Objective: To determine chronological and corrected ages at acquisition of motor abilities up to independent walking in very low birth weight preterms and to determine up to what point it is necessary to use corrected age.
Methods: This was a longitudinal study of preterms with birth weight < 1,500 g and gestational age ≤ 34 weeks, free from neurosensory sequelae, selected at the high-risk infants follow-up clinic at the Hospital das Clínicas, Faculdade de Medicina de Botucatu, Universidade Estadual Paulista (UNESP) in Botucatu, Brazil, between 1998 to 2003, and assessed every 2 months until acquisition of independent walking.
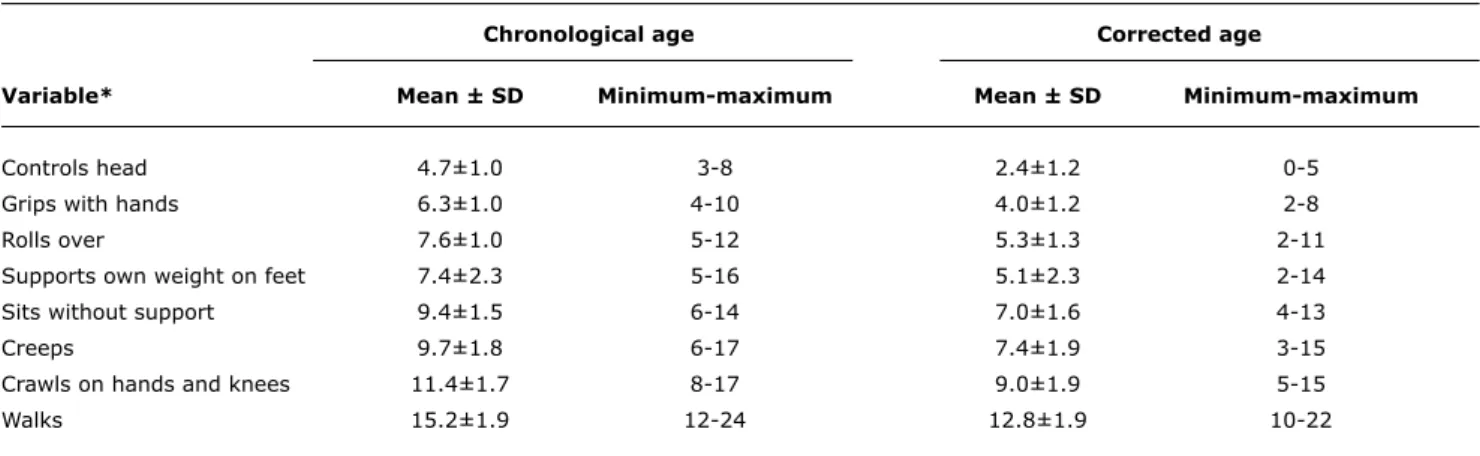
Results: Nine percent of the 155 preterms recruited were excluded from the study, leaving a total of 143 patients. The mean gestational age was 30±2 weeks, birth weight was 1,130±222 g, 59% were female and 44% were small for gestational age. Preterms achieved head control in their second month, could sit independent at 7 months and walked at 12.8 months’ corrected age, corresponding to the 4th, 9th and 15th months of chronological age. There were signiicant differences between chronological age and corrected age for all motor abilities. Preterms who were small for their gestational age acquired motor abilities later, but still within expected limits.
Conclusions: Very low birth weight preterms, free from neurosensory disorders, acquired their motor abilities within the ranges expected for their corrected ages. Corrected age should be used until independent walking is achieved.
J Pediatr (Rio J). 2010;86(2):143-148: Very low birth weight newborn, motor activity, development, gestational age.
ORiginal aRtiCle
Copyright © 2010 by Sociedade Brasileira de Pediatria143 introduction
Among the perinatal factors that determine neurological prognosis, prematurity merits the greatest attention because of its elevated incidence and because it is the most prevalent event among the etiologic factors of cerebral
palsy. This justiies taking the precaution of assessing child
development in a systematic manner, utilizing validated instruments and putting emphasis on motor development
during the irst years of life.1,2
It is recommended that corrected ages should be used when evaluating the development of premature infants in order not to underestimate their capacities. Notwithstanding, chronological age should also be taken into consideration because the development of some premature infants can be overestimated using corrected age.1,3,4
Over the last decade, many studies have been conducted into the neuromotor and cognitive development of
acquisition of motor abilities up to independent walking
in very low birth weight preterm infants
Sandra C. P. Volpi,1 lígia M. S. S. Rugolo,2 José C. Peraçoli,3 José eduardo Corrente4
1. Terapeuta ocupacional. Mestre, Obstetrícia. Supervisora, Unidade de Reabilitação, Hospital das Clínicas, Faculdade de Medicina de Botucatu, Universidade Estadual Paulista (UNESP), Botucatu, SP, Brazil.
2. Neonatologista. Chefe, Disciplina de Neonatologia, Departamento de Pediatria. Professora adjunta, Faculdade de Medicina de Botucatu, UNESP, Botucatu, SP, Brazil.
3. Ginecologista. Obstetra. Professor titular, Obstetrícia, Faculdade de Medicina de Botucatu, UNESP, Botucatu, SP, Brazil. 4. Professor adjunto, Departamento de Bioestatística, Instituto de Biociências, UNESP, Botucatu, SP, Brazil.
This study was carried out at Universidade Estadual Paulista (UNESP), Botucatu, SP, Brazil.
No conflicts of interest declared concerning the publication of this article.
Suggested citation: Volpi SC, Rugolo LM, Peraçoli JC, Corrente JE. Acquisition of motor abilities up to independent walking in very low birth weight preterm infants. J Pediatr (Rio J). 2010;86(2):143-148.
Manuscript submitted Aug 11 2009, accepted for publication Jan 20 2010.
premature infants during their irst years of life, primarily
focusing on predicting developmental risk factors and comparing premature and full term infants and different risk subsets among premature infants. There is a diverse range of study methodology, with variable results when the performance of premature and full term newborn infants are compared, and emphasis is on evaluating the development of premature infants within a risk context
aimed at preventing deiciencies and at identifying variables
that predict abnormal development.5 One feature that has
received little attention in development studies is the age at which motor abilities are acquired, especially sitting and walking, which can exhibit great variation among healthy children and may be delayed among premature children.6
The objective of this study was therefore to determine the chronological and corrected ages at which preterm infants born weighing less than 1500 g and free from neurosensory sequelae acquire their motor abilities and to evaluate up to what point it is necessary to use age correction.
Methods
This was a longitudinal study of very low birth weight preterm infants recruited at a neonatal intensive care unit and followed by the lead author at the rehabilitation unit of the Hospital das Clínicas, Faculdade de Medicina de Botucatu, Universidade Estadual Paulista (UNESP) in Botucatu, Brazil,
between 1998 and 2003. The study was approved by the
Research Ethics Committee at the institution, and mothers gave informed consent before their children were enrolled on the study.
The neonatology department basically treats patients on the Brazilian National Health Service (Sistema Único de Saúde) and provides multidisciplinary outpatients follow-up free of charge to all high risk infants until they reach school age. The neonatologists use the Denver II test every follow-up visit to screen infant’s development and Bayley II scores are calculated at 12 months of corrected age by the department’s psychologist. Children with developmental delays according to the Denver test or the Bayley scales are evaluated by the neuropediatrician. The occupational therapist is involved in follow-up and carries out two-monthly evaluations of the children at the rehabilitation unit, advising their carers about the best postures during routine activities to encourage the child’s motor development. Where
there are motor development delays speciic neuromotor
interventions are undertaken.
Since the study was designed to determine the normal age ranges for acquisition of motor abilities among very low birth weight preterms, preterms at lower neonatal risk of motor development problems were selected, on the basis of the following inclusion criteria:
- Start of follow-up at less than 4 months of chronological
age.
- Gestational age less than or equal to 34 weeks and birth
weight less than 1,500 g.
- Born at the UNESP maternity unit.
- 5 minute Apgar score greater than 3.
- Absence of neurological abnormalities during hospitalization, periventricular-intraventricular
hemorrhage grades 3-4 and/or periventricular
leukomalacia, major congenital malformations, genetic syndromes and congenital infections; not on oxygen at discharge; free from retinopathy of prematurity; and with a normal hearing test result.
The premature infants enrolled were seen every 2 months until they were able to walk, exhibited normal development, on the basis of Denver II and Bayley II results and did not
receive any speciic neuromotor interventions. In order
to avoid examiner bias, all children were evaluated by the same examiner (the occupational therapist) who was aware of the neuromotor development diagnosis, but did not have access to the results of the items assessed on the two scales until the end of the study.
At each consultation the therapist assessed the child’s motor performance, focusing on those abilities that should be present at the current child’s age, according to the limits for normality used at the department, which are based on data proposed for full term newborns by Bobath, the Brazilian Ministry of Health and Flehmig.7-9 If an appointment was
missed, the family was contacted by telephone and asked whether the motor abilities for that age had been achieved and in order to schedule the next consultation.
Data on the age at which each motor ability was acquired were obtained from the mothers and from the occupational therapist’s assessment, with preference given to the
therapist’s indings if the mother’s reports were in contrast
with the child’s performance during the consultation.
The following were exclusion criteria:
- Less than four consultations during the irst year of
life or dropping out of follow-up before acquisition of walking.
- Failure to attend two consecutive consultations.
- Need for neuromotor intervention or sensory deiciency,
convulsions or other intercurrent conditions that could compromise neuromotor development, such as
meningitis, fractures and/or surgery with hospitalization of 30 days or more.
Study variables: gestational age, taking the best available estimate, in the following order: precise date of last menstruation, obstetric ultrasonography before 20 weeks or New Ballard method10; anthropometry at birth;
appropriateness of birth weight for gestational age, according to the Alexander et al. criteria,11 deining appropriate weights
as between the 10th and 90th percentiles for gestational age and small when below the 10th percentile; sex; 5 minute Apgar score; and neonatal morbidity.
Outcomes of interest were the ages at which motor abilities were acquired in relation to the ranges of normality adopted at our institution’s rehabilitation unit7-9:
- Controls head = 1-3 months. - Grips with hands = 4-6 months. - Rolls over = 4-7 months.
- Supports own weight on feet = 5-6 months. - Creeps = 6-7 months.
- Sits without support = 7-9 months.
- Crawls on hands and knees = 8-10 months. - Walks = 12-15 months.
The premature infants were evaluated with respect to both their chronological and corrected ages. Corrected age was calculated as follows:
Corrected Age (weeks) = Chronological Age (weeks) - [40
- Gestational Age (weeks)].
The ages at which motor abilities were acquired were analyzed according to sex and appropriateness of birth weight for gestational age.
For the descriptive data analysis, continuous variables are presented as means and standard deviations with minimums
and maximums and categorical variables are expressed as frequencies and proportions of events. Differences between means for different groups were tested using Student’s t
test and proportions were compared using the chi-square
test. The signiicance level was set at 5% for all tests.
Results
During the period studied, 155 very low birth weight
preterms met the inclusion criteria, but 9% (n = 12) of
them were excluded from the study, four because they required neuromotor interventions and eight because of severe conditions that could compromise their development.
The remaining 143 premature infants comprised the study
sample and the ages at which each of them acquired each of their motor abilities up to independent walking was recorded.
The mean gestational age was 30±2 weeks (variation of 24-34 weeks), mean birth weight was 1,130±222 g (variation of 560-1,490 g), mean length was 37±2.7 cm and mean head circumference was 27±2.0 cm. The majority of the sample (86%) had a 5 minute Apgar greater than 7 and 59% were girls. There was a high percentage of small for gestational age premature infants (44%). Respiratory
distress syndrome was the most common neonatal disease,
affecting 55% of the sample. The motor ability acquisition
ages did not differ according to the infants’ sex.
The mean ages for all motor abilities were within the expected ranges according to corrected age and even using chronological age several abilities were present within the range of normality, with head control, creeping and crawling on hands and knees being acquired later (Table 1).
table 1 - Mean chronological and corrected ages (months) of motor ability acquisition for 143 very low birth weight preterms
SD = standard deviation.
* The number of observations was 143 for all variables.
Chronological age Corrected age
Variable* Mean ± SD Minimum-maximum Mean ± SD Minimum-maximum
Controls head 4.7±1.0 3-8 2.4±1.2 0-5
Grips with hands 6.3±1.0 4-10 4.0±1.2 2-8
Rolls over 7.6±1.0 5-12 5.3±1.3 2-11
Supports own weight on feet 7.4±2.3 5-16 5.1±2.3 2-14
Sits without support 9.4±1.5 6-14 7.0±1.6 4-13
Creeps 9.7±1.8 6-17 7.4±1.9 3-15
Crawls on hands and knees 11.4±1.7 8-17 9.0±1.9 5-15
Figure 1 - Percentage of premature infants acquiring motor abilities within expected age range, according to chronological and corrected ages
table 2 - Mean chronological and corrected ages of motor ability acquisition (months) for very low birth weight infants according to appropriateness of birth weight for gestational age
AGA = appropriate for gestational age; SGA = small for gestational age. * For all variables, AGA: n = 80 and SGA: n = 63.
Chronological age Corrected age
Variable* aga (n = 80) Sga (n = 63) p aga (n = 80) Sga (n = 63) p
Controls head 4.7±0.9 4.6±1.0 0.372 2.1±1.1 2.7±1.1 0.001
Grips with hands 6.4±1.0 6.1±1.1 0.175 3.7±1.1 4.2±1.1 0.008
Rolls over 7.6±1.1 7.4±1.0 0.349 5.0±1.3 5.6±1.2 0.006
Supports own weight on feet 7.6±2.3 7.2±2.2 0.327 5.0±2.4 5.4±2.2 0.294
Sits without support 9.4±1.4 9.3±1.7 0.667 6.7±1.4 7.4±1.7 0.009
Creeps 9.8±1.9 9.6±1.6 0.559 7.1±2.0 7.7±1.7 0.050
Crawls on hands and knees 11.3±1.6 11.4±1.8 0.682 8.6±1.7 9.5±1.9 0.004
Walks 15.2±1.6 15.4±1.7 0.142 12.2±1.5 13.5±2.0 < 0.001
Figure 1 illustrates that the great majority of the premature infants acquired their abilities within the expected
range for their corrected ages, with a signiicant difference
in comparison with the chronological ages, according to which a lower percentage acquired all abilities.
Discussion
The neuromotor development of premature infants has been the subject of great interest in the literature and has been investigated using a variety of different standardized assessment instruments. However, infants’ performance varies depending on socioeconomic and cultural factors, which can affect the results obtained using instruments validated in different cultures, which emphasizes the need to determine the range of normality for Brazilian children, which is the objective that prompted this study.1,2,4,12
Several different studies have shown the importance of correcting gestational age, have demonstrated that there are many risk factors for abnormal development and have illustrated differences between the performance of premature infants and those born at full term. Restiffe & Gherpelli1 studied the motor development of premature
infants free from neurological sequelae using the Alberta scale and found that scores were higher using corrected
age than using chronological age for the irst 12 months
of life, leading them to recommend that corrected age be
used for the irst year. There is not, however, consensus on the subject. Some authors correct for the irst 6 or 12 months; the majority use corrected ages to the irst 2 years;
others use partial correction, i.e., take the midpoint between chronological and corrected age; and some authors question whether age correction should be used at all.4,13-15 The data
from our study show the importance of age correction up to
the acquisition of independent walking, since 90% of these
premature infants walked within the normal range for their
corrected ages, whereas only 67% did so according to their
chronological ages. This means that without age correction a high percentage of these premature infants would have had their development underestimated when they achieved independent walking (Figure 1).
This sample of premature infants achieved satisfactory motor development, since even taking their chronological ages several abilities were achieved within the expected According to the corrected age, all abilities, with the
age ranges. Allen & Alexander16 found similar results when
they studied 100 premature infants with gestational ages
of 32 weeks or less and emphasize the importance of age
correction, since according to chronological age motor
abilities were achieved 2 to 3 months later.
Age correction had the greatest impact on the results for head control. It is to be expected that very low birth weight preterms who have been kept in incubators for prolonged periods and deprived of social and environmental interaction will take longer to acquire head control.17
According to corrected ages, these premature infants acquired their motor abilities within the normal age ranges, but there was great variation between minimum and maximum ages, which suggests that for some premature infants age correction overestimates their development, whereas others acquired their motor abilities later, even with age correction. In this study there was an evident delay in acquisition of the ability to creep, however this did not have repercussions for motor development since the majority of the premature infants were able to sit and walk independent within the expected age ranges. This
inding may indicate that premature infants have a different neuromotor development proile.18
One important result of this study is the observation that small for gestational age premature infants had worse performance than appropriate for gestational age infants with
signiicant differences in the corrected acquisition ages for
the majority of the motor abilities investigated. Of particular note was the fact that, on average, small for gestational age infants crawled and walked 1 month after appropriate for gestational age premature infants. This demonstrates the deleterious effects of inadequate fetal growth on the developmental prognosis of premature infants, evident with the correction for the degree of prematurity. This is a topic of concern in the literature, although the results published to date have not been uniform.19-21
When the Bayley scales were used to assess the mental
and motor development of 36 pairs of monozygotic twins, 58% of whom were premature infants, at between 12 and 42 months’ corrected ages, no inluence from intrauterine
growth restriction was detected.22 Notwithstanding, several
different studies have shown an association between fetal and postnatal growth and neurocognitive development. A recent study showed that being small for gestational age is an independent risk factor for poor neurodevelopment
among premature infants born before 30 weeks, multiplying
their chances of developmental delays by a factor of
4.5.23 When schoolchildren who had been very low birth
weight preterms were assessed, it was observed that inadequate intrauterine growth had an effect on cognitive development, but not on motor development.24
This variation between study results is probably because of differences in patient samples, methods and follow-up duration, but, in general, the data warn that small for
gestational age premature infants have poor developmental prognosis, having been exposed to a situation of double risk: a reduced gestation period and intrauterine growth restriction.
Independent walking is the inal result of successful
gross motor development. In order to achieve this ability a child must have exercised global corporal mobility and must have had experience with kneeling and walking with support.25,26 From this perspective, our results are most
satisfactory, showing that very low birth weight preterms free from neurosensory sequelae learn to walk within the expected age range, i.e. at 12.8 months’ corrected age, whereas studies published by Gabriel et al.6 and de Jeng
et al.26 describe very low birth weight preterms walking at 13.6 and 14 months, respectively. Nevertheless, premature
infants were enrolled on those studies with greater neonatal morbidity and neurosensory sequelae.6,26
This study suffers from the limitations inherent in a descriptive study that did not investigate the perinatal and neonatal factors associated with motor ability acquisition ages and from the limitation of not including a full term control group. Nevertheless, selecting a large and homogenous sample of premature infants at low risk of motor development problems and assessing them repeatedly at short time intervals means that the data obtained can be considered to illustrate the “motor ability acquisition expectancy for very low birth weight preterms”. The study has therefore allowed us to answer the main question: what are the corrected and chronological acquisition ages for the principal motor abilities in very low birth weight preterms, in addition to demonstrating the importance of age correction up to acquisition of walking, providing useful information in the daily practice of professionals involved in infants’ healthcare.
Pediatricians and the entire healthcare team should be encouraged to accept information provided by mothers and to assess children’s motor performance during medical consultations, since doing so provides fundamental data on motor development and makes it possible to put expectations about premature infants’ motor performance
during the irst years of life into perspective.
It can be concluded that very low birth weight preterms free from neurosensory sequelae acquire their motor abilities within the normal ranges for their corrected ages. Corrected age should be used until independent walking is achieved.
acknowledgements
References
1. Restiffe AP, Gherpelli JL. Comparison of chronological and corrected ages in the gross motor assessment of low-risk
preterm infants during the irst year of life.Arq Neuropsiquiatr. 2006;64:418-25.
2. Almeida KM, Dutra MV, Mello RR, Reis AB, Martiins PS. Concurrent validity and reability of the Alberta Infant Motor Scale in premature infants. J Pediatr (Rio J). 2008;84:442-8.
3. Wilson SL, Cradock MM. Review: accounting for prematurity in developmental assessment and the use of age-adjusted scores.
J Pediatr Psychol. 2004;29:641-9.
4. Rugolo LM. Crescimento e desenvolvimento a longo prazo do prematuro extremo. J Pediatr (Rio J). 2005;81:S101-10. 5. Formiga CK, Linhares MB. Avaliação do desenvolvimento
inicial de crianças nascidas pré-termo. Rev Esc Enferm USP. 2009;43:472-80.
6. Marín Gabriel MA, Pallás Alonso CR, De La Cruz Bértolo J, Caserío Carbonero S, López Maestro M, Moral Pumarega M, et al. Age of sitting unsupported and independent walking in very low birth weight preterm infants with normal motor development at 2 years.
Acta Paediatr. 2009;98:1815-21.
7. Bobath K. Uma base neuroisiologica para o tratamento da Paralisia Cerebral. 2nd ed. São Paulo: Manole; 1990.
8. Ministério da Saúde. Secretaria de Políticas de Saúde. Saúde da criança: acompanhamento do crescimento e desenvolvimento infantil. Normas e manuais técnicos, n173. Série cadernos de atenção básica, série A. Brasília; 2002.
9. Flehmig I. Texto e atlas do desenvolvimento normal e seus desvios no lactente: diagnóstico e tratamento precoce do nascimento até o 18º mês. São Paulo: Atheneu; 2005.
10. Ballard JL, Khoury JC, Wedig K, Wang L, Eilers-Walsman BL, Lipp R. New Ballard Score, expanded to include extremely premature infants. J Pediatr. 1991;119:417-23.
11. Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstet Gynecol. 1996;87:163-8.
12. Magalhães LM, Barbosa VM, Araújo RA, Paixão ML, Figueiredo EM, Gontijo AP. Análise do desempenho de crianças pré-termo no teste de desenvolvimento de Denver nas idades de 12, 18 e 24 meses. Rev Paul Pediatr. 1999;21:330-9.
13. Siegel LS. Correction for prematurity and its consequences for the assessment of the very low birth weight infant. Child Dev. 1983;54:1176-88.
14. Lems W, Hopkins B, Samson JF. Mental and motor development in preterm infants: the issue of corrected age. Early Hum Dev. 1993;34:113-23.
15. Rugolo LM, Bentlin MR, Rugolo AJ, Dalben I, Trindade CE. Crescimento de prematuros de extremo baixo peso nos primeiros dois anos de vida. Rev Paul Pediatr. 2007;25:142-9.
16. Allen MC, Alexander GR. Using motor milestone as a multistep process to screen preterm infants for cerebral palsy. Dev Med Child Neurol. 1997;39:12-6.
17. Bonvicine C. Aquisição do controle de cabeça em lactentes nascidos pré-termo e a termo. Fisioterap Pesq. 2004;12:45-50.
18. Rosenbaum P. Variation and “abnormality”: recognizing the differences. J Pediatr. 2006;149:593-4.
19. Gutbrod T, Wolke D, Soehne B, Ohrt B, Riegel K. Effects of gestation and birth weight on the growth and development of very low birthweight small for gestational age infants: a matched group comparision. Arch Dis Child Fetal Neonatal Ed. 2000;82: F208-14.
20. Vohr BR, Wright LL, Dusick AM, Mele L, Verter J, Steichen JJ, et al. Neurodevelopmental and functional outcomes of extremely low birth weight infants in the National Institute of Child Health and
Human Development Neonatal Research Network, 1993-1994.
Pediatrics. 2000;105:1216-26.
21. Walker DM, Marlow N. Neurocognitive outcome following fetal growth restriction. Arch Dis Child Fetal Neonatal Ed. 2008;93: F322-5.
22. Reolon RK, Rotta NT, Agranonik M, Silva AA, Goldani MZ. Inluence
of intrauterine and extrauterine growth on neurodevelopmental outcome of monozygotic twins. Braz J Med Biol Res. 2008;41:694-9.
23. Kiechl-Kohlendorfer U, Raiser E, Pupp Peglow U, Reiter G, Trawöger R. Adverse neurodevelopmental outcome in preterm infants:
risk factor proiles for different gestational ages.Acta Paediatr. 2009;98:792-6.
24. Franz AR, Pohlandt F, Bode H, Mihatsch WA, Sander S, Kron M, et al. Intrauterine, early neonatal, and postdischarge growth and neurodevelopmental outcome at 5.4 years in extremely preterm infants after intensive neonatal nutritional support. Pediatrics. 2009;123:e101-9.
25. Béziers MM, Hunsinger Y. O bebê e a coordenação motora: os gestos apropriados para lidar com a criança. 2nd ed. São Paulo: Summus Editorial; 1994.
26. Jeng SF, Yau KI, Liao HF, Chen LC, Chen PS. Prognostic factors for walking attainment in very low birthweight preterm infants. Early Hum Dev. 2000;59:159-73.
Correspondence:
Sandra Cristina Pizzocaro Volpi
Faculdade de Medicina Campus de Botucatu, Universidade Estadual Paulista
Seção Técnica de Reabilitação
Tel.: +55 (14) 3811.6049, +55 (14) 3815.1207, +55 (14) 3815.2656
Fax: +55 (14) 3814.0596 E-mail: sandravolpi@uol.com.br Lígia M. S. S. Rugolo
Departamento de Pediatria/Neonatologia Tel.: +55 (14) 3811.6274