www.journalpulmonology.org
ORIGINAL
ARTICLE
Intra-hospital
mortality
for
community-acquired
pneumonia
in
mainland
Portugal
between
2000
and
2009
F.
Teixeira-Lopes
a,∗,
A.
Cysneiros
a,
A.
Dias
a,
V.
Durão
a,
C.
Costa
a,
F.
Paula
a,
M.
Serrado
a,
B.
Nunes
b,c,
A.
Diniz
a,
F.
Froes
aaDepartamentodoTórax,CentroHospitalarLisboaNorte,Av.Prof.EgasMoniz,1649-035Lisbon,Portugal
bDepartamentodeEpidemiologia,InstitutoNacionaldeSaúdeDr.RicardoJorge,Av.PadreCruz,1649-016Lisbon,Portugal cCentrodeInvestigac¸ãoemSaúdePública,EscolaNacionaldeSaúdePública,Av.PadreCruz,1600-560,Lisbon,Portugal
Received1November2017;accepted2June2018
KEYWORDS Community-acquired pneumonia; Mortality; Intra-hospital mortality; Pneumonia; Inpatientmortality Abstract
Introduction:Community-acquiredpneumonia(CAP)remainsacommonandseriousinfection withwidevariabilityinintra-hospitalmortality.
Methods:WeperformedaretrospectiveanalysisofadultpatientsadmittedwithCAPin main-landPortugalbetweentheyears2000and2009.
Results:Theintra-hospitalmortalityratewas20.4%withdeathsinallagegroups.Theaverage ageofdeceasedpatientswas79.8years,significantlyhigherthansurvivingpatientswith71.3 years.Patientsaged50ormorepresentedarelativeriskofdeath4.4timestheriskofpatients underthisagegroup.Likewise,inpatientsaged65ormore theriskofdeathwas3.2times theriskofpatients<65years.Mendiedmoreatayoungeragethanwomen,themenwhodied were,onaverage,4yearsyoungerthanwomen,78.1vs82.1yearsold.Relativeriskofdeath inmenwas17%higherthanwomenafteradjustmentforyearofadmissionandage.
Conclusion: CAPremainsanimportantcauseofhospitalmortalityinallagegroups.
© 2018Sociedade Portuguesa dePneumologia. Published by Elsevier España,S.L.U. This is anopenaccessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/ by-nc-nd/4.0/).
∗Correspondingauthor.
E-mailaddress:franciscateixeiralopes@gmail.com
(F.Teixeira-Lopes).
Introduction
Community-acquiredpneumonia(CAP)isanimportantcause ofmorbidityandmortalityaswellasexpenditureofhealth resources.Ahigherincidenceofthisdiseasewasreported inmenandolderpatients.1
https://doi.org/10.1016/j.pulmoe.2018.06.004
2531-0437/©2018SociedadePortuguesadePneumologia.PublishedbyElsevierEspaña,S.L.U.ThisisanopenaccessarticleundertheCC BY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Severalstudies2---4inthelastdecadeshowedanincrease
inhospitaladmissionsforCAP.Portugalwasnoexception.5
Between2000and2009CAPwasresponsiblefor3.7%ofall hospitaladmissions whichincreasedto7%in patients≥65 yearsofage.5
CAP istheleadingcauseofdeathbyinfectiousdisease indevelopedcountries,6it istheeighthcauseofdeathin
theUnitedStates(US) in2014.7InaUSstudy with33,000
patientsconductedin1996,CAPintra-hospitalmortalitywas 13.6%increasingto36.5%inICUpatients.8
InEuropeancountries,mortalityduetoCAPvaries.Ina 2012 review withmore than 30 studies performed over 9 Europeancountries,Welteetal.1concludedthatvariability
ofintra-hospital mortalityinCAP wassignificantly related toseveralfactors. This ledtomortalityrates of between 1.0%and43%dependingonage(≥65years),co-morbidities, severity (multilobarpneumonia, septic shock, ICU admis-sion),immunestatus,antibioticsensitivityandresponseto treatment.
In Portugal,themortality ratein adultsadmitted with CAP between 1998 and 2000 was 17.3% without gender predominance.9 Mortality was greater in older patients,
rangingfrom4.5%inthoseyoungerthan50years,19.4%in patients≥50yearsand21.4%inthoseolderthan≥65years.9
Thepresentstudyaimstodescribetheevolutionof intra-hospitalmortality within the Portuguese adult population admittedwithCAPbetween2000and2009andunderstand itsdistributionbyageandgender.
Methods
DatawasgatheredthroughtheCentralAdministrationofthe NationalHealthSystem(NHS)whichhasclinicaldataforall patientsadmittedtoPortugueseNHShospitals.Thiscovers nearly the entire resident population of mainland Portu-gal.Medicaldata,includingdiagnosisandprocedures,were encoded from the discharge summaries by trained physi-ciansusingtheInternationalClassificationofDiseases,9th Revision---ClinicalModification(ICD-9-CM).
In this study, we retrospectively analyzed the hospital admissionsofadultswithaprimarydiagnosisofpneumonia (ICD-9-CM480-486and487.0)betweentheyears2000and 2009.We thenanalyzed all inpatientdeathsregardless of thelengthofhospitalstay.Thesecodesexcluded tuberculo-sispneumonia,obstructivepneumonia(e.g.associatedwith lungcancer),patientsunder18yearsofageandthosefor whompneumoniawasnotthemain diagnosis.AsICD-9-CM doesnotspecifywhetherpneumoniaiscommunityacquired, we excluded patients withHIV (ICD-9-CM 042-044 and/or diagnosis-relatedgroups488,489and490),individualswho were immunocompromised by anti-cancer or immunosup-pressivetreatment(externalcauseofdiseasecodeE933.1) andtransplantrecipients(V42).
Patient anonymity was maintained throughout clinical analysis.Comparisonofthemeanagebetweengroupswas performedusingtheStudent’sTtestortheMann---Whitney testwhentheassumptionsoftheTtestwerenotobserved. Theriskofdeathwascomparedbetweenagegroups,gender andyearofadmissionwiththechi-squaredtest.Therelative riskofinpatientdeathwascalculatedforeachgroupaswell
Table1 Evolutionofintra-hospitalmortalityratebetween 2000and2009.
Year Totaladmissions Deaths(%)
2000 23,679 4046 (17.1%) 2001 22,442 4147 (18.5%) 2002 26,093 4930 (18.9%) 2003 27,978 5549 (19.8%) 2004 26,582 5366 (20.2%) 2005 31,302 6569 (21.0%) 2006 29,131 6320 (21.7%) 2007 33,726 7235 (21.5%) 2008 34,083 7652 (22.5%) 2009 39,011 8111 (20.8%) 2000---2004 126,774 24,038 (19.0%) 2005---2009 167,253 35,887 (21.5%) Total(2000---2009) 294,027 59,925 (20.4%)
variable(agegroup,genderandyearofadmission)onthe riskofdeathadjustedtotheothervariables,alog-binomial regressionwasused.Alltestsusedhadasignificancelevel set at 5%. Dataanalysis was performed using SPSS20 and STATASE11.
Results
Annualintra-hospitalmortalityrates
Between the years 2000 and 2009, 294,027 adults were admittedtohospitalwithamaindiagnosisofCAP.Ofthose, 59,925(20.4%)diedduringtheirhospitaladmission.
Table1representstheinpatientmortalityrateperyearof
admissionbetween2000---2004and2005---2009.The annual mortalityrateshowedasteadyincreasebetweentheperiod 2000---2004 and 2005---2009 witha constant rise of 13.2%, exceptfortheyears2007and2009.
Ageandgendercharacterization
ThepatientsadmittedwithaprimarydiagnosisofCAPhada meanageof73.1years(standarddeviation---SD:16.0).The deceasedpatientshadameanageof79.8years(SD:11.3) andamedianageof82years.Thiswassignificantlyhigher thanthemeanageofthesurvivingpatientswith71.3years (p<0.01).
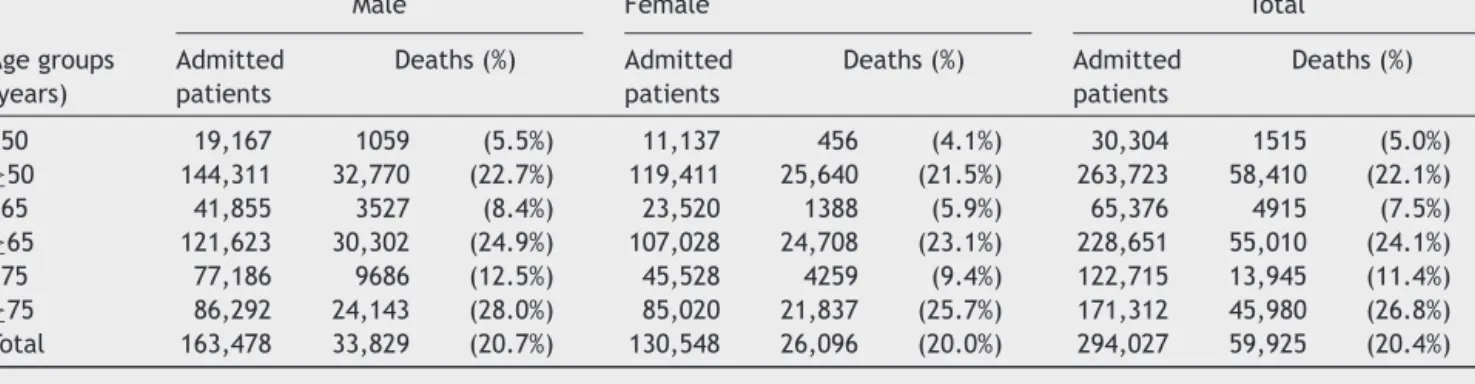
Theinpatientmortalityrateformalepatientswas20.7% while in femalepopulation it was20.0%(p<0.01). Within thetotalofdeceasedpatients,56.5%weremalewithamean ageof78.1yearsand43.5%werefemalewithameanageof 82.1years.Thedifferencebetweenthemeanagesinboth groupswasstatisticallysignificant(p<0.01).
Thereweredeathsinallagegroups,however,thelowest mortalityratewasobservedinthoseaged29yearswitha mortalityrateof1.7%.
Table2representsthemortalityrateofadmittedpatients
by gender and age group (<50, ≥50, <65, ≥65, <75, ≥75 years).
Community-acquiredpneumonia 3
Table2 Intra-hospitalmortalitybygenderandagegroups(ageinferiororequaltoandgreaterthan50,65and75years).
Male Female Total
Agegroups (years) Admitted patients Deaths(%) Admitted patients Deaths(%) Admitted patients Deaths(%) <50 19,167 1059 (5.5%) 11,137 456 (4.1%) 30,304 1515 (5.0%) ≥50 144,311 32,770 (22.7%) 119,411 25,640 (21.5%) 263,723 58,410 (22.1%) <65 41,855 3527 (8.4%) 23,520 1388 (5.9%) 65,376 4915 (7.5%) ≥65 121,623 30,302 (24.9%) 107,028 24,708 (23.1%) 228,651 55,010 (24.1%) <75 77,186 9686 (12.5%) 45,528 4259 (9.4%) 122,715 13,945 (11.4%) ≥75 86,292 24,143 (28.0%) 85,020 21,837 (25.7%) 171,312 45,980 (26.8%) Total 163,478 33,829 (20.7%) 130,548 26,096 (20.0%) 294,027 59,925 (20.4%)
was4.4times(CI95%4.2---4.7)theriskforthoseunderthis agegroup.Inthepopulation≥65yearstherelativeriskof deathwas3.2times(CI95%3.1---3.3)theriskofthe<65years population(p<0.01).
Table3representstheannualevolutionofmeanageand
mortalityrateinpatientsadmittedanddeceasedbetween theyears2000and2009.Exceptfor2009,therewasa con-sistentannualincreaseinthemeanageaswellasmortality rate.
Adjustedmortalityrateinadmittedpatients(year, ageandgender)
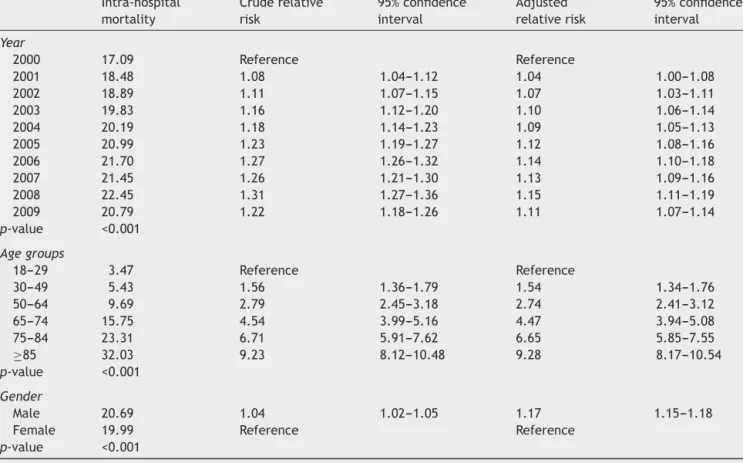
Table 4represents therelative risk of deathadjusted for
yearofadmission,ageandgender.Therelativeriskofdeath variedsignificantlybetween2001and2009whencompared to2000.
Data shows a steady increase in mortality rateby age group,withasmallvariationofrelativeriskafteradjusting foryearofadmissionandgender.
Theriskofdeathwashigherinmalesandthisdifference wasevenhigherwhen adjustedfor year ofadmission and age.Menhada17%higherrelativeriskofdeaththanwomen.
Discussion
From2000to2009theoverallintra-hospitalmortalityrate for patients admitted with CAP in mainland Portugal was 20.4%. This is within the range observed in a European reviewpublishedin 20121 withan intra-hospitalmortality
raterangingbetween1%and43%.LiketheEuropeanstudy inouranalysismortalityalsoincreasedwithage,withthose ≥75havingamortalityrateof26.8%,morethantwicethan those<75,which had11.4% mortalityrate. This was irre-spectiveofyearofadmissionandgender.Thereweredeaths in all age groups with a highlight 5.0% mortality rate in patientsyoungerthan50yearsold.Overthestudiedperiod inpatientmortalityrateshowedasteadyincrease,withtwo exceptions:2007and2009.Theseaccompaniedchangesin themean ageof hospitalized anddeceased patients. The averageage ofdeceased patientswassignificantlyhigher, 79.8years,against71.3yearsinsurvivingpatients.
After adjustment for age and gender, the increase in the relative risk of death during hospitalization over the yearsmaintainedstatisticalsignificance,withan11%raise between 2000 and 2009. Patientsaged 50 or more had a relativeriskof death4.4times therisk of patientsunder thisagegroup. Likewise,in patients aged65or morethe risk of deathwas 3.2 the risk of patients <65. More men
Table3 Meanagesandintra-hospitalmortalityratesofadmittedanddeceasedpatientsbetween2000and2009.
Year Meanage(years) Intra-hospitalmortalityrate(%)
Admittedpatients(N:294,027) Deceasedpatients(N:59,925)
2000 70.1 78.1 17.1 2001 71.3 78.3 18.5 2002 71.6 79.0 18.9 2003 72.1 79.3 19.8 2004 73.3 79.7 20.2 2005 73.8 80.0 21.0 2006 73.8 80.0 21.7 2007 74.2 80.5 21.5 2008 75.0 80.8 22.5 2009 73.6 80.7 20.8 2000---2009 73.1 79.8 20.4
Table4 Intra-hospitalmortalityadjustedforyearofadmission,agegroupsandgender. Intra-hospital mortality Cruderelative risk 95%confidence interval Adjusted relativerisk 95%confidence interval Year 2000 17.09 Reference Reference 2001 18.48 1.08 1.04---1.12 1.04 1.00---1.08 2002 18.89 1.11 1.07---1.15 1.07 1.03---1.11 2003 19.83 1.16 1.12---1.20 1.10 1.06---1.14 2004 20.19 1.18 1.14---1.23 1.09 1.05---1.13 2005 20.99 1.23 1.19---1.27 1.12 1.08---1.16 2006 21.70 1.27 1.26---1.32 1.14 1.10---1.18 2007 21.45 1.26 1.21---1.30 1.13 1.09---1.16 2008 22.45 1.31 1.27---1.36 1.15 1.11---1.19 2009 20.79 1.22 1.18---1.26 1.11 1.07---1.14 p-value <0.001 Agegroups 18---29 3.47 Reference Reference 30---49 5.43 1.56 1.36---1.79 1.54 1.34---1.76 50---64 9.69 2.79 2.45---3.18 2.74 2.41---3.12 65---74 15.75 4.54 3.99---5.16 4.47 3.94---5.08 75---84 23.31 6.71 5.91---7.62 6.65 5.85---7.55 ≥85 32.03 9.23 8.12---10.48 9.28 8.17---10.54 p-value <0.001 Gender Male 20.69 1.04 1.02---1.05 1.17 1.15---1.18
Female 19.99 Reference Reference
p-value <0.001
diedandat ayoungerage thanwomen. Themean ageof deceased men was 78.1 years, 4 years younger than the meanage ofdeceased womenwhich was82.1 years. Rel-ativerisk ofdeathin menwas17% higherthan inwomen afteradjustmentforyearofadmissionandage.
Ourstudy hasseverallimitations. Primarily, itis a ret-rospectivestudythatusesanadministrativedatabasewith codedinformationfromdischargesummaries.However,in Portugal,codificationisdoneonlybymedicaldoctorswith specific training. The process is regularly internally and externallyauditedwhichcontributestoguaranteeaccuracy. DuetothelackofaspecificCAPcodeinICD-9-CM,weonly analyzedadulthospitaladmissionswherethemaindiagnosis waspneumonia.Patientswithamaindiagnosisofrespiratory failureorsepsisassociatedtoasecondarydiagnosisof pneu-moniawere not included. The latter couldbe associated withahighermortalityrate10butalsowithnosocomial
pneu-monia.Still,weacknowledgethepossibilitythatsomecases ofhospital-acquired pneumonia couldhave been included inour study.This is possible due tocoding error but also becausethedatabase doesnotallow fordiscriminationof pneumoniaafterrecenthospitaldischarge,hence pneumo-niathatisnotstrictlycommunityacquired.Similarly,itisnot possibletoidentifypatientslivinginnursinghomesorusing long-term care facilities, hence it is expected that cases of healthcare-associated pneumonia have been included, particularly in the elderly. However, this concept and its inclusion in nosocomial pneumonia remain the source of controversyforsomeauthorsinEurope.11Themethodology
usedmadeitimpossibletoexcludeallrehospitalizationsof thesamepatientwithpneumoniaduringtheperiodstudied, sothecalculatedvaluesrefertohospitaladmissions.
Thegreateraccessibilitytohospitalinstitutionsandthe fearofdyingathome,bothforpatientsandtheirfamilies, mightexplaintheinclusionofpatientswithend-of-life pneu-monia.Thesewilllikelyhave ahigherimpactin theolder agegroups.
The methodology used allowed for the exclusion of patients with tuberculosis, obstructive pneumonia, those withHIV,recipientsoftransplantedorgans,the immunosup-pressedandthoseundertreatmentforcancer.
In this study, the length of hospitalization was not assessed,whichcouldhavecontributedtoagreater speci-ficityofthemethodology.12Itwasneitherpossibletoobtain
information onmortality at 30 daysafter hospital admis-sion or to identify the subset of patients requiring ICU admission.Ourdatabasehadnoinformationonpneumonia severity, co-morbidities or immunizationstatus, regarding influenza or pneumococcal disease. Despite these limita-tions, the methodology used has been considered valid and is appliedin multiple studies carried outin different countries.3,5,9,13---15
Thisstudyhastheadvantageofanalysingaperiodof10 years,minimizingtheimpactofyearsthatdeviatefrom nor-mality,suchas2009,whentheA(H1N1)influenzapandemic occurred. Regarding theyear 2009, therewere moreCAP admissions5andthiscouldberelatedtotheinfluenza
Community-acquiredpneumonia 5 whichwaslowerin2009thaninpreviousyears.Meanageof
admissioncouldbeacontributingfactortolowermortality sinceitwaslowerin2009.AccordingtoPortugueseofficial data therewere 124 deaths attributableto the influenza pandemicthroughserologictesting(1.17deathsper100,000 inhabitants)withameanageof47.6years.16 Insummary,
duringtheinfluenzapandemicthereweremoreadmissions ofyoungpatientswithCAP.
The database analysis could not identify factors con-tributingtotheannualincreaseinintra-hospital mortality rates even after adjusting for age, gender or the higher riskofdeathinmales.Factorssuchassmoking,alcoholism, severityofpneumonia,clinicalmanagementofthedisease and,aboveall,theincreasingprevalenceof comorbidities in the Portuguese population maybe associated with the increaseinmortality.
CAP remains an important cause of hospital mortality in all age groups. Further studies are needed to better understand which factors are associated with the annual increaseinintra-hospitalmortalityrates.Howeverourstudy fullyjustifiestheadoptionoflifestyle-modifyingmeasures aswellasgreater appreciationofanti-influenza and anti-pneumococcalvaccinations.17
Conflicts
of
interest
Dr. Froes reports personal fees and non-financial support from Pfizer, personal fees and non-financial support from MSD, personal fees and non-financial support from TEVA, non-financial support from Sanofi, non-financial support from AstraZeneca, non-financial support from Bayer, per-sonalfeesfromNovartis,outsidethesubmittedwork.
Dr.Teixeira-Lopesandtheotherco-authorshavenothing todisclose.
Acknowledgments
The authors would like to thank Prof. Cristina Bárbara (CHLN, FML), Prof. Ana Escoval (ENSP, UNL) and the ACSS/MS,inparticular,F.CardosoandL.Faustino,for allow-ingustoaccessthedatabase.
References
1.WelteT,TorresA,NathwaniD.Clinicalandeconomicburdenof community-acquiredpneumoniaamongadultsinEurope. Tho-rax.2012;67:71---9.
2.FryAM,ShayDK,HolmanRC,CurnsAT,AndersonLJ.Trendsin hospitalizationsforpneumoniaamongpersonsaged65yearsor olderintheUnitedStates,1988---2002.JAMA.2005;294:2712---9.
3.Trotter CL, Stuart JM, George R, Miller E. Increasing hos-pital admissions for pneumonia, England. Emerg Infect Dis. 2008;14:727---33.
4.Thosem RW, RiisA, NorgaardM, Jacobsen J, Christensen S, McdonaldCJ,etal.Risingincidenceandpersistentlyhigh mor-talityofhospitalizedpneumonia:a10-year population-based studyinDenmark.JInternMed.2006;259:410---7.
5.FroesF,DinizA,MesquitaM,SerradoM,NunesB.Hospital admis-sionsofadultswithcommunity-acquiredpneumoniainPortugal between2000and2009.EurRespirJ.2013;41:1141---6. 6.NiedermanMS,McCombsJS,UngerAN,KumarA,PopovianR.
Thecostoftreatingcommunity-acquiredpneumonia.ClinTher. 1998;20:820---37.
7.KennethD,KochanekMA,SherryL,MurphyBS,JiaquanXu, Bet-zaidaTejada-Vera.Deaths:finaldatafor2014.NatlVitalStat Rep.2016;65.
8.FineMJ,SmithMA,CarsenCA,MuthaSS,SankeySS,Weissfeld LA,etal.Prognosisandoutcomesofpatientswith community-acquired pneumonia: a meta-analysis. JAMA. 1996;275: 134---41.
9.FroesF.[Pneumoniaintheadultpopulationincontinental Por-tugal---incidenceand mortalityinhospitalizedpatientsfrom 1998to2000].RevPortPneumol.2003;9:187---94.
10.Lindenauer PK, Lagu T, Shieh M-S, Pekow PS, Rothberg MB. Associationofdiagnosticcodingwithtrendsinhospitalizations andmortalityofpatientswithpneumonia,2003---2009.JAMA. 2012;307:1405---13.
11.EwigS,WelteT,ChastreJ,TorresA.Rethinkingtheconcepts ofcommunity-acquiredandhealth-care-associatedpneumonia. LancetInfectDis.2010;10:279---87.
12.YuO,NelsonJC,BoundsL,JacksonLA.Classificationalgorithms to improve the accuracy of identifyingpatientshospitalized withcommunity-acquiredpneumoniausingadministrativedata. EpidemiolInfect.2011;139:1296---306.
13.Marrie TJ, Carriere KC, Jin Y, Johnson DH. Factors asso-ciated with death among adults <55 years of age hospi-talized for community-acquired pneumonia. Clin Infect Dis. 2003;36:413---21.
14.Gil-PrietoR,García-GarcíaL,Álvaro-MecaA,MéndezC,García A, de Miguel AG.The burdenfor community-acquired pneu-monia(CAP)andpneumococcalpneumoniainadultsinSpain (2003---2007).Vaccine.2011;29:412---6.
15.Martins M, Boavida JM, Raposo JF, Froes F, Nunes B, Ribeiro RT, et al. Diabetes hinders community-acquired pneumoniaoutcomesinhospitalizedpatients.BMJOpen Dia-betes Res Care. 2016;4:e000181,http://dx.doi.org/10.1136/ bmjdrc-2015-000181.
16.Direc¸ão-Geralda Saúde.Relatório daPandemiadaGripe em Portugal 2009, Direc¸ão --- Geral da Saúde, Junho de 2010, www.dgs.pt.
17.FroesF,BlasiF,TorresA.Achoo,achis,ATCHIN!Vaccineyou. Eur Respir J. 2018;51:1702558, http://dx.doi.org/10.1183/ 13993003.02558-2017.