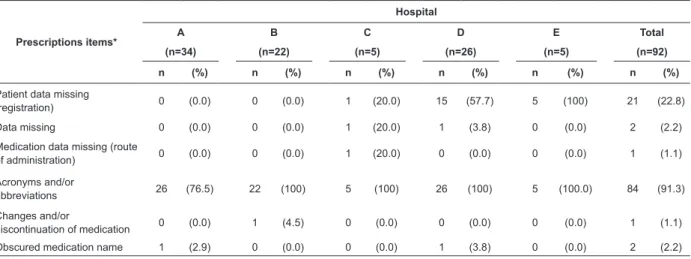
Table 3 presents the analysis of items in the
prescriptions that may be related to wrong-route
administrations according to the studied hospital.
According to Table 3, of the 34 medication
administered via routes different from those prescribed
in hospital A, 26 (76.5%) had acronyms and/or
abbreviations in the dosage wording even though the
prescriptions were electronic.
Table 3 – distribution of the frequency with medication wrong-route administrations occurred in medical wards of
ive Brazilian hospitals according to the presence or absence of items in the prescription. Ribeirão Preto, SP, Brazil.
2006
Prescriptions items*
Hospital
A B C D E Total
(n=34) (n=22) (n=5) (n=26) (n=5) (n=92)
n (%) n (%) n (%) n (%) n (%) n (%)
Patient data missing
(registration) 0 (0.0) 0 (0.0) 1 (20.0) 15 (57.7) 5 (100) 21 (22.8)
Data missing 0 (0.0) 0 (0.0) 1 (20.0) 1 (3.8) 0 (0.0) 2 (2.2)
Medication data missing (route
of administration) 0 (0.0) 0 (0.0) 1 (20.0) 0 (0.0) 0 (0.0) 1 (1.1)
Acronyms and/or
abbreviations 26 (76.5) 22 (100) 5 (100) 26 (100) 5 (100.0) 84 (91.3)
Changes and/or
discontinuation of medication 0 (0.0) 1 (4.5) 0 (0.0) 0 (0.0) 0 (0.0) 1 (1.1)
Obscured medication name 1 (2.9) 0 (0.0) 0 (0.0) 1 (3.8) 0 (0.0) 2 (2.2)
* Each prescription may have more than one error.
The following acronyms and abbreviations were
found: TB for tablets (e.g. “Complex B 1 TB”); the
use of the letter D to indicate the number of days an
antibiotic should be administered (e.g. “metronidazole
100 mg tablet oral beginning on 06/22/2005 D1/3”);
IU instead of International Units (e.g. heparin sodium
5,000 IU subcutaneously); DRP referring to drops (e.g.
“clonazepam 10 DRP orally”), among others. In hospitals
B, C, D and E, 100% of the prescriptions had acronyms and/or abbreviations.
Yet, according to Table 3, the patients’ registration information was missing in 100% of the prescriptions where the medication was administered via routes
different from those speciied in hospital E and in 15
Discussion
A study conducted in the United States of
America identiied 1.8% of medication wrong-route
administrations in a total of 146,974 events reported in
the United States Pharmacopeia system (USP)(4). Only
one (0.4%) route error was detected in a total of 240
events in an large American university hospital(8).
Among the 798 administered doses investigated
by a study conducted in six European hospitals, 1%
was wrong-route administrations(9). In another study
carried out in a French hospital, 102 (19.0%) cases of
medication wrong-route administrations were identiied
in a total of 538 adverse events related to medication.
Most of these events were related to the administration
of doses through nasogastric tubes (NGT) instead of oral
administration,, similar to data found in this study and
which corroborates the results of other studies(5,10-11).
The frequency of wrong-route administrations
found in this study is considerably divergent from other
studies, probably due to the different methods adopted,
since not all consider an error to have occurred when
medication is administered through gastric or enteric
tubes instead of orally or vice-versa(9). In practice, what
normally occurs is that the nursing team crushes tablets
or pills, or open capsules and dissolves the powder in
some liquid to enable the administration of medication
actually prescribed for the oral route in patients with
gastric or enteric tubes(12).
However, it must be noted that it is crucial in the
administration of medication to consider the medication’s
pharmaceutical form and the chemical and physical
features of each drug. Among these characteristics are
solubility, partition coeficient, dissolution rate, dosage
form and stability. For instance, pH variation in the
gastrointestinal tract affects the degree of ionization of
the drug molecules, which in turn inluences its solubility
and absorption capacity(12-13). Hence, the administration
of medication via routes different from those indicated
by the manufacturer may represent a variation in the
bioavailability of the drug and consequently change its
therapeutic response.
Additionally, the process of crushing and dissolving
solid oral dosage forms may generate other problems
such as destroying the protective coating of enteric or
controlled release medications or even clogging the
tube, consequently increasing the risk of morbidity and
mortality and also costs related to drug therapy(14).
Considering these aspects, the literature has
demonstrated that among wrong-route administrations,
the most frequent situation is that in which medication
prescribed for oral use is administered through tubes
(5,10-11). Many factors contribute to these errors, such as lack
of knowledge or information concerning the therapy
and alternative pharmaceutical forms, inappropriate
evaluation and use of patients’ information, prescription
and confusing drug nomenclature, wrong calculation of
dosage and inappropriate pharmaceutical form, factors
that also contribute to the occurrence of prescription
errors(6,15).
Properly administering medication to patients is the
role of the nursing team, which represents an important
barrier for the interception of errors(15). However, it
is necessary for professionals to be technically and
scientiically supported to safely and eficiently administer
pharmacotherapy. A study carried out in Europe showed
that integrated multidisciplinary actions involving nurses,
pharmacists, physicians and nutritionists, promoted the
correct implementation of medication therapy, especially
in patients using gastric and enteral tubes(14).
In regard to pharmacological groups, medication
wrong-route administrations were the most frequent
in the groups C, N, and A, that is, medication for the
cardiovascular, nervous and digestive systems. Other
investigations also indicate that cardiovascular and
digestive medication are the main classes involved in the
occurrence of discrepancies between the prescribed and
administered routes(10-11). This inding may be explained
by the large use of these classes of medication, especially
captopril and ranitidine, in medical wards.
Hospital A, in which prescriptions were electronic,
accounted for the highest frequency of wrong-route
administrations. Electronic prescription is a technology
that should be used to facilitate and ensure the safer
use of medications(16), however, when not appropriately
used, it does not meet such objectives. It is apparent
that the implementation of electronic prescriptions does
not eliminate the possibility of medication errors since
wrong-route administrations still frequently occurs in
Brazilian hospitals and around the world. Such indings
are of concern because we know that, depending on the
medication and its pharmacological class, errors may
lead to severe adverse events, including death.
In relation to the writing of medical prescriptions
and what may have contributed to this type of error,
the use of acronyms and abbreviations was the most
common. It seems that the use of these is seen as a
way to save time during the writing of the prescription,
since a single physician is responsible for prescribing
Rev. Latino-Am. Enfermagem 2011 Jan-Feb;19(1):11-7.
to be reviewed by physicians, since many of these
acronyms and abbreviations are not understood by all
the professionals who handle prescriptions, especially
when there is not a formal standard in the facility.
Even when acronyms and abbreviations are
standardized, the health team should avoid them,
especially when the method of prescription is manual
since illegible handwriting may lead to a misunderstanding
with a consequent inappropriate use of medication (e.g.
the acronym SC may be easily misunderstood as SL, and
IV may also be read as IM).
Additionally, the omission of information in
prescriptions can greatly contribute to errors. In a
situation that occurred in hospital C, the absence of
the route of administration in the prescription was
possibly the main cause that led to the wrong-route
administration. It shows that a correctly written
prescription with complete and necessary information
for the safe administration of medication is a barrier to
medication errors(16).
Another important factor contributing to errors
in the medication system is the presence of obscured
writing in prescriptions, which may confuse the nursing
team. The error situation presented in Table 1 involving
dipyrone demonstrates that the dosage form was
changed (drops and ampoule), which may have been
induced by damage to the prescription that led to the
administration of the injectable form instead of the
oral form. It is also recommended that professionals
carefully read the medical prescription identifying the
“ive rights” of medication safety that includes the route
of administration so to ensure the correct administration
of medication(17).
We also know that the analysis of the origins
of such events reveal they are related to a deicit of
knowledge on the part of the health team, as well as
a deicit of performance(18), which requires that the quality of teaching of pharmacology in undergraduate
and graduate nursing programs be reviewed and also
the implementation and maintenance of permanent
education programs in health units promoted by nurses
and the other members of the nursing staff.
There has been growing interest in studies addressing
medication errors from the perspective that deeper
knowledge regarding this topic may represent increased
safety for patients and, consequently, increased quality
of health services. Therefore, studies have addressed
the occurrence of errors in the prescription, dispensation
and administration of medication that need to be
analyzed more deeply to determine their causes and
intervenient factors(16-22). Hence, this study contributes
to an analysis of the importance of medical prescriptions
in the prevention of medication administration errors,
especially in relation to errors related to the route of
administration.
Conclusion
This study’s results revealed that most of the 92 medication wrong-route administrations occurred in
hospital A, whose prescription method is electronic.
In relation to the pharmacological classes most
involved in this type of error, 25.0% included
anti-hypertensives followed by analgesics, antipyretics
and anti-inlammatory medication. Steroids and
glucocorticoids presented a frequency of 9.8%, while
antiulcer drugs represented 8.7% of total cases.
In relation to the items in the medical prescription
that may have contributed to wrong-route administrations,
91.3% of the prescriptions written in the ive studied
hospitals had acronyms and/or abbreviations such
as SC (subcutaneous) and GTT (gastrotomy), while there were acronyms and/or abbreviations in 100% of
the prescriptions involved in this type of error in the
hospitals B, C, D and E.
Even though the use of electronic prescriptions
was adopted in one of the studied hospitals, it did not
eradicate medication errors, since it permits the use of
acronyms and/or abbreviations, a factor that may lead to misunderstanding information. From this perspective,
health professionals need to be continually trained so
as to avoid the use of acronyms and abbreviations in
prescriptions even if standardized by the hospital, as well
as erasures, which may also lead to misunderstanding.
Therefore, the implementation of permanent education for the professionals involved in the medication
process can minimize harm caused to hospitalized
patients due to medication wrong-route administrations,
consequently improving the quality of care delivery.
References
1. Kohn LT, Corrigan JM, Donaldson MS, editores. To Error
is human: building a safer health system. Washington (DC): Committee on Quality of Health Care in America,
National Academy of Institute of Medicine; 2001.
2. Benjamin DM. Reducing medication errors and
increasing patient safety: case studies in clinical
pharmacology. J Clin Pharmacol. 2003;43:768-83.
de redação e opiniões de usuários. Rev Esc Enferm USP.
2003;37(4):51-60.
4. Santell JP, Hicks RW, McMeekin J, Cousins DD.
Medication errors: experience of the United States
Pharmacopeia (USP) medmarx reporting system. J Clin
Pharmacol. 2003;43:760-7.
5. Prot S, Fontan JE, Alberti C, Bourdon O, Farnoux C,
Macher MA, et al. Drug administration error and their
determinants in pediatric in-patients. Int J Qual Health
Care 2005;1(5):381-9.
6. Kaushal R, Bates DW, Landrigan C, McKenna KJ,
Clapp MD, Federico F, et al. Medication errors and
adverse drug events in pediatric inpatients. JAMA.
2001;285(16):2114-20.
7. Cassiani SHB. Identificação e análise dos erros de medicação em seis hospitais brasileiros. Ribeirão Preto
(SP): EERP; 2006. 60 p.
8. Winterstein AG, Thomas E, Rosenberg EI, Hatton
RC, Gonzalez-Rothi R, Kanjanarat P. Nature and
causes of clinically significant medication errors in
a tertiary care hospital. Am J Health Syst Pharm.
2004;61(18):1908-16.
9. Cousins DH, Sabatier B, Bengue D, Schmitt C,
Hoppe-Tichyl T. Medication errors in intravenous drug
preparation and administration: a multicentre audit in
the UK, Germany and France. Qual Saf Health Care.
2005;14:190-5.
10. Lesar TS. Medication prescribing errors
involving the route of administration. Hosp Pharm.
2006;41(11):1053-66.
11. Van den Bemt PMLA, Fijn R, Van der Voort PH,
Gossen AA, Egberts TC, Brouwers JR. Frequency and
determinants of drug administration errors in the
intensive care unit. Crit Care Med. 2002;30(4):846-50.
12. Heydrich J, Heineck I, Bueno D. Observation of
preparation and administration of drugs by nursing
assistants in patients with enteral feeding tube. Braz J
Pharm Sci. 2009;45(1):117-20.
13. Ansel HC, Popovich NG, Allen-Jr, LV. Formas
farmacêuticas e sistemas de liberação de fármacos. 6.
ed. São Paulo (SP): Artmed; 2000.
14. Van den Bemt PMLA, Cusell MBI, Overbeeke PW,
Trommelen M, Van Dooren D, Ophorst WR, Egberts ACG.
Quality improvement of oral medication administration
in patients with enteral feeding tubes. Qual Saf Health
Care. 2006;15:44–7.
15. Leape LL, Bates DW, Cullen DJ, Cooper J, Demonaco
H J, Gallivan T, et al. Systems analysis of adverse drug
events. JAMA. 1995; 274(1):35-43.
16. Gimenes FRE, Teixeira TCA, Silva AEBC, Optiz SP,
Mota MLSM, Cassiani SHB. Influência da redação da prescrição médica na administração de medicamentos
em horários diferentes do prescrito. Acta Paul Enferm.
2009;22(4):380-4.
17. Teixeira TCA, Cassiani SHB. Análise de causa
raiz: avaliação de erros de medicação de um Hospital
Universitário. Rev Esc Enferm USP. 2010;44(1):139-46.
18. The Massachusetts Coalition for the Prevention
of Medication Errors (USA). Safety First: wrong-route
errors. Massachusetts: Massachusetts Coalition for the
Prevention of Medication Errors; 1999.
19. Miasso AI, Silva AEBC, Cassiani SHB, Grou CR, Oliveira
RC, Fakih FT. O processo de preparo e administração de medicamentos: identificação de problemas para propor melhorias e prevenir erros de medicação. Rev.
Latino-Am. Enfermagem. 2006;14(3):354-63.
20. Oliveira RC, Cassiani SHB. Caracterização da estrutura
para o preparo de medicamentos em hospitais de ensino:
fatores que interferem na qualidade da assistência. Rev.
Latino-Am. Enfermagem. 2007;15(2):224-9.
21. Telles Filho PCP, Praxedes MFS. Periódicos de
enfermagem e administração de medicamentos: identificação e categorização das publicações
de 1987 a 2008. Rev. Latino-Am. Enfermagem.
2009;17(5):721-9.
22. Miasso AI, Oliveira RC, Silva AEBC, Lyra DP Junior,
Gimenes FRE, Fakih FT, et al. Prescription errors in
Brazilian hospitals: a multi-centre exploratory survey.
Cad Saude Pública. 2009;25(2):313-20.
Received: Oct. 8th 2009