www.jped.com.br
ORIGINAL
ARTICLE
Cholelithiasis
in
obese
adolescents
treated
at
an
outpatient
clinic
夽
,
夽夽
Marília
M.
de
A.
Nunes
a,b,∗,
Carla
C.M.
Medeiros
c,d,
Luciana
R.
Silva
a,eaMedicineandHealth,UniversidadeFederaldaBahia(UFBA),Salvador,BA,Brazil bUniversidadeFederaldeCampinaGrande(UFCG),CampinaGrande,PB,Brazil
cChildandAdolescentHealth,UniversidadeEstadualdeCampinas(UNICAMP),Campinas,SP,Brazil dUniversidadeEstadualdaParaíba,CampinaGrande,PB,Brazil
ePediatricGastroenterologyandHepatologyStudyCenter,UniversidadeFederaldaBahia(UFBA),Salvador,BA,Brazil
Received30April2013;accepted21August2013 Availableonline20December2013
KEYWORDS Obesity; Cholelithiasis; Hepaticsteatosis; Children;
Adolescent
Abstract
Objective: todescribethefrequencyandthefactorsassociated withcholelithiasisinobese adolescents.
Methods: thiswasacross-sectionaldescriptivestudyperformedwiththeadolescentsbetween
10and19yearsofagetreatedattheChildandAdolescentObesityOutpatientClinicfromMay
toDecemberof2011.Obesitywasdefinedasbodymassindex(BMI)>P97,andoverweightas
BMI>P85,forageandgender,accordingtothe2007WorldHealthOrganizationreference.A
questionnaireconcerningthepresenceofsignsandsymptoms,suchasabdominalpain,nausea,
vomiting,andintolerancetofat,wasadministered.Patientswereaskedabouthowmany
kilo-gramstheyhadlostandinhowmuchtime.Laboratoryparameterswere:triglycerides,total
cholesterol,highdensitylipoprotein(HDL),lowdensitylipoprotein(LDL),aspartate
aminotrans-ferase (AST),andalanine aminotransferase(ALT) levels.Cholelithiasisandhepaticsteatosis
werediagnosedbyultrasonography.
Results: cholelithiasiswasdiagnosedin6.1%(4/66)oftheobeseadolescents,mostofwhom
were female(3/4);hepaticsteatosiswasidentifiedin21.2% (14/66).Intolerancetodietary
fat wasreportedby allpatientswithcholelithiasis (4/4)andby17.7% (11/62)ofthegroup
withoutcholelithiasis(p=0.001).Theaverageweightlosswas6.0±2.9kginthepatientswith
夽 Pleasecitethisarticleas:NunesMM,MedeirosCC,SilvaLR.Cholelithiasisinobeseadolescentstreatedatanoutpatientclinic.JPediatr
(RioJ).2014;90:203---8.
夽夽StudyconductedattheUniversidadeFederaldaBahia(UFBA).
∗Correspondingauthor.
E-mail:alberto.marilia@uol.com.br(M.M.d.A.Nunes).
cholelithiasisand3.2±4.8kginthegroupwithoutcholelithiasis(p=0.04).However,therewas
nodifferencebetweenthetwogroupsregardingthetimeofweightloss(p=0.11).
Conclusions: cholelithiasis andhepaticsteatosisarefrequent among obeseadolescentsand
shouldbeinvestigatedsystematicallyinthepresenceorabsenceofsymptoms.
©2013SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Allrightsreserved.
PALAVRAS-CHAVE Obesidade;
Litíasebiliar; Esteatosehepática; Crianc¸a;
Adolescente
Litíasebiliaremadolescentesobesosatendidosemambulatório
Resumo
Objetivo: descreverafrequênciaeosfatoresassociadosàlitíasebiliaremadolescentesobesos.
Métodos: estudodescritivotipocortetransversalcomadolescentesentre10e19anos
aten-didosemambulatóriodeobesidadeinfanto-juvenil,noperíododemaioadezembrode2011.
Aobesidadefoidefinidacomoíndicedemassacorporal>P97eosobrepeso>P85,paraidadee
sexo,segundooreferencialOMS2007.Foiaplicadoumquestionáriocomdadosrelacionados
àpresenc¸adesinaisesintomas,como:dorabdominal,náusea,vômitoeintolerânciaà
gor-dura.Ospacientesforamquestionadossobrequantosquilosperderameemquantotempo.As
variáveislaboratoriaisforam: triglicerídeos,colesteroltotal, lipoproteínadealta densidade
(HDL) elipoproteína de baixa densidade (LDL),aspartato aminotransferase(AST) e alanina
aminotransferase(ALT).Alitíasebiliareaesteatosehepáticaforamdiagnosticadaspor
ultra-ssonografia.
Resultados: alitíasebiliarfoidiagnosticadaem6,1%(4/66)dosadolescentesobesos,amaioria
dosexofeminino(3/4);aesteatosehepáticafoiidentificadaem21,2%(14/66).Intolerânciaà
gorduradadietafoireferidaportodososportadoresdelitíasebiliar(4/4)epor17,7%(11/62)
dogruposemlitíasebiliar(0,001).Amédiadeperdadepesofoide6,0±2,9kgnospacientes
comlitíasebiliare3,2±4,8kgnogruposemlitíase biliar(p=0,04). Porém,em relac¸ão ao
tempodeperdanãohouvediferenc¸aentreosdoisgrupos(p=0,11).
Conclusões: alitíasebiliareaesteatosehepáticasãofrequentesentreadolescentesobesose
devemserinvestigadassistematicamentenapresenc¸aouausênciadesintomas.
©2013SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Todososdireitos
reservados.
Introduction
Theprevalenceofobesityinchildrenandadolescents con-tinuestoriseinmanycountries.IntheUnitedStates,obesity hasmorethandoubledinchildrenandtripledinadolescents over the last30 years.1,2 In Brazil, a study of 4,914
chil-drenaged4to6 yearsconductedinthepublicschools of RioGrandedoSulandSantaCatarinafoundaprevalenceof obesityof14.4%and7.5%,respectively.3InBahia,astudy
thatincluded1,056childrenaged0to5yearsfounda15.2% prevalenceofoverweight/obesity.4
Several studies have described the deleterious effects ofobesity,suchasmetabolicsyndrome,cardiovascular dis-ease,jointdisease,polycysticovarysyndrome,fattyliver, gallstones,aswellassocialandpsychologicalproblems.5---7
Cholelithiasisisarecognizedcomorbidityinobeseadults,8
although little studied in pediatric patients.9,10 Another
epidemiologicalfindingisthehigherfrequencyof cholecys-tectomyinthisagegroupthathasbeenobservedinrecent years.11
Infants, children and adolescents with cholelithiasis appearto comprise threedifferent populations regarding pathogenesisandpredisposingfactors.10 Intheprepubertal
cases,blackpigmentcalculi predominate,whichare asso-ciatedwithhemolysis, parenteralnutrition, cirrhosis,and heartvalvereplacement.12Cholesterolcalculiarethemost
frequentduringandafter adolescence,12 whenchangesin
estrogenmetabolismmayresultinincreasedbile litogenic-ityandformationofthistypeofgallstones.13
Particularattentionmustbegiventoobese,dyslipidemic adolescents,pregnantwomen,andoralcontraceptiveusers, astheseindividualsaremorelikelytodevelop gallstones, inadditiontothehighpercentageofidiopathiccases.10,14
Overweightadolescentsaretwiceaslikelytohavegallstones whencomparedtoadolescentswithnormalbodymassindex (BMI).14 Forthe obese,thechance increasesby four-fold,
andforthosewithsevereobesity,thelikelihoodofhaving thisconditionissix-foldhigher.14
Clinicallysilentcholelithiasisisincreasinglydiagnosedas anincidentalfindingduringimagingexaminations, particu-larlyabdominalultrasound.Inadults,50%to70%ofcasesare asymptomatic,15 andprogressiontosymptomaticdiseaseis
relativelylow,rangingfrom10%to25%.15Conversely,most
children and adolescents present symptoms, from unspe-cificabdominalpainsymptomstobiliarysymptoms,suchas biliarycolicandjaundice.9,10,13
observingpatientswithobesityorotherriskfactorsfor gall-stoneformationthroughrepeatedcontrolultrasoundsforat leasttenyears.
ThiswasthefirstBrazilianstudyoncholelithiasisinobese adolescents.Theaimofthisstudywastodescribethe fre-quencyandfactorsassociatedwithcholelithiasisinagroup ofobeseadolescents.
Methods
This wasa descriptive,cross-sectional studyconductedat theChildandAdolescentObesityOutpatientClinicof Insti-tutodeSaúdeElpídiodeAlmeida(ISEA),CampinaGrande, Paraíba,Brazil.Alladolescentsaged10to19yearstreated between May and December of 2011 who were obese (BMI>97th percentile)oroverweight(BMI>85th percentile)
forageandgender,accordingtothe2007WorldHealth Orga-nization(WHO)referencecharts,wereincluded.17 BMIwas
calculatedbythe Queteletindex(BMI=weight/height[2]). Clinicalandlaboratorycharacteristicsof66patientsofboth genderswereanalyzed.Patientswithanemia,genetic syn-dromes,pregnantpatients,usersofcorticosteroidtherapy or oral contraceptives, or those who habitually used or abusedalcoholwereexcluded.
Clinical variables included: waist circumference, pres-ence of signs and symptoms, such as abdominal pain, nausea, vomiting, and intolerance to fat. Patients were askedabouthowmanykilograms theyhadlostandinhow muchtime.Laboratory variableswere:triglycerides,total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL), aspartate aminotransferase (AST), and alanineaminotransferase(ALT)levels,aswellasthe ultra-sonographicdiagnosisofcholelithiasisandhepaticsteatosis. Anthropometric measurementswereobtained at a sin-gle weight measurement on a calibrated platform scale, inadditiontotheheightmeasurementwithastadiometer. ThetechniquesusedwerestandardizedbytheWHO.18The
adolescentwaspositionedintheorthostaticpositioninthe center of the scale, barefoot with heels placed together, straightback,armshangingatthesides,andwearinglight clothes.
Abdominalcircumference(AC)wasmeasuredusinga non-extensiblemeasuringtapewiththepatientinthestanding position,usingasreferencethemidpointbetweenthelast riband the iliac crest,at the timeof expiration. AC was measuredincentimetersinaccordancewithTayloretal.19
Cholelithiasis was identified on ultrasound, using SA 8000 EX Medison equipment (Samsung Medison), with a multi-frequencyconvextransducer of3-7MHz,by asingle specialisttrainedindiagnosticimaging.
After the informedconsent was signed by the adoles-centandtheparent/guardian,datacollectionwasinitiated throughinterviews and physical examination, followedby laboratory tests andultrasound assessment. Patientswith cholelithiasiswerereferredtothesurgicaloutpatientclinic forevaluationandmanagement.
DataanalysiswasperformedusingtheStatisticalPackage forSocialSciences(SPSS)software21.0.Initially,all varia-bleswereanalyzeddescriptively.Student’st-testwasused tocomparethemeansoftwogroups(presenceorabsence of cholelithiasis). When the assumptionof data normality
was rejected, the nonparametric Mann-Whitney test was used. To test the homogeneity between proportions, the chi-squared test or Fisher’s exact test were used, when theexpectedfrequencieswere<5.Themultivariate logis-ticregressionmodel wasusedtostudytheseveralfactors influencingtheoccurrenceofcholelithiasis.Thesignificance levelusedforthetestswassetat5%.
Theproject wasapprovedbytheResearchEthics Com-mittee on Human Subjects of the Hospital Universitário AlcidesCarneiro(HUAC),underprotocolnumber 20091412-053.
Results
Thepresentstudyincluded66patients,40ofwhom(60.6%) were females, with a mean age of 14.3±2.2 years, who residedinCampinaGrandeandsurroundingcities.
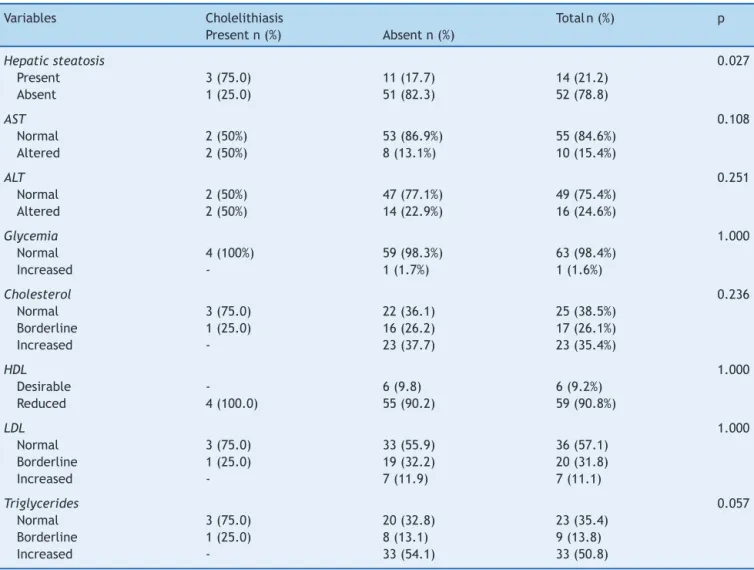
Cholelithiasis was diagnosed in three of the 66 (4.5%) obese adolescents. By including an adolescent who had undergonecholecystectomy,cholelithiasisaffectedfourof the 66 adolescents (6.1%), with a predominance of the female gender (3/4). Hepatic steatosis was identified in 21.2%patients(14/66),ofwhom57.1%(8/14)hadthemild form and 42.9% (6/14) a moderate form of the disease. Hepatic steatosis was observed in 75% (3/4) of patients withcholelithiasis and in 17.7% (11/62) of those without cholelithiasis;thisdifferencewassignificant(p=0.02).
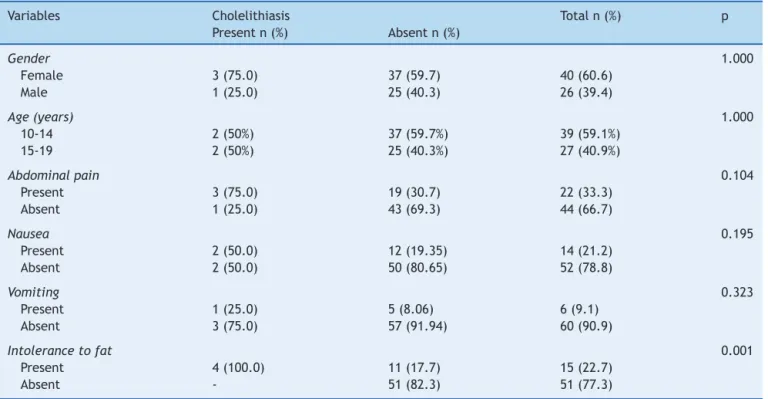
All patients with cholelithiasisreported intolerance to fattyfoods (4/4), whichwasalsomentioned by 11of the 62(17.7%)patientswithoutcholelithiasis,showinga signif-icantdifference(p=0.001).Othersymptomspresented no significant difference between the groups with and with-out cholelithiasis (Table 1). The mean weight loss was 6.0±2.9kgincholelithiasispatientsand3.2±4.8kginthe groupwithoutcholelithiasis(p=0.04).However,inrelation totimeofweightloss,therewasnodifferencebetweenthe twogroups(p=0.11).
Familyhistoryof cholelithiasiswaspositivein threeof four(75%)patientswithcholelithiasisandin22of61(36.1%) patientswithoutit,but thisdifferencewasnotsignificant (p=0.28).Oneadolescenthadbeenadopted.
In the group of patients withcholelithiasis, mean BMI (37.9±9.1kg/m2) was higher than in the group
with-out cholelithiasis (30±4kg/m2), but the difference was
not significant (p=0.18). The mean AC was also greater amongadolescentswith(109.4±24.7cm)when compared topatientswithoutcholelithiasis(91.4±10.2cm),although thedifferencewasnotsignificant(p=0.14).
Onepatientwhohadmoderatehepaticsteatosisalso pre-sented elevated blood glucose,but nocholelithiasis. The resultsof lipid andaminotransferase profileare shown in Table2.
Discussion
Thefrequencyofcholelithiasisinthisstudy(6.1%)washigh. To date, the only study of cholelithiasis in patients with childhoodobesity wasperformedin GermanybyKaechele etal.,20whofoundafrequencyof2%among493hospitalized
Table1 Distributionofmedicalhistoryvariablesaccordingtothepresenceofcholelithiasis.
Variables Cholelithiasis Totaln(%) p
Presentn(%) Absentn(%)
Gender 1.000
Female 3(75.0) 37(59.7) 40(60.6)
Male 1(25.0) 25(40.3) 26(39.4)
Age(years) 1.000
10-14 2(50%) 37(59.7%) 39(59.1%)
15-19 2(50%) 25(40.3%) 27(40.9%)
Abdominalpain 0.104
Present 3(75.0) 19(30.7) 22(33.3)
Absent 1(25.0) 43(69.3) 44(66.7)
Nausea 0.195
Present 2(50.0) 12(19.35) 14(21.2)
Absent 2(50.0) 50(80.65) 52(78.8)
Vomiting 0.323
Present 1(25.0) 5(8.06) 6(9.1)
Absent 3(75.0) 57(91.94) 60(90.9)
Intolerancetofat 0.001
Present 4(100.0) 11(17.7) 15(22.7)
Absent - 51(82.3) 51(77.3)
Later,apopulation-basedstudyconductedinthatsame countrybyKratzer etal.21 found afrequencyof1%in307
adolescentsaged12to18years.Inthatstudy,twoofthe threeadolescentswithgallstoneswereobeseandthus,the authorsconcludedthatobesityappearstobeariskfactor inthedevelopmentofgallstones inchildhoodand adoles-cence.
Thehighfrequencyobservedinthepresentstudyis prob-ablyrelated toenvironmental factors,suchas diet.Diets low in fiber witha high intake of refinedsugars andfats contribute to gallstone formation and are related to the developmentof obesity,which is considered a risk factor forcholelithiasis.19,22,23Moreover,inthepresentsampleall
participantswereoverweightorobese.
IntheUnitedStates,acohortstudyperformedby Koeb-nick et al.14 detected 766 cases of cholelithiasis among
510,816adolescentswhoparticipatedinthestudy,a preva-lenceof0.1%.Theauthorsobservedthattheprevalenceof gallstonesincreasedwithincreasingweight,but the asso-ciationwasstrongerinfemalesthaninmales.Thepresent study confirmed thisfinding, sincethreeof the four ado-lescents with lithiasis were female. Several studies have shown a higher frequency of cholelithiasis in the female gender.8,22
Thefemalegenderisassociatedwithcholelithiasis, espe-ciallyduringthechildbearingyears.Estrogensincreasethe secretionofcholesterolanddecreasethesecretionofbile salts,whereasprogestogensact byreducingthe secretion ofbilesaltsandtheemptyingofthegallbladder,leadingto stasis.24
The frequency of hepatic steatosis (21.2%) was lower thanthatreportedbyLiraetal.,25whoobserveditin27.7%
ofthe172adolescents,andgreaterthanthat reportedby Schwimmeretal.,26whoreporteditin9.6%amongchildren
andadolescents.
These authors reported that the prevalence increases withage,rangingfrom0.7%fromages2to4yearsto17.3% fromages15to19years.7Inthepresentstudy,the
signifi-cantassociationbetweencholelithiasisandhepaticsteatosis is spurious,sinceobesity isimplicated asarisk factorfor both.16,22 Regardingthephysiopathology,cholelithiasisand
hepaticsteatosisbehaveasindependentvariables.19
Thepresenceofsymptomsassociatedwithcholelithiasis inthisstudywasgreaterthanthatreportedintheliterature, asallfourpatientsweresymptomatic;however,only intoler-ancetodietaryfatwassignificant.Ruibaletal.27studied123
children and adolescents withcholelithiasis and observed that66%hadsymptoms;approximately35%hadabdominal painassociatedwithvomitingand27%hadisolated abdom-inalpain.
Wesdorp et al.11 studied the clinical presentation of
82 childrenandadolescentswithcholelithiasis,mostwith hemolyticdisease(32/82)andonlythreewithobesity,and observed that 17% were asymptomatic, 52% had biliary symptoms (biliarycolic and jaundice),24% had unspecific abdominalpain,and7%hadacuteabdominalpainwithfever. Amongpatientswithbiliarysymptoms,10%reported intol-erancetofat.
However,certainvaguecomplaintssuchassymptomsof dyspepsiawithcertainfoods,flatulence,nausea,and bloat-ingthathavebeeninthepastattributedtocholelithiasisare notacceptedtoday,mainlybecauseoflackofimprovement aftercholecystectomy,andarethusattributedtoirritable bowel syndromeor other organicor functionaldiseases.16
Table2 Distributionofcomplementaryexaminationvariablesaccordingtothepresenceofcholelithiasis.
Variables Cholelithiasis Total n(%) p
Presentn(%) Absentn(%)
Hepaticsteatosis 0.027
Present 3(75.0) 11(17.7) 14(21.2)
Absent 1(25.0) 51(82.3) 52(78.8)
AST 0.108
Normal 2(50%) 53(86.9%) 55(84.6%)
Altered 2(50%) 8(13.1%) 10(15.4%)
ALT 0.251
Normal 2(50%) 47(77.1%) 49(75.4%)
Altered 2(50%) 14(22.9%) 16(24.6%)
Glycemia 1.000
Normal 4(100%) 59(98.3%) 63(98.4%)
Increased - 1(1.7%) 1(1.6%)
Cholesterol 0.236
Normal 3(75.0) 22(36.1) 25(38.5%)
Borderline 1(25.0) 16(26.2) 17(26.1%)
Increased - 23(37.7) 23(35.4%)
HDL 1.000
Desirable - 6(9.8) 6(9.2%)
Reduced 4(100.0) 55(90.2) 59(90.8%)
LDL 1.000
Normal 3(75.0) 33(55.9) 36(57.1)
Borderline 1(25.0) 19(32.2) 20(31.8)
Increased - 7(11.9) 7(11.1)
Triglycerides 0.057
Normal 3(75.0) 20(32.8) 23(35.4)
Borderline 1(25.0) 8(13.1) 9(13.8)
Increased - 33(54.1) 33(50.8)
AST,aspartateaminotransferase;ALT,alanineaminotransferase;HDL,high-densitylipoprotein;LDL,low-densitylipoprotein.
etal.20 observedthatobesechildrenandadolescentswith
cholelithiasis lost an average of 10.1±7.0kg compared withonly5.8±5.0kglost inthe groupwithout cholelithi-asis.Amongthetenobesepatientswithcholelithiasis,nine reported undergoing dieting for weight reduction. As for the time of weight loss, the present study found no dif-ferencebetweenthetwogroups.Thebestevidencecomes fromprospectivestudies,showingthatrapidweightloss,as thatobservedinhypocaloricdiets,markedlyincreasesthe formationofgallstones.28
The mainmechanismof gallstoneformationinpatients with weightgain or rapid weight loss is reduction of the gallbladdermotilityandincreasedexcretionofcholesterol inthebile,causingcholesterolsupersaturation,with subse-quentformationofgallstones.16
In thepresent study,the reportingof familyhistoryof the disease by 75% of adolescents with cholelithiasis is consistent with the literature. In the study by Kaechele etal.,20threeoutof10(30%)obesepatientswith
cholelithi-asisreportedpositivefamilyhistory,andthemotherswere affectedinallthreecases.Wesdorpetal.9observedalower
frequency,withapositivefamilyhistoryinsevenoutof82 (8.5%)patientswithcholelithiasis.
A cohort study29 with individuals with symptomatic
cholelithiasisobservedthatmenwithBMI>28.5kg/m2have
a2.48-foldhigherchanceofdevelopingcholelithiasiswhen comparedtothosewithBMI<22.2kg/m2.Furthermore,
indi-vidualswith AC>102.6cm have a 2.66-fold higher risk of developingcholelithiasisthanindividualswithAC<86.4cm. The authors demonstrated that AC predicts the risk of cholelithiasisregardlessoftheBMI.29 Inthepresent study,
obese adolescents with cholelithiasis had higher BMI and ACmeasurementswhencomparedwithadolescentswithout cholelithiasis.
Halfof obeseadolescentswithsymptomatic cholelithi-asis had abnormal levels of aminotransferases, and this findingwasconsistentwiththeliterature.Wesdorpetal.9
Cholelithiasisandhepaticsteatosisarecommoninobese adolescents,andgastrointestinalsymptomsshouldbe con-sidered,astheyareoftenunderestimatedinadolescence, through attribution to a psychosomatic or other type of cause. Therefore, it is recommended to maintain active screeningusingultrasound toidentifythiscondition inall symptomaticorasymptomaticobeseadolescents.
Funding
Coordination of Improvement of Higher Level Personnel (CAPES)
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.OgdenCL,CarrollMD,KitBK,FlegalKM.Prevalenceofobesity andtrendsinbodymassindexamongUSchildrenand adoles-cents,1999-2010.JAMA.2012;307:483---90.
2.National Centerfor Health Statistics(NCHS).Health, United States,2011:withspecialfeaturesonsocioeconomicstatusand health.Hyattsville:NCHS;2012.p.583p.
3.Schuch I,Castro TG, Vasconcelos FA, DutraCL,Goldani MZ. Excesso de peso em crianc¸as de pré-escolas: prevalência e fatoresassociados.JPediatr(RioJ).2013;89:179---88. 4.MatosSM,JesusSR,SaldivaSR,PradoMS,D’InnocenzoS,Assis
AM,etal.Velocidadedeganhodepesonosprimeirosanosde vida e excessode peso entre5-11 anos de idade, Salvador, Bahia.BrasilCadSaudePublica.2011;27:714---22.
5.Morrison JA, Friedman LA, Gray MC. Metabolic syndrome in childhoodpredictsadultcardiovasculardisease25yearslater: thePrincetonlipidresearchclinicsfollow-upstudy.Pediatrics. 2007;120:340---5.
6.RosenfieldRL.Identifyingchildrenatriskforpolycysticovary syndrome.JClinEndocrinolMetab.2007;92:787---96.
7.Schwimmer JB, Deutsch R, Kahen T, Lavine JE, Stanley C, BehlingC.Prevalenceoffattyliverinchildrenandadolescents. Pediatrics.2006;118:1388---93.
8.TorresOJ,BarbosaES,PantojaPB,DinizMC,SilvaJR,Czeczko NG.Prevalênciaultra-sonográficadelitíasebiliarempacientes ambulatoriais.RevColBrasCir.2005;32:47---9.
9.WesdorpI,BosmanD,GraaffA,AronsonD,BlijF,TaminiauJ. Clinical presentationsand predisposingfactors of cholelithi-asis and sludge in children. J Pediatr Gastroenterol Nutr. 2000;31:411---7.
10.BotturaAC,HesselG,TommasoAM.Litíasebiliarnão-hemolítica nainfânciaenaadolescência.RevPaulPediatria.2007;25:90---7. 11.Miltenburg DM, Schaffer R, Breslin T, Brandt ML. Chang-ing indications for pediatric cholecystectomy. Pediatrics. 2000;105:1250---3.
12.StringerMD,TaylorDR,SolowayRD.Gallstonecomposition:are childrendifferent?JPediatr.2003;142:435---40.
13.Schweizer P, Lenz MP, Kirschner HJ. Pathogenesis and symptomatology of cholelithiasis in childhood. Dig Surg. 2000;17:459---67.
14.KoebnickC, Smith N, BlackMH,Porter AH, RichieBA, Hud-sonS, et al. Pediatric obesity and gallstone disease. JPGN. 2012;55:328---33.
15.SakorafasGH,MilingosD,PerosG.Asymptomaticcholelithiasis: ischolecystectomyreallyneeded?Acriticalreappraisal15years aftertheintroductionoflaparoscopiccholecystectomy.DigDis Sci.2007;52:1313---25.
16.DominiciAJ.Litíasebiliar.In:Mattos AA,CorrêaEB,editors. Tratadodehepatologia.RiodeJaneiro:Rubio;2010.p.781-7. 17.deOnisM,OnyangoAW,BorghiE,SiyamA,NishidaC,Siekmann J.DevelopmentofaWHOgrowthreferenceforschool-aged chil-drenandadolescents.BullWorldHealthOrgan.2007;85:660---7. 18.Physicalstatus:theuseandinterpretationof,anthropometry., Report ofa,WHO., Expert, Committee.WorldHealth Organ TechRep,Ser.1995;854:1---452.
19.Taylor RW,Jones IE, Williams SM,Goulding A. Evaluation of waistcircumference,waist-to-hipratio,andtheconicityindex asscreeningtoolsforhightrunkfatmass,asmeasuredby dual-energyX-rayabsorptiometry,inchildrenaged3-19y.AmJClin Nutr.2000;72:490---5.
20.Kaechele V, Wabitsch M, Thiere D, Kessler AL, Haenle MM, MayerH,etal.Prevalenceofgallbladderstonediseaseinobese childrenand adolescents:influenceofthedegreeofobesity, sex,andpubertaldevelopment.JPediatrGastroenterolNutr. 2006;42:66---70.
21.KratzerW, WalcherT, ArnoldF,AkinliAS, MasonRA, Denzer C,et al. Gallstone prevalence and riskfactors for gallstone diseaseinanurbanpopulationofchildrenandadolescents.Z Gastroenterol.2010;48:683---7.
22.CuevasA,MiquelJF,ReyesMS,ZanlungoS,NerviF.Dietasa riskfactorforcholesterolgallstonedisease.JAmCollofNutr. 2004;23:187---96.
23.MehtaS, LopezME, ChumpitaziBP, MazziottiMV,BrandtML, FishmanDS.Clinicalcharacteristicsandriskfactorsfor symp-tomaticpediatricgallbladder.Pediatrics.2012;129:82---8. 24.EtminanM,DelaneyJA,BresslerB,BrophyJM.Oral
contracep-tivesandtheriskofgallbladderdisease:acomparativesafety study.CMAJ.2011;183:899---904.
25.Lira AR, Oliveira FL, Escrivão MA, Colugnati FA, Taddei JA. Esteatose hepática em uma populac¸ão escolar de adoles-centescomsobrepesoeobesidade.JPediatr(RioJ).2010;86: 45---52.
26.SchwimmerJB,McGrealN,DeutschR,FinegoldMJ,LavineJE. Influenceofgender,race,andethnicityonsuspectedfattyliver inobeseadolescents.Pediatrics.2005;15:561---5.
27.RuibalFJ,AleoLE,ÁlvarezMA,Pi˜neroME,GómezCR. Coleliti-asisenlainfância-análisisde24pacientesyrevisiónde123 casospublicadosenEspa˜na.AnEspPediatr.2001;54:120---5. 28.Gebhard RL, Prigge WF, Ansel HJ, Schlasner L, Ketover SR,
SandeD,etal.Theroleofgallbladderemptyingingallstone formationduringdiet-inducedrapidweightloss. Hepatology. 1996;24:544---8.