Mariana Filipa Pereira Ferreira
Catheter Ablation of Atrial Fibrillation in Patients with Heart
Failure with Reduced Left Ventricular Ejection Fraction:
An Updated Systematic Review
Mestrado Integrado em Medicina
Área: Cardiologia Tipologia: Dissertação
Trabalho efetuado sob a Orientação de: Professor Doutor José Pedro Lopes Nunes E sob a Coorientação de: Doutor Luís Miguel Adão Martins
Trabalho organizado de acordo com as normas da revista: Porto Biomedical Journal
Reduced Left Ventricular Ejection Fraction:
An Updated Systematic Review
À minha Avó, Ao Diogo,
Obrigada por tudo o que fazem por mim
“The future belongs to those who believe in the beauty of
their dreams.”
Um sincero agradecimento ao meu orientador de Tese de Mestrado, o Professor Doutor José Pedro Nunes, pelos conselhos que me transmitiu e por toda a orientação prestada, assim como ao meu coorientador, Doutor Luís Miguel Adão Martins.
Um agradecimento também ao Doutor Xavier Resende por todo o apoio prestado na elaboração deste trabalho.
Catheter Ablation of Atrial Fibrillation in Patients with Heart
Failure with Reduced Left Ventricular Ejection Fraction:
An Updated Systematic Review
Mariana Ferreira1*, Carlos Xavier2, Luís Adão2, José Pedro L. Nunes1,2.
1. Faculdade de Medicina da Universidade do Porto, Porto, Portugal.
2. Department of Cardiology, Centro Hospitalar Universitário São João, Porto, Portugal.
Correspondence: Mariana Ferreira, Faculdade de Medicina da Universidade do Porto, Porto, Portugal, up201709077@med.up.pt
ABSTRACT
Aim: Systematic review of clinical trials concerning catheter ablation of atrial fibrillation (AF) in patients with heart failure (HF) with reduced left ventricular ejection fraction.
Methods: Search conducted in two databases: Medline (PubMed) and ISI Web of Science.
Results: Nine studies were selected for further analysis. Ablation led to higher AF freedom rates compared to medical treatment, and also improved heart failure symptoms, functional capacity, quality of life and left ventricular function.
Conclusions: Catheter ablation can be a valuable treatment option in patients with atrial fibrillation and heart failure with reduced ejection fraction since it leads to favourable clinical outcomes such as heart failure symptoms, functional capacity, quality of life, left ventricular function improvement as well as higher AF freedom rates when compared with medical treatment. Furthermore, catheter ablation may have a relevant role in the reduction of overall mortality.
KEYWORDS: Catheter Ablation; Atrial Fibrillation; Heart Failure; Reduced Left
INTRODUCTION
Atrial fibrillation (AF) is one of the most common cardiac arrhythmias and its prevalence has increased substantially over the past few years1. Heart failure (HF)
is among the most prevalent cardiac diseases, particularly in the elderly. These two conditions are frequently associated, mainly due to the fact that they have some important risk factors in common and either of them can cause the other. When isolated, each one has an important impact on patient morbidity and mortality, but when seen together, the impact is increased2.
It is crucial to treat these patients in order to prevent thromboembolism and, simultaneously either to control heart rate or to restore sinus rhythm. For this latter purpose, there are two main types of strategies: pharmacologic and non-pharmacologic therapy (catheter or surgical ablation)3. Despite several options, it is
still unclear which is the best treatment for AF in patients with associated HF4. Some
antiarrhythmic drugs are contraindicated in patients with HF, limiting its choice, mainly restricted to amiodarone or dofetilide. However, the latter requires hospitalization for its administration while amiodarone has poor adherence to long-term treatment due to several adverse effects4. When rhythm control therapy is
chosen to treat HF patients with AF, catheter ablation (CA) could be a good option since this strategy could have clinical and prognostic benefits, such as improvement of systolic function, reduced mortality, as well as improving the quality of life as demonstrated in previous studies4-6. Therefore the 2019 AHA/ACC/HRS Focused
Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation states that “AF catheter ablation may be reasonable in selected patients with symptomatic AF and HF with reduced left ventricular (LV) ejection
fraction (EF) (HFrEF) to potentially lower mortality rate and reduce hospitalization for HF” - recommendation IIa, level B-R of evidence7.
The CA strategy has been increasingly used in the treatment of many different symptomatic cardiac arrhythmias, such as atrioventricular nodal reentrant tachycardia, atrioventricular reentrant tachycardia, atrial flutter and even in AF resistant to pharmacologic control8,9. Regarding AF, there is still considerable
controversy, especially in patients with HF, mainly due to the greater recurrence and complication rates in these patients, as a result of the extent of remodelling and underlying heart disease10, and some studies have shown no benefits and/or
controversial results regarding CA in patients with concomitant AF and HF. Although this procedure is probably less effective than in patients with preserved cardiac function10, CA therapy “may result in freedom from AF recurrence 3 to 4
times greater than that of antiarrhythmics”4. There are several CA techniques
available, but pulmonary-vein isolation is the most frequently used worldwide. This technique started being used when it was discovered that AF could be generated by foci of ectopic beats created in the pulmonary veins. It involves the insertion of a transvenous irrigated radiofrequency ablation catheter, most frequently through the femoral pathway, aiming at the circumferential elimination of the ostia of the pulmonary veins through radiofrequency energy. The end-point of ablation is the disappearance of pulmonary veins potentials11.
This report aims to update the systematic review of the randomized clinical trials in patients with heart failure with reduced ejection fraction (EF<50%) comparing the benefits and/or risks of catheter ablation in this population versus medical therapy.
METHODS
Search strategy
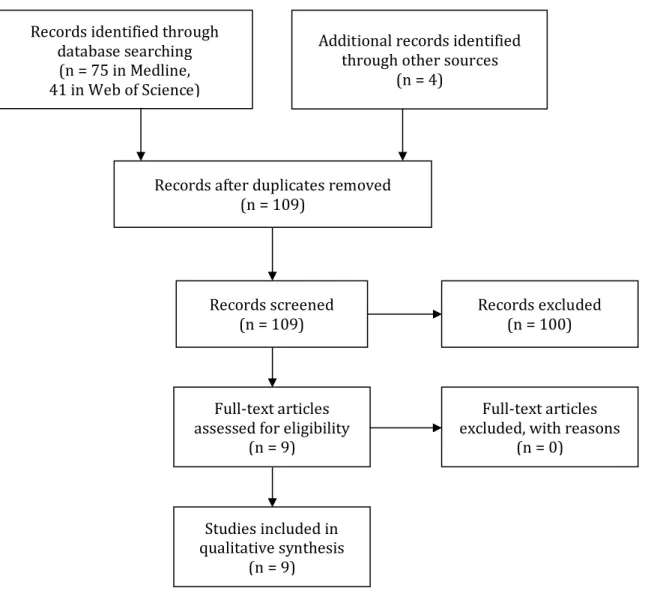
This study was performed in accordance with the guidelines of the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA). The search was conducted using the query “Ablation AND Atrial Fibrillation AND Heart Failure AND Clinical Trial” in two databases: Medline (PubMed) and ISI Web of Science. Initially seventy-five articles were identified in PubMed and forty-one in ISI Web of Science. This selection was carried out between July and August 2019 and there were no articles deleted based on publication data. Besides these, four other studies were included after searching the references of previous review articles. The largest clinical trial published so far12 included mostly non heart failure patients, although
with an important number of heart failure patients. These latter patients were the subject of a sub-analysis report, which was taken for further analysis13.
Inclusion criteria
Randomized clinical trials (RCT’s), in patients with heart failure with reduced left ventricular ejection fraction (EF<50%).
Exclusion criteria
We excluded studies that included patients with heart failure with preserved ejection fraction (EF>50%). Retrospective and cohort studies, case-reports, systematic reviews and meta-analysis were also excluded, as well as studies presented in any language other than English.
Data collection process
Study quality and eligibility were individually assessed by two independent researchers who, initially, analysed all the titles and abstracts, and then (if the inclusion and exclusion criteria were met) the full-text articles of the query selection
and the studies found after searching the references of previous review articles. Data extraction (Table 1) was individually done from the data published in the articles and then compared by two investigators.
RESULTS
Through the initial analysis, based on the titles and abstracts, we selected 5 articles from Medline (PubMed) and ISI Web of science (4 articles and 1 further article respectively), which fulfilled the inclusion criteria. Besides these, we found 4 more studies of interest after searching the references of previous review articles. Thus, we selected 9 RCT’s6,12-19 to be analysed by the authors. After full-text analysis, no
articles were excluded. A flowchart presenting the search method, as well as the final number of articles selected, is shown in Figure 1. The articles included were published between 2008 and 2019 and included a total of 1742 patients.
Study characteristics (Table 1)
The main characteristics of the study population in each article, as well as the general characteristics of the studies, such as intervention, endpoints and major results, are shown in Table 1. The total number of patients under study was 1742, the mean or median lowest age being fifty-five years and the highest mean or median age being sixty-eight years. The shortest follow-up was 6 months 6,19 and the
longest follow-up was 48.5 months12. Regarding the type of AF we found studies that
only evaluated patients with a specific type of AF (persistent14-17,19) and others that
evaluated patients with all different types of AF6,12,13,18. One study, “Effect of
Catheter Ablation vs Antiarrhythmic Drug Therapy on Mortality, Stroke, Bleeding, and Cardiac Arrest Among Patients With Atrial Fibrillation – the CABANA trial”12
included mostly non heart failure patients, and therefore we used the subgroup analysis involving only heart failure patients13.
Intervention
Regarding the type of intervention, all the studies included a group of patients undergoing AF catheter ablation – study group. All RCT’s have a comparison group composed by patients with similar baseline characteristics to the study group. Two different types of treatment were compared in the selected studies: CA vs medical treatment12-19 or CA vs atrio-ventricular node ablation (AV-node ablation) +
biventricular pacing6. All the CA procedures were based on pulmonary vein isolation
(PVI) strategy.
Endpoints
Major results of the several studies are synthetized in Table 1. All studies reported greater rates of AF freedom at the end of follow up in the group of patients submitted to CA in comparison with the patients submitted to other type of treatment. The highest rate of AF freedom was seen in the “A randomized trial to assess catheter ablation versus rate control in the management of persistent atrial fibrillation in heart failure” (ARC-HF) trial16 with 88% of the patients in CA group in sinus rhythm
(SR) at the end of 12 months of follow-up.
Mean Left Ventricular Ejection Fraction (LVEF) was the main measure used to assess cardiac function. The studies accessed LVEF through echocardiography (mainly using Simpson’s biplane method) except for: the Catheter Ablation Versus Medical Rate Control in Atrial Fibrillation and Systolic Dysfunction (CAMERA-MRI) trial19, that used both echocardiography and cardiovascular magnetic resonance
(CMR); the ARC-HF study16 that used radionuclide ventriculography; MacDonald et
significantly better improvement of LVEF in patients who underwent CA. The greatest improvement was seen in the CAMERA-MRI19 study, where there was a
change of +18.3% in the CA group (p<0.0001) versus +4.4% in the medical rate control group (p=0.0145), and at 6 months of follow-up, 58% of the CA patients had normalized LVEF (≥50%) versus 9% in the medical rate control group (p=0.0002). In terms of symptoms and quality of life, several studies evaluated the change in the New York Heart Association (NYHA) functional class and applied various types of questionnaires depending on the study (Minnesota Living with Heart Failure – MLWHF; 36-item Short-Form Health Survey - SF-36, etc.). All studies reported positive results on improvement of NYHA functional class. Regarding quality of life, most reports show an improvement in this parameter, except for one article, by MacDonald et al.17 that did not find significant differences in quality of life between
the two groups of patients under study.
The three largest studies in this review evaluated global mortality related to CA and all of them found a significant reduction in overall mortality: Ablation Versus Amiodarone for Treatment of Persistent Atrial Fibrillation in Patients With Congestive Heart Failure and an Implanted Device (AATAC)14 - p=0.037; Catheter
Ablation for Atrial Fibrillation with Heart Failure (CASTLE-AF)18 - hazard ratio (HR)
0.53; 95% Confidence Interval, 0.32 to 0.86; Ablation of atrial fibrillation in heart failure patients: additional outcomes of the CABANA trial13 – HR 0.59 with a 95% CI
of 0.44 – 0.75, p < 0.0001.
Finally, regarding procedure-related complications, the “Pulmonary-vein isolation for atrial fibrillation in patients with heart failure” - PABA-CHF study6 showed no
significant differences between the study groups. However, other studies reported significant complications rates, as it happened with MacDonald et al. (15%) and
CAMERA-MRI (4.7% per procedure and 7.7% per patient)15,17,19. Overall, the main
complications were groin bleeding, pericardial effusion, cardiac tamponade, pulmonary edema, stroke and pulmonary vein stenosis.
DISCUSSION
The present systematic review shows that catheter ablation may be beneficial in the treatment of atrial fibrillation in patients with concomitant heart failure with reduced ejection fraction. This analysis demonstrated major benefits in global mortality, improvement of LV function and quality of life.
A total of nine RCT’s, investigating the outcomes of patients with AF and HF who underwent CA for the treatment of AF, were analysed. Of these set of studies, seven6,13-16,18,19 showed benefits of CA, regarding the main outcome in comparison
with other treatment (medical treatment or AV-node ablation + biventricular pacing), and two12,17 did not show benefits or had mixed results. In all of the studies,
the group of patients submitted to CA showed a greater percentage of AF freedom in comparison with the control group. The control group, in many studies, had all patients maintaining AF6,15,17,19 after the follow-up time, thus showing superiority of
catheter ablation as compared to medical treatment and to atrioventricular-node ablation + biventricular pacing (in Pulmonary-Vein Isolation for Atrial Fibrillation in Patients with Heart Failure - PABA-CHF study6) in this regard.
To better analyse the results, we will divide the studies into 2 groups: with short follow-up period (≤12 months)6,15-17,19 and studies with long follow-up period (> 12
months)12-14,18.
Starting with studies with shorter follow-up, the PABA-CHF study6, with a 6 months
biventricular pacing in patients with symptomatic AF and LVEF≤40%. This study included 81 patients and showed significant improvements in clinical outcomes, such as in the MLWHF score and 6-min-walk distance (6MWD). In this study, a subgroup analysis, comparing patients with paroxysmal AF to nonparoxysmal AF both submitted to PVI, showed that patients with nonparoxysmal AF had a greatest benefit in LVEF, 6MWD, MLWHF score and left atrial internal diameter. Concerning complications, this study showed fewer complications related to the CA procedure (two patients developed pulmonary-vein stenosis, one patient with pericardial effusion and pulmonary edema in another) and these complications were not very different from the control group. However, this low complication rate can be related to the fact that these CA procedures were performed at centers with experienced ablationists, so results may not be reproducible.
The CAMERA-MRI trial19, also with 6 months of follow-up, enrolled 66 patients with
persistent AF and idiopathic cardiomyopathy (LVEF≤45). Patients submitted to PVI ablation had a higher improvement in LVEF.The authors reported that patients who did not have significant ventricular fibrosis in CMR had significantly higher improvement in LVEF. In terms of quality of life, there was an improvement in NYHA class but not in 6MWD test, SF-36 physical or mental component scores.
In the “A randomized controlled trial of catheter ablation versus medical treatment of atrial fibrillation in heart failure - (CAMTAF) trial”15 the ablation procedure was
compared to medical therapy in 50 patients with persistent AF e HF (EF < 50%). Despite freedom from AF after the ablation procedure being reported in 73% of the patients, without antiarrhythmic drugs (AAD’s), at 12 months of follow-up, the single-procedure success rate was only 38%. In contrast, in the ARC-HF trial16, the
(with a multiple-procedure success of 92%). Overall, this study reported a success of ablation showing a greater improvement in all primary (LV function) and secondary outcomes (functional capacity, NYHA class, HF symptoms and quality of life) in patients submitted to ablation. In the complications section, this study did not find differences in the safety of this procedure in this set of patients in comparison with patients without structural heart disease.
In contrast with PABA-CHF6 and CAMTAF15 studies, the ARC-HF16 study, with 6
months of follow-up, showed some controversial results: it did not show any significant improvement in LVEF and 6MWD despite the improvement in 12-month change in peak oxygen consumption (primary endpoint), in brain natriuretic peptide (BNP) and MLWHF score.
MacDonald and colleagues17 conducted a trial comparing radiofrequency ablation
with medical treatment in patients with persistent AF and EF < 35%, with 9.7 months of mean follow-up. They reported a greater improvement of LVEF (using radionuclide ventriculography) in the ablation group versus the control group. On the other hand, there was no significant difference between the two groups regarding 6MWD or Quality of Life. Furthermore, the authors registered a 15% rate of major complication on the ablation group. Additionally, the investigators did a post-hoc analysis, which revealed that patients in SR at the end of the study had a superior improvement in LVEF versus patients who continued on AF and that the patients in SR at the end of the study were “younger, less likely to have coronary heart disease and more likely to have AF of a shorter duration”.
Regarding longer follow-up studies, the AATAC trial14 was a larger multicentre
randomized trial and with a follow-up duration of 24 months, with 203 patients, that compared CA with amiodarone for the treatment of persistent AF in patients with
congestive heart failure. The authors reported greater improvement of LVEF, 6MWD and quality of life (reduction on MLHFQ) in the ablation group, when compared to the control group. This study was the first to analyse standard cardiovascular clinical outcomes, commonly used in HF trials, namely AF and HF-related unplanned hospitalisations, all-cause mortality and other complications. The authors found a reduction of these cardiac outcomes in patients who underwent ablation, showing a relative risk reduction (RRR) of AF and HF-related unplanned hospitalisations of 45% and an RRR of 56% of all-cause mortality. Regarding complications, the authors showed a relatively unimpressive complication rate in the CA group.
The CASTLE-AF trial18, with 37.8 months of follow-up, compared the cardiovascular
outcomes in patients with symptomatic persistent or paroxysmal AF and HF (EF≤35%) submitted to CA versus medical therapy (rate and rhythm control). The primary endpoint was a composite of death from any cause or hospitalization for worsening HF. Patients submitted to ablation had a significant decrease in the primary endpoint, in overall mortality, in hospitalization for worsening heart failure and in cardiovascular mortality. They also reported an improvement in LVEF, in 6MWD and a reduced burden of AF. However, the restrict inclusion criteria (all patients were required to have absence of response to, unacceptable side effects from or unwillingness to take AAD’s and to have had an implantable cardioverter-defibrillator (ICD) device or a cardiac resynchronization therapy cardioverter-defibrillator (CRT-D)) significantly reduced the initial number of patients (3013), including in the end only 363 of them. This can be seen as a limitation of this study. Recently was carried out an retrospective study to evaluate the generalization of these results obtained in CASTLE-AF - Generalizability of the CASTLE-AF Trial: Catheter Ablation for Patients with Atrial Fibrillation and Heart Failure in Routine Practice, by
Noseworthy, P.A., et al20. The authors concluded that the “benefit associated with
ablation appears to be more modest in practice than that reported in the CASTLE-AF trial”, showing that there is some difficulty in generalizing the results to the real population or routine practice 20. On the other hand, the long-term follow-up (up to
60 months) period is an argument in favour of the results of this study, since the mortality benefit of ablation only reached significance after 3 years of follow-up. Finally, the CABANA trial12 had the longer follow-up duration of 48.5 months and is
the most recent trial included in the present review. The authors analysed the effects of CA versus antiarrhythmic drug therapy on mortality, stroke, bleeding and cardiac arrest in patients with AF. A total number of 2204 patients were included, having symptomatic AF with 65 years of age or older or younger than 65 years with more than one risk factor for stroke. In this set of patients, 886 (40%) of them had concomitant HF and/or NYHA class ≥ 2. Since this review aimed to compare two types of treatment (catheter ablation vs medical therapy) in patients with heart failure, we used this subgroup analysis of CABANA trial involving heart failure patients13. In this analysis, 32% of patients had paroxysmal AF and 68% had
persistent or long-standing AF. Of 886 patients, 441 were randomized to receive catheter ablation and 445 were randomized to receive medical therapy, including rate and/or rhythm control drugs. The primary endpoint was a composite of death, disabling stroke, serious bleeding or cardiac arrest and there was a significant reduction in this endpoint as well as in all-cause mortality.
Therefore, there was a noteworthy difference in the outcomes of these studies: in addition to the outcomes regarding AF freedom, quality of life and LV function and dimensions, the studies with a longer follow-up duration evaluated the hard endpoints like heart failure hospitalization or worsening, all-cause mortality,
cardiovascular mortality, major bleeding among others, that are important data for assessing the benefits from CA ablation. In terms of AF freedom and/or recurrence, LV function or complication rate studies with short and long follow-up duration showed relatively similar results.
Limitations of the study
This review has several limitations: The trials under study used different inclusion criteria for the selection of patients and different drug regimens in the control arm, and some used rate control while others used rhythm control. Many of the studies present a small patient set. Some studies took place in a single centre, which may have limited the results. The duration of the follow-up time of the studies, is very different; some studies have a very short time of follow-up, and this can confuse the results. Many patients underwent more than one ablation procedure. The majority of the procedures were done in centres with vast experience and therefore the published results may not be reproducible in other centres with less experience. Finally, most of the studies did not include hard endpoints, such as unplanned hospitalisations, mortality or cost-effectiveness.
CONCLUSION
Catheter ablation can be a valuable treatment option in patients with of atrial fibrillation and heart failure with reduced ejection fraction since it leads to favourable clinical outcomes such as heart failure symptoms, functional capacity, quality of life, left ventricular function improvement as well as higher AF freedom rates when compared with medical treatment. Furthermore, catheter ablation may have a relevant role in the reduction of overall mortality.
REFERENCES
1. Lubitz SA. Atrial Fibrillation in Congestive Heart Failure. Heart Failure Clin 6 2010;187–200.
2. Khand AU, Rankin AC, Kaye GC, Cleland JG. Systematic review of the management of atrial fibrillation in patients with heart failure. Eur Heart J 2000;21:614-32.
3. Kowey PR. Pharmacologic and Nonpharmacologic Options to Maintain Sinus Rhythm: Guideline-Based and New Approaches. Am J Cardiol 2003 2003;91.
4. Verma A, Kalman JM, Callans DJ. Treatment of Patients With Atrial Fibrillation and Heart Failure With Reduced Ejection Fraction. Circulation 2017;135:1547-63. 5. Zhao Y, Di Biase L, Trivedi C, et al. Importance of non-pulmonary vein triggers ablation to achieve long-term freedom from paroxysmal atrial fibrillation in patients with low ejection fraction. Heart Rhythm 2016;13:141-9.
6. Khan MN, Jais P, Cummings J, et al. Pulmonary-vein isolation for atrial fibrillation in patients with heart failure. N Engl J Med 2008;359:1778-85.
7. January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation 2019;140:e125-e51.
8. Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2016;67:1575-623.
9. Hsu LF, Jais P, Sanders P, et al. Catheter ablation for atrial fibrillation in congestive heart failure. N Engl J Med 2004;351:2373-83.
10. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2014;64:e1-76.
11. Haegeli LM, Calkins H. Catheter ablation of atrial fibrillation: an update. Eur Heart J 2014;35:2454-9.
12. Packer DL, Mark DB, Robb RA, et al. Effect of Catheter Ablation vs Antiarrhythmic Drug Therapy on Mortality, Stroke, Bleeding, and Cardiac Arrest Among Patients With Atrial Fibrillation: The CABANA Randomized Clinical Trial. JAMA 2019;321:1261-74. 13. Packer DL, Monahan KH, Al-Khalidi HR, et al. Ablation of atrial firbrillation in heart failure patients : additional outcomes of the CABANA trial Hearth & Rhythm 2019;16:S35.
14. Di Biase L, Mohanty P, Mohanty S, et al. Ablation Versus Amiodarone for Treatment of Persistent Atrial Fibrillation in Patients With Congestive Heart Failure and an Implanted Device: Results From the AATAC Multicenter Randomized Trial. Circulation 2016;133:1637-44.
15. Hunter RJ, Berriman TJ, Diab I, et al. A randomized controlled trial of catheter ablation versus medical treatment of atrial fibrillation in heart failure (the CAMTAF trial). Circ Arrhythm Electrophysiol 2014;7:31-8.
16. Jones DG, Haldar SK, Hussain W, et al. A randomized trial to assess catheter ablation versus rate control in the management of persistent atrial fibrillation in heart failure. J Am Coll Cardiol 2013;61:1894-903.
17. MacDonald MR, Connelly DT, Hawkins NM, et al. Radiofrequency ablation for persistent atrial fibrillation in patients with advanced heart failure and severe left ventricular systolic dysfunction: a randomised controlled trial. Heart 2011;97:740-7. 18. Marrouche NF, Brachmann J, Andresen D, et al. Catheter Ablation for Atrial Fibrillation with Heart Failure. N Engl J Med 2018;378:417-27.
19. Prabhu S, Taylor AJ, Costello BT, et al. Catheter Ablation Versus Medical Rate Control in Atrial Fibrillation and Systolic Dysfunction: The CAMERA-MRI Study. J Am Coll Cardiol 2017;70:1949-61.
20. Noseworthy PA, Van Houten HK, Gersh BJ, et al. Generalizability of the CASTLE-AF Trial: Catheter Ablation for Patients with Atrial Fibrillation and Heart Failure in Routine Practice. Heart Rhythm 2020.
AUTHOR (S) Nº OF PATIENTS FOLLOW-UP (MONTHS) INTERVENTIO N PATIENTS CHARACTERISTICS PRIMARY/SECONDARY
CLINICAL END POINTS MAJOR RESULTS
Khan M.N et al, 2008 (PABA-CHF) Nº: 81 PVI ablation group (n=41) AV-node ablation + biventricular pacing (n=40) Follow-up: 6 PVI ablation vs AV-node ablation + biventricular pacing
Age(y): 60±8 (PVI ablation
group); 61±8 (AV-node ablation + biventricular pacing).
All patients had EF ≤ 40% Type of AF: paroxysmal (49% -
PVI ablation group; 54% - AV-node ablation + biventricular pacing); persistent or long-standing persistent (51%- PVI ablation group; 46%- AV-node ablation + biventricular pacing).
Mean EF (%) 27±8 – PVI
ablation group; 29±7 – AV-node ablation + biventricular pacing.
LA size (mm): 49±5 – PVI
ablation group; 47±6 - AV-node ablation + biventricular pacing.
Primary:
-Composite of EF; -Distance on the 6MWD; -MLWHF score.
Secondary:
-Freedom from AF; -LA internal diameter.
The difference in the mean EF between the two groups was significant: 35±9% for PVI ablation group, as compared with 28±6% for AV-node ablation + biventricular pacing (P<0.001). LA size decreased in the PVI ablation group (from 49±5 to 45±4 mm) whereas increased in the AV-node ablation + biventricular pacing group (from 47±6 to 49±6) (p<0.001). In the PVI ablation group 88% of the patients receiving antiarrhythmic drugs and 71% of those not receiving such drugs were free of AF at 6 months.
The PVI ablation group had a greater improvement in 6MWD (change of 71m on average) and in MLWHF score (from 89±12 to 60±8) in comparison with AV-node ablation + biventricular pacing group (change of 16m on average on 6MWD; improvement from 89±11 to 82±14 in MLWHF score; p<0.001 for all comparisons).
MacDon ald et al, 2011 Nº: 41 CA group (n=22) Medical therapy group (n=19) Follow-up: 9.7 (ablation group); 6.9 (medical therapy group). CA (PVI) vs Medical therapy Age(y): 62 ± 6.7 (ablation group); 64.4 ± 8.2 (medical therapy group).
All patients had EF < 35% Type of AF: persistent (all
patients).
NYHA class: II (11%-medical
therapy group; 9.7%-ablation group), III (89%- medical therapy group; 91%-ablation group).
Previous HF hospitalisation:
79% - medical therapy group; 77% - ablation group. Primary: CMR EF Secondary: - radionuclide LVEF; - 6 MWD; - NT-proBNP
- Quality of life (QoL).
50% of the patients in the ablation group were in sinus rhythm vs none in medical therapy group. Patients in the ablation group had a greater improvement in LVEF (by CMR) (+4.5±11.1%) in comparison with the medical therapy group (+2.8±6.7%) (p=0.6). There was a superior increase in radionuclide LVEF in the ablation group (+8.2±12%) vs medical therapy group (+1.4±5.9%) (p=0.032). There was no significative difference between the groups regarding the NT-proBNP, 6MWD or QoL. Serious complications due to ablation occurred in 15% of the patients.
ablation group. Jones DG. et al, 2013 (ARC-HF) Nº: 52 CA group (n=26) Rate control group (n=26) Follow-up: 12 CA (PVI) vs Rate control Age(y): 63±9
All patients had EF ≤ 35% All patients had persistent AF HF aetiology: Ischemic
(27%-rate control group; 38%-ablation group); Nonischemic (73%-rate control group; 62%-ablation group).
NYHA class: class II (50%-rate
control group; 54%-ablation group), III (50%-rate control group; 46%-ablation group).
Radionuclide LVEF (%): 25±7
– rate control group; 22±8 – ablation group.
LA size (mm): 46±7 – rate
control group; 50±6 - ablation group.
Primary: 12-month
change in peak oxygen consumption.
Secondary: QoL, BNP,
6-min walk distance, EF.
The peak oxygen consumption at 12 months had a significant increase in the ablation group versus rate control group (difference +3.07 ml/kg/min, 95% CI, 0.56 to 5.59; p = 0.018).
88% of the patients in the ablation group kept sinus rhythm (single-procedure success 72% and multiple-procedure success was 92%). In the rate control group, the target rate was achieved in 96% of the patients. Ablation improved Minnesota score (p=0.019) and BNP (p=0.045) and showed nonsignificant trends toward improved 6-min walk distance (p=0.095) and EF (p=0.055). Hunter R.J. et al, 2014 (CAMTA F) Nº: 50 CA group (n=26) Medical therapy group (n=24) Follow-up: 6 (was extended up to 12 months on the ablation group) CA (PVI) vs Medical therapy
Age(y): 55 (ablation group), 60
(medical group).
All patients had EF<50% All patients had persistent AF NYHA class (class II – 42%
ablation group, 50% medical group; class III – 58% ablation group, 50% medical group).
Cause of HF: Ischemic heart
disease (23% - ablation group; 29% - medical group)
Mean EF (%): 31.8±7.7-ablation
group, 33.7±12.1-medical
group.
LA size (mm): 52 - ablation
group, 50 - medical group.
Primary: Effect on LV function. Secondary: - Reduction in LV end systolic volume (%), - VO2 max; - Plasma BNP; - NYHA class; - MLWHF score; - 36-SF.
Freedom from AF was achieved in 81% of the patients in the ablation group at 6 months without AAD’s. There was a significative improvement in EF in the ablation group (40±12%) vs the medical group (31±13%); p = 0.015. The patients in the ablation group showed an improvement on NYHA score since the first month after the intervention (p<0.001). At 6 months, the NYHA score was 1.6 (CI 95%, 1.4–1.9) in the ablation group compared with 2.4 (CI 95%, 2.1–2.6) in the medical group (p<0.001). This improvement in the CA group was sustained at 1 year (1.7; CI 95%, 1.4– 2.0). The ablation group had a greater improvement (23.7; CI, 14.6 - 32.8) in MLWHF score than the medical group (47.0; CI, 36.5 – 57.6).
The patients in ablation had higher SF-36 score (meaning better QoL) for several parameters: physical functioning (p=0.007), physical role functioning (p=0.004), bodily pain (p=0.005) and vitality (p=0.009).
Di Biase et al, 2016 (AATAC ) (n=102) Amiodarone group (n=101) Follow-up: 24
Amiodarone All patients had EF<40%
All patients had persistent AF NYHA class: II - III.
Mean AF (%):29±5 - ablation group; 30±8 - amiodarone group. LA size (mm): 47±4.2mm ablation group; 48±4.9mm amiodarone group. (defined as freedom from AF, atrial flutter, or atrial tachycardia of >30 seconds duration off AADs at follow-up).
Secondary:
- Complications; - All-cause mortality;
- AF- and HF-related
unplanned hospitalizations; - change in LVEF; 6MWD,
and QoL (MLHFQ)
patients free from AF (95% CI, 25% -44%). The unplanned hospitalizations rate was 31% in the CA group and 57% in the amiodarone group, showing 45% relative risk reduction (relative risk, 0.55; 95% confidence interval, 0.39–0.76). It was also observed a reduction on all-cause mortality in the CA group (8% of mortality rate) in comparison with the amiodarone group (18% of mortality rate) – p=0.037. Group 1, in comparison with group 2, showed better improvement in LVEF (mean change of 8.3% vs 6.2%, p=0.02), 6MWD (19m vs 6m, p=0.02) and QoL (reduction on MLHFQ of 10 vs 5, p=0.04). Prabhu S. et al, 2017 (CAMER A-MRI study) Nº: 66 CA group (n=33) Rate control (n=33) Follow-up: 6 CA (PVI and posterior wall isolation) vs Rate Control
Age(y): 59 (ablation group); 62
(control group).
All patients had EF≤45% Type of AF: 100% of the patient
have persistent AF and 74% of
them have Longstanding
persistent AF.
Mean EF (%): 32 - ablation
group vs 34 - control group (by CMR). LA size (mm): 48±5.5 - ablation group vs 47±8.2 – control group. Late gadolinium enhancement present (CMR): 12% in each group.
Previous direct current
Cardioversion (DCCV): 95% of all patients. Primary: change in LVEF on repeat CMR at 6 months. Secondary: - Cardiac chamber dimensions (LV systolic volume, LV end-diastolic volume, LA
volume, LV stroke
volume); - LVEF
(echocardiography); - Average NYHA class; - BNP;
- 6MWD;
- SF-36 physical and
mental component
scores.
Both groups had a significant improvement in LVEF:
18±13% in the ablation group (p < 0.0001) vs4.4±13% in
the control group (p = 0.0145), but this improvement was superior in the ablation group. 58% in the ablation group vs 9% in the control group had normalized the LVEF (p = 0.0002). Left ventricular end-systolic volume (LVESV) was significantly decreased in the ablation group (-24±24ml/m²) compared with the control group (-8.0±20 ml/m²) (p = 0.007). Also left atrial volume significantly decreased in the ablation group (-12±13 ml/m²), unlike the control group which have no change (1.7±14 ml/m²; p < 0.0001). Patients who that doesn’t have significative fibrosis in CMR had higher significative improvement in LVEF (p=0.0069). NYHA class (p<0.0001) and BNP levels (p=0.0131) had a significative improvement in the ablation group vs medical group. On the contrary 6MWD test (p=0.34), 36 physical component scores (0.62) and SF-36 mental component scores (0.49) did not significantly improve in either group.
Marrou che N.F. et al, 2018 Nº: 363 CA group (n=179) CA (PVI) vs Medical Therapy Age(y): 64
All patients had EF≤35% Type of AF: in CA group 30%
are paroxysmal, 70% persistent
Primary: composite of
death from any cause or
hospitalization for
worsening HF.
The CA group had a significant decrease in primary end point (HR, 0.62; 95% CI, 0.43 to 0.87), in overall mortality (hazard ratio, 0.53; 95% CI, 0.32 to 0.86), in hospitalization
Follow-up: 37.8 are paroxysmal, 65% persistent (30% long-standing persistent). NYHA class: CA group (I- 11%,
II- 58%, III- 29%, IV- 2); Medical therapy group (I- 11%, II- 61%, III- 27%, IV- 1%).
Aetiology of HF: in CA group
40% are Ischemic and 60%
Nonischemic; in medical
therapy group 52% are
Ischemic and 48% Nonischemic. Mean EF (%): 32.5 % in CA group, 31.5% in medical therapy group. LA size (mm): 48 mm in CA group; 49.5 mm in medical therapy group. - HF hospitalization; - Cardiovascular death; - Cardiovascular hospitalization;
- Hospitalization for any cause;
- Cerebrovascular accident.
63.1% of patients in CA group vs 21.7% of patients in medical group (p<0.001) were in SR. The mean absolute increase in LVEF was 8% in CA group vs 0.2% in medical group (p=0.005). Packer D.L. et al, 2019 (CABAN A) Nº: 886 CA group (n=441) Drug Therapy group (n=445) Follow-up: 48.5 CA (PVI) vs Drug Therapy Age(y): 68
Type of AF: 32.1% were
paroxysmal and 67.9% were persistent.
AF severity (CCS class): class 0
(9.5% - CA group; 10.8% - drug therapy group); class 1 (15.1% - CA group; 15.9% - drug therapy group); class 2 (31.8% - CA group; 32.4% - drug therapy group); class 3 (36.5% - CA group; 35% - drug therapy group); class 4 (7.1% - CA group; 6% - drug therapy group).
NYHA Functional class: class I
(13.9% - CA group; 11.6% - drug therapy group); class II/III
Primary: composite of
death, disabling stroke, serious bleeding or cardiac arrest.
Key Secondary:
all-cause mortality;
mortality or CV
hospitalization; and
recurrence of AF.
There was a significant reduction in primary endpoint with a hazard ratio (HR) of 0.66 with a 95% confidence interval (CI) of 0.43 – 0.99. There was also a significant reduction in all-cause mortality with a HR of 0.59 with a 95% confidence interval (CI) of 0.44 – 0.75, p < 0.0001.
Comorbidities:
- Heart failure: 15.7% - CA group; 14.9% - drug therapy group. - Coronary artery disease: 18.8%
- CA group; 19.7% - drug therapy group.
Mean EF (%): 4.8% in the CA
group and 4.2% in the drug therapy group had an EF ≤35%.
LEGEND: AADs - Antiarrhythmic Drugs; AATAC – Ablation Versus Amiodarone for Treatment of Persistent Atrial Fibrillation in Patients With Congestive
Heart Failure and an Implanted Device; AF – atrial fibrillation; ARC-HF – A Randomized Trial to Assess Catheter Ablation Versus Rate Control in the Management of Persistent Atrial Fibrillation in Heart Failure; AV – Atrioventricular; BNP – Brain Natriuretic Peptide; CA – Catheter Ablation; CABANA - Effect of Catheter Ablation vs Antiarrhythmic Drug Therapy on Mortality, Stroke, Bleeding, and Cardiac Arrest Among Patients With Atrial Fibrillation; CASTLE-AF - Catheter Ablation for Atrial Fibrillation with Heart Failure; CAMERA-MRI – Catheter Ablation Versus Medical Rate Control in Atrial Fibrillation and Systolic Dysfunction; CAMTAF – A Randomized Controlled Trial of Catheter Ablation Versus Medical Treatment of Atrial Fibrillation in Heart Failure; CCS – Canadian Cardiovascular Society; CI – Confidence Interval; CMR – Cardiac Magnetic Resonance; EF – Ejection Fraction; HF – Heart Failure; HR – Hazard Ratio; LA – Left Atrium; LV – Left Ventricle; LVEF - Left Ventricular Ejection Fraction; MLWHF – Minnesota Living with Heart Failure; NP- pro BNP – NT-proB-type Natriuretic Peptide; NYHA – New York Heart Association; PABA-CHF – Pulmonary-Vein Isolation for Atrial Fibrillation in Patients with Heart Failure; PVI – Pulmonary Vein Isolation; QoL – quality of life; SF-36 – 36-Item Short Form; SR – Sinus Rhythm; 6MWD - 6-minute walk test distance.
Figure 1. Flowchart showing the literature search method. database searching
(n = 75 in Medline, 41 in Web of Science)
Additional records identified through other sources
(n = 4)
Records after duplicates removed (n = 109)
Records screened
(n = 109) Records excluded (n = 100)
Full-text articles assessed for eligibility
(n = 9)
Full-text articles excluded, with reasons
(n = 0)
Studies included in qualitative synthesis