www.revportcardiol.org
Revista
Portuguesa
de
Cardiologia
Portuguese
Journal
of
Cardiology
ORIGINAL
ARTICLE
Protocol-based
follow-up
program
for
heart
failure
patients:
Impact
on
prognosis
and
quality
of
life
João
R.
Agostinho
a,∗,
Inês
Gonc
¸alves
a,
Joana
Rigueira
a,
Inês
Aguiar-Ricardo
a,
Afonso
Nunes-Ferreira
a,
Rafael
Santos
a,
Tatiana
Guimarães
a,
Pedro
Alves
b,
Nelson
Cunha
a,
Tiago
Rodrigues
a,
N´
Zinga
André
a,
Mónica
Pedro
a,
Fátima
Veiga
a,
Fausto
J.
Pinto
a,
Dulce
Brito
a,
for
the
RICA-HFteam
Investigators
aServic¸odeCardiologia,DepartamentodeCorac¸ãoeVasos,HospitaldeSantaMaria,CentroHospitalarUniversitáriodeLisboa
Norte,E.P.E.,CCUL,CentroAcadémicodeMedicinadeLisboa,FaculdadedeMedicina,UniversidadedeLisboa,Portugal
bFaculdadedeMedicina,UniversidadedeLisboa,Portugal
Received22June2018;accepted31March2019 Availableonline28January2020
KEYWORDS Heartfailure; Follow-upprogram; Readmission; Mortality Abstract
Introduction:Heartfailureisassociatedwithhighratesofreadmissionandmortality,andthere is a needfor measures toimprove outcomes. This study aimsto assess the impact ofthe implementationofaprotocol-basedfollow-upprogramforheartfailurepatientsonreadmission andmortalityratesandqualityoflife.
Methods:A quasi-experimentalstudywas performed,withaprospectiveregistry of50 con-secutivepatientsdischargedafterhospitalizationforacuteheartfailure.Thestudygroupwas followed byacardiologist atdays7-10andthefirst, third,sixthand12th monthafter dis-charge,withpredefinedprocedures.Thecontrolgroupconsistedofpatients hospitalizedfor heartfailurepriortoimplementationoftheprogramandfollowedonaroutinebasis. Results:Nosignificantdifferenceswereobservedbetweenthetwogroupsregardingmeanage (67.1±11.2vs.65.8±13.4years,p=0.5),NYHAfunctionalclass(p=0.37),ormedianleft ventric-ularejectionfraction(27%[19.8-35.3]vs.29%[23.5-40];p=0.23)atdischarge.Meanfollow-up afterdischargewassimilar(11±5.3vs.10.9±5.5months,p=0.81).
The protocol-based follow-up program was associated with asignificant reductionin all-causereadmission (26%vs.60%,p=0.003),heart failurereadmission (16%vs.36%,p=0.032), andmortality(4%vs.20%,p=0.044).Inthestudygrouptherewasasignificantimprovementin allqualityoflifemeasures(p<0.001).
∗Correspondingauthor.
E-mailaddress:joaoragostinho@gmail.com(J.R.Agostinho).
https://doi.org/10.1016/j.repc.2019.03.006
0870-2551/©2020SociedadePortuguesadeCardiologia.PublishedbyElsevierEspa˜na,S.L.U.ThisisanopenaccessarticleundertheCC BY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Conclusion:Aprotocol-basedfollow-upprogramforpatientswithheartfailureledtoa signif-icantreductioninreadmissionandmortalityrates,andwasassociatedwithbetterqualityof life.
©2020SociedadePortuguesadeCardiologia.PublishedbyElsevierEspa˜na,S.L.U.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/). PALAVRAS-CHAVE Insuficiência cardíaca; Programade seguimento; Reinternamento; Mortalidade
Programadeseguimentoprotocoladodedoentescominsuficiênciacardíaca:impacto noprognósticoenaqualidadedevida
Resumo
Introduc¸ão: Osdoentescominsuficiênciacardíaca(IC)apresentamtaxaselevadasde reinter-namentoemortalidade,tornandonecessáriaaimplementac¸ãodemedidasqueconduzamàsua reduc¸ão.Avaliou-seoimpactodaimplementac¸ãodeumprogramadeseguimentoestruturado dedoentescomICnastaxasdereinternamentoemortalidadeenaqualidadedevida. Métodos: Estudoquasi-experimental, de registoprospetivo, que incluiu 50doentes consec-utivos com alta após internamento por insuficiência cardíaca aguda. Os doentes iniciaram seguimentoprotocoladoapósalta,porcardiologista,comconsultaaos7-10dias,1,3,6e12 meses,comprocedimentospré-definidos.Ogrupo-controlofoiconstituídopordoentes inter-nadosporinsuficiênciacardíacapreviamenteàimplementac¸ãodoprograma,seguidosapósa altaemconsultasderotina.
Resultados: Não houve diferenc¸as entre ambos os grupos no respeitante à idade média (67,1±11,2versus65,8±13,4anos;p=0,5),classefuncionaldaNYHA(p=0,37)emedianada frac¸ãodeejec¸ãodoventrículoesquerdo[27%(19,8-35,3)versus29%(23,5-40);p=0,23]àdata daalta;otempodeseguimentomédiofoiidêntico(11±5,3versus10,9±5,5meses;p=0,81).
Oseguimentoprotocoladoassociou-seareduc¸ãosignificativadastaxasdereinternamentopor qualquercausa(26%versus60%,p=0,003),reinternamentoporinsuficiênciacardíaca(16%versus 36%,p=0,032)emortalidadetotal(4%versus20%,p=0,044).Nogrupoemestudoverificou-se melhoriasignificativaemtodososparâmetrosdequalidadedevida(p<0,001).
Conclusão:Umprogramadeseguimentoprotocoladodedoentescominsuficiênciacardíaca per-mitiureduc¸ãosignificativanastaxasdereinternamentoemortalidadeeassociou-seamelhoria daqualidadedevida.
©2020SociedadePortuguesadeCardiologia.PublicadoporElsevierEspa˜na,S.L.U.Este ´eum artigoOpen Accesssobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Heartfailure(HF)isanimportantpublichealthproblemdue toitshighprevalenceandimpactonpatients’qualityoflife andsurvival.1---11
InEuropeandtheUSA,theestimatedprevalenceofHF is1-2%inadults,1anda10-15%increaseinthenumberof
affectedindividualsis projectedforthenext10-15 years, reflectingtheagingofthepopulation (mainlydueto gen-eralimprovementsinhealthcare),theimpactofriskfactors onthegenesisofthesyndrome,andtheroleof comorbidi-ties,particularlyintheelderly.2---4InPortugal,theestimated
prevalenceofHFis4.4%,reaching8%intheseventhdecade oflife,ahigherprevalencethantheEuropeanaverage.4---6
Despite the therapeutic advances achieved in recent decades, especially with respect to reductions in sudden cardiac death,7 the mortality attributed to HF remains
high.8,9Thisisespeciallytruefollowinghospitalizationdue
todecompensated HF, when reported mortality is 17-24% duringtheyearafterdischarge.10,11
TheimportanceofhospitalizationforHFisduenotonly totheassociatedmortality,butalsotothehighreadmission rate,12whichimposesasignificanteconomicburdenonthe
healthsystem---80%ofthecostsrelatedtothesyndrome2
---andpoorqualityoflifeforpatientswithHF.
Thereadmissionrateisparticularlyhighinthevulnerable phase(thefirstmonthsafterdischarge),withone-fourthof patientsbeingreadmittedinthefirstmonthafterdischarge andtwo-thirdsinthefollowingyear.10,13Thetransitionphase
(pre-andpost-discharge)is thereforeof particular impor-tanceintermsofcare,planningandfollow-up,sinceoneof themainfactorsresponsibleforearlyreadmissionislackof coordinationofcareafterhospitaldischarge.6,14
Several post-discharge follow-up strategies have been proposed,althoughnotallhaveshownasignificantimpact onoutcomes.15---17 Structuredfollow-up programsbasedon
hospitalconsultationsareoftenassociatedwithareduction inreadmissionsduringthefirstyear(relativeriskreduction [RRR] of 19-30%),15,16,18 andalso in therisk of death.15---17
therefore recommended by the European Society of Car-diology (ESC).19 However,muchof the evidenceonwhich
this recommendation is based derives from a time when some contemporary therapies, particularly cardiac resyn-chronization therapy (CRT) and implantable cardioverter defibrillators(ICD),werenotwidelyavailable.15---17Thereis
alsonoevidence onthe impactof theimplementationof suchprogramsinPortugal.
The objective ofthis single-centerstudy wastoassess theresultsofimplementingastructuredfollow-upprogram forHFpatients onreadmission andmortalityratesandon qualityoflife,afteranepisodeofhospitalizationduetothe syndrome.
Methods
Designandpopulation
This wasaquasi-experimental design study carriedoutin asinglecenter(the cardiologydepartmentofSanta Maria UniversityHospital,Lisbon,Portugal).
Thestudypopulationconsistedof50consecutivepatients admitted for acute heart failure (AHF), defined as new-onsetAHFordecompensatedchronic heartfailure,tothe generalcardiologyward(indexhospitalization),whowere discharged after the implementation of a protocol-based follow-upprogram(beginninginApril2016).Thediagnosisof HFwasestablishedaccordingtotheESCguidelines,through theidentificationofsymptomsand/orsignsofHFcausedby a structural and/or functional cardiac abnormality, resul-tinginreducedcardiacoutputand/orelevatedintracardiac pressures.19
Thecontrolgroupconsistedofpatientsselectedfroma cohort hospitalized for AHF in the same cardiology ward immediately before the beginning of the program (from October 2014 to April 2016). Patients from both cohorts (study group andcontrol group) were classifiedaccording to New York Heart Association functional class(NYHA) at discharge(NYHAIvs.NYHAII vs.NYHAIIIorIV),left ven-tricularejectionfraction(LVEF)(tertiles),andage(tertiles). Foreachofthepatientsinthestudygroupapatientfrom thecontrolcohortwithsimilarscoresineachofthethree variableswasrandomlyselected.
Demographic, clinical, laboratory, echocardiographic, electrocardiographic and therapeutic data regarding the index hospitalization and the follow-up period after dis-charge were collected for the study group and for all patientswhoconstitutedthecontrolcohort.Qualityoflife wasassessedatdischargeandatsix-monthfollow-upusing the validated Portuguese version of the Kansas City Car-diomyopathyQuestionnaire(KCCQ).20
Interventionsdifferentiatingthestudygroup
Themaindifferentiatinginterventionintheprotocol-based follow-up program was consultations by a cardiologist at days7-10 andthe first,third, sixthand12th month after discharge(andadditionally,wheneverconsiderednecessary) withpre-specifiedprocedures.Theseincluded:
(a) Clinicalassessmentaimedatidentifyingsignsor symp-tomsofHFdecompensation,residualcongestionorlow cardiacoutput;
(b) Laboratoryassessment,includingmonitoringofplasma N-terminal pro-brain natriuretic peptide (NT-proBNP) level,end-organdysfunction,anddevelopmentof com-mon comorbidities in HF patients (diabetes, chronic pulmonary disease, dyslipidemia, thyroid dysfunction, anemia,irondeficiency)19;
(c) Electrocardiogram at every visit, and transthoracic echocardiogrambetweenthethirdandsixthmonthsand every 12 months of follow-up; when considered nec-essary, cardiac magnetic resonanceimaging study was requested;
(d) Assessmentofadherenceandtolerancetotherapy; (e) Individualized titration of therapy in accordance with
theESCguidelines19;
(f) Patient educationregardingself-care,lifestyle modifi-cations,andmanagementofHFdecompensation.19
Studyoutcomes
Theprimaryoutcome wasall-causereadmission. HF read-mission, death and the composite endpoint of all-cause readmissionordeathweresecondaryoutcomes.
In the structuredfollow-up program group, changes in qualityoflifeparameterswasalsoconsideredasecondary outcome.
Also,in the study group, LVEF change was assessed in thesubgroupofpatientswithLVEF<50%,andthe prescrip-tionrateofneurohormonalantagonistsandchangesintheir respectivedosesduringfollow-upwasassessedinthe sub-groupofpatientswithHFwithreducedLVEF(HFrEF)(LVEF <40%).
Statisticalanalysis
Assuming that the estimated annual rate of all-cause readmissionwouldbe65%in thecontrolgroupand35%in thestudy group(basedonHFpopulationalstudies10,13 and
HFpost-dischargeprogramsstudies,15respectively),itwas
estimated that 42 patients would need tobe followed in eachgroupfor12monthstoprovidethestudywithapower of80%todetect asignificantrelativereductionintherisk ofall-causereadmissioninthefollow-upprogramgroup,at anoveralltwo-sidedalphalevelof0.05.
The statistical analysis wasperformed usingIBM SPSS® Statisticsversion20 (Chicago,IL, USA).Categorical varia-blesarereportedasabsolutenumberandpercentageand continuous variables are reported as mean and standard deviationormedianandinterquartilerange.Theimpactof inclusioninthestructuredfollow-upprogramonreadmission andmortalityrates wasassessedusingCoxregressionand Kaplan-Meiersurvivalanalysis.Wilcoxon’stestwasusedto assesstheimpactofthefollow-upprogramonqualityoflife, dosesof neurohormonal antagonists andLVEF.Differences between the groups regarding demographic, clinical and therapeuticdatawereestablishedusingtheMann-Whitney, Student’st,chi-square,one-wayANOVAandFisher’sexact tests. p values of <0.05 were considered to indicate statisticalsignificance.
Ethicalconsiderations
Thestudywasapprovedbythelocalethicscommitteeand bythenationalDataProtectionAuthority.Patient confiden-tialitywasensuredthroughanonymizationofthecollected data.Allstudyprocedureswerecarriedoutin accordance withtheethicalprinciplesexpressedinthe2013revisionof theDeclarationofHelsinki.21
Results
Populationcharacteristics
Thefirstpatientwasenrolledintheprotocol-based follow-upprograminApril2016andthe50thpatientinNovember 2017.Themeanfollow-upwas11±5.3monthsinthestudy groupand10.9±5.5monthsinthecontrolgroup(p=0.81).
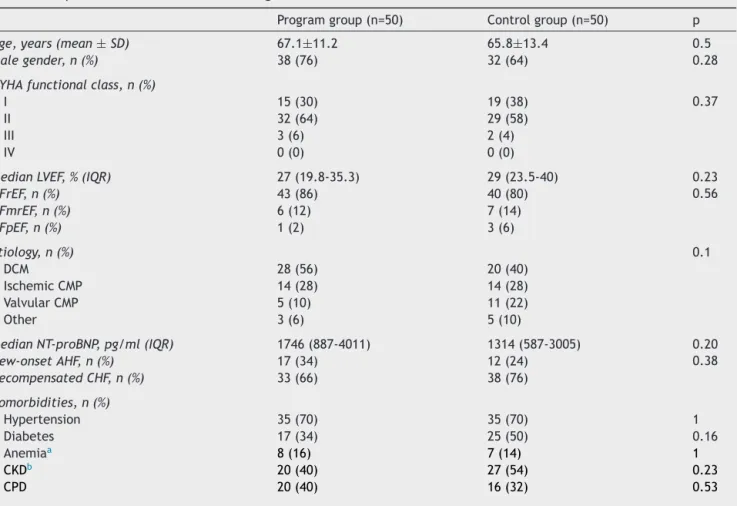
Patients’demographicandclinicalcharacteristicsat dis-chargearedescribedinTable1.
The mean age of the follow-up program group was 67.1±11.2 years and 38 patients (76%) were male. Most patients wereinNYHA I(30%)or II(64%) atdischarge; all patients were in NYHA III (52%) or IV (48%) on admission (index hospitalization). The median LVEF documented at discharge was27% (19.8-35.3), and43 (86%) patients had HFrEF. Therewere nosignificant differences between the twogroupsregardingage,NYHAorLVEF.
ThemostfrequentHFetiologyinboth groupswas idio-pathic dilatedcardiomyopathy (56%vs. 40%), followed by ischemic heart disease (28% vs.28%). Overall, 70% of the patientshadahistoryofhypertension,makingitthemost commoncomorbidityinbothgroups.
MedianlengthofstayandmedianplasmaNT-proBNPat dischargedidnotdiffersignificantlybetweengroups.
Mortalityandreadmissionrates
Comparedtopatientsinthecontrolgroup,thoseincluded in the structured follow-up program showed a significant
Table1 Populationcharacteristicsatdischarge.
Programgroup(n=50) Controlgroup(n=50) p
Age,years(mean±SD) 67.1±11.2 65.8±13.4 0.5
Malegender,n(%) 38(76) 32(64) 0.28
NYHAfunctionalclass,n(%)
I 15(30) 19(38) 0.37
II 32(64) 29(58)
III 3(6) 2(4)
IV 0(0) 0(0)
MedianLVEF,%(IQR) 27(19.8-35.3) 29(23.5-40) 0.23
HFrEF,n(%) 43(86) 40(80) 0.56 HFmrEF,n(%) 6(12) 7(14) HFpEF,n(%) 1(2) 3(6) Etiology,n(%) 0.1 DCM 28(56) 20(40) IschemicCMP 14(28) 14(28) ValvularCMP 5(10) 11(22) Other 3(6) 5(10)
MedianNT-proBNP,pg/ml(IQR) 1746(887-4011) 1314(587-3005) 0.20
New-onsetAHF,n(%) 17(34) 12(24) 0.38 DecompensatedCHF,n(%) 33(66) 38(76) Comorbidities,n(%) Hypertension 35(70) 35(70) 1 Diabetes 17(34) 25(50) 0.16 Anemiaa 8(16) 7(14) 1 CKDb 20(40) 27(54) 0.23 CPD 20(40) 16(32) 0.53
Lengthofstay,days(median(IQR) 10(6-14.5) 9(5-17) 0.44 aHemoglobin<12g/dl(women)and<13g/dl(men).
b Estimated glomerularfiltration rate<60 ml/min/1.73m2 (calculatedbytheChronicKidneyDiseaseEpidemiology Collaboration
formula).
AHF:acuteheartfailure;CHF:chronic heartfailure; CKD:chronic kidneydisease; CMP:cardiomyopathy; CPD:chronicpulmonary disease;DCM:dilatedcardiomyopathy;HFmrEF:heartfailurewithmid-rangeejectionfraction;HFpEF:heartfailurewithpreserved ejectionfraction;HFrEF:heartfailurewithreducedejectionfraction;LVEF:leftventricularejectionfraction;NT-proBNP:N-terminal pro-brainnatriureticpeptide;NYHA:NewYorkHeartAssociation.
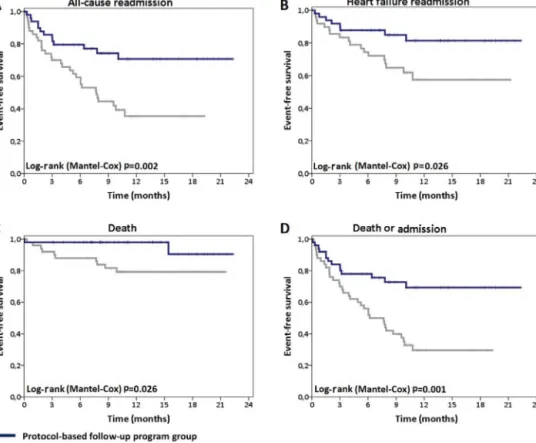
Figure 1 Kaplan-Meier survival curves for all-causereadmission (A), heart failure readmission (B), death (C),and deathor admission(D).
reduction in all-cause readmissions (26% vs. 60%; hazard ratio[HR] 0.38 [0.2-0.73];p=0.003) (Figure1A). The RRR was56.7%andthenumberneededtotreat(NNT)was2.91.A similarbenefitwasachievedinHFreadmission(RRR:64.4%; NNT:3.45)(Figure1B).Eighteen(36%)patientsinthecontrol groupwerehospitalizedduetoAHF.Implementationofthe protocol-basedfollow-upprogramledtoanHFreadmission rateof16%(eightpatients)(HR0.4[0.17-0.92];p=0.032).
Mortality was significantly lower in patients enrolled in the follow-up program (4% vs. 20%; HR 0.21 [0.05-0.96]; p=0.044).The RRR was80% andthe NNT was 6.25 (Figure1C).
During follow-up two (4%) patients in the study group died, one due toright ventricular failure in the immedi-atepostoperativeperiodfollowingcardiacsurgery,andthe otherduetosuddendeath.ThelatterpatientunderwentICD implantation during the index hospitalization and sudden deathoccurred in thefirst week afterhospital discharge, beforethefirstprotocol-basedfollow-upvisit.Autopsywas notperformedandinterrogationoftheICDshowedno dys-rhythmiaorevidenceofdevicedysfunction.Inthecontrol group,two(4%)patientsdiedduringHFhospitalization,and four(8%)duringhospitalizationduetoothercauses.
Thesecondaryoutcomeofdeathorall-cause hospitaliza-tionwassignificantlylessfrequentinthefollow-upprogram group(28%vs.68%;HR0.36[0.19-0.67];p=0.001),withan NNTofonly2.5(Figure1D).
Qualityoflifeandfunctionalclass
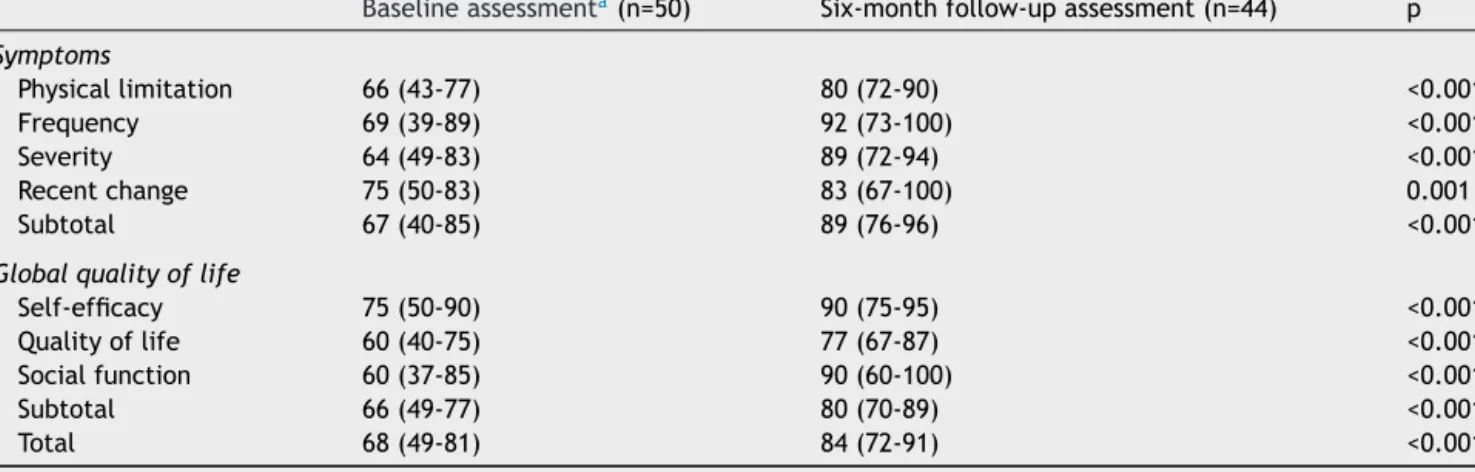
Inthestudygroup,asignificantimprovementwasobserved in all KCCQ domains, especially in the overall summary scoresforsymptoms(67%vs.89%,p<0.001)andqualityof life(66%vs.80%,p<0.001)(Table2).
Parallel to the improvement in the KCCQ symptoms domain reported by the patients, there wasa significant improvement in NYHA class documented by the cardiolo-gistin the lastfollow-up visit comparedtoNYHA classat discharge.In the last clinical assessment performed most patientswereinNYHAI(64%vs.30%,p<0.001)(Figure2).
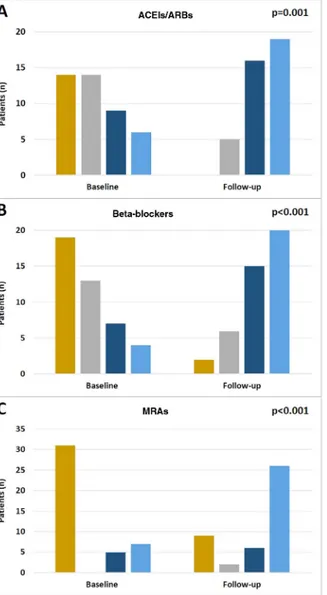
Therapywithneurohormonalantagonists
As stated above, the majority of patients in both groups presented HFrEF.Table 3 describes ongoing therapy (neu-rohormonalantagonistsandcardiacdevices)atthetimeof thelastclinicalassessment.
The rateofprescription ofbeta-blockers, mineralocor-ticoid receptorantagonists (MRAs)and ivabradine didnot differ between the two groups. However, a significantly higherrateofprescriptionofangiotensin-convertingenzyme inhibitors(ACEIs)/angiotensinreceptorblockers(ARBs)was observed in patients included in the follow-up program groupcomparedtocontrols(100%vs.85%, p=0.01).There
Table2 QualityoflifeinthestudygroupasassessedbytheKansasCityCardiomyopathyQuestionnaire(validatedPortuguese version).
Baselineassessmenta(n=50) Six-monthfollow-upassessment(n=44) p Symptoms Physicallimitation 66(43-77) 80(72-90) <0.001 Frequency 69(39-89) 92(73-100) <0.001 Severity 64(49-83) 89(72-94) <0.001 Recentchange 75(50-83) 83(67-100) 0.001 Subtotal 67(40-85) 89(76-96) <0.001
Globalqualityoflife
Self-efficacy 75(50-90) 90(75-95) <0.001
Qualityoflife 60(40-75) 77(67-87) <0.001
Socialfunction 60(37-85) 90(60-100) <0.001
Subtotal 66(49-77) 80(70-89) <0.001
Total 68(49-81) 84(72-91) <0.001
aBaselineassessmentwasperformedathospitaldischarge.
DataarereportedasmedianandIQR.
Figure2 ChangesinNewYorkHeartAssociation(NYHA)functionalclassduringfollow-up.
werenosignificantdifferencesregardingCRTorICD implan-tationrates(Table3).
Consideringthewholepopulation,therewereno signif-icantdifferencesin diuretictherapyprescription between groups(44 vs.47patients, p=NS). Allthesepatientswere medicatedwithloopdiuretics;fourpatientsinthe follow-upprogramgroupandsixpatientsinthecontrolgroupwere underanassociationofaloopplusathiazidediuretic(p=NS). Therewerenodifferencesin myocardial revasculariza-tion procedures, either percutaneous angioplasty (6% vs. 8%, p=NS), or coronary artery bypassgraft surgery (2% in bothgroups, p=NS). Ratesof aortic(6% vs.8%,p=NS)and mitral(6%vs.4%,p=NS)valveinterventions(percutaneous orsurgical)werealsosimilarinbothgroups.
In the study group there was an effective optimiza-tionof treatment during follow-up, including up-titration of recommendeddrugs. Significant increasesin the doses of ACEIs/ARBs (p=0.001), beta-blockers (p<0.001) and MRAs(p<0.001)(Figure3A-C,respectively) wereobserved betweenadmissionandthelastfollow-upvisit.
In the subgroup of patients with HFrEF or HF with mid-rangeejectionfractionenrolledintheprotocol-based follow-upprogram(n=49),therewasasignificant improve-ment in LVEF during follow-up (27% [19.8-35.3] vs. 39.5% [29.5-50];p<0.001).
Discussion
TheimpactofhospitalizationsonthenaturalhistoryofHF isillustratedbythefrequentlyreportedincreasein mortal-ityduringtheperiodthatfollowsahospitaladmissiondue tothesyndrome.Inthisperiod,notonlydoesthemortality risk increase,but aviciouscycle leadingtofurther hospi-talizationsistriggered.10,22Thisisofmajorimportanceata
timewhen,despiteallthetherapeuticadvances,HF read-missionratescontinuetoincrease.9,23InPortugal,according
tothelatest publishedreportoftheNational Programfor Cerebro-Cardiovascular Diseases,9 the number of hospital
admissions due to HF episodes was19 434 in 2015 (2365 deaths), an increase of 4000 episodes compared to 2011
Table3 Pharmacologicaltherapyandcardiacdevicesatlastclinicalassessment.
Programgroup(n=43) Controlgroup(n=40) p Pharmacologicaltherapy Beta-blocker 41(95.3) 35(87.5) 0.25 ACEI/ARB 43(100)a 34(85) 0.01 MRA 34(79.1) 29(72.5) 0.61 Ivabradine 5(11.6) 2(5) 0.44 Cardiacdevices CRT-P 3(7) 6(15) 0.32 CRT-D 11(25.6) 9(22.5) 0.8 0.12 ICD 11(25.6) 4(10) 0.09
a Thisgroupincludesthreepatientstreatedwithsacubitril/valsartan.
Dataarereportedastotalnumberandpercentage.ACEI:angiotensin-convertingenzymeinhibitor;ARB:angiotensinreceptorblocker; CRT-D:cardiacresynchronizationtherapy withcardioverter-defibrillator;CRT-P:cardiac resynchronizationtherapy-pacemaker;ICD: implantablecardioverter-defibrillator;MRA:mineralocorticoidreceptorantagonist.
Figure 3 Changes in the doses of angiotensin-converting enzymeinhibitors(ACEIs)/angiotensinreceptorblockers(ARBs) (A),beta-blockers(B)andmineralocorticoidreceptor antago-nists(MRAs)(C)duringfollow-up.
(15 583 hospitalizations, 2046 deaths), making it impera-tivetoestablishstrategiesthatmayleadtoareductionin the(re)hospitalizationrate,andconsequentlyinmortality, inthesepatients.6
Inthisstudywepresentthecharacteristicsandresultsof aprotocol-basedfollow-upprogramconductedatthe car-diology department of a European tertiary hospital. Prior totheimplementationoftheprogram,onthebasisofthe frequencyofmajoreventsinthecontrolgroup,readmission (60%)andmortality(20%)afterhospitaldischargeinpatients admittedfor anHFepisodeweresimilartoorevenhigher thanthose reportedin the literature.10,11,13 The HF
read-missionrate in ourcontrol population wassimilartothat reportedin publisheddataonPortuguesecohorts (36%vs. 30.5%),althoughmortalitywaslower(20%vs.34.3%).24
How-ever,implementationof thestructuredfollow-upprogram ledtoamarked reductionin all-causereadmission (abso-luteriskreductionof40%),andalsotoaconsiderablethough smallerreductioninreadmissionsduetodecompensatedHF (absoluteriskreductionof20%).Concomitantlyasignificant reductioninmortalitywasobtained(from20%to4%).
Thebenefitofincludingpatientsinthefollow-upprogram isevidentwhenthesecondaryendpoint(deathor readmis-sion)isanalyzed,asthereductionofmajoreventsresulted inanNNTof2.5,whichis,interestingly,abetterresultthan thatreportedforconventionalHFtherapies.25---32
Unlikevarious other follow-upor monitoring strategies designedtoreducehospitalizationsandmortalityintheHF population, suchas telemonitoring or follow-up programs based on telephone contacts,33,34 protocol-based
follow-upprogramshavedemonstratedconsistentbenefits.These benefitsdo,however,notreachthemagnitudereportedin thisstudy.15---17Onepossiblereasonforthisdifferencemay
bethatmostofthebeneficialevidencefromthese follow-upprogramsgoesbacktoatimewhensomeofthecurrent HFtreatmentoptionswerenotyetavailable.
Additionally, the magnitude of benefit achieved may berelatedtotheintrinsiccharacteristics of our protocol-basedfollow-upprogram.Atfirst,duringhospitalizationand in the pre-discharge period, a careful management plan wasset up according to the patients’ characteristics and needs. The follow-up program after discharge was based
onface-to-faceconsultationsandonpredefinedprocedures (seeMethods)withdemonstratedbenefits inevent reduc-tion, favoring a holistic approach based on international guidelines.19
Itisimportanttohighlightthefrequencyofthe consul-tations,withparticularemphasisonthevisitsatdays7-10 andatonemonthafterdischarge.Earlypost-discharge vis-its have important benefits for reducing readmission and mortality,notonly duringthefirstmonth afterdischarge, but also thereafter.18,22,35 This is related to the
impor-tanceofthehospital-hometransitionandtotheproblems thatpatients usuallyface,includingdifficultiesin manag-ing medication, unfamiliarity with the necessary changes in lifestyle, lack of knowledge about their disease, and managementofworseningsymptoms.Theroleoftheearly post-dischargeconsultationsfocuses onhelpingwiththese problemsand,whennecessary,ontherapeuticoptimization. At each visit, the presence of symptoms or signs indicative of decompensation was carefully assessed and appropriate therapeutic measures were taken. This may havecontributeddecisivelytothemarkedreductioninHF readmission.However,itshouldbenotedthatmuchofthe benefitderivedfromthisprogramwasseeninthereduction inall-causereadmissions.Toaccomplishthis,itwascrucial to pay particular attention to the monitoring and mana-gement of comorbidities,which have a significant impact onHFpatients’ prognosis,asmost hospitalizations inthis populationarefornon-cardiaccauses.23
Itisalsoworthemphasizingtheeffectoftheprogramon theup-titrationofneurohormonalantagonistdoses,asthe vastmajorityofpatientswithHFrEFweretreatedwith beta-blockers(95.3%),ACEIs/ARBs(100%),andMRAs(79.1%),and inmanypatientstargetdoseswereachieved(46.5%,47.5% and60.5%, respectively). The frequency of hospital visits andassessmentoftherapeutictolerancemayhaveplayeda partinthisachievement.However,althoughoptimizationof pharmacologictherapy mayhavehadanimportantrolein theobservedmarkedreductionofeventsduringfollow-up, itshouldalsobenotedthatthenumberofpatientstreated withthese drugsin thecontrol groupwasalsohigh, even higherthanpreviouslyreportedinPortugueseHFcohorts.24
TherateofCRTandICDimplantationwassimilarbetween the two groups and similarto that reported in European cohorts.10 This finding supports the added benefit of this
follow-upprogramwithholisticinterventionsontopofthe benefitassociatedwithmedicalanddeviceHFtherapies.
The follow-up program was also associated with sig-nificant improvements in both NYHA functional class and qualityoflifeandsymptomsasassessedbytheKCCQ.The scoresobtainedinboth domainsat dischargeweresimilar tothose in the literature (66% and67% vs. 56% and 63%, respectively),36 whereas at the sixth month of follow-up
the scores reported herein were significantly higher (80% and89%,respectively).Particularattentionshouldbegiven tothe‘self-efficacy’sub-domain,whichassessespatients’ perceivedabilitytomanagetheirownsymptoms.The pop-ulationincludedinthe follow-upprogramhadarelatively highself-efficacyscore(75%)atthetimeofdischarge,which maybeduetotheeducationonpatientself-careprovided duringhospital stay.Nevertheless, a significant additional improvement(90%)wasobservedduringfollow-up, demon-stratingtheeffectivenessoftheHFself-caremanagement
andhealth-relatededucationreinforcementcarriedoutat each consultation. This may also have accounted for the reductioninmajoradverseevents.
To our knowledge this is the first study reporting the efficacyofaprotocol-basedfollow-upprograminreducing readmissionandmortalityinaPortuguesepopulationwith HF,fillinganapparentevidencegap6,37 and,wehope,
per-hapshelpingtoencouragethedevelopmentofthistypeof programinotherhospitalcenters.
Limitations
Thedatareportedshouldbeinterpretedinthelightof cer-tain limitations, particularly the fact that this was not a randomizedcontrolledstudyandthatthesamplesizewas small (thefirst 50 patients enrolledand followed by pro-tocol). Besides, only patients admitted to the cardiology department were included, which naturally entails selec-tionbias,resultinginapopulationwithahigherproportion ofpatientswithHFrEFandyoungerthanthosereportedin studiesthatincludedpatientsadmittedtointernalmedicine departments.24Additionally,cost-effectivenessanalysiswas
notperformed, soitisnotpossible todetermine whether the reduction in events during the follow-up period was accompaniedbyareductionincostsattributedtoHF. How-ever, assignificant reductions in the admission rate were obtained,thisprobablytranslatedintoreductionsin costs related tothe syndromeand toassociated comorbidities. Finally,thestudyonlyincludedpatientswitharecent admis-sionduetoAHF,soitisnotpossibletoassesstheimpactof thisfollow-up programonstablepatients withchronic HF butwithnopreviousrecentHF-relatedhospitaladmissions. As reported, most adverse events in HF patients occur in thefirstyearafterhospitaldischarge.10,11,13Infact,despite
thesmallnumberofpatientswhocompletedmorethan12 months of follow-up in our population, through the data obtainedfromtheKaplan-Meiersurvivalcurves(Figure 1A-D),itmaybeassumedthattheincidenceofmajoradverse eventsduringthesecondyearoffollow-upwouldhavebeen low,suggesting a reducedbenefitof this typeof program instablepatients,aspreviouslysuggested.38,39However,we
considerthat more evidenceis needed in orderto estab-lishtheidealdurationofthistypeofprogram,accordingto patients’clinicalprofileanddiseaseprogression.
Conclusions
Despite all the advances achieved in the treatment of patientswithHF---includingdrugsdesignedtomodify prog-nosis,cardiacdevicesandmanagementofcomorbidities ---morbidityandmortalityattributedtothesyndromeremain high.Structuredfollow-upprogramsmayhaveakeyrolein themanagementofthesepatients.
Thisstudyreports theresultsoftheimplementationof suchaprograminthecardiologydepartment ofatertiary hospital,andis thefirsttodocumentitsbenefitsina Por-tuguese population with HF. The program was associated withmarkedreductionsinHFreadmission,all-cause read-missionandmortality,andwithsignificantimprovementsin functionalclassandinpatients’self-reportedqualityoflife.
Theresultssupporttheneedforinvestmentinthistype ofprogramasameanstoimprovetheprognosisofpatients withHF,andconsequentlytoreducetheburdenattributed tothecondition.
Authors’
contributions
JRA and DB designed the protocol and wrote the manuscript. JRA performed the statistical analysis. All authorscontributedsimilarlytodatacollection, recording andinterpretation,reviewedthearticleandgavetheirfinal approvalfortheversiontobepublished.
Sponsorship
Thestudydidnotreceiveanysponsorship.
Conflicts
of
interest
Theauthorshavenoconflictsofinteresttodeclare.
References
1.Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart.2007;93:1137---46.
2.Heidenreich PA,Albert NM, Allen LA, et al. Forecasting the impactofheart failurein theUnitedStates: a policy state-mentfrom the American Heart Association. Circ Heart Fail. 2013;6:606---19.
3.Massie BM, Shah NB. Evolving trends in the epidemiological factors of heart failure: rationale for preventive strate-gies and comprehensive disease management. Am Heart J. 1997;133:703---12.
4.FonsecaC,BrásD,AraújoI,etal.Heartfailure innumbers: estimatesforthe21st centuryinPortugal.RevPortCardiol. 2018;37:97---104.
5.CeiaF,FonsecaC,MotaT,etal.Prevalenceofchronicheart failureinSouthwesternEurope:theEPICAstudy.EurJHeart Fail.2002;4:531---9.
6.FonsecaC,BritoD,CernadasR,etal.Fortheimprovementof HeartFailuretreatmentinPortugal---consensusstatement.Rev PortCardiol.2017;36:1---8.
7.Shen L, Jhund PS, Petrie MC, et al. Declining risk of sudden death in heart failure. N Engl J Med. 2017;377: 41---51.
8.LaribiS,AoubaA,NikolaouM,etal.Trendsindeathattributed toheartfailureoverthepasttwodecadesinEurope.EurJHeart Fail.2012;14:234---9.
9.Direc¸ão-GeraldaSaúde.RelatóriodoProgramaNacionalparaas Doenc¸asCérebro-Cardiovasculares;2017.Availableatwww.dgs. pt/em-destaque/relatorio-do-programa-nacional-para-as-doencas-cerebro-cardiovasculares-2017.aspx
10.MaggioniAP,DahlstroU,FilippatosG,etal.EURObservational ResearchProgramme:regionaldifferences and1-year follow-upresultsoftheHeartFailurePilotSurvey(ESC-HFPilot).Eur JHeartFail.2013;15:808---17.
11.TavazziL, SenniM, Metra M, et al. Multicenterprospective observationalstudyonacuteandchronicheartfailure:one-year follow-upresultsofIN-HF(Italian Networkon HeartFailure) outcomeregistry.CircHeartFail.2013;6:473---81.
12.Hall MJ, DeFrances CJ, Williams SN, et al. National hospi-tal discharge survey: 2007 summary. Natl Health Stat Rep. 2010;26:1---20.
13.Cowie MR, Anker SD, Cleland J, et al. Improving care for patients with acute heart failure: before, during and after hospitalization; 2014. Available at www.oxford healthpolicyforum.org/files/reports/ahf-report.pdf
14.VanWalraven C,Bennett C,Jennings A, etal. Proportionof hospitalreadmissionsdeemedavoidable:asystematicreview. CMAJ.2011;183:E391---402.
15.Phillips CO, Wright SM, Kern DE, et al. Comprehensive discharge planning with postdischarge support for older patientswithcongestiveheartfailure:ameta-analysis.JAMA. 2004;291:1358---67.
16.McAlisterFA,StewartS,FerruaS,etal.Multidisciplinary strate-giesforthemanagementofheartfailurepatientsathighrisk foradmission:asystematicreviewofrandomizedtrials.JAm CollCardiol.2004;44:810---9.
17.Feltner C, Jones CD, Cene CW, et al. Transitional care interventionsto preventreadmissions for persons withheart failure:asystematicreviewandmeta-analysis.AnnInternMed. 2014;160:774---84.
18.PachoC,DomingoM,NunezR,etal.Anearlypost-discharge intervention planned to reduce 30-day readmissions in old and frail heartfailure patientsremains beneficial at1 year. Rev Esp Cardiol. 2018. Available at www.revespcardiol. org/es/an-early-post-discharge-intervention-planned/avance-resumen/S1885585718300306/
19.Ponikowski P,VoorsAA, AnkerS, et al.2016 ESC Guidelines for the diagnosis and treatmentof acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developedwiththespecialcontributionof theHeart FailureAssociation(HFA)of theESC.EurHeartJ. 2016;37:2129---200.
20.Nave-LealE,Pais-RibeiroJ,OliveiraM,etal.Propriedades psi-cométricasdaversãoportuguesadoKansasCity Cardiomyopa-thyQuestionnairenamiocardiopatiadilatadacominsuficiência cardíacacongestiva.RevPortCardiol.2010;26:353---72.
21.WorldMedicalAssociation.WorldMedicalAssociation Declara-tionofHelsinki:ethicalprinciplesformedicalresearchinvolving humansubjects.JAMA.2013;310:2191---4.
22.Hernandez AF, Greiner MA, Fonarow GC,et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heartfailure. JAMA.2010;303:1716---22.
23.Gerber Y, Weston SA, Redfield MM, et al. A contemporary appraisaloftheheartfailureepidemicinOlmstedCounty, Min-nesota,2000to2010.JAMAInternMed.2015;175:996---1004.
24.MarquesI,AbreuS,BertãoMV,etal.Characteristicsand out-comesofheartfailurehospitalizationbeforeimplementation ofa heartfailureclinic: thePRECICstudy.RevPort Cardiol. 2017;36:431---8.
25.Packer M, Coats AJ, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001;344:1651---8.
26.GargR,YusufS.Overviewofrandomizedtrialsof angiotensin-converting enzyme inhibitors on mortality and morbidity in patientswithheartfailure.JAMA.1995;273:1450---6.
27.Granger CB, McMurray JJV, Yusuf S, et al. Effects of can-desartan in patients withchronic heartfailure and reduced left-ventricular systolic function intolerant to angiotensin-converting-enzyme inhibitors: the CHARM-Alternative trial. Lancet.2003;362:772---6.
28.PittB,ZannadF,RemmeWJ.Theeffectofspironolactoneon morbidityandmortalityinpatientswithsevereheartfailure.N EnglJMed.1999;341:709---17.
29.McMurrayJJ,PackerM,DesaiAS,etal.Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371:993---1004.
30.Swedberg K, Komajda M, Böhm M, et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlledstudy.Lancet.2010;376:875---85.
31.ClelandJ,DaubertJ,ErdmannE,etal.Theeffectofcardiac resynchronizationonmorbidityandmortalityinheartfailure. NEnglJMed.2005;352:1539---49.
32.Connolly SJ, Hallstrom AP, Cappato R, et al. Meta-analysis of the implantable cardioverter defibrillator secondary pre-vention trials.AVID, CASHand CIDS studies.Antiarrhythmics vsImplantableDefibrillatorstudy.Cardiac ArrestStudy Ham-burg. Canadian Implantable DefibrillatorStudy. EurHeart J. 2000;21:2071---8.
33.Lynga P, Persson H, Hagg-Martinell A, et al. Weight mon-itoring in patients with severe heart failure (WISH). A randomized controlled trial. Eur J Heart Fail. 2012;14: 438---44.
34.BoyneJJJ,VrijhoefHJM,CrijnsHJGM,etal.Tailored telemoni-toringinpatientswithheartfailure:resultsofamulticentre
randomized controlled trial. Eur J Heart Fail. 2012;14: 791---801.
35.PachoC,DomingoM,NunezR,etal.Earlypostdischarge STOP-HF-Clinicreduces30-dayreadmissionsinoldandfrailpatients withheartfailure.RevEspCardiol.2017;70:631---8.
36.JosephSM1,NovakE,ArnoldSV,etal.Comparableperformance oftheKansasCityCardiomyopathyQuestionnaireinheart fail-urepatientswithpreservedandreducedejectionfraction.Circ HeartFail.2013;6:1139---46.
37.FonsecaC.Anapproachtoimprovingheartfailuremanagement -alocalcontribution.RevPortCardiol.2017;36:439---41.
38.SchouM,GustafssonF,VidebaekL,etal.Extendedheartfailure clinicfollow-upinlow-riskpatients:arandomizedclinicaltrial (NorthStar).EurHeartJ.2013;34:432---42.
39.LuttikML,JaarsmaT,vanGeelPP,etal.Long-termfollow-up inoptimallytreatedandstableheartfailurepatients:primary carevsheartfailureclinic.ResultsoftheCOACH-2study.EurJ HeartFail.2014;16:1241---8.