JPediatr(RioJ).2017;93(s1):75---83
www.jped.com.br
REVIEW
ARTICLE
Viral
bronchiolitis
in
young
infants:
new
perspectives
for
management
and
treatment
夽
Mauricio
T.
Caballero
a,∗,
Fernando
P.
Polack
a,
Renato
T.
Stein
baFundaciónINFANT,BuenosAires,Argentina
bPontifíciaUniversidadeCatólicadeRioGrandedoSul,CentroINFANT,PortoAlegre,RS,Brazil
Received11July2017;accepted13July2017 Availableonline30August2017
KEYWORDS
Viralbronchiolitis; Infants;
Respiratorysyncytial virus
Abstract
Objective: Theaimofthisreviewwastoaddressadvancesinmanagementandtreatmentof
acuteviralbronchiolitisininfants.
Sources: A systematic review search was made including all articles published in English
between2010and2017,andavailableintheelectronicdatabasesPubMedandCochrane Cen-tralRegisterofControlledTrials(CENTRAL)andspecializedregisteroftheAcuteRespiratory InfectionsGroup(Cochranereviewgroup).ThefollowingMESHtermsinEnglishwereincluded, usingdifferentBooleanoperatorsforthesearchstrategy:‘‘bronchiolitis,viral,’’‘‘diagnosis,’’ ‘‘epidemiology,’’‘‘etiology,’’‘‘therapy,’’‘‘virology,’’‘‘preventionandcontrol,’’‘‘respiratory syncytialvirus,human.’’Additionalfilterswereused.
Summaryoffindings: Few effectiveinterventions arerecommendedfor themanagementof
RSVbronchiolitisinyounginfants.Themaingoalistoensureanadequateoxygen supplemen-tationandfluidbalancewheneverdeemednecessary.Hypertonicsalinenebulizationishelpful onlyforhospitalizedinfants.NumerousantiviraldrugsandspecificvaccinesforRSVareunder evaluationandforetelladvancesindiseasemanagementinthenearfuture.
Conclusion: A number of promisingnew technologies areadvancingin thefield. Untilnew
interventionsbecamefeasible,earlydetectionandmodificationofpreventableriskfactorsis essentialtoimproveoutcomes.
©2017SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/ 4.0/).
夽
Pleasecitethisarticleas:CaballeroMT,PolackFP,SteinRT.Viralbronchiolitisinyounginfants:newperspectivesformanagementand
treatment.JPediatr(RioJ).2017;93:75---83.
∗Correspondingauthor.
E-mail:mcaballero@infant.org.ar(M.T.Caballero).
http://dx.doi.org/10.1016/j.jped.2017.07.003
76 CaballeroMTetal.
PALAVRAS-CHAVE
Bronquioliteviral; Neonatos; Vírussincicial respiratório
Bronquioliteviralemneonatosjovens:novasperspectivasparamanejoetratamento
Resumo
Objetivo: Oobjetivodestaanáliseéabordaravanc¸osnomanejoenotratamentode
bronquio-liteviralagudaemneonatos.
Fontes: Umapesquisadeanálisesistemáticafoirealizadaeincluiutodososartigospublicados
eminglêsentre2010e2017edisponíveisnasbasesdedadoseletrônicasPubMed,noRegistro CentraldeEnsaiosControlados(CENTRAL)daCochraneenoregistroespecializadodoGrupode Infecc¸õesRespiratóriasAgudas(grupoderevisãoCochrane).OsseguintestermosMESHeminglês foramincluídosnaabordagemutilizandodiferentesoperadoresbooleanosparaaestratégiade pesquisa: ‘‘bronquiolite,viral’’, ‘‘diagnóstico’’,‘‘epidemiologia’’, ‘‘etiologia’’, ‘‘terapia’’, ‘‘virologia’’,‘‘prevenc¸ãoecontrole’’,‘‘vírussincicialrespiratório,humano’’.Foramutilizados filtrosadicionais.
Resumodosachados: Poucasintervenc¸õesefetivassãorecomendadasparaomanejoda
bron-quioliteporVSRemneonatosjovens. Oprincipalobjetivoégarantirumasuplementac¸ãode oxigênioadequadaeequilíbriodefluidossemprequeconsideradonecessário.Anebulizac¸ãode soluc¸ãosalinahipertônicaajudaapenasemcasosdeneonatoshospitalizados.Vários medica-mentos antivirais e vacinasespecíficas contraVSR estão em fase de avaliac¸ão e predizem avanc¸osnomanejodadoenc¸anofuturopróximo.
Conclusão: Váriasnovastecnologiaspromissorasestãoavanc¸andonocampo.Atéqueasnovas
intervenc¸ões setornem viáveis,adetecc¸ão precoceeamodificac¸ão defatores deriscode prevenc¸ãosãofundamentaisparamelhorarosresultados.
©2017SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Este ´eumartigo OpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4. 0/).
Introduction
Respiratory syncytial virus (RSV) bronchiolitis is the most frequentcauseoflowerrespiratorytractillness(LRTI)and hospitalizationinyoung infants worldwide.1,2 This disease
isassociatedwithupto199,000deathseveryyear in chil-dren undertheage of 5years,and approximatelymillion hospitalizationsannually.1---4 Ofthesedeaths,99% occurin
developingcountries.1In developedcountries,RSVdeaths
are infrequent and associated with chronic lung disease, neuromusculardisorders,heartdisease,Down’ssyndrome, andpretermbirth.5Bytheageof2years,over95%ofthe
childrenhavebeeninfectedbythevirus.6
AcuteRSVbronchiolitisisaseasonaldisease,whichoften startseveryyearbetweenfallandspring,andpeaksin win-ter.Thetropicsaretheexception,andthereisnospecific seasonalityin theseregions,although someepidemicsare hypothesizedtobeassociatedwiththerainyseason.2RSV
infection is typically mild and begins with upper respira-torytractsigns,mimicking acommoncold.7,8After afew
days, some patients will progress to experience disease affectingthedistalbronchioles,withclinicalsignsof tachyp-nea,wheezing,crackles,rhonchus,andchestretractions.7,9
Approximately 1---3% of infected children develop feeding difficulties, apnea, or are unable to maintain adequate oxygensaturation (SpO2), requiring hospitaladmission for supportive therapy.2,4,10 A small number of infants,
espe-ciallythosewithco-morbidities,willprogresstorespiratory failureordeath.1,2,5Thereareseveralstudiessuggestingan
associationbetweenseverebronchiolitisbyRSVand recur-rentwheezing,anassociationthatdisappearsbytheendof thefirstdecadeoflife.11---13WithgreaterfrequencythanRSV,
rhinoviruses,whencombinedwithearlylifeatopic sensitiza-tion,areassociatedwithasthma.14 In2009,thetotalcost
forhospitalizationsduetobronchiolitisintheUnitedStates wasclosetotwobilliondollars. Althoughtrends in hospi-talizationsratesintheUShavedeclinedbetween2000and 2009,costshaveraisedattheexpenseofincreaseduseof intensivecareforhigh-riskpatients.15Despiteitshigh
mor-bidity,theeconomicexpenses,concerningmortalityratesin developingcountries,andtheassociationofRSVwith tran-sientlungsequelae(e.g.,recurrentwheezing),treatmentof RSVLRTIisstillsymptomaticandhassignificantgaps. More-over,overfiftyyearsafteritsdiscovery,nolicensedvaccine againstRSVisavailable. Palivizumab,aneffective human-izedmonoclonalantibody(mAb)againsttheRSVfusion(F) protein,isavailable forpreterminfants,infantswithBPD, andinfants withcyanoticcongenitalheartdisease.16 Even
though palivizumab significantly reducessevere RSV LRTI, thedrugisexpensiveandrequiresseveraldoses,limitingits use inindustrialized anddeveloping countries.Therefore, safeandinexpensivevaccinesandtreatmentsareurgently neededtodecreasetheimpactofRSVinchildren.
Sources
Viralbronchiolitisinyounginfants 77
in English were included in the approach using differ-ent Boolean operators in PubMed: ‘‘bronchiolitis, viral,’’ ‘‘diagnosis,’’ ‘‘epidemiology,’’ ‘‘etiology,’’ ‘‘therapy,’’ ‘‘virology,’’ ‘‘prevention and control,’’ ‘‘respiratory syn-cytial virus, human’’. Additional filters were used: ages between1and23months,andstudymethodology(clinical trial,comparativestudy,controlledclinicaltrial,guideline, meta-analysis, practice guideline, randomized controlled trial, and systematic reviews). In addition, studies were searchedintheCochranelibrary,followingspecialized reg-ister in ‘Acute Respiratory Infections Group,’ topic‘child health,’ ‘lung and airways, respiratory infections: bron-chiolitis and respiratory syncytial virus.’ MESH terms for CENTRALsearchwere‘‘respiratorysyncytialvirus,human’’ and‘‘bronchiolitis,viral.’’
AsearchwasmadeinClinicalTrials.govtofindnew vac-cines, antibodies, and antivirals technologies against RSV infection.Forthisaim,termsinEnglishwereincluded,such as‘‘respiratorysyncytialvirusinfections,’’filteredbystudy status(active,recruiting,notyetrecruiting,enrolling), eli-gibility criteria(child andpregnant adult), interventional studytype,andstudyphase(1---3).
Summary
of
findings
Diagnosisandmonitoring
There is no widely validated score for RSV LRTI severity. A thorough and physical exam is critical for the initial assessmentofpatients.Evidenceofinadequatefeedingor fluid intake, history of apnea, lethargy, or moderate to severerespiratorydistress(nasalflaring,tachypnea, grunt-ing,retractionsorcyanosis),and/oranSpO2≤92%inroom air(cutoffsforacceptableSpO2varypercountry),warrant hospitalization,ideallyinasecondarycarelevelhospital.8,17
ThepathogenesisofacuterespiratoryfailureinRSV bron-chiolitisischaracterizedbyobstructionofthesmallairways, increased airways resistance, alveolar atelectasis, muscle fatigue,andhypoxemiaduetomismatchbetween ventila-tionandperfusion.18Therefore,pediatricintensivecareunit
(PICU)admissionshouldbeconsideredinpatientspresenting withclinicalsignsofexhaustion,markersofacute respira-toryfailure(definedasPaO2/FiO2≤300mmHg),orsignsof apnea.2,8,17,18
Oxygensaturation
One of the main concerns during severe RSV LRTI is an inadequateoxygensupplytothetissues(hypoxemia).8The
arterialoxygen contentthatis distributedthroughtissues canbemeasuredthrougharterialoxygensaturation(SaO2), whichrepresentsaratiobetweenoxyhemoglobin concentra-tionandtotalhemoglobinconcentration.8Themostwidely
used tool to assess SaO2 is pulse oximetry (SpO2), since it is a noninvasive technique.8 Despite its frequent use,
SpO2 is knowntopresent a variabilityof ±2%.8,17,19 Moni-toringoxygensaturationisnotrecommendedinoutpatients whose clinical and feeding status are adequate, because thisinterventioncouldpotentiallyinduceunnecessary hos-pital admissions. Since the cutoff criteria for SpO2 tend to differ between studies and between clinical practice
guidelines,a good clinical evaluation is important in the decision process.8,19 The AmericanAcademy of Pediatrics
(AAP)recommendsaSpO2of90%asalimitforthe adminis-trationof supplemental oxygen.19 Inthe absenceof clear
evidence about SpO2 levels to predict the progression of bronchiolitis,the Committee of the National Institute for Health and Care Excellence (NICE), determined a SpO2 of92% asthe cutofffor supplementation.8 Other factors,
includingathoroughclinicalevaluationandanassessment oflivingconditionsandsocialriskfactors,shouldalso con-tributetothedecision-makingprocess.
Blood gas testing is not routinely indicated for hos-pitalized patients, and it is not helpful in the routine management of viral bronchiolitis. The exception is for patients withsigns of respiratory exhaustion, apnea, and unabletomaintainanadequateSpO2levelsdespite supple-mentaloxygenuse.8
Etiologicaltesting
Etiologic diagnosis is common during clinical practice at hospitals,andthenorminepidemiologicalstudies.20While
virus-specifictherapiesarenotyetavailable,virus identifi-cationmayhelpreducetheuseof antibiotics.17 Real-time
protein chain reaction (qPCR) is the gold standard for diagnosis, although its costs, particularly in developing countries,hinderitsroutineuse.17,19,21Immunofluorescence
ischeaper,withverygoodsensitivityforRSVinparticular, butitisoperator-dependent.17Whilethereisnogood
rea-sontoobtainbloodculturesorleukocytecountsinpatients withacutebronchiolitis,bacterialinfectionshouldbe inves-tigated in those with signs of sepsis or pneumonia.2,19
Bacterial sepsis in young infants with viral bronchiolitis, particularlyepisodestriggeredbyGram-positivecocci,has been associatedwithan increased risk of deathin devel-opingcountries.2Chestradiographycouldbeconsideredin
patientswithimpedingrespiratoryfailure.8,19,22
Suggested
management
Respiratorysupportivecare
SixguidelinesandtenCochranedatabasesystematicreviews were analyzed to summarize the recommended manage-mentinacuteviralbronchiolitis(Table1).8,19,21---34Overall,
fewtreatment interventionsaresuggested for bronchioli-tis,andthemaingoalduringacuteillnessistoachievean adequatefluidbalanceandnormaloxygensaturationlevels (Table1).Infantswithviralbronchiolitispresentincreased mucusproduction,epithelialdebrisinvadingthebronchiolar lumen,peribronchiolaredema,andleukocyteinfiltration.In addition,smallairwaysandalveolarsacsindevelopmentare morepronetocollapse,generatingaventilation/perfusion imbalancethatoftenleadstohypoxemiaand,inadvanced stages, to hypercapnia.18 Therefore, when SpO
2 is below 90---92%, supplemental oxygen should be administrated to increase oxyhemoglobin levels.8,17 Several oxygen
78
Caballero
MT
et
al.
Table1 Bronchiolitismanagementrecommendationsbasedonguidelines.
Typeofintervention NICE8 AAP19 Spanish17 Finnish23 CanadianPaediatric
Society21
Italianintersociety22
Supplementaloxygen IfSpO2is<92% Ifoxyhemoglobin saturation<90%
Iftheinfanthave severerespiratory difficulty,cyanosisor SpO2<92%
Notevaluated IfSpO2<90% IfSpO2<90%at ambientair conditions
Fluidadministration Enteralfluids administration (nasogastricor orogastric)if inadequateoral intake.Isotonic intravenousfluid supportifRF.
Nasogastricor intravenousfluids administrationfor infantswith inadequateoral hydration.
Feedingby nasogastrictubeif riskofdehydrationor progressive
respiratory difficulties.
Intravenoushydration ifRF.
Notevaluated Ifrespiratoryrate>60 b/m,nasogastric feedsshouldbe given.Isotonic intravenousfluid supportisequal effectiveinLOS.
Nasogastricor intravenousfluids administrationfor infantswith moderatetosevere bronchiolitis.
Upperairway suctioning
Considerinpatients withrespiratory distressorfeeding difficulties. Recommendedin patientswithapnea.
Insufficientevidence. Aspirationof secretionsbefore feedsandwhensigns ofobstructionare detected.
Notevaluated Insufficientevidence. Ifitisperformed,it shouldbedone superficiallyand regularly.
Superficialaspiration.
Chestphysiotherapy Considerinpatients withcomorbidities andimminentRF.
Notrecommended Notrecommended Notevaluated Notrecommended Notrecommended
Positiveairway pressure(CPAP)
ConsidertoavoidRF Notevaluated IfRF,hypercapniaor recurrentapnea.
Notevaluated Notevaluated Notevaluated
Inhaled-agonist Notrecommended Notrecommended Notrecommended. Therapeutictest,if responsecontinuing treatment.
Notrecommended Notrecommended Considerasingle therapeutictrialin infantswithafamily historyofallergy, asthmaoratopy. Inhaledadrenaline Notrecommended Notrecommended Notrecommended Notrecommended Insufficientevidence Notrecommended Systemic
corticosteroids
Notrecommended Notrecommended Notrecommended Notrecommended Notrecommended Notrecommended
Inhaled corticosteroids
V
iral
bronchiolitis
in
young
infants
79
Table1(Continued)
Typeofintervention NICE8 AAP19 Spanish17 Finnish23 CanadianPaediatric
Society21
Italianintersociety22
Nebulizedhypertonic salinesolution
Notrecommended Considerjustin infantshospitalized.
Recommendedin hospitalizedinfants.
CouldreduceLOS Nebulized3%saline couldbehelpfulin theinpatientwith longerLOS.No recommendin outpatients.
Recommended.It improvesclinical scoreandLOS.
Antibiotics Notrecommended Ifthereisaconfirmed bacterialinfection,or considerifthereisa strongsuspicion.
Inseverebronchiolitis requiringmechanical ventilation,altered bloodcount,CRP,or PCT.
Notevaluated Notrecommended Ifdocumented bacterialinfectionby cultureormolecular testorICUadmission.
Helioxinhalation Notrecommended Notevaluated Insufficientevidence Notevaluated Notevaluated Notevaluated Highflownasal
cannulainhalation
Insufficientevidence Notevaluated Insufficientevidence Insufficientevidence Notevaluated Insufficientevidence
Antileukotriene Notrecommended Notevaluated Notrecommended Notevaluated Notevaluated Notrecommended Nebulized
deoxyribonuclease
Notevaluated Notevaluated Notrecommended Notevaluated Notevaluated Notrecommended
Surfactanttherapy Notevaluated Notevaluated Insufficientevidence Notevaluated Notevaluated Notevaluated Ribavirin Notevaluated Notevaluated Notrecommended.
Considerin immuno-compromised.
Notevaluated Notrecommended Notrecommended
Ipratropiumbromide Notrecommended Notevaluated Notrecommended Notevaluated Notevaluated Notevaluated
NICE,NationalInstituteforHealthandCareExcellence;AAP,AmericanAcademyofPediatrics;SpO2,oxygensaturation;CPAP,continuouspositiveairwaypressure;RF,riskfactor;CRP,
80 CaballeroMTetal.
improving the ventilation/perfusion ratio. Despite these potentialbenefits,HFNCwasnotsuperiortostandard oxy-gen supplementation when the main outcome was time on/offsupplementaloxygen,timetodischarge,andlength of stay.31 Continuous positive airwaypressure (CPAP) is a
non-invasivemechanicalventilationthat improvesairways resistance,reducing theimpactof atelectasisby distend-ing bronchial/bronchiolar lumen diameter. Patients with worsening and severe acute bronchiolitis despite oxygen supplementationmaybenefitfromCPAP.17
Fluidadministration
Maintenanceofgoodoral hydrationand breastfeedingare crucialmeasuresinthemanagementofbronchiolitis. Never-theless,ifahospitalizedinfantcannotreceiveoralfeedings due toa high respiratory rate (>60breaths/min), a naso-gastric tube can be placed to restore adequate feeding andhydration.8,17,19,21,22Althoughintravenousisotonicfluids
administrationdoesnotappeartobebetterthan nasogas-trichydration,itisusedinpatientsadmittedtoPICU,those withclinical signs of exhaustion, and those intolerant to nasogastrictubefeeding.8,17,19,21,22
Bronchodilatorsandinhaledsteroids
Noevidence supports the administrationof systemic cor-ticosteroids and/or inhaled -agonist and/or epinephrine for the treatment of hospitalized patients with viral bronchiolitis.8,17,19,21---24Nevertheless,both theSpanishand
Italianguidelinesconsiderthatinhaled-agonistscouldbe tried once at the beginning of treatment, especially if a patienthasapersonalorfamilyhistoryofatopy,asthma,or eczema.17,22Somestudieshavesuggestedapotential
bene-fitwhenepinephrinewasusedinchildreninanemergency roomsetting,loweringtheriskofhospitaladmission.24
How-ever,theobservedclinicalimpactisverymodest,andthe patients’lengthofhospitalstayanddaysonoxygen supple-mentationwerenotsignificantlyaffected.
Hypertonicsaline
Nebulizedhypertonicsalinesolutionhasosmoticproperties andproven effectivenessin patientswithCOPDandcystic fibrosis.35 This intervention improves airway clearanceby
reducingairwayedema,mucusproduction,andrehydrating theairwaysurfaceliquid.36 Recent studiesandsystematic
reviews suggest that nebulized hypertonic saline may be beneficialonlytoinfantsalreadyhospitalized,butitsimpact inpreventingadmissionsispoor.17,19,21---23
Antibiotics
The misuse of antibiotics in patients with viral bronchi-olitisis often observed in clinical practice. Although it is sometimes difficult todistinguish between viral and bac-terialinfections through clinical and radiological criteria, infantswithRSVLRTIareonlyexceptionallyco-infectedand needantibiotics.8,17,19Childrenwhoprogresstosevere
dis-ease with respiratory failure areadmitted to a PICU and
willlikely receiveempiricantibiotic therapy for bacterial co-infections.2,17,19,22,37,38
Newtreatmentperspectives
To date, no effective and accessible treatments for RSV bronchiolitis are available. Recent experimental trials in adults yielded encouraging results with novel candi-date antivirals.Intwoseparate sophisticatedstudies, the administration of fusion inhibiting and nucleoside analog formulations improved respiratory symptoms when com-paredwithplacebo.39,40However,inthesecontrolled,early
studies,thedrugswereadministratedsimultaneouslywith experimentalinoculation.Therefore,theyactedagainstRSV beforeanyobservablesignsandsymptoms.Whethera sim-ilar benefit will be observed in infants when treatment is initiated days later, upon presentation to the hospital, remainsunclear.
Theadministrationofpalivizumabinspecificriskgroups islimitedbyitsexpensivecostinmanylowtomiddleincome countries.16ConsequentlypreventionofRSVLRTIisapublic
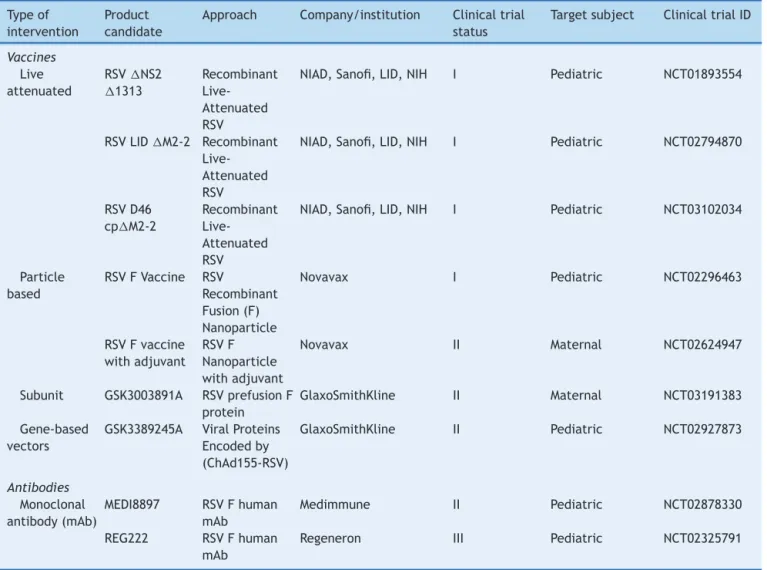
healthpriority,andglobalinitiativeshaveadvanced numer-ouseffortstoexpandthefield(Table2).
Vaccines
The development of RSVvaccines is challenging. The his-tory ofenhancedrespiratorysyncytialvirus disease(ERD), the need to immunize in early life, and the possible interference by natural maternal antibodies complicates immunizationstrategies.41 Asuitablevaccine must ideally
generate protective antibodies in infants younger than 2 monthsofage,whorepresentthegroupatgreaterrisk of hospitalizations.1---3 Six different formulations of RSV
can-didatevaccinesarebeingtestedin preclinicalandclinical studies: live attenuated or chimeric, whole inactivated, particlebased,subunit,nucleicacid,andgenebased vec-tors (Table 2).42 Furthermore, passive protection through
administrationofmonoclonalantibodiesofprolonged half-lifeinearlyliferepresentsanattractivealternativeunder evaluation.43
Althoughpalivizumab reducessevere RSV infections by 55%, its administration is cumbersome and the drug is expensive.16,43 Therefore, its use is restricted to
popula-tions at high risk for severe disease.16 A new monoclonal
antibodyagainstthepre-fusionconformationofRSVF pro-tein(MEDI8897)hasanextendedhalf-lifeandhigherpotency (allowingasingleintramusculardose),andisanattractive potentialalternative for thefuture.43,44 Other similar
for-mulationsarealsounderevaluation.45
Otherperspectives
Viralbronchiolitisinyounginfants 81
Table2 Newvaccinesandantibodiescurrentlybeingtested.
Typeof intervention
Product candidate
Approach Company/institution Clinicaltrial status
Targetsubject ClinicaltrialID
Vaccines
Live attenuated
RSVNS2 1313
Recombinant Live-Attenuated RSV
NIAD,Sanofi,LID,NIH I Pediatric NCT01893554
RSVLIDM2-2 Recombinant Live-Attenuated RSV
NIAD,Sanofi,LID,NIH I Pediatric NCT02794870
RSVD46 cpM2-2
Recombinant Live-Attenuated RSV
NIAD,Sanofi,LID,NIH I Pediatric NCT03102034
Particle based
RSVFVaccine RSV
Recombinant Fusion(F) Nanoparticle
Novavax I Pediatric NCT02296463
RSVFvaccine withadjuvant
RSVF Nanoparticle withadjuvant
Novavax II Maternal NCT02624947
Subunit GSK3003891A RSVprefusionF protein
GlaxoSmithKline II Maternal NCT03191383
Gene-based vectors
GSK3389245A ViralProteins Encodedby (ChAd155-RSV)
GlaxoSmithKline II Pediatric NCT02927873
Antibodies
Monoclonal antibody(mAb)
MEDI8897 RSVFhuman mAb
Medimmune II Pediatric NCT02878330
REG222 RSVFhuman mAb
Regeneron III Pediatric NCT02325791
RSV,respiratorysyncytialvirus.
publichealthaction.Humanmilkisabonafide,inexpensive intervention of excellent effectivenessfor all infants and shouldalsocomplementpalivizumabinhighriskinfants.47
Other dietary and habit interventions that have been associatedwithsevereLRTIincludeahighintakeof carbohy-dratesoralcoholduringthelasttrimesterofpregnancy.4,48
Reducingalcoholandexposuretotobaccosmokeduringand afterpregnancywillbenefitnotonlythebaby,butalsothe mother.
Other studies suggest that TLR4 heterozygosity (Asp299Gly, rs4986790) and urban habits may explain a poor response to palivizumab in preterm infants, and promotesevere RSV LRTIina subgroup ofterm infantsin the community.49,50 It remains to be seen whether these
infants will respond adequately to new generation mAbs andtransplacentalimmunity.
Conclusion
RSVbronchiolitisisthemaincauseofinfanthospitalization worldwide, and an important cause of death in develop-ing countries.1 A number of promising new technologies
areadvancinginthefield.Untilnewinterventionsbecame
feasible, early detection and modification of preventable riskfactorsisessentialtoimproveoutcomes.Pediatricians, families, and public health officials should contribute to theseeffortsthroughindividualactions(e.g.,smoking ces-sation)andbyaddressingmodifiableriskfactorsforsevere disease,whileprovidingthebestpossiblemedicalcare.
Conflicts
of
interest
MTCdeclaresno conflictsofinterest, FPP served in Advi-soryBoardsatPfizer,Janssen,Novavax,BavarianNordicand Sanofi,andRTSwasaspeakerforAbbvie.
References
1.NairH,NokesDJ,GessnerBD,DheraniM,MadhiSA,Singleton RJ,etal.Globalburdenofacutelowerrespiratoryinfections duetorespiratorysyncytialvirusinyoungchildren:asystematic reviewandmeta-analysis.Lancet.2010;375:1545---55. 2.Geoghegan S, Erviti A, Caballero MT, Vallone F, Zanone
82 CaballeroMTetal.
3.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboy-ans V,et al. Global and regional mortalityfrom 235causes of death for 20 age groups in 1990 and 2010: a systematic analysisfortheGlobalBurdenofDiseaseStudy2010.Lancet. 2012;380:2095---128.
4.Ferolla FM, Hijano DR, Acosta PL, Rodriguez A, Duenas K, Sancilio A, et al. Macronutrients duringpregnancy and life-threatening respiratorysyncytial virusinfections inchildren. AmJRespirCritCareMed.2013;187:983---90.
5.ByingtonCL,WilkesJ,KorgenskiK,ShengX.Respiratory syncy-tialvirus-associatedmortalityinhospitalizedinfantsandyoung children.Pediatrics.2015;135:e24---31.
6.GlezenWP,TaberLH,FrankAL,KaselJA.Riskofprimary infec-tionandreinfectionwithrespiratorysyncytialvirus.AmJDis Child.1986;140:543---6.
7.ThompsonM,VodickaTA,BlairPS,BuckleyDI,HeneghanC,Hay AD,etal.Durationofsymptomsofrespiratorytractinfections inchildren:systematicreview.BMJ.2013;347:f7027.
8.NationalInstituteforHealthCareandExcellence.Bronchiolitis:
diagnosisandmanagementofbronchiolitisinchildren.Clinical,
June2015,guidelinen◦9.
9.HalasaN,WilliamsJ,FaouriS,ShehabiA,VermundSH,Wang L,etal.Naturalhistoryandepidemiologyofrespiratory syncy-tialvirusinfectionintheMiddleEast:hospitalsurveillancefor childrenunderagetwoinJordan.Vaccine.2015;33:6479---87. 10.Hall CB, Weinberg GA, BlumkinAK, Edwards KM, Staat MA,
SchultzAF,etal.Respiratorysyncytialvirus-associated hospital-izationsamongchildrenlessthan24monthsofage.Pediatrics. 2013;132:e341---8.
11.Blanken MO, Rovers MM, Molenaar JM, Winkler-Seinstra PL, Meijer A, Kimpen JL, et al. Respiratory syncytial virus and recurrentwheezein healthypreterminfants. NEngl JMed. 2013;368:1791---9.
12.MochizukiH,KusudaS,OkadaK,YoshiharaS,FuruyaH,Simoes EA.Palivizumabprophylaxisinpreterminfantsandsubsequent recurrentwheezing:six-yearfollowupstudy.AmJRespirCrit CareMed.2017;196:29---38.
13.SteinRT,SherrillD,MorganWJ,HolbergCJ,HalonenM,Taussig LM,et al.Respiratorysyncytial virusinearlylifeandriskof wheezeandallergybyage13years.Lancet.1999;354:541---5. 14.JacksonDJ,EvansMD,GangnonRE,TislerCJ,PappasTE,Lee
WM,etal.Evidenceforacausalrelationshipbetweenallergic sensitizationandrhinoviruswheezinginearlylife.AmJRespir CritCareMed.2012;185:281---5.
15.HasegawaK,TsugawaY,BrownDF,MansbachJM,CamargoCA Jr.TrendsinbronchiolitishospitalizationsintheUnitedStates, 2000---2009.Pediatrics.2013;132:28---36.
16.American Academy ofPediatricsCommittee onInfectious D, American Academy of Pediatrics. Bronchiolitis Guidelines C. Updated guidancefor palivizumabprophylaxisamonginfants andyoungchildrenatincreasedriskofhospitalizationfor respi-ratorysyncytialvirusinfection.Pediatrics.2014;134:e620---38. 17.Working Group of the Clinical Practice Guideline on Acute
Bronchiolitis.QualityplanfortheSpanishnationalhealthcare systemoftheSpanishMinistryforHealthandSocialPolicy; Cata-lan Agencyfor Health Technology Assessment; 2010.Clinical PracticeGuidelinesintheSpanishNationalHealthcareSystem: CAHTAno.2007/05.
18.Lopez-FernandezY,AzagraAM,delaOlivaP,ModestoV,Sanchez JI, Parrilla J, et al. Pediatric Acute Lung Injury Epidemiol-ogyandNaturalHistorystudy:incidenceand outcomeofthe acuterespiratorydistresssyndromeinchildren.CritCareMed. 2012;40:3238---45.
19.RalstonSL,LieberthalAS,MeissnerHC,AlversonBK,BaleyJE, GadomskiAM, et al. Clinicalpractice guideline: the diagno-sis, management,and preventionofbronchiolitis.Pediatrics. 2014;134:e1474---502.
20.ZanoneSM,KrauseLK,MadhiSA,BassatQ,JhaP,SimoesEA, etal.ChallengesinestimatingRSV-associatedmortalityrates. LancetRespirMed.2016;4:345---7.
21.FriedmanJN,RiederMJ,WaltonJM,CanadianPaediatricSociety ACCDT, Hazardous SubstancesC.Bronchiolitis: recommenda-tionsfordiagnosis,monitoringandmanagementofchildrenone to24monthsofage.PaediatrChildHealth.2014;19:485---98. 22.BaraldiE,LanariM,ManzoniP,RossiGA,VandiniS,RiminiA,
etal.Inter-societyconsensusdocumentontreatmentand pre-ventionofbronchiolitisinnewbornsandinfants.ItalJPediatr. 2014;40:65.
23.TapiainenT,AittoniemiJ,ImmonenJ,JylkkaH,MeinanderT, NuolivirtaK,etal.Finnishguidelinesforthetreatmentof laryn-gitis,wheezing bronchitisand bronchiolitis inchildren. Acta Paediatr.2016;105:44---9.
24.HartlingL,BialyLM,VandermeerB,TjosvoldL,JohnsonDW, PlintAC,etal.Epinephrineforbronchiolitis.CochraneDatabase SystRev.2011:CD003123.
25.FernandesRM,BialyLM,VandermeerB,TjosvoldL, PlintAC, Patel H, et al. Glucocorticoids for acute viral bronchiolitis in infants and young children. Cochrane Database Syst Rev. 2013:CD004878.
26.LiuF, Ouyang J, Sharma AN, LiuS, Yang B, XiongW, et al. Leukotrieneinhibitorsforbronchiolitisininfantsandyoung chil-dren.CochraneDatabaseSystRev.2015:CD010636.
27.EnriquezA,ChuIW,MellisC,LinWY.Nebulised deoxyribonucle-aseforviralbronchiolitisinchildrenyoungerthan24months. CochraneDatabaseSystRev.2012;11:CD008395.
28.UmorenR,OdeyF,MeremikwuMM.Steaminhalationor humidi-fiedoxygenforacutebronchiolitisinchildrenuptothreeyears ofage.CochraneDatabaseSystRev.2011:CD006435.
29.ZhangL, Mendoza-SassiRA, WainwrightC,Klassen TP. Nebu-lisedhypertonicsalinesolutionforacutebronchiolitisininfants. CochraneDatabaseSystRev.2013:CD006458.
30.VentreK,Haroon M,DavisonC.Surfactanttherapy for bron-chiolitisin critically ill infants.Cochrane DatabaseSyst Rev. 2006:CD005150.
31.Beggs S,Wong ZH,Kaul S, Ogden KJ,Walters JA. High-flow nasalcannulatherapyforinfantswithbronchiolitis.Cochrane DatabaseSystRev.2014:CD009609.
32.FarleyR,SpurlingGK,ErikssonL, DelMarCB.Antibioticsfor bronchiolitis in children under two years of age. Cochrane DatabaseSystRev.2014:CD005189.
33.RoqueiFigulsM,Gine-GarrigaM,GranadosRugelesC,Perrotta C,VilaroJ.Chestphysiotherapyforacutebronchiolitisin paedi-atricpatientsbetween0and24monthsold.CochraneDatabase SystRev.2016;2:CD004873.
34.LietJM,DucruetT,GuptaV,CambonieG.Helioxinhalation ther-apyfor bronchiolitis ininfants. CochraneDatabaseSyst Rev. 2015:CD006915.
35.WarkPA,McDonaldV,JonesAP.Nebulisedhypertonicsalinefor cysticfibrosis.CochraneDatabaseSystRev.2005:CD001506. 36.DaviskasE,AndersonSD,GondaI,EberlS,MeikleS,SealeJP,
etal.Inhalationofhypertonicsalineaerosolenhances mucocil-iaryclearanceinasthmaticandhealthysubjects.EurRespirJ. 1996;9:725---32.
37.SilvaFilho LV, Pinto LA, SteinRT. Use ofmacrolides in lung diseases: recent literature controversies. J Pediatr (Rio J). 2015;91:S52---60.
38.BeigelmanA,Isaacson-SchmidM,SajolG,BatyJ,RodriguezOM, LeegeE, et al. Randomized trialto evaluate azithromycin’s effectson serumand upperairway IL-8levelsand recurrent wheezingininfantswithrespiratorysyncytialvirus bronchioli-tis.JAllergyClinImmunol.2015;135,1171---8e1.
Viralbronchiolitisinyounginfants 83
40.DeVincenzoJP,WhitleyRJ,MackmanRL,Scaglioni-WeinlichC, HarrisonL,FarrellE,etal.OralGS-5806activityinarespiratory syncytialviruschallengestudy.NEnglJMed.2014;371:711---22. 41.PolackFP.Thechanginglandscapeofrespiratorysyncytialvirus.
Vaccine.2015;33:6473---8.
42.PATH. RSV vaccine and mAb snapshot. Available from:
http://www.path.org/vaccineresources/details.php?i=1562
[cited03.03.17].
43.ZhuQ,McLellanJS,KallewaardNL,UlbrandtND,PalaszynskiS, ZhangJ,etal.Ahighlypotentextendedhalf-lifeantibodyasa potentialRSVvaccinesurrogateforallinfants.SciTranslMed. 2017;9,pii:eaaj1928.
44.Mazur NI, Martinon-Torres F, Baraldi E, Fauroux B, Gree-nough A, Heikkinen T, et al. Lower respiratory tract infectioncausedbyrespiratorysyncytialvirus: current man-agement and new therapeutics. Lancet RespirMed. 2015;3: 888---900.
45.Reichert JM. Antibodies to watch in 2016. MAbs. 2016; 8:197---204.
46.LibsterR,BugnaHortonedaJ,LahamFR,CasellasJM,IsraeleV, PolackNR,etal.Breastfeedingpreventsseverediseaseinfull termfemaleinfantswithacuterespiratoryinfection.Pediatr InfectDisJ.2009;28:131---4.
47.KleinMI,BergelE,GibbonsL,CovielloS,BauerG,BenitezA, etal.Differentialgenderresponsetorespiratoryinfectionsand totheprotectiveeffectofbreastmilkinpreterminfants. Pedi-atrics.2008;121:e1510---6.
48.LibsterR, FerollaFM, HijanoDR,AcostaPL,Erviti A, Polack FP,etal.Alcoholduringpregnancyworsensacuterespiratory infectionsinchildren.ActaPaediatr.2015;104:e494---9.
49.Caballero MT, Serra ME, Acosta PL, Marzec J, Gibbons L, SalimM, etal. TLR4genotype and environmentalLPS medi-ateRSVbronchiolitisthrough Th2polarization.JClinInvest. 2015;125:571---82.