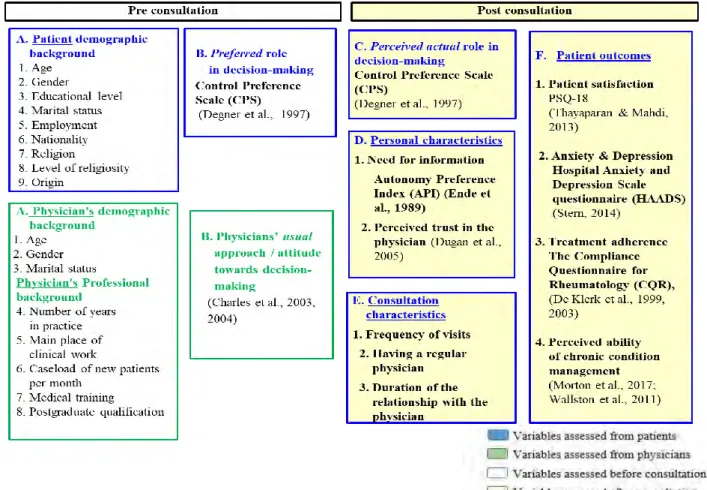
SDM implementation in the conceptual framework of Israeli healthcare culture as constructed according to the current study.3 Figure 2.
Introduction
General Theoretical Perspective
In the present study, these models served as a theoretical framework, highlighting important steps toward improved quality of chronic health care that can be achieved by improving patient-physician communication and involving patients in treatment decisions. In the paternalistic model, the physician makes the final treatment decision without considering the patient's needs and values.
Conceptual framework
In the IDM model, the patient has absolute control over the treatment DMP, after receiving all information. All concerned parties, i.e. national (health policy makers), medical professionals and the patients themselves, must participate in the success of the SDM implementation (Barry & Edgman-Levitan, 2012).
Research approach and methodology
Research design
What are the factors that hinder or promote the ability of cancer patients to participate in DM during clinical consultations in Israel. What facilitators and barriers do physicians see as important for the use of SDM in the practice of cancer patients in Israel?).

The Quantitative Phase
After obtaining the necessary approvals, invitations to participate, accompanied by a letter describing the study procedure, were distributed by email after a telephone call from the researcher of the current study, with the aim of recruiting the participants and obtaining approval for their participation to obtain. . Once the invited participant chose to participate, the researcher of the current study then contacted each of the participants directly (via telephone) to obtain the potential participant's consent.
Qualitative phase
Research approval and ethical considerations
The Request for Review Form for ethical approval of this study was submitted to the Faculty of Socio-Political Sciences' ethics committee, the ethics committee of the Department of Sociology and Social Work and the Maccabi HMO Helsinki ethics committees for non-intervention studies. An informed consent form was created for all participants in this study (patients and physicians). The form confirmed that the participants had secured and protected certain rights, and agreed to participate in the current study.
Participant anonymity was preserved by numerically coding each returned questionnaire and keeping responses confidential. In addition, anonymity was ensured and participants were guaranteed confidential treatment of the collected data.
Results
- Phase 1: Quantitative findings (obtained from research questions 1 - 3)
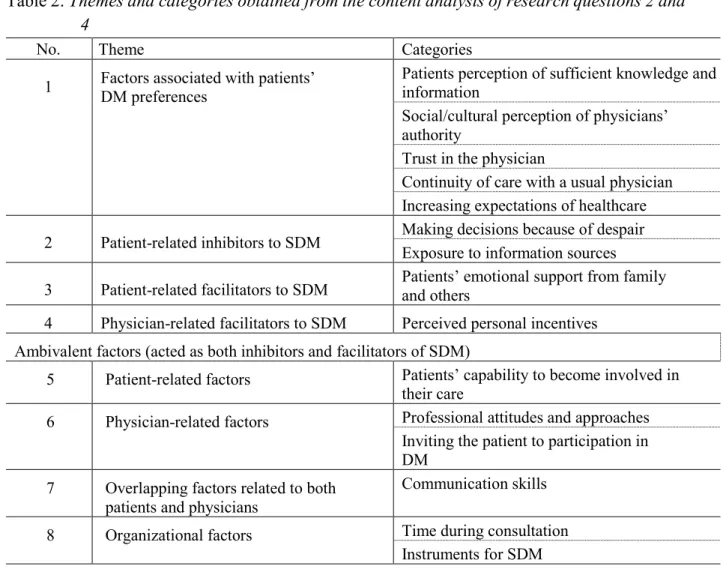
- Phase 2: Qualitative findings (research questions 2 and 4)
70% of patients perceived themselves to be passively involved in DMP (paternalistic/passive approach) after consulting their doctor, compared to 26% who perceived their role as shared/collaborative. Furthermore, cancer patients' preference for involvement in DMP (pre-consultation) and their perceived decision-making role (post-consultation) were inconsistent p<0.001), with a greater preference for shared participation than experienced. What factors are associated with patients' and physicians' SDM behaviors and DM preferences during routine primary care of patients diagnosed with cancer.
Difference in desired level of patient participation in diabetes was examined by patient sociodemographic factors, personal characteristics, and consultation characteristics. Non-significant differences (p > 05) in the preferred role of DM were found between men and women and according to patients' marital status and between different levels of patients' religiosity. Regarding patients' personal characteristics, differences in patients' preferences were characterized by their need for information (F p < 0.003) and their perceived trust in the doctor (F p < 0.003), with the highest need for information and the lowest perceived trust in physician reported by patients who prefer shared/collaborative involvement in DM compared to those who prefer a paternalistic/passive decision-making role.
Regarding the characteristics of the consultation, the differences in patients' preferences were significant in relation to having a regular doctor (consultations with the same doctor) (Cramer's v =.349, p <.000) and the frequency of visits (Cramer's v = .376, p < .000) . These results confirmed hypothesis (2.1) regarding patients' demographic data: age, education level, occupation and origin, but were rejected regarding gender, marital status and religiosity level. Patients who perceived their perceived participation in DM post-consultation as shared/collaborative reported higher levels of satisfaction, treatment adherence and perceived ability to manage their cancer and lower levels of anxiety and depression compared to patients who perceived their experience in DM as paternalistic. /passive.
Interpretation and discussion of findings - main points
- Patients’ preferences for involvement in decision-making process (DMP)
- The status of SDM and the factors affecting its implementation in the Israeli chronic
- The effect of SDM on chronic patients’ health outcomes
The present study also assessed the factors influencing patients' participatory roles in the DMP preferences. This category deals with patients' perceptions and beliefs regarding the quality of care provided to them in the social/cultural context. It seemed that cultural diversity in Israel may influence patients' preferences for involvement in DM.
This study highlighted that patients' preference for involvement in DMP stemmed from the socio-cultural paradigm. The fourth category derived from the content analysis referred to the nature of the relationship between the patient and the doctor and its impact on patients' preferences for involvement in the DMP. This category dealt with patients' expectations of the quality of care provided to them and the health system as a factor influencing their preference for involvement in the DMP.
A screening of patients' preferences could be useful and could facilitate communication between the clinician and the patient. This category referred to oncologists' perception of patients' exposure to multiple medical information sources and databases as a barrier to SDM. This category dealt with both patients' and oncologists' perceptions of patients. opportunity to participate in DMP, which acted as both an inhibitor and a facilitator of SDM.
This category referred to oncologists' acknowledgment of the possibility of patients being part of SDM, as observed by patients in the current study. The findings of the present study regarding the effect of SDM patients' knowledge of their care and health literacy warranted further investigation.
Conclusions and recommendations
- Factual conclusions
- Conceptual Conclusions
Consistent with the literature and the findings of the present study, SDM could serve as a measure of patients' behavioral change in the improved ability to manage their chronic condition, develop better self-care skills, and increase their autonomy in self-management. The results of the current study have shown that this can be achieved through the process of SDM, as it can generate patients' knowledge about their disease and treatment options and increase their self-efficacy in their ability to independently manage their disease. One of the most beneficial effects of SDM was its impact on patients' improved knowledge and increased self-efficacy as a measure of other health behavior changes, such as improved adherence to treatment and management of chronic conditions, developing better self-care skills and increasing the effectiveness of SDM. their autonomy in self-management, and thus better control over their disease.
Furthermore, the current research provided additional knowledge and understanding about the predictors of patients' preferences for involvement in the DMP and, consequently, to the identification of potential approaches to promote patient involvement in decision making (DM). The findings of the present study illustrated that patients' socio-demographic background and personal characteristics, such as the need for information and trust in the physician, played a significant role in their preferences for involvement in the DMP, as it influenced patients' perceived directly affected the person. appropriateness and self-efficacy for participation. The present study also highlighted that patients' preference for involvement in DMP stems from the socio-cultural paradigm.
The current study also confirmed that cancer patients' involvement in their care was essential not only for the well-being of the patients, but also for better health outcomes, for the physicians and the healthcare system. One of the most beneficial effects of SDM was its impact on patients' improved knowledge and increased self-efficacy as a measure of other health behavior changes, such as improved adherence to treatment and management of chronic conditions. Four main concepts and factors were central to the conceptual framework for improving SDM implementation, as observed by both patients and physicians in the current study: (1) patient-physician relationship; (2) patient/physician perceptions, attitudes, and behaviors toward SDM; (3) patients' preferences for involvement (motivation); and (4) (organizational) factors in the healthcare system.
The contribution of the present study
Strengths and limitations of the present study
The current study was conducted in one of four Health Maintenance Organizations (HMOs) in Israel. Thus, the option of generalizing the results to all Israeli primary health care can be questioned. Thus, a multi-health center study is needed to confirm the results of this study and to assess other contributing factors associated with patient participation in shared decision making (SDM).
The second limitation was that there was no assessment of patients' health-related factors, which, according to the medical literature, may influence patients' preferences for the level of involvement in DMP. The present study treated only one type of cancer, without treating other types of cancer, nor the stage of colorectal cancer (CRC) disease, as factors influencing patient preferences, which may limit the generalizability of the results of this study to others. . types of groups of patients with cancer and at different stages of CRC disease.
Recommendations for future research
Iranian cancer patients' perceptions of barriers to participation in decision making: Potential impact on patient-centered care. Shared decision-making in the medical meeting:. or it takes at least two to tango). An overview of patient involvement in health care decision-making: A situational analysis of the Malaysian context.
Barriers and facilitators to shared decision making in child and adolescent mental health: Clinician perspectives using the Theoretical Domains Framework. A patient perspective on shared decision making in stage I non-small cell lung cancer: A mixed methods study. A 5-item version of the Compliance Questionnaire for Rheumatology (CQR5) successfully identifies low adherence to DMARDs.
A systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Barriers to and facilitators of evidence-based decision making at the point of care: Implications for delivery systems, payers, and policy makers. Physician-Identified Barriers to and Facilitators of Shared Decision Making in the Emergency Department: An Exploratory Analysis.