Risk factors for laryngeal penetration aspiration in patients with acute traumatic cervical spinal cord injury. In addition, the thesis aimed to provide a description of the recovery of penetration-aspiration and functional oral nutrition outcome in these patients.
Traumatic Cervical Spinal Cord Injury
Basic Anatomy of the Spinal Cord
Traumatic SCI
The degree of injury is classified based on the American Spinal Injury Association (ASIA) Impairment Scale (AIS) (Kirshblum et al., 2011; Kirshblum, Waring et al., 2011). In Iceland and Finland, even higher rates for traumatic cervical SCI has been reported (57% and 70%, respectively) (Knutsdottir et al., 2012; Koskinen et al., 2014).
Clinical Consequences and Treatment of Traumatic
In addition, Wong and colleagues (Wong et al., 2012) reported that patients with SCI are particularly vulnerable to malnutrition. Nutritional support and early enteral feeding (start within 72 hours) are generally recommended (Dhall et al., 2013).

Evaluation of Dysphagia
Basic Physiology of Normal Swallowing
After the pharyngeal trigger of the swallow, it usually takes a second or less for the bolus to move through the pharynx to the esophagus. This phase ends when the lower esophageal sphincter opens and the bolus enters the stomach.
Screening and Bedside Evaluation
Aspiration without coughing or choking—silent aspiration—remains, however, difficult to identify with screening procedures. Unfortunately, silent aspiration is frequent as shown in two retrospective studies with large heterogeneous groups of dysphagic patients (Garon, Sierzant, & Ormiston, 2009; Smith, Logemann, Colangelo, Rademaker, & Pauloski, 1999): the incidence of aspiration silent among patients who aspirated ranged from 55% to 59%.
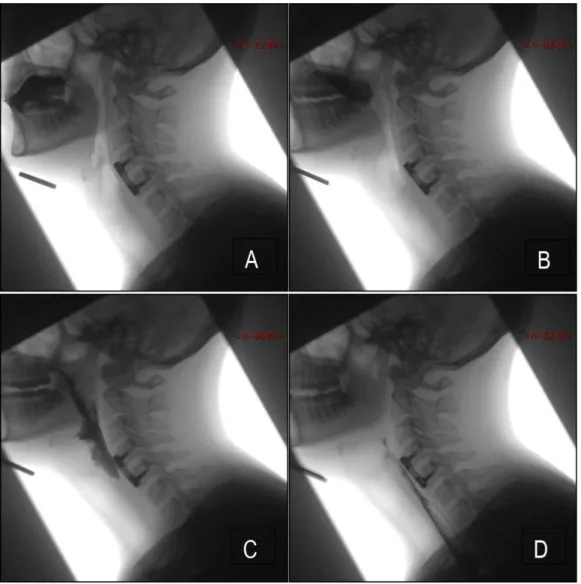
Instrumental Assessment
In addition, 5 ml of nectar-thick and 5 ml of pudding-thick barium are administered in the anterior-posterior view. In comparison, the MBSImp protocol evaluates a total of 17 different physiological components of swallowing, starting with lip closure and ending with esophageal clearance in the upright position (Martin-Harris et al., 2008).
Dysphagia in patients with cervical SCI
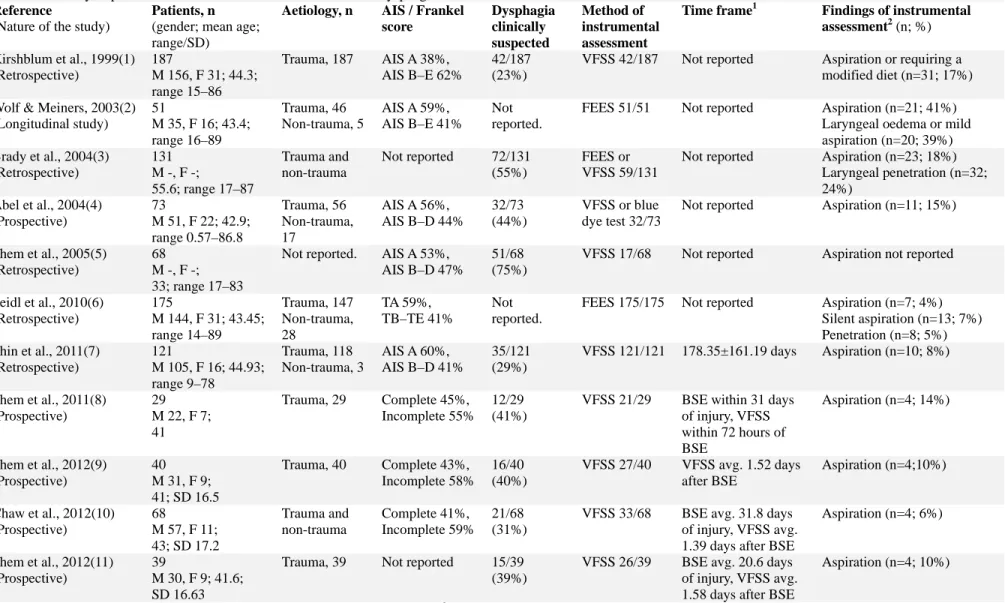
Incidence of Dysphagia
Furthermore, ordinary liquids and food can be used during the examination, although it is easier to visualize colorful liquids (i.e., milk and water with food coloring) (Langmore, 2017).

Risk Factors for Dysphagia
Additionally, Brady and colleagues (2004) reported that cervical SCI patients with dysphagia had a statistically significantly higher co-incidence of traumatic brain injury. Heterogeneity in the diagnostic criteria of dysphagia, study methodologies and large characteristic differences between study populations are some of the main reasons for this situation.
Recovery of Dysphagia
The aim of this thesis is to reveal the incidence and risk factors for laryngeal penetration aspiration in a group of patients with traumatic cervical SCI. In addition, another study aim is to evaluate the recovery of penetrating aspiration and functional oral feeding outcome of these patients.
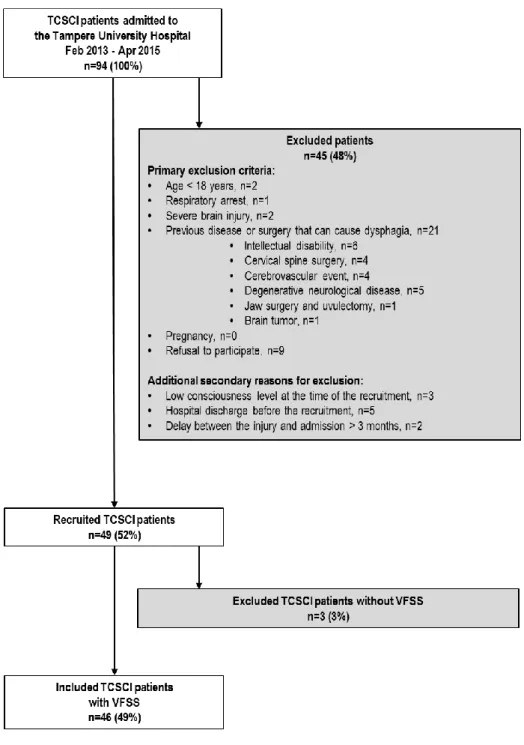
Design and Ethical Aspects
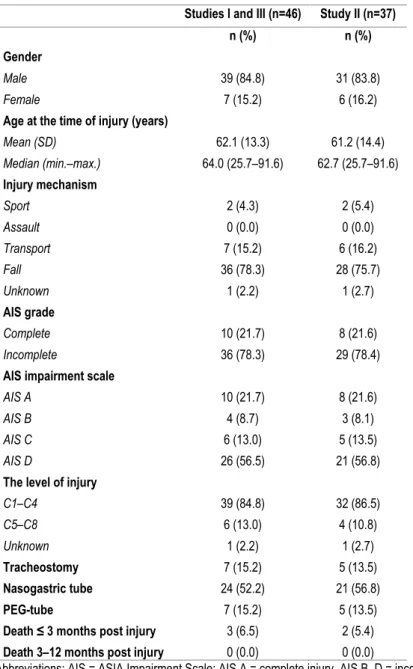
Subjects
Medical and Background Data
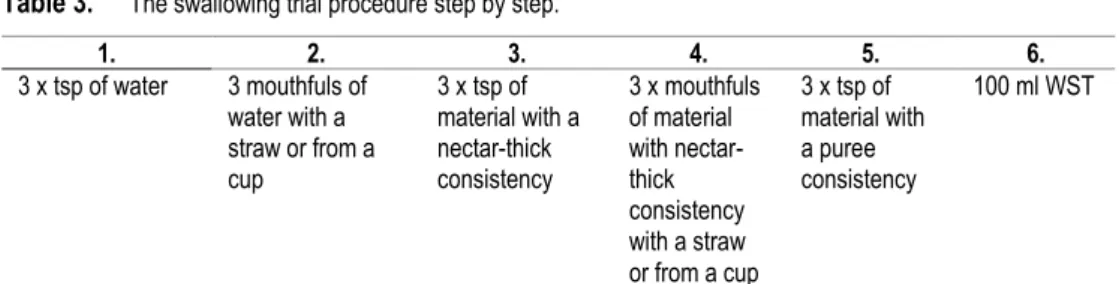
Evaluation Procedures and Measures
Penetration is scored as either 2 or 3 if any remnant remains above the vocal folds and as 4 or 5 if any remnant accesses the level of the vocal folds. Material enters the airway, remains above the vocal folds and is not expelled from the airway (PAS 3).

Speech Therapeutic Interventions
Counseling involved providing information to the patient and his/her relatives about the patient's swallowing ability, the use of compensatory strategies, and the means and goals of swallowing rehabilitation. VitalStim® Therapy is one form of neuromuscular electrical stimulation that can only be delivered by a certified VitalStim® Therapy System provider.
Statistical Analysis
Incidence of Penetration-Aspiration (Study I)
Risk Factors and Clinical Signs for Penetration-Aspiration (Study II)
Risk Factors
Group comparisons between penetrator/aspirators and non-penetrator/aspirators in terms of demographic, injury- and treatment-related, and radiological variables. Surgery on the cervical spine was performed on 28 patients (75.7%) before the VFSS was performed. The penetrator/aspirators had more often anterior surgeries and anterior plate fixations, but the difference was not statistically significant.
The only statistically significant difference between these two groups was that lower level anterior operations were performed more frequently in the penetrator/aspirators compared to the non-penetrator/aspirators (p=0.050, OR=6.1, 95% CI=1.1-33.2 ).

Clinical Signs
Group comparisons between penetrators/aspirators and nonpenetrators/aspirators on swallowing clinical trial variables.
Independent Risk Factors and Clinical Signs
Recovery of Penetration-Aspiration (Study III)
Thus, of the 46 patients who participated in this study, one patient (2.2%) was still suffering from aspiration at the end of the follow-up period (273 days after injury). The VFSS monitoring flow chart and penetration-aspiration results are presented in Figure 8.
Functional Oral Intake Outcome (Study III)
However, by the time of the final follow-up, the majority (88.1%) of patients scored at FOIS level 7, indicating that they were on total oral intake without restrictions. In the penetrator/aspirators group (n=19), fifteen patients (79.0%) patients required partial or full non-oral nutrition via a nasogastric feeding tube at the time of the first bedside evaluation. However, almost every second patient (47.4%) achieved total oral intake without restrictions within a maximum of 63 days after injury and by the time of the final follow-up, 17 patients (89.5%) could enjoy total oral intake without restrictions.
In addition, more than half (52.2%) of non-penetrator aspirators were able to begin (n=1) or continue (n=11) total oral intake without restriction based on initial VFSS . Twenty patients (87.0%) were able to eat by mouth without restriction by the time of the last follow-up. Time frames between the injury and the first bedside evaluation, the first VFSS, and at the time of the last follow-up in non-penetrator/aspirators (PAS ≤2, n=23) and penetrator/aspirators (PAS ≥3, n=19). days after the injury) FIRST BED SIDE.

Incidence of Penetration-Aspiration
The present study found that the incidence rate for aspiration was 33%, supporting the findings of Wolf and Meiners (2003) and indicating that patients with traumatic cervical SCI are susceptible to aspiration. However, there are some important differences between the patients in the present study and those of Wolf and Meiners (2003). Wolf and Meiners (2003) included only cervical SCI patients with respiratory failure and 59% of patients had a complete injury (AIS A) and 77% had an injury level ≥ C4.
In addition, the mean age of patients (62.1 years) in the current study is higher than that reported by Wolf and Meiners (2003) (mean age 43.4 years). Thus, the current study shows that not only severely injured patients with respiratory insufficiency are prone to aspiration. In comparison, the current study and that of Wolf and Meiners (2003) were prospective studies that focused on the acute and subacute phases of treatment of consecutively admitted patients.
Risk factors and Clinical Signs for Penetration-Aspiration
Therefore, in patients with traumatic cervical SCI, the VFSS-verified incidence rate of penetration aspiration may be higher than assumed if based only on the results of the bedside examination. The present study showed that C5 to Th1 level anterior surgery increased the risk of penetration aspiration. This discrepancy may be related to the differences in the prevalence of penetration-aspiration.
Nevertheless, it is reasonable to assume that bronchoscopy is necessary for the therapeutic management of aspiration and excess bronchial secretion due to penetration aspiration. However, it is necessary to ask whether the bronchoscopy is a cause or a consequence of penetration aspiration. In addition, the present study found no relationship between the completeness or level of traumatic cervical SCI and penetrative aspiration.
Recovery of Penetration-Aspiration and Functional Feeding
Moreover, the number of cervical injuries is currently increasing and the average age of trauma patients with cervical SCI is increasing (Devivo, 2012; Knutsdottir et al., 2012; Koskinen et al., 2014). For these reasons, it would be premature to claim that there is no relationship between age and penetration-aspiration based on our findings. Differences between FOIS scores at first clinical assessment and final follow-up were statistically significant for the entire study sample and between penetrators/aspirators and non-penetrators/aspirators subgroups.
In addition, the current study showed that the penetrator/aspirators received statistically significantly more speech therapy interventions than the non-penetrator/aspirators. In addition, the time frame for final follow-up differed statistically significantly between subgroups, indicating that penetrator/aspirators required a longer period of speech therapy interventions. In this study, all treatment decisions were made based on the clinical needs of the patients, not just their penetration aspiration status.
Strengths and Limitations
A frame rate of 30 frames per second is recommended in the literature in order not to miss any significant pathology (Belafsky & Kuhn, 2014; Martin-Harris & Jones, 2008). Thin fluid was chosen because it is the most sensitive consistency for detecting penetration-aspiration: thicker consistencies are used clinically as compensatory strategies for thin fluid aspiration (Clave et al., 2006; Leonard, White, McKenzie, . & Belafsky, 2014). ; Logemann et al., 2008). Of course, the systematic use of a wider range of volumes and different consistencies, as used for example in the MBSImp protocol (Martin-Harris et al., 2008) across the entire study sample, would allow for a more comprehensive assessment of swallowing function. .
In comparison, some studies used mean PAS scores as the outcome measure (Langmore et al., 2016; Pearson, Davidoff, Smith, Adams, & Langmore, 2016). It is well established that aspiration confirmed by VFSS is associated with an increased risk of pneumonia in acute and subacute settings (Holas, DePippo, & Reding, 1994; Kidd, Lawson, Nesbitt, & MacMahon, 1995; . Pikus et al., 2003). . In addition, a few studies have reported that the incidence of pneumonia is significantly higher in cervical SCI patients with dysphagia than in those without dysphagia (Abel et al., 2004; Chaw et al., 2012; Shem et al., 2011; Shem et al., 2011). al., 2012b).
Future Perspectives
Reference for the 2011 revision of the international standards for the neurological classification of spinal cord injury. OBJECTIVE: The aim of this study was to investigate the risk factors for penetration-aspiration in patients with acute traumatic cervical spinal cord injury (TCSCI). The set of swallow test variables was adapted from Logemann et al.[10]Mean time from injury to clinical swallow test was 6.9 days (SD=5.7, mean=4.0, min=1, max=23).
Differences between FOIS scores at first clinical assessment and 258. final follow-up were statistically significant for the entire study sample and between subgroups 259. aspirators/penetrators vs. non-aspirators/penetrators).