www.revportcardiol.org
Revista
Portuguesa
de
Cardiologia
Portuguese
Journal
of
Cardiology
ORIGINAL
ARTICLE
Characteristics
and
outcomes
of
heart
failure
hospitalization
before
implementation
of
a
heart
failure
clinic:
The
PRECIC
study
Irene
Marques
a,∗,
Sara
Abreu
b,
Manuela
V.
Bertão
b,
Betânia
Ferreira
b,
Raquel
Lopes
Ramos
b,
Juliana
Lopes
b,
Sandra
Nunes
b,
Denisa
Mendonc
¸a
c,
Laetitia
Teixeira
daDepartmentofInternalMedicine,CentroHospitalardoPorto,InstitutodeCiênciasBiomédicasdeAbelSalazar,Universidadedo
Porto,Porto,Portugal
bDepartmentofInternalMedicine,CentroHospitalardoPorto,Porto,Portugal
cDepartmentofPopulationStudies,InstitutodeCiênciasBiomédicasdeAbelSalazar,EPIUnit-InstitutodeSaúdePública,
UniversidadedoPorto,Porto,Portugal
dDepartmentofPopulationStudies,InstitutodeCiênciasBiomédicasdeAbelSalazar,CINTESIS/ICBAS-UP,EPIUnit-Institutode
SaúdePública,UniversidadedoPorto,Porto,Portugal Received10May2016;accepted11October2016 Availableonline31May2017
KEYWORDS Heartfailure; Mortality; Hospitalization; Patient rehospitalization; Hospitalreadmission Abstract
Objective: Thisstudyaimstocharacterizepatientshospitalizedforacuteheartfailure(HF)in aninternalmedicinedepartmentandtheirone-yearmortalityandrateofrehospitalizationfor decompensatedHF.
Methods:Thisretrospectiveobservationalstudyenrolledallpatientsdischargedin2012after hospitalizationforacuteHF.Dischargesummaries,clinicalrecordsandtelephone interviews wereanalysed.Thedatareportstotheyearbeforeimplementationofaheartfailureclinic.
Results:Fourhundredandtwenty-ninepatientswereenrolled,withameanageof79years, 62.5% female. The most prevalent comorbidity andetiology was hypertension (86.7%) and themostfrequentdecompensationtriggerwasinfection.HFwithpreservedejectionfraction (HFpEF)waspresentin70.5%.In-hospitalmortalitywas7.9%.Atdischargemorethanhalfofthe patientswereprescribedbeta-blockers(52.8%)andangiotensin-convertingenzymeinhibitors (52%).WomenpresentedasignificantlyhigherproportionofHFpEFthanmen(75.3%vs.62.7%,
∗Correspondingauthor.
E-mailaddress:mirenemarquesm@gmail.com(I.Marques).
http://dx.doi.org/10.1016/j.repc.2016.10.011
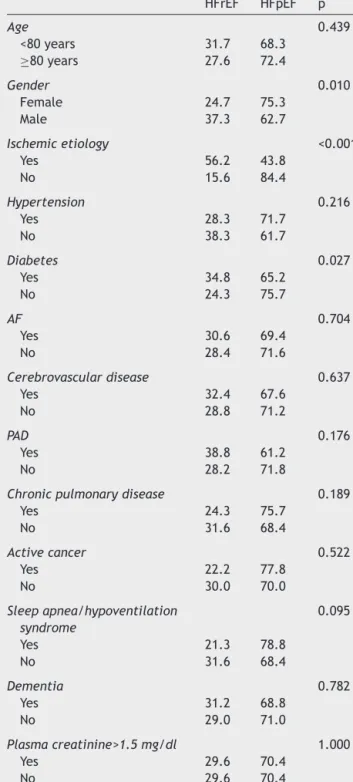
p=0.01).Patientswithdiabetesandthosewithischemicetiologyhadsignificantlyhigher pro-portionsofHFwithreducedejectionfraction(HFrEF)(34.8%vs.24.3%innon-diabeticpatients, p=0.027,and56.2%vs.15.6%forotheretiologies,p<0.001).TheHFrEFgroupweremore fre-quentlydischargedunderbeta-blockersandspironolactone(75.2%vs.46.4%intheHFpEFgroup, p<0.001and31.2%vs.12.6%intheHFpEFgroup,p<0.001,respectively).Mortalitywas34.3% andrehospitalizationforHFwas30.5%inone-yearfollow-up.
Conclusions:Thepopulationcharacterizedisanelderlyone,mainlyfemaleandwithHFpEF. Nearlyathirdofpatientsdiedand/orwererehospitalizedintheyearfollowingdischarge. ©2017SociedadePortuguesadeCardiologia.PublishedbyElsevier Espa˜na, S.L.U.Allrights reserved. PALAVRAS-CHAVE Insuficiência cardíaca; Mortalidade; Hospitalizac¸ão; Reinternamento; Rehospitalizac¸ão
Característicaseprognósticodahospitalizac¸ãoporinsuficiênciacardíacaPRÉviosa umaClínicadeInsuficiênciaCardíaca:estudoPRECIC
Resumo
Objetivo:Caracterizar os doentes hospitalizados por Insuficiência Cardíaca(IC) aguda num Servic¸odeMedicinaInterna,amortalidadeerehospitalizac¸ãoporICnoprimeiroano.
Métodos: Estudoretrospetivoobservacionalincluindotodososdoentescomaltaem2012de hospitalizac¸ãoporICaguda,combaseemNotasdeAlta,registosclínicoseentrevistas tele-fónicas.Reporta-seaoanoprévioàimplementac¸ãodeumaclínicadeIC.
Resultados: Identificaram-se429doentes,comidademédiade79anos;62,5%erammulheres. A comorbilidade e etiologia mais prevalente foi a hipertensão arterial (86,7%) e o fator precipitantemaisfrequente dadescompensac¸ãofoiainfec¸ão.Verificou-seFrac¸ãodeEjec¸ão Preservada(FEp)em70,5%dosdoentes.Amortalidadeintra-hospitalarfoi7,9%.Àalta,a maio-riadosdoentestinhaprescric¸ãodebetabloqueadores(BB)(52,8%)einibidoresdeenzimade conversãodaangiotensina(52%).AsmulheresapresentarammaisfrequentementeFEpdoque oshomens(75,3%versus62,7%,p=0,01).Osdoentesdiabéticoseoscometiologiaisquémica apresentarammaisfrequentementeFrac¸ãodeEjec¸ãoReduzida(FEr)(34,8%versus24,3%em nãodiabéticos,p=0,027e56,2%versus15,6%comoutrasetiologias,p<0,001,respetivamente). NogrupocomFEr,osBBeaespironolactonaforammaisprescritosàalta(75,2%versus46,4% nogrupocomFEp,p<0,001e31,2%versus12,6%nogrupocomFEp,p<0,001,respetivamente). Noprimeiroano,ataxademortalidadefoi34,3%ederehospitalizac¸ãoporIC30,5%.
Conclusões:Apopulac¸ãoestudadaéidosa,predominantementefemininaeapresentaICcom FEp.Umterc¸omorreue/oufoireinternadanoanoseguinte.
©2017SociedadePortuguesadeCardiologia.PublicadoporElsevierEspa˜na,S.L.U.Todosos direitosreservados.
Listofabbreviations
ACE angiotensin-convertingenzyme AF atrialfibrillation
ARB angiotensinreceptorblocker EF ejectionfraction
HF heartfailure
HFpEF heartfailurewithpreservedejectionfraction HFrEF heartfailurewithreducedejectionfraction ICD-9 International Classification of Diseases, 9th
Revision
NIV non-invasiveventilation
NT-proBNP N-terminal-pro-Btypenatriureticpeptide
Introduction
Heart failure (HF) is a major global burden in terms of patients’ quality and duration of life and of health expenditure.1---4 Approximately 1-2% of the adult
popula-tion in developed countrieshas HF, the prevalence rising to ≥10% among those 70 years of age or older.1,5,6 In
Portugal, the overall prevalence of chronic HF was 4.36% inacommunity-basedepidemiologicalsurveycarriedoutin 1998,rising sharplywithage;thiswasslightlyhigherthan thatofotherEuropeancountries.7
Across the globe, 17-45% of patients hospitalized with HFdiewithinayearofhospitalization3,4,8andaquarterare
rehospitalizedwithinonemonthanduptotwo-thirdswithin ayear.1,8---10HFisthemostcommonreasonforhospitalization
in peopleover 65yearsof agein economicallydeveloped regions.6,9,11---13
According to national registries of the Portuguese Directorate-GeneralofHealth,in201418588patientswere hospitalizedfor HFand thein-hospitalmortality ratewas 12.5%.14
The increasing incidence of acute HF and associated morbidityandmortalitymeanthereisanurgentneedto bet-terunderstand this patientpopulation.15 Despite thehigh
prevalence ofacuteHF, few studieshave been conducted specifically in the hospitalized HF population, and data onclinicalcharacteristics andoutcomesforthesepatients are lacking, especially in Portugal. Observational studies provide useful information about real-world patients and routineclinicalpractice.2Interestin thistypeofresearch
hasbeengrowinginrecentdecades,forvariousreasons.4
According to the latest guidelines on heart failure, thestandard-of-care for HFpatients recentlyhospitalized for acute de novo or chronic decompensated HF should includeenrollmentinamultidisciplinarycaremanagement program,5,16alsoknownasaheartfailureclinic.17
Thepresentstudycoverstheyearbeforethe implemen-tation of an HF clinic, using a multidisciplinary approach to HF patients, in a Portuguese tertiary university hospi-tal. The studywasdesigned toimproveknowledge of the characteristics ofpatientshospitalizedandtreatedfor HF in an internal medicine department and to present one-yearfollow-upoutcomes,reportingin-hospitalandone-year mortality and rehospitalization for HF, which will help to evaluatetheimpactofourHFcliniconthoseoutcomes.
Methods
Studydesignandclinicalsetting
Thiswasasingle-centerretrospectiveobservationalstudy. All patients hospitalized in the internal medicine depart-ment of a tertiary university hospital and discharged betweenJanuary1andDecember31,2012wereconsidered forenrollment.Thestudypopulationwasselectedusingthe International Classification of Diseases, 9th Revision (ICD-9)codes,aslistedinthedischargesummary.Alldischarge summariesreportingoneoftheICD-9HFcodes(428,428.0, 428.1,428.2, 428.3,428.4, 428.9,402.01, 402.11,402.91 or398.91)inthefirstthreecodeswerereviewed.Basedon reviewofthedischargesummary,patientswereselectedif theyhad been hospitalized for acute,de novo or chronic decompensatedHFasstated in theirmedicalrecord, and were aged18 yearsor older. HF wasdiagnosedaccording toEuropean SocietyofCardiology guidelines.5 Allpatients
without an echocardiogram had relevant cardiac disease documentedin theirclinical recordand NT-proBNPvalues higherthan1000pg/ml.
For the purposes of the study,the first hospitalization foracuteHFinthestudyperiodwasconsideredtheindex hospitalization.
Datacollection
Datawerecollectedbasedondischargesummaries,medical recordsandtelephoneinterviews.
The following data were collected from the discharge summary: gender, age, risk factors for HF, comorbidities, functionalstatus,HFetiology,decompensationtriggerand treatment. HFcomorbidities considered for analysiswere hypertension, diabetes, cerebrovascular disease, periph-eralarterialdisease,atrial fibrillation(AF),activecancer, chronic lung disease, sleepapnea and/or hypoventilation syndrome,anddementia.
Other clinical records were reviewed for biometric, laboratory,echocardiographic,follow-upand rehospitaliza-tiondata.The etiology ofcardiacdiseasewasestablished throughclinical dataand echocardiography. Only rehospi-talizationsatthestudycenterwereconsidered.
Mortalitydatawereobtainedthroughclinicalrecordsand telephoneinterviews.
Outcomes
The main outcomeswere the characteristics of the study population, namely age, gender, comorbidities, HF risk factors and etiology, HF decompensation trigger, left ventricularejectionfraction(EF),in-hospitalmortality, dis-chargetreatments,rehospitalizationfordecompensatedHF anddeathin the year following discharge fromtheindex hospitalization.
Studyoversight
The two lead authors prepared the manuscript, and all authorsreviewedit.Alltheauthorsvouchfortheaccuracy andcompletenessofthedataandanalysis.
Statisticalanalysis
Categoricalvariables arepresented aspercentages, while continuousvariablesarepresentedasmeansandstandard deviation (SD)plus median andinterquartile range (IQR). Proportionswerecomparedusingthechi-squaretestfor cat-egorical variables. The statistical analysis was performed usingSPSSforWindows,version22.
Results
Patientsandcomorbidities
Inthe study period429 patientswere identifiedand ana-lyzed,asdepicted in Figure 1.The characteristics of the studygrouparereportedinTable1.Meanagewas79years andthemajorityofpatientswerefemale(62.5%).Themost prevalentcomorbiditywashypertension,followedbyAFand diabetes.
Onaverage,eachpatienthadthreecomorbidities.Athird ofpatientshadmorethanthreecomorbidities.
Regarding functional ability, 96 patients (22.4%) had severedisability,beingcompletelydependentonacaregiver fortheirdailyneeds.
626 discharge summaries reporting one HF ICD-9 code in
the first three
429 patients admitted for acute HF
3746 hospitalized patients
Figure1 Flowdiagramofpatientenrollment.Thedatarefer toadmissionstotheinternalmedicinedepartmentinthestudy period.HF:heartfailure;ICD-9:InternationalClassificationof Diseases,9thRevision.
Heartfailure
IschemicetiologyofHFwasrecordedin139patients(34.6%) andvalvediseaseinmorethan74(18.4%),ofwhichsevere aorticstenosiswasthemostcommon,foundin27patients
(6.7%)(datanotshown).Anechocardiogramwasavailablein 400patients,mostofthemwithHFwithpreservedejection fraction(HFpEF) (70.5%),definedasEF >40%,andonly 36 patients(9%)hadEF≤25%.
ThemostfrequentHFdecompensationtriggerwas infec-tion,followedbynon-adherencetotreatment andrhythm disturbances(Table1).Atriggerwasnotfoundinonlytwo cases.
Non-invasiveventilation
Duringhospitalstay,80patients(18.6%)weretreatedwith non-invasiveventilation(NIV),51%ofwhomwerenot diag-nosedwithsleepapnea/hypoventilationsyndrome. Dischargemedication
Atdischarge,394patientswerealiveandprescribed appro-priate cardiovascularmedications,asreportedinTable 2. About half of the patients discharged were prescribed a beta-blocker andan angiotensin-converting enzyme (ACE) inhibitor or an angiotensin receptor blocker (ARB). Beta-blockers wereprescribedsignificantlymorefrequentlyfor patientswithHFwithreducedejectionfraction(HFrEF)but ACEinhibitors/ARBswerenot.
Oral anticoagulants were prescribed for 118 (29.9%) patients, mainly to the 201 patients with a history of AF
Table1 Characteristicsofthestudypopulation.
n
Age(years),mean±SD;median(IQR) 79±10;81(11) 429
Female,% 62.5 429
Ischemicetiology,% 34.6 402
AdmissionSBP(mmHg),mean±SD;median(IQR) 139.5±29.2;136(36) 420
Ejectionfraction>40%,% 70.5 400
Hypertension,% 86.7 429
Diabetes,% 47.8 429
AF,% 51.7 429
Cerebrovasculardisease,% 19.1 429
Peripheralarterialdisease,% 11.7 429
Chronicpulmonarydisease,% 28 429
Activecancer,% 6.8 429
Sleepapnea/hypoventilationsyndrome,% 19.3 429
Dementia,% 24.7 429 >3comorbidities,% 31.9 429 Physicallyactive,% 77.6 429 HFdecompensationtrigger 429 Infection,% 39.4 Non-adherencetotreatment,% 17.5 Rhythmdisturbances,% 16.1 Anemia,% 4.9 Plasmacreatinine>1.5(mg/dl)%) 30.8 428
Admissionplasmacreatinine(mg/dl),mean±SD;median(IQR) 1.3±0.6;1.2(0.78) 428
Admissionsodium(mmol/l),mean±SD;median(IQR) 136.4±5.7;137(6) 428
Hemoglobin(g/dl),mean±SD;median(IQR) 12±2.1;12(2.8) 429
FirstNT-proBNP(pg/ml) 6698±10848;2697(6105) 366
AF:atrialfibrillation;IQR:interquartilerange;NT-proBNP:N-terminal-pro-Btypenatriureticpeptide;SBP:systolicbloodpressure;SD: standarddeviation.
Table2 Medicationsprescribed atdischargefor the394 patientsdischargedalive.
Patients
Drug
All HFrEFa HFpEFa p
Beta-blocker 52.8 75.2 46.4 <0.001
ACEinhibitor/ARB 52.0 58.7 51.3 0.237 Spironolactone 17.3 31.2 12.6 <0.001 Anticoagulant 29.9
ACE:angiotensin-convertingenzyme;ARB:angiotensinreceptor blocker;HFpEF:heartfailurewithpreservedejectionfraction; HFrEF:heartfailurewithreducedejectionfraction.
Valuesrefertopercentageofpatientsdischargedineachgroup.
a Ejectionfractionwasavailablein400patients.
(83.1%), of whom 48.8% had anticoagulants prescribedat discharge, while only 10.4% of those without AF received anticoagulation (p<0.001). This represents 20 patients anticoagulated for reasons other than AF, mainly arte-rialperipheraldisease,venousthromboembolism,previous ischemic stroke or mechanical prosthetic cardiac valves; onlytwohada historyof intracardiacthrombus(datanot shown).Thesmallnumberofpatientspreventsfurther sta-tisticalanalysis.
Relationbetweenejectionfractionandother clinicalcharacteristics
TherelationsbetweenEFandcharacteristicsincludingage, gender, HF etiology, comorbidities, plasma creatinine at admissionandHFdrugtherapyprescribedatdischargeare presentedinTable3.Womenpresentedasignificantlyhigher proportionofHFpEFthanmen.
Patients with diabetes and those with ischemic etiol-ogyhadsignificantlyhigherproportionsofHFrEF.TheHFrEF group weremorefrequently prescribedbeta-blockers and spironolactoneatdischarge(Table2).Age,other comorbidi-tiesandplasmacreatinineatadmissionwerefoundtohave nostatisticalrelationwithEF.
Follow-upoutcomes
In-hospitalmortalitywas7.9%.Mortalityinone-year follow-upwas34.3%(Figure2A).Onepatientwaslosttofollow-up afterdischarge.Thecauseofdeathwasestablishedin136 patients(92.5%of deaths)andacardiovascularcausewas foundin42.9%(datanotshown).
RehospitalizationatleastonceforHFoccurredin30.5% ofpatientsduringthefirstyearoffollow-up,withinamedian of86days(IQR176)afterdischarge(Figure2B).Thenumber ofrehospitalizationsperpatientrangedbetweenoneandsix (Table4).
Duringthefirstyearoffollow-upafterdischarge,62%of patientshadanoutpatientappointmentwithacardiologist oraninternistinourhospital.Itwasnotdeterminedwhich patientswerefollowedpreviouslybyoneofthese special-tiesorwhethertheappointmentwasscheduledpriortothe HFhospitalization.Themediantimebetweendischargeand appointmentwas63days(IQR64.5).
Table 3 Relation between ejection fraction and other characteristics. HFrEF HFpEF p Age 0.439 <80years 31.7 68.3 ≥80years 27.6 72.4 Gender 0.010 Female 24.7 75.3 Male 37.3 62.7 Ischemicetiology <0.001 Yes 56.2 43.8 No 15.6 84.4 Hypertension 0.216 Yes 28.3 71.7 No 38.3 61.7 Diabetes 0.027 Yes 34.8 65.2 No 24.3 75.7 AF 0.704 Yes 30.6 69.4 No 28.4 71.6 Cerebrovasculardisease 0.637 Yes 32.4 67.6 No 28.8 71.2 PAD 0.176 Yes 38.8 61.2 No 28.2 71.8
Chronicpulmonarydisease 0.189
Yes 24.3 75.7 No 31.6 68.4 Activecancer 0.522 Yes 22.2 77.8 No 30.0 70.0 Sleepapnea/hypoventilation syndrome 0.095 Yes 21.3 78.8 No 31.6 68.4 Dementia 0.782 Yes 31.2 68.8 No 29.0 71.0 Plasmacreatinine>1.5mg/dl 1.000 Yes 29.6 70.4 No 29.6 70.4
AF:atrialfibrillation;PAD:peripheralarterialdisease. Data on 400 patients with ejection fraction estimated by echocardiography.Valuesrefertopercentageofpatientsineach group.
Regarding potential admission to our HF clinic, 73% of patients were considered candidates. Referral to the clinic is considered for all patients hospitalized for acute HF. Exclusion criteria are total dependence on caregivers for basic daily needs and inability to communicate.
1.0 0.8 0.6 0.4 Cum ulativ e sur viv al Cum ulativ e sur viv al 0.2 0.0 1.0 0.8 0.6 0.4 0.2 0.0 0 30 61 91 122 152 183 213 Time (days) 244 274 304 335 365 0 30 61 91 122 152 182 213 Time (days) 243 274 304 334 365 First rehospitalization Mortality after discharge
A
B
Figure2 Kaplan-Meiercurvesfortimetodeath(A)and rehos-pitalizationforheartfailure(B).
Table4 Readmissionsforacuteorchronicdecompensated heartfailureduringfollow-up.
No.ofreadmissions Patients(n)
1 77 2 38 3 9 4 3 5 3 6 1 Total 131
Dataon394patientsdischargedalive.
Discussion
Themainresultsofthisstudyconsistoftheclinicalfindings of a large population hospitalized for HF in the inter-nalmedicine departmentof atertiaryuniversity hospital. In Portuguese hospitals, many HF patients aretreated by internists, even in hospitals where there is a cardiology department,18,19sothisisareal-worldsurvey,enrollingall
patientsdischargedfollowing hospitalizationdue toacute orchronicdecompensatedHFduringaone-yearperiod.
Ourpatientsareolder,morefrequentlyfemaleandmore oftenwithHFpEFthanHFpatientsinotherseries,whotend tobemainlyhospitalizedincardiologydepartments.2,4The
mean age is similar to that reported in a recent French single-day surveyin 170hospitals of allpatients hospital-ized for acute HF,13 but 10 years older than in a recent
Portuguese study enrolling patients hospitalizedfor acute HFonlyinthecardiologydepartmentoftheothertertiary universityhospitalinthecitywhere ourstudytookplace. In that study 73.2% of patients had HFrEF, which reflects considerable differences between the two study popula-tionsandisevidenceofhowobservational studiesprovide valuableinformationabout acuteHFmanagedindifferent clinicalscenarios.20,21Ourdataongenderareinagreement
withother reports showing that elderlypatients hospital-ized with HF are mainly women22 and that patients with
HFpEF are older and more often female than those with HFrEF.1,5,6,8,13 HFpatients managedby internists aremore
likelytohavethecharacteristicsofthosemanagedby gen-eralpractitioners.IntheUK,themeanageofHFpatients ingeneralpracticeis77years,similartothatofour popu-lation.TheHFpatientseeningeneralpracticeisgenerally 15 yearsolder, more often female,more likelyto have a historyofhypertensionandlesslikelytohavehad myocar-dialinfarctionthantheHFpatientseenbyacardiologist.1,6
It has been shown that in Portugal chronic HFpEF mainly affectsolder women7andthat patientsagedover 75
hos-pitalizedforacuteHFinaninternal medicinedepartment mainlyhaveHFpEF.19
Theaverageofthreecomorbiditiesperpatientshowsthe complexityofthispopulationandisinagreementwithdata onolderpeoplewithHFin theUSA.16 Ofnote,the
preva-lences ofthetwocommonest comorbidities,hypertension anddiabetes,inourstudyweresimilartothatreport;this is notthecase forAF,which wastwice ascommonin the presentstudy.16Patientswithmorethanthreecomorbidities
haveahigherriskofdeathandHFhospitalization,asshown by vanDeursen etal.,23 althoughin their studyonly
non-cardiovascularcomorbiditieswereanalyzed.Anotherstudy, onincidentHF,reportedthatpatientswithHFpEFweremore likelytohavebothcardiacandnon-cardiaccomorbidities.24
AFandahistoryofhypertensionweremoreprevalentin thisstudypopulationthaninothersinwhichHFrEFwasmore prevalentthanHFpEFandpatientswereenrolledin cardiol-ogywards.2,4ThisisconsistentwiththeliteratureonHFpEF
populationsandwithdataonPortugueseHFpatients.4,19,25
Hypertension was the main etiology for HF, according toitsprevalencein thispopulation, buttheretrospective natureofthestudyandthenon-invasivediagnosticmethods usedfordeterminingHFetiologypreventfurtheranalysis.
An ischemic etiology was less prevalent (34.6%) than reported by the above-cited European observational tri-als, which includedmostly HFrEFpatients (42%-50.7%),as expected.1,3,4,13 It is knownthat patients withHFpEF are
less likelytohavecoronaryheart disease andmorelikely tohave hypertensionandAFthanthosewithHFrEF.5,6 We
confirmedthatischemicHFpatientsmoreoftenhadHFrEF. Thepatientcharacteristicsinthisstudyweresimilarto thosereportedby aSpanish heartfailureunit ina recent paperfromtheinternalmedicinedepartmentofatertiary referralhospital,whichdescribesanelderlypopulationwith ameanageof80.3years,ofwhom54.8%werefemale,72.2%
hadHFpEF(≥50%accordingtothecriteriaofthisstudy)and themainetiologieswereischemicandhypertensiveinthe HFpEFgroupandischemicintheHFrEFgroup.26
InfectionwasthemostfrequenttriggerofHF decompen-sationinourstudy,ashasbeenfound inotherPortuguese andEuropeansurveys.7,13,25
Inadditiontothesignificantcorrelation betweensleep apnea/hypoventilationsyndromeandtreatmentbyNIV dur-ing hospitalization, it is noteworthy that the numbers of patients undergoing NIV with and without one of these diagnosesweresimilar.This probablymeansthatrelieving acutepulmonary congestion andimproving pulmonary gas exchangewerethemaintreatmentgoalsinalargenumber ofthosetreatedwithNIV.
Ourin-hospitalmortalitywasdouble(7.9%)thatreported inalargeEuropeanobservationalsurvey(3.8%)2andinaUS
registry(4.0%)27 but similartothatreportedin other
Por-tuguesestudiesandinItalianandFrenchsurveys(7.7%,6.9% and8.2%,respectively).4,13,25
Pharmacological treatmentat dischargeshouldbe con-sidered in the light of the prevalence of HFpEF in this population.Bearinginmindthatnodrugtherapyhasbeen proved to change prognosis in the HFpEF phenotype,5,16
it is interesting to see that half of the patients were prescribed beta-blockers or ACE inhibitors. This propor-tion is similartothat reported in the OFICAstudy in the HFpEF subgroup, in which 44.2% and 47.3% of this group ofpatientsweredischargedunderACEinhibitorsand beta-blockers,respectively.13Thisreflectstheuseofthesedrug
classesinHFpEFpatientswiththeaimofcontrollingblood pressureandventricularrateinAFanddecreasing hospital-izations.Ceiaetal.foundthattherapywithACEinhibitors inPortuguesechronicHFpatientswasalsosimilarbetween patientswithHFpEFandHFrEF.28
Ourfindingthatbeta-blockersandspironolactonewere moreoftenprescribedforHFrEFpatientsshowsadherence tocurrent guidelines and their incorporation intoclinical practice.Therateofsuchprescriptionissimilartothatina Europeansurveyforbeta-blockers(75.2%vs.80%)butlower foraldosteroneblockers(31.2%vs.52%).2
The total one-year mortality was higher than that reportedfromthesameEuropeanregion(34.3%vs.24.7%)by Maggionietal.intheESC-HFPilotsurveyfortheperiod 2009-2010andinanItaliansurvey(24%).2,4Cardiovascularcauses
accounted for half of deaths, a smaller proportion than reportedinotherobservationaltrials,probablybecausethe typeofHFpatientshospitalizedincardiologydepartments aremoreliabletodieofcardiovascularcauses,whilethose hospitalizedininternalmedicinewardsareequallylikelyto dieofothercauses.Inthisrespect,itisnoteworthythatthe patientsinourstudywere10yearsolderandhadahigher prevalence of comorbidities.3,4 Comorbidity was found to
beone of theprime determinants ofprognosis in astudy ofpatientshospitalizedwithHF1 andHFpEFpatientshave
ahigherlikelihoodofnon-cardiovasculardeath,6supporting
ourfindings.
It should be noted that, although it is commonly accepted that the lower the EF the worse the survival,5
in our predominantly HFpEF population neither mortality norrehospitalizationrateswerelower.Thisisinagreement withother hospital-based studies of patients hospitalized withHF that reported similarone-year mortality rates in
patientswithHFpEFcomparedtothosewithHFrEF,1,6 but
notwiththeOFICAstudy,whichreportedhighermortality intheHFrEFpopulation.13
The rehospitalization rate for HF in the first year of follow-up was similar in this study to that found for the sameEuropean regionin thepreviously mentioned survey (30.5%vs.33.9%,respectively).Ofnote,thehighestratesof mortalityandrehospitalizationforHFwereobservedinthis region,incomparisonwiththreeotherEuropeanregions.3,4
BearinginmindthedifferencesinprevalenceofHFpEF,this isinagreementwithstudiesreportingthatHFpEFpatients areaslikelytoberehospitalizedasHFrEFpatients.6
The median time between discharge and first follow-upappointment wasmuch longer than therecommended 7-14days,16asituationthatweexpecttochangedrastically
withtheimplementationofourheartfailureclinic. ToourknowledgethisisthelargestPortuguese observa-tionalstudy of patientshospitalized for HF, andthe most recent.
Our findings should be considered in the context of several limitations. This was a retrospective registry and didnot include all patients hospitalized for HF, including thoseadmitted to the cardiology department of our hos-pital.Unmeasured variables may have been present that couldhave influencedthefindings.Chronicrenal dysfunc-tionwasnotincluded inthe comorbiditiesbecauseofthe difficultyofascertainingthechronicityofrenaldysfunction insomepatientswithcardiorenalsyndromes. Rehospitaliza-tionswereconsideredonlyatthestudycenter,andthusmay havebeenunderestimated.Wedidnotexaminetheuseof cardiacdevices,althoughthereisunlikelytobeasignificant numberofpatientswithsuchdevices,giventhelow preva-lenceof reducedejectionfractionandtheoldageofthis population.
Conclusions
Thisisoneofthefewpublishedobservationalstudies show-ingthesituationinPortugalintermsof HFhospitalization andoutcomes.Wecharacterizedalarge groupofpatients admittedtoaninternalmedicinedepartmentwithacuteHF: elderly,mostlyfemale,withhypertensionandHFpEF. Dia-beticpatientsandthosewithischemicheartdiseasewere significantlymorelikelytohaveHFrEF.Atdischarge,more thanhalfofpatientswereprescribedbeta-blockersandACE inhibitors/ARBs, and those with HFrEF were significantly more often prescribed beta-blockers and spironolactone. Nearlyathirdof patientsdiedand/orwererehospitalized inthefollowingyear.
Multicenter observational studies in thePortuguese HF populationareanunmetneed.Forthetimebeing,thedata presented here will be helpful tomeasure the impact of theheartfailureclinicatourinstitutioninimportantareas, particularlymortalityandrehospitalizationoutcomes.
Ethical
disclosures
Protection of human and animal subjects.The authors declarethatnoexperimentswereperformedonhumansor animalsforthisstudy.
Confidentialityofdata.Theauthorsdeclarethattheyhave followedtheprotocolsoftheirworkcenteronthe publica-tionofpatientdata.
Right to privacy and informed consent.The authors declarethatnopatientdataappearinthisarticle.
Conflicts
of
interest
Theauthorshavenoconflictsofinteresttodeclare.
Acknowledgments
TheauthorswishtothankJoãoPedroFerreiraforhis contri-butiontothedesignanddatacollectionfor thisstudyand InêsSilveirafordatacollection.
Novartis Pharma supported the statistical analysis throughanunrestrictedgrant.
BetâniaFerreiraiscurrentlyanemployeeofHospitalda LuzArrábida,GrupoLuzSaúde,VilaNovadeGaia,Portugal. SandraNunesiscurrentlyanemployeeofCentroHospitalar EntreDouroeVouga,E.P.E,SantaMariadaFeira,Portugal.
References
1.Mosterd A, HoesAW. Clinical epidemiology of heart failure. Heart.2007;93:1137---46.
2.MaggioniAP,DahlstromU,FilippatosG,etal.EURObservational ResearchProgramme: theHeartFailure PilotSurvey (ESC-HF Pilot).EurJHeartFail.2010;12:1076---84.
3.MaggioniAP,DahlstromU,FilippatosG,etal.EURObservational ResearchProgramme:regionaldifferencesand1-yearfollow-up resultsoftheHeartFailurePilotSurvey(ESC-HFPilot).EurJ HeartFail.2013;15:808---17.
4.Tavazzi L, Senni M, MetraM, et al. Multicenterprospective observationalstudyonacuteandchronicheartfailure:one-year follow-upresultsofIN-HF (Italian NetworkonHeart Failure) outcomeregistry.CircHeartFail.2013;6:473---81.
5.McMurrayJJV,AdamopoulosS,AnkerSD,etal.ESCGuidelines forthediagnosisandtreatmentofacuteandchronicheart fail-ure2012.EurHeartJ.2012;33:1787---847.
6.LamCSP,DonalE,Kraigher-KrainerE,etal.Epidemiologyand clinicalcourseofheartfailurewithpreservedejectionfraction. EurJHeartFail.2011;13:18---28.
7.CeiaF,FonsecaC,MotaT,etal.,onbehalfoftheEPICA Inves-tigators. Prevalenceofchronic heartfailurein Southwestern Europe:theEPICAstudy.EurJHeartFail.2002;4:531---9. 8.Ponikowski P, Anker SD, AlHabib KF, et al. Heart failure:
preventing disease and deathworldwide. ESC Heart Failure. 2014;1:4---25.
9.CowieMR,AnkerSD,ClelandJ,etal.Improvingcareforpatients withacuteheartfailure:before,duringandafter hospitaliza-tion.ESCHeartFailure.2014;1:110---45.
10.Dunbar-YaffeR,StittA,LeeJJ,etal.Assessingriskand preven-ting30-dayrehospitalizationsindecompensatedheartfailure: opportunitytointervene?CurrHeartFailRep.2015;12:309---17.
11.Rodriguez-ArtalejoF,BanegasJRB,Guallar-CastillonP. Epidemi-ologyofheartfailure.RevEspCardiol.2004;57:163---70. 12.HallMJ,LevantS, DeFrancesCJ. Hospitalizationfor
conges-tiveheartfailure:UnitedStates,2000-2010.NCHSDataBrief. 2012:1---8.
13.LogeartD,IsnardR,Resche-RigonM,etal.,onbehalfofthe workinggrouponHeartFailureoftheFrenchSocietyof Cardi-ology.Currentaspectsofthespectrumofacuteheartfailure syndromesinareal-lifesetting:theOFICAstudy.EurJHeart Fail.2013;15:465---76.
14.Portugal --- Doenc¸as Cérebro-Cardiovasculares em numer-ous---2015. Availableat: www.dgs.pt/em-destaque/portugal-doencas-cerebro-cardiovasculares-em-numeros-201511.aspx. 15.AbrahamWT,FonarowGC,AlbertNM,etal.TheOPTIMIZE-HF
InvestigatorsandCoordinators,Predictorsofin-hospital mortal-ityinpatientshospitalizedforheartfailure.JAmCollCardiol. 2008;52:347---56.
16.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/AmericanHeartAssociationTaskForceonpractice guidelines.Circulation.2013;128:1810---52.
17.HauptmanPJ,RichMW,HeidenreichPA,etal.Theheartfailure clinic:aconsensusstatementoftheHeartFailureSocietyof America.JCardiacFail.2008;14:801---15.
18.CeiaF,FonsecaC,BritoD,et al.Heartfailure treatmentin Portuguese hospitals: results of a survey. Rev Port Cardiol. 2001;20:1259---66.
19.FonsecaC,CeiaF,BritoD,etal.Howpatientsaremanagedin Portugal.EurJHeartFail.2002;4:563---6.
20.Pinho-GomesAC,SilvaCardosoJ,AzevedoLF,etal. Character-izationofacuteheartfailurehospitalizationsinaPortuguese cardiologydepartment.RevPortCardiol.2013;32:567---75. 21.BritoD.ProfileoftheacuteheartfailurepatientinPortugal.
RevPortCardiol.2013;32:577---9.
22.NieminenMS,Harjola VP,HochadelM,etal. Genderrelated differences in patients presenting with acute heart failure. Results from EuroHeart Failure Survey II. Eur J Heart Fail. 2008;10:140---8.
23.vanDeursenVM,UrsoR, LarocheC,et al.Co-morbiditiesin patientswithheartfailure:ananalysisoftheEuropeanHeart FailurePilotSurvey.EurJHeartFail.2014;16:103---11. 24.GurwitzJH,MagidDJ,SmithDH,etal.Contemporary
preva-lenceandcorrelatesofincidentheartfailurewithpreserved ejectionfraction.AmJMed.2013;126:393---400.
25.SarmentoPM,FonsecaC,MarquesF,etal.InsuficiênciaCardíaca Aguda:Característicasde uma Populac¸ãoHospitalare Opor-tunidades paraa Melhoriados Cuidados Prestados. Rev Port Cardiol.2006;25:2---13.
26.Martínez-BrãnaL,Mateo-MosqueraL,Bermúdez-RamosM,etal. Clinicalcharacteristicsandprognosisofheartfailureinelderly patients.RevPortCardiol.2015;34:457---63.
27.FonarowGC,AdamsKFJr,AbrahamWT,etal.,fortheADHERE ScientificAdvisoryCommittee,StudyGroup,andInvestigators. Riskstratificationforin-hospitalmortalityinacutely decompen-satedheartfailure:classificationandregressiontreeanalysis. JAMA.2005;293:572---80.
28.CeiaF,FonsecaC,MotaT,etal.Aetiology,comorbidityanddrug therapyofchronicheartfailureintherealworld:theEPICA substudy.EurJHeartFail.2004;6:801---6.