RevBrasAnestesiol.2017;67(2):180---183
REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologia www.sba.com.brSCIENTIFIC
ARTICLE
Accuracy
of
a
smartphone
to
test
laryngoscope’s
light
and
an
audit
to
our
laryngoscopes
using
an
ISO
standard
Diogo
Alcino
de
Abreu
Ribeiro
Carvalho
Machado
a,∗,
Dina
da
Assunc
¸ão
Azevedo
Esteves
b,
Pedro
Manuel
Araújo
de
Sousa
Branca
aaHospitalPedroHispanoE.P.E.,UnidadeLocaldeSaúdedeMatosinhos,DepartamentodeAnestesia,Matosinhos,Portugal bHospitalPedroHispanoE.P.E.,UnidadeLocaldeSaúdedeMatosinhos,BlocoOperatório,Matosinhos,Portugal
Received29May2016;accepted20July2016 Availableonline17August2016
KEYWORDS
Laryngoscope; Laryngoscopy; Light; Accuracy; Smartphone;
Luxmeter
Abstract
Backgroundandobjectives: Laryngoscopeis akeytool inanesthetic practice. Direct laryn-goscopy is acrucial moment and inadequatelaryngoscope’s light can lead tocatastrophic consequences.From ourexperiencelaryngoscope’s lightisassessed inasubjectivemanner andwe believeamore preciseevaluationshouldbeused.Our objectiveisto comparethe accuracyofasmartphonecomparedtoaluxmeter.SecondlyweauditedourOperatingRoom laryngoscopes.
Methods:Wedesignedapragmaticstudy,usingasprimaryoutcometheaccuracyofa smart-phone compared to the lux meter. Further we audited with both the lux meter and the smartphone all laryngoscopes and blades ready to use in our Operating Rooms, using the InternationalStandardformtheInternationalOrganizationforStandardization.
Results:Forprimaryoutcomewefoundnosignificantdifferencebetweendevices.Ouraudit showed that only2in 48 laryngoscopes complied withthe ISO norm. Whencomparing the measurementsbetweentheluxmeterandthesmartphonewefoundnosignificantdifference.
Discussion: Ideallyeverylaryngoscopeshouldperformasrequired.Webelievealllaryngoscopes shouldhaveapracticalbutreliableandobjectivetestpriortoitsutilization.Ourresultssuggest thesmartphonewasaccurateenoughtobeusedasaluxmeter totestlaryngoscope’slight. Auditresultsshowingonly4%complywiththeISOstandardareconsistentwithotherstudies.
Conclusion:The tested smartphone has enough accuracy to perform light measurementin laryngoscopes. We believe this is a step further to perform an objectiveroutine check to laryngoscope’slight.
©2016PublishedbyElsevierEditoraLtda.onbehalfofSociedadeBrasileiradeAnestesiologia. Thisisanopenaccess articleundertheCCBY-NC-NDlicense(http://creativecommons.org/ licenses/by-nc-nd/4.0/).
∗Correspondingauthor.
E-mail:diogodh@gmail.com(D.A.Machado).
http://dx.doi.org/10.1016/j.bjane.2016.07.007
Accuracyofasmartphonetotestlaryngoscope’slight 181
PALAVRAS-CHAVE
Laringoscópio; Laringoscopia; Luz;
Precisão;
Smartphone; Luxímetro
Precisãodeumsmartphoneparatestaraluzdelaringoscópioeumaauditoria denossoslaringoscópiosusandoasnormasdaISO
Resumo
Justificativaeobjetivo: Olaringoscópioéumaferramentaessencialnapráticaanestésica.A laringoscopiadiretaéummomentocrucialeumaluzinadequadadolaringoscópiopodelevara consequênciascatastróficas.Deacordocomnossaspesquisas,aluzdolaringoscópioéavaliada deformasubjetivaeacreditamosqueumaavaliac¸ãomaisprecisadeveserfeita.Nosso obje-tivofoicompararaprecisãodeumsmartphonecomadeumluxímetro.Depois,fizemosuma auditoriadenossoslaringoscópiosemsaladeoperac¸ão.
Métodos: Estudopragmáticousandocomodesfechoprimárioaprecisãodeumsmartphoneem comparac¸ãocomadeumluxímetro.Subsequentemente,fizemosumaauditoriatantocomo luxímetroquantocomosmartphonedetodososlaringoscópioselâminasprontosparausoem nossassalas decirurgia,usandoasnormasdaInternationalOrganization forStandardization (ISO).
Resultados: Paraodesfechoprimárionãoencontramosdiferenc¸asignificativaentreos disposi-tivos.Nossaauditoriamostrouqueapenasdoisem48laringoscópiossatisfizeramasnormasda ISO.Aocompararasmensurac¸õesentreoluxímetroeosmartphone,nãoencontramosdiferenc¸a significativa.
Discussão: Idealmente,todososlaringoscópiosdeviamfuncionarconformeprevisto. Acredita-mosquetodos oslaringoscópiosdevemsersubmetidos aum testeprático, masconfiávele objetivo,antesdeserem usados.Nossosresultadossugeremqueosmartphonefoiprecisoo suficienteparaserusadocomoumluxímetroparatestaraluzdolaringoscópio.Osresultados daauditoriamostrandoapenas4%deconformidadecomasnormasdaISOcorroboramosde outrosestudos.
Conclusão:O smartphonetestado tem precisão suficiente para fazer a medic¸ão deluz em laringoscópios. Acreditamos que esse é um passo adiante na execuc¸ão de uma verificac¸ão objetivaderotinadaluzdolaringoscópio.
©2016PublicadoporElsevierEditoraLtda.emnomedeSociedadeBrasileiradeAnestesiologia. Este ´eum artigo Open Access sob umalicenc¸aCC BY-NC-ND(http://creativecommons.org/ licenses/by-nc-nd/4.0/).
Background
and
objectives
Laryngoscope is a key tool in anesthetic practice. Direct
laryngoscopyisacrucialmomentintheinductionphaseof
anesthesiaandinadequatelaryngoscope’slightcanleadto
catastrophic consequences.From our experience
laryngo-scope’slight isassessedworldwideinasubjectivemanner
andwebelieveamorepreciseevaluationshouldbeused.
Thereareafewstudiesaddressinglaryngoscope’slightand
the results show insufficient light in most of the tested
laryngoscopes.1,2
InasmallinformalsurveyinourAnesthesiologyand
Oper-atingRoomdepartmentswefoundlaryngoscope’slightasa
frequent complain.Ourobjectiveis tocompare the
accu-racyofasmartphonecomparedtoaluxmeterandsecondly
weauditedourOperatingRoomlaryngoscopes.Our
hypoth-esisstatesthatasmartphonehasaccuracysimilartoalux
meter.Further,wealsoauditedalllaryngoscopesreadyto
useinallOperatingRooms.
Methods
We designed a pragmaticstudy totest the accuracy of a
smartphonemeasuring illuminanceusinga lux meteras a
reference.Secondlyweauditedourready-to-useOperating
Roomlaryngoscopes.
Primary outcome was the accuracy of the smartphone
compared to the lux meter. The null hypothesis was no
difference between measurements from the smartphone
comparedtotheluxmeter.
Beforeperformingthestudy,institutional authorization
wasgranted.Twodifferentprotocolsweremade,onetotest
theaccuracyofthesmartphonecomparedtotheluxmeter,
andothertoauditthelaryngoscopes.
Totest theaccuracy ofthesmartphonemeasuring
illu-minancewe usedaslight sourceawhitefluorescentlamp
(OSRAM Licht AG®) with a dimmer to produce different
lightintensities.Thesmartphoneusedtotestforaccuracy
wasaMotorola® MotoGXT1068 andthecontrolwasalux
meter(HDE®LX-1010B).Motorolawascontactedandsaidwe
shouldexpect80%accuracyinarangefrom5to10,000lux,
whiletheluxmeter advertises95%accuracy inarangeof
0---50,000.
Sincethecut-offoftheISOstandardis500lux3we
arbi-trarilysetatotalof20lightintensitiesfrom50to1000lux inincreasesof50lux.Toseteachlightintensitywedimmed
thelampinadarkroomandmeasuredtheilluminancewith
theluxmeter untilwegot theexpectedvalue.This
mea-surementwasperformed in aroomwithnoexternal light
182 D.A.Machadoetal.
20mmawayfromit.Aftersettingthedesirablelight inten-sityusingthediming andcontrollingitwiththeluxmeter,
the smartphone’s light sensor (position previously known
fromtechnicalspecifications)wasplacedinthesameplace
astheluxmetersensorandilluminancevaluewasmeasured
usingaspecific application.Once opened thesmartphone
application, it continually readsthe raw values retrieved
fromthelight sensorof thesmartphoneand outputthem
inthesmartphonedisplay.Toreducepotentialbiasofusing
andunknowncoded apptomeasurelightfromthe
smart-phonesensorweprogramedtheAndroidTMapplicationand
publisheditssourcecodeonline.4
Werepeatedthesmartphonemeasurementthreetimes
for each light intensity tested (using the lux meter as a
control)andthencalculatedthemeanvalue.
Resultscomparingthesmartphoneaccuracyinthe
spec-ified light intensities wereperformed withpaired sample
t-testusingap-valueof0.05,withIBM®SPSS®Statistics22.
To audit our laryngoscopes we used as reference the
internationalstandardformtheInternationalOrganization
for Standardization (ISO 7376:2009) which specifies
mini-mumilluminanceof 500lux after 10min for hook-ontype
laryngoscopesmeasured20mmfromlaryngoscope’stip.3
Toperformourauditweconstructedadevicecapableto
holdthelaryngoscopestandstillinsuchamannerthatthetip
oflaryngoscope’slightwas20mmfromtheluxmetersensor
asrequiredbytheISOstandard.Ourdevicewasalsoableto
protecttheluxmetersensorfromexternallightevenwith
themeasurementsperformed in a darkroom. To perform
theauditwemeasuredilluminanceusingthesameluxmeter
(HDE®LX-1010B).
Allthemeasurementswereperformed inthesameday
and our sample was all ready-to-use laryngoscopes from
14 Operating Rooms. All the tested laryngoscopes were
reusable,battery-operatedandxenonbulb-in-handle,from
WelchAllyn®orHeine®brands.Bladeswerehook-on
MacIn-toshtypesizes3---5.Weperformedatotalof48tests,testing
eachready-to-usecombinationofhandleandbladeineach
OperatingRoom,inatotalof48testsperformed.
Measurementsweremadeplacingthelaryngoscope
(han-dleandblade)inthedevicebuiltandrecordedtheluxmeter
valueontenthminuteafterturnedon.Datafromtheaudit
wasanalyzedusingIBM® SPSS® Statistics22.
Results
Fortheprimaryoutcome, we calculatedthe mean ofthe
3measurementsmadewiththesmartphoneandcompared
withthevaluefromtheluxmeter.Wefoundnosignificant
difference between devices; t(19)=−1.489, p>0.05. The
meandifferencebetweenmeasurementswas−0.35luxwith
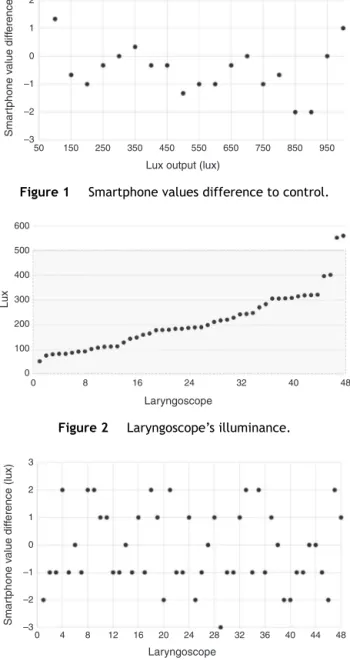
astandarddeviationof1.05118lux.Resultsarerepresented inFig.1.
Intheauditionmadeonly2in48laryngoscopesshowed
aminimumilluminanceof500lux(Fig.2).Meanilluminance
was 212.48lux with a standard deviation of 114.810lux.
Interquartile ranges were Q1=112.25, Q2=189.00 and
Q3=300.50lux.
When comparing the measurements between the lux
meterandthesmartphone(Fig.3)we foundnosignificant
3 2 1 0 –1 –2 Smar tphone v alue diff erence (lux) –3
50 150 250 350 450 550
Lux output (lux)
650 750 850 950
Figure1 Smartphonevaluesdifferencetocontrol.
600 500 400 300 200 100 Lux 0
0 8 16 24 32 40
Laryngoscope
48
Figure2 Laryngoscope’silluminance.
3 2 1 0 –1 –2 Smar tphone v alue diff erence (lux) –3
0 4 8 12 16 20 24 28 32 36 40 44
Laryngoscope
48
Figure3 Smartphonevalue’sdifferencetolaryngoscopes.
difference;t(47)=−0.831,p>0.05withameandifference
of−0.167luxandastandarddeviationof1.389lux.
Discussion
Laryngoscopy is one of the most frequent and important
techniques performed by the anesthesiologist in his daily
practiceandideallyeverylaryngoscope shouldperformas
required.Webelieveeverylaryngoscopeshouldhavea
prac-ticalbutreliableandobjectivetestpriortoitsutilization. Ourresultssuggestthatsmartphonescanbereliablytotest
laryngoscopes’illuminance.
Inourtests,wefoundameandifferencebetweenthelux
meterandthesmartphonelessthan1lux.Asthemaingoal
istoknowifthelighthasaminimumoutputof500lux,we
believe oursmartphonewascapable of performthattask
Accuracyofasmartphonetotestlaryngoscope’slight 183
Our auditresults showingonly 4% comply withtheISO
standard are consistent with other studies.1,2 We believe
regularauditsshouldbemadeandattitudestofixthat
situ-ation.Inourstudywedidnotaddresswhatwastheproblem
ineachlaryngoscope.
AlthoughMotorola®saidweshouldexpectanaccuracyof
80%intherangefrom5to10,000webelievethisisa
con-servativevaalueandwefoundoursmartphonemuchmore
accurate.
We identified some limitations. Not all smartphones
have a light sensor and even those with it, their
accu-racy can be variable and its position can be difficult to
find.Eachsmartphoneshouldbetestedforaccuracybefore
beingused.Therearedifferentapps tomeasurelight
val-ues, and to reduce this bias we designed and published
its source code. The used lux meter was the best
pos-sible however we are aware that there are much more
precise lux meters, although we believe our lux meter
was precise enough. Measurements from 50 to 1000lux
in intervals of 50lux were arbitrarily set. As our audit
waspragmatictoall readyto uselaryngoscopes, insome
casesthesamelaryngoscopewastestedwithtwodifferent
blades.
Conclusions
Wepropose thatasmartphonecanbeaccurateenoughto
classifylaryngoscope’slightasadequatetoperform
laryn-goscopy.Ourconclusionis thatthetestedsmartphonehas
enoughaccuracytoperformlightmeasurementin
laryngo-scopeslight. Sinceeach smartphonecan have a different
lightsensorthisconclusioncannotbegeneralized.
In the future more studies are needed to test other
deviceslike smartphones and to understand if perform a
laryngoscopelighttestbeforeeachusecanhaveapositive
influenceinthelaryngoscopyandoutcomeof thepatient.
Thereisalsoaneedofstudiestounderstandthesourceof
theproblemtolaryngoscopesdo notcomply withthe ISO
norm.
Webelievethiscouldbeastepfurtherinperformingan
objectiveroutinechecktolaryngoscope’slight.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
Thisresearchreceivedanyfundorgrantspecificgrantfrom
anyfundingagency inthepublic, commercial,or
not-for-profitsectors.
References
1.BakerPA,McQuoidS,ThompsonJM,etal.Anauditof laryngo-scopesandapplicationofanewISOstandard.PaediatrAnaesth. 2011;21:428---34.
2.VolskyPG,MurphyMK,DarrowDH.Laryngoscopeilluminanceina tertiarychildren’shospital:implicationsforqualitylaryngoscopy. JAMAOtolaryngolHeadNeckSurg.2014;140:603---7.
3.InternationalOrganisationforStandardisationISO7376:2009(E). Anaestheticandrespiratoryequipment---laryngoscopesfor tra-chealintubation.2nded;2009.p.1---34.