w w w . e l s e v i e r . c o m / l o c a t e / b j i d
The
Brazilian
Journal
of
INFECTIOUS
DISEASES
Brief
communication
Does
SOFA
predict
outcomes
better
than
SIRS
in
Brazilian
ICU
patients
with
suspected
infection?
A
retrospective
cohort
study
Regis
Goulart
Rosa
a,∗,
Rafael
Barberena
Moraes
b,
Thiago
Costa
Lisboa
b,
Daniel
Pretto
Schunemann
c,
Cassiano
Teixeira
aaHospitalMoinhosdeVento,DepartamentodeCuidadosIntensivos,PortoAlegre,RS,Brazil
bHospitaldeClínicasdePortoAlegre,DepartamentodeCuidadosIntensivos,PortoAlegre,RS,Brazil
cHospitalMoinhosdeVento,DepartamentodeMedicinaInterna,PortoAlegre,RS,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received4July2017 Accepted26September2017 Availableonline13October2017
Keywords:
Sepsis
Intensivecareunit Organdysfunction Outcomes
a
b
s
t
r
a
c
t
Wecomparedthediscriminatorycapacityofthesequentialorganfailureassessment(SOFA) versusthesystemicinflammatoryresponsesyndrome(SIRS)scoreforpredictingICU mor-tality,needforandlengthofmechanicalventilation,ICUstay,andhospitalizationinpatients withsuspectedinfectionadmittedtoamixedBrazilianICU.Weperformedaretrospective analysisofalongitudinalICUdatabasefromatertiaryhospitalinSouthernBrazil.Patients werecategorizedaccordingtowhethertheymetthecriteriaforsepsisaccordingtoSOFA (variation≥2pointsoverthebaselineclinicalcondition)andSIRS(SIRSscore≥2points).
FromJanuary2008toDecember2014,1487patientswereadmittedtotheICUdueto sus-pectedinfection.SOFA≥2identifiedmoreseptic patientsthanSIRS≥2(79.0%[n=1175] vs.68.5%[n=1020],p<0.001).Therewasnodifferencebetweenthetwoscoresin predict-ingICUmortality(areaunderthereceiveroperatingcharacteristiccurve(AUROC)=0.64vs. 0.64,p=0.99).SOFA≥2wasmarginallybetterthanSIRS≥2inpredictingneedfor
mechan-icalventilation(AUROC=0.64vs.0.62,p=0.001),ICUstay>7days(AUROC=0.65vs.0.63,
p=0.004),andlengthofhospitalization>10days(AUROC=0.61vs.0.59,p<0.001).Therewas nodifferencebetweenthetwoscoresinpredictingmechanicalventilation>7days.
©2017SociedadeBrasileiradeInfectologia.PublishedbyElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/ by-nc-nd/4.0/).
Sepsis results in significant mortality,1–3 morbidity, and resourceutilizationduringandaftercriticalillnesses.4
ThepreviousconsensusdefinitionsofSepsis(Sepsis-1and Sepsis-2)5,6reliedonthesystemicinflammatoryresponse
syn-∗ Correspondingauthor.
E-mailaddress:regis.rosa@hmv.org.br(R.G.Rosa).
drome(SIRS)toinfectionasafundamentalaspectofsepsis diagnosis.In2016,theSepsis-3definitionchangedthefocus from thepresenceofinfection-relatedSIRStothepresence ofinfection-relatedorgandysfunction.7Thenewconsensus wasmainlysupportedbytheretrospectivestudybySeymor etal.,8whichshowedthatsequentialorganfailureassessment (SOFA)resultedinbetterpredictiveaccuracyformortalitythan SIRSamongUSandEuropeanICUpatients.
http://dx.doi.org/10.1016/j.bjid.2017.09.002
However,somehealthcaresocieties9andexperts10 have expresseddisappointmentwiththenewrecommendations, mainlyduetothelackofstudiesontheperformanceofthe organ dysfunctionscores indeveloping countries. Thus, to safelyadoptthenewcriteriaproposedbySepsis-3inabroader context,it isnecessary tovalidateit inscenariosdifferent fromthoseoriginallytested.Inaddition,otheroutcomes rele-vanttocriticalcarepatientsbesidesdeathshouldbeassessed. Therefore,weaimedtocomparethediscriminatorycapacity ofSOFAversusSIRSforpredictingrelevantoutcomesamong adultpatientsadmittedtoamixedintensivecareunit(ICU)of atertiaryhospitalinSouthernBrazilduetosuspected infec-tion.
Weperformedaretrospectiveanalysisofacomprehensive prospectivelycollectedlongitudinalICUdatabasecomposed of4221patientsadmittedtothe31-bedmixedICUofHospital MoinhosdeVento,PortoAlegre, Brazil,overa7-yearperiod (January2008toDecember2014).Thisstudywasapprovedby theResearchEthicsCommitteeatHospitalMoinhosdeVento. Theneedforinformedconsentwaswaived.Allpatientswith suspectedinfectionsatICUadmissionwereconsidered eligi-bleforthestudy.Patientswereidentifiedusinginfection,sepsis,
severesepsis,septicshock,pneumonia,urinarytractinfection, blood-streaminfection,intra-abdominalinfection,centralnervoussystem infection, osteoarticularinfection,and skin andsoft tissue infec-tionassearchtermsinthesyndromicdiagnosis fieldofthe database.
Theexposurevariableswerediagnosisofsepsisaccording toSOFAandSIRSdefinitionsatICUadmission.Patientswere classifiedas havingsepsisaccordingtoSOFAif theyhad a scorevariation≥2pointsoverthebaselineclinicalcondition.7
TheSOFAwasassumedtobezeroinpatientsnotknownto havepreexistingorgandysfunction.Inpatientswithchronic organdysfunction,thebaselineSOFAwasassumedtobe4in patientsundergoingchronicrenalreplacementtherapy,and2, 3or4inpatientswithcirrhosis,dependingonbaseline biliru-binlevels.Patientswereclassifiedashavingsepsisaccording toSIRSiftheypresentedatleasttwoofthefollowingsigns ofsystemicinflammation:temperature>38◦Cor<36◦C,heart
rate>90 beats per minute,respiratory rate>20 breaths per minuteorPaCO2<32mmHg,abnormalwhitebloodcellcount (>12,000/Lor<4000/Lor>10%immatureforms).5Inorderto
evaluatetheprognosisofpatientsaccordingtothepresence or absenceoforgan dysfunction (SOFAvariation≥2points
overthebaselineclinicalcondition)andSIRS(SIRSscore≥2
points)wecreatedfourgroups:(1)patientswithorgan dys-functionand SIRS;(2)patientswithSIRSbutwithoutorgan dysfunction;(3)patientswithorgandysfunctionbutwithout SIRS;and(4)patientswithinfection,butwithneitherSIRSnor organdysfunction.
Theoutcomesevaluatedwereall-causeICUmortality,need andlengthofforinvasivemechanicalventilation(MV),length ofICUstay,andlengthofhospitalization.ProlongedMV,ICU stay,and hospitalization weredefined asduration ofthese variablesabovethe75thpercentileofthestudiedpopulation. Theaccuracyofthedifferent sepsisdefinitions for predict-ingtheseoutcomeswasevaluatedthroughtheareaunderthe receiveroperatingcharacteristic(ROC) curve (AUROC). Uni-variatemodelingofthetwodefinitionswascomparedusing
theChi-squaredtest.Acomparisonofoutcomesamongthe study groups was made using the Kruskal–Wallis test for continuousvariablesand thePearson’sChi-squaredtestfor dichotomous variables. Among post hoc tests, Dunn’s test wasappliedaftertheKruskal–Wallistest,andBonferroni cor-rection wasappliedafterthe Pearson’sChi-squared test.A significance level of0.05 was adopted forall comparisons. Statav.12(StataCorpLP,CollegeStation,TX,USA)wasused forstatisticalanalysis.
SOFA≥2identifiedahighernumberofsepticpatientsin
comparisontotheSIRS≥2(79.0%[n=1175]vs.68.5%[n=1020], p<0.001).Baselinecharacteristicsofpatientsaccordingtothe differentdefinitionsofsepsiswere comparable.There were no statistical differences in the proportionofmales (SOFA
≥2, 55.6% vs. SIRS ≥2, 54.0%), median age (SOFA≥2, 75.0
[interquartile range{IQR}, 63.0–83.0]vs. SIRS≥2,75.0 [IQR,
63.0–83.0]), mediannumber ofcomorbidities (SOFA≥2, 3.0
[IQR,2.0–4.0]vs.SIRS≥2,3.0[IQR,2.0–4.0]),median
APACHE-IIscoreatICU admission(SOFA≥2,21.0[IQR,16.0–25.0]vs.
SIRS≥2,21.0[IQR,16.0–26.0]),andmedianSOFAscoreatICU
admission(SOFA≥2,5.0[IQR,3.0–8.0]vs.SIRS≥2:5.0[IQR,
3.0–8.0]).
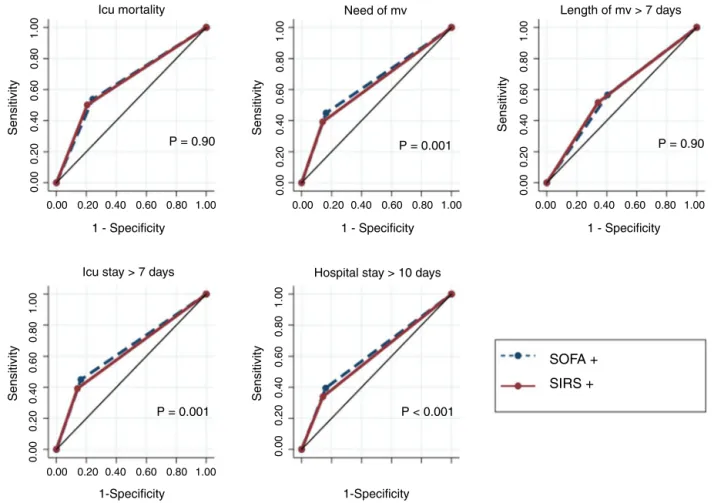
Acomparisonofthepredictiveaccuracyforthestudy out-comesbetweenSOFA≥2andSIRS≥2isshowninFig.1.SOFA ≥2andSIRS≥2showedsimilardiscriminatorycapacityforICU
mortality(AUROC0.64[0.62–0.67]vs.0.64[0.62–0.67],p=0.99). SOFA≥2hadamarginallybetterdiscriminatorycapacitythan
SIRS≥2forneedforMV(AUROC0.64[95%CI,0.62–0.65]vs.
0.62[95%CI,0.61–0.63],p=0.001),lengthofICUstay>7days (AUROC 0.65 [95%CI,0.63–0.66] vs.0.63 [95%CI,0.62–0.64],
p=0.004),andlengthofhospitalization>10days(AUROC0.61 [95%CI,0.60–0.63]vs.0.59[95%CI,0.58–0.61],p<0.001).There wasnodifferencebetweenthescoresintermsofthe predict-inglengthofMV>7days.
Table 1shows acomparisonofthe outcomes according to thepresenceor absence oforgan dysfunctionand SIRS. Patients with both organ dysfunction and SIRS had worst outcomescomparedtopatientsofothergroups:higherICU mortality,higherneedofMV,andlongerICUstay.The com-parisonofoutcomesamongpatientswithSIRSbut without organ dysfunctionandpatientswithorgan dysfunctionbut withoutSIRSshowednostatisticaldifference.Patientswith neitherorgandysfunctionnorSIRShadbetteroutcomes:lower ratesofmortalityandMVandshorterlengthofICUstayin comparisontopatientsfromothergroups.
InthisstudyconstitutedofBraziliancriticalcarepatients with suspected infections who were admitted to a mixed medical-surgical ICU, the SOFA ≥2 criteria identified more
patientswithsepsisthantheSIRS≥2criteria.Therewasno
differencebetweenthetwoscoresinpredictingICU mortal-ity;however,SOFA≥2showedamarginallybetterpredictive
accuracyforneedforMV, lengthofICUstay,and lengthof hospitalizationincomparisontotheSIRS≥2definition.The
prognosisofpatientsclassifiedashavingsepsisbySOFA≥2
but notbySIRS≥2(n=308),was generallypoorer than the
prognosisofpatientswithinfectionbutwithoutSIRSororgan dysfunction.Conversely,somepatientspreviouslyclassified ashavingsepsisbySIRS≥2werenotcapturedbytheSOFA≥2
Icu mortality
0.00
0.00
0.20
0.20
0.40
0.40
0.60
0.60
0.80
0.80
1.00 0.00 0.20 0.40 0.60 0.80 1.00 0.00 0.20 0.40 0.60 0.80 1.00
0.00
0.20
0.40
0.60
0.80
1.00
0.00
0.20
0.40
0.60
0.80
1.00
0.00 0.20 0.40 0.60 0.80 1.00
1.00
0.00
0.20
0.40
0.60
0.80
1.00
0.00
0.20
0.40
0.60
0.80
1.00
Icu stay > 7 days
P = 0.001 P < 0.001
P = 0.001 P = 0.90
P = 0.90
Hospital stay > 10 days
SOFA
+
SIRS +
Need of mv Length of mv > 7 days
1 - Specificity 1 - Specificity
1-Specificity 1-Specificity
1 - Specificity
Sensitivity
Sensitivity
Sensitivity
Sensitivity Sensitivity
Fig.1–ComparisonofpredictiveaccuracyforoutcomesamongSOFAandSIRScriteriadefiningsepsisin1487criticalcare patientswithinfectionatICUadmission.Abbreviations:AUROC,areaunderreceiveroperatingcharacteristiccurve;CI, confidenceinterval;ICU,intensivecareunit;MV,mechanicalventilation.
Note:SOFA+,patientswithSOFAvariation≥2overtheirbaselineclinicalscores.SIRS+,patientswithatleast2ofthe
followingsignsofSIRS:temperature>38◦Cor<36◦C,heartrate>90beatsperminute,respiratoryrate>20breathsper minuteorPaCO2<32mmHg,abnormalwhitebloodcellcount(>12,000/Lor<4000/Lor>10%immatureforms).
ICUmortality:SOFA+AUROC0.64(95%CI,0.62–0.67);SIRS+AUROC0.64(95%CI,0.62–0.67).NeedforMV:SOFA+AUROC0.64 (95%CI,0.62–0.65);SIRS+AUROC0.62(95%CI,0.61–0.63).LengthofMV>7days:SOFA+AUROC0.57(95%CI,0.55–0.60); SIRS+AUROC0.58(95%CI,0.56–0.61).ICUstay>7days:SOFA+AUROC0.64(95%CI,0.62–0.65);SIRS+AUROC0.62[95%CI, 0.61–0.63).Hospitalstay>10days:SOFA+AUROC0.61(95%CI,0.60–0.63);SIRS+AUROC0.59(95%
CI,0.58–0.61).
incomparisontopatientswithinfectionbutwithoutSIRSor organdysfunction.
SepsisdefinitionsbasedonSIRScriteriahavebeen ques-tioned due to low specificity.11 Critical care patients may presentsignsofSIRSduetodistinctcausesofinfectionsuch assurgery,trauma,inflammatoryconditions,blood transfu-sions,andmedicationuse.12Conversely,immunosuppressed patientsmaynotmanifestSIRSeveninmoreseverecasesof infectionduetoanimpairedhostresponsetopathogens.13
Inthissense,SOFA≥2criteriaidentifiedahighernumber
ofsepticpatientsincomparisontotheSIRS≥2criteria.This
findingmayberelatedtothecharacteristicsofourpopulation, giventhatweevaluatedmainlyolderpatientswitharelevant comorbidityburden.Particularlyinthispopulation,thesigns ofSIRStendtobelessprevalentduetoweakerimmune sys-temactivation.14Thishypothesisissupportedinastudyby Kaukonenetal.,inwhichuptooneineveryeightpatients
withinfectionandorgandysfunctiondidnotmeettheSIRS criteria.15
Raith et al.16 showed that an increase in SOFA score of 2 or more points had a better prognostic accuracy for in-hospital mortality than SIRS criteria amongadultswith suspectedinfectionadmittedtoAustralianandNewZealand ICUs,suggestingthat SIRScriteriamay havelimited utility for predictingmortalityin the critical caresetting. Similar results were foundin a study byCheng et al.,17 in which Sepsis-3 showed better predictive accuracy for in-hospital mortality than Sepsis-1 amongICU patients in China.The BrazilianstudybyBesenetal.18showedthatthenewSepsis-3 definitionsweresuperiortothepreviousdefinitionsin strati-fyingmortalityaswell.Ourstudyfailedtoshowadifference in thepredictive accuracyfor ICUmortality betweenSOFA
≥2criteriaandSIRS≥2criteria;however, thebetter
Table1–ComparisonofoutcomesamongSOFAandSIRScriteriadefiningsepsisin1487criticalcarepatientswith infectionatICUadmission.
Outcomes Group1SIRS+ Group2SIRS+ Group3SIRS− Group3SIRS− Kruskal–Wallisor PearsonChi2
Comparison group
Posthoc p-value SOFA+ SOFA− SOFA+ SOFA−
(n=867) (n=153) (n=308) (n=159)
ICUmortality,%(n) 26.8(233) 16.3(25) 14.2(44) 5.6(9) Chi251.1 1vs.2 0.03
p<0.001 1vs.3 <0.001 1vs.4 <0.001 2vs.3 0.44 2vs.4 0.01 3vs.4 0.03
NeedforMV,%(n) 68.5(594) 45.7(70) 54.2(167) 20.1(32) Chi2144.8 1vs.2 <0.001
p<0.001 1vs.3 <0.001 1vs.4 <0.001 2vs.3 0.18 2vs.4 <0.001 3vs.4 <0.001
LengthofMV,days, median(IQR)
6(3,13) 6(2,11) 4(1,10) 2(1,7) Chi219.3 1vs.2 0.90
p<0.001 1vs.3 0.004 1vs.4 0.002 2vs.3 0.22 2vs.4 0.10 3vs.4 0.32
LengthofICUstay, days,median(IQR)
10(5,19) 7(4,15) 7(4,15) 4(2,9) Chi283.5 1vs.2 <0.001
p<0.001 1vs.3 <0.001 1vs.4 <0.001 2vs.3 0.99 2vs.4 <0.001 3vs.4 <0.001
Lengthof hospitalization, days,median(IQR)
18(10,34) 14(8,29) 16(9,32) 11(7,22) Chi229.9 1vs.2 0.15
p<0.001 1vs.3 0.62 1vs.4 <0.001 2vs.3 0.68 2vs.4 0.42 3vs.4 <0.001
ICU,intensivecareunit;IQR,interquartilerange;MV,mechanicalventilation;SIRS,systemicinflammatoryresponsesyndrome;SOFA,sequential organfailureassessment.
Note:SOFA+,patientswithSOFAvariation≥2overtheirbaselineclinicalscore.SIRS+,patientswithatleast2ofthefollowingsignsofSIRS:
temperature>38◦Cor<36◦C,heartrate>90beatsperminute,respiratoryrate>20breathsperminuteorPaCO
2<32mmHg,abnormalwhite
bloodcellcount(>12,000/Lor<4000/Lor>10%immatureforms).
outcomes(i.e.,needofMV,lengthofICU,andhospitalstay)
indicates that SOFA may bea useful index toassess the
impactoftherapiesonclinicallyand economicallyrelevant outcomesin ICUs.Interestingly,the useofSIRS≥2criteria
identifiedaconsiderablenumberofpatientswithhigh mor-talityrates notclassified as havingsepsis bythe SOFA ≥2
criteria. Also, the use ofSIRS ≥2 in addition to the SOFA
criteriaallowedtheidentificationofasubgroupofpatients
withbothSIRSandorgandysfunction,whichhadtheworst
prognosis.
Somelimitationsmustbeacknowledged.First,a retrospec-tivestudydesignissusceptibletoselectionbias;notablythe useofsearchtermsintheICUdatabaseasastrategyto iden-tifypatientsadmittedduetosuspectedinfectionsmayhave
contributedtoselectionbiasgivenitslowsensitivity.Second, thisstudywasperformedatasinglecenter,whichmaylimit its externalvalidity. Third, wedidnotevaluatethe impact ofthedifferentdefinitionsofsepsisonlong-termoutcomes ofICUpatients.Thestrengthsofourstudyincludethe sub-stantialnumberofpatientsevaluatedandtheassessmentof relevantoutcomesinadditiontomortality.
incriticallyillpatientsinasettingotherthanthoseoriginally published.However,theSIRSscoreisstillimportantin strati-fyingtheseverityofpatientswithinfectionandshouldnotbe abandoned.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgement
TheauthorsthanktheICUteamofHospitalMoinhosdeVento whocreatedthedatabase.
r
e
f
e
r
e
n
c
e
s
1. FleischmannC,ScheragA,AdhikariNK,etal.Assessmentof globalincidenceandmortalityofhospitaltreatedsepsis. Currentestimatesandlimitations.AmJRespirCritCareMed. 2016;193:259–72.
2. AngusDC,Linde-ZwirbleWT,LidickerJ,ClermontG,Carcillo J,PinskyMR.EpidemiologyofseveresepsisintheUnited States:analysisofincidence,outcome,andassociatedcosts ofcare.CritCareMed.2001;29:1303–10.
3. MartinGS,ManninoDM,EatonS,MossM.Theepidemiology ofsepsisintheUnitedStatesfrom1979through2000.NEngl JMed.2003;348:1546–54.
4. KahnJM,BensonNM,ApplebyD,CarsonSS,IwashynaTJ. Long-termacutecarehospitalutilizationaftercriticalillness. JAMA.2010;303:2253–9.
5. BoneRC,BalkRA,CerraFB,etal.Definitionsforsepsisand organfailureandguidelinesfortheuseofinnovative therapiesinsepsis.TheACCP/SCCMconsensusconference committee.Americancollegeofchestphysicians/societyof criticalcaremedicine.Chest.1992;101:1644–55.
6. LevyMM,FinkMP,MarshallJC,etal.
CCM/ESICM/ACCP/ATS/SISinternationalsepsisdefinitions conference.IntensiveCareMed.2003;29:530–8.
7.SingerM,DeutschmanCS,SeymourCW,etal.Thethird internationalconsensusdefinitionsforsepsisandseptic shock(Sepsis-3).JAMA.2016;315:801–10.
8.SeymourCW,LiuVX,IwashynaTJ,etal.Assessmentof clinicalcriteriaforsepsis:forthethirdinternational consensusdefinitionsforsepsisandsepticshock(Sepsis-3). JAMA.2016;315:762–74.
9.MachadoFR,Assunc¸ãoMS,CavalcantiAB,JapiassúAM, AzevedoLC,OliveiraMC.Gettingaconsensus:advantages anddisadvantagesofSepsis-3inthecontextof
middle-incomesettings.RevBrasTerIntensiva. 2016;28:361–5.
10.VincentJL,MartinGS,LevyMM.qSOFAdoesnotreplaceSIRS inthedefinitionofsepsis.CritCare.2016;20:210.
11.VincentJL,OpalSM,MarshallJC,TraceyKJ.Sepsisdefinitions: timeforchange.Lancet.2013;381:774–5.
12.BalkRA.Systemicinflammatoryresponsesyndrome(SIRS): wherediditcomefromandisitstillrelevanttoday? Virulence.2014;5:20–6.
13.SevilleMT,KrystofiakS,KusneS.Infectioncontrolissues aftersolidorgantransplantation.In:BowdenRA,LjungmanP, SnydmanDR,editors.Transplantinfection.Lippincott Williams&Wilkins;2010.p.667–88.
14.CliffordKM,Dy-BoarmanEA,HaaseKK,MaxvillK,PassS, AlvarezCA.Challengeswithdiagnosingandmanagingsepsis inolderadults.ExpertRevAntiInfectTher.2016;14:231–41.
15.KaukonenKM,BaileyM,PilcherD,CooperDJ,BellomoR. Systemicinflammatoryresponsesyndromecriteriain definingseveresepsis.NEnglJMed.2015;372:1629–38.
16.RaithEP,UdyAA,BaileyM,etal.AustralianandNewZealand intensivecaresociety(ANZICS)centreforoutcomesand resourceevaluation(CORE).PrognosticaccuracyoftheSOFA score.SIRSCriteria,andqSOFAscoreforin-hospitalmortality amongadultswithsuspectedinfectionadmittedtothe intensivecareunit.JAMA.2017;317:290–300.
17.ChengB,LiZ,WangJ,etal.Comparisonoftheperformance betweenSepsis-1andSepsis-3inICUsinChina:a
retrospectivemulticenterstudy.Shock.2017[Epubaheadof print].