UNIVERSIDADE FEDERAL DO RIO GRANDE DO NORTE CENTRO DE CIÊNCIAS DA SAÚDE
PROGRAMA DE PÓS-GRADUAÇÃO EM CIÊNCIAS DA SAÚDE
RESILIÊNCIA E ADESÃO AO TRATAMENTO EM PACIENTES COM LÚPUS ERITEMATOSO SISTÊMICO
Daniella Antunes Pousa Faria Coelho
UNIVERSIDADE FEDERAL DO RIO GRANDE DO NORTE CENTRO DE CIÊNCIAS DA SAÚDE
PROGRAMA DE PÓS-GRADUAÇÃO EM CIÊNCIAS DA SAÚDE
RESILIÊNCIA E ADESÃO AO TRATAMENTO EM PACIENTES COM LÚPUS ERITEMATOSO SISTÊMICO
Tese apresentada ao Programa de Pós-Graduação em Ciências da Saúde da Universidade Federal do Rio Grande do Norte, como requisito para obtenção de Título de Doutor em Ciências da Saúde.
Aluno: Daniella Antunes Pousa Faria Coelho Orientadora: Profª. Drª. Eulália Maria Chaves Maia Co-orientadora: Profª. Drª. Maria José Pereira Vilar
Natal 2014
UNIVERSIDADE FEDERAL DO RIO GRANDE DO NORTE CENTRO DE CIÊNCIAS DA SAÚDE
PROGRAMA DE PÓS-GRADUAÇÃO EM CIÊNCIAS DA SAÚDE
RESILIÊNCIA E ADESÃO AO TRATAMENTO EM PACIENTES COM LÚPUS ERITEMATOSO SISTÊMICO
Coordenador do Curso de Pós-Graduação: Prof. Dr. Eryvaldo Socrates Tabosa do Egito
Natal 2014
UNIVERSIDADE FEDERAL DO RIO GRANDE DO NORTE CENTRO DE CIÊNCIAS DA SAÚDE
PROGRAMA DE PÓS-GRADUAÇÃO EM CIÊNCIAS DA SAÚDE
RESILIÊNCIA E ADESÃO AO TRATAMENTO EM PACIENTES COM LÚPUS ERITEMATOSO SISTÊMICO
Banca Examinadora:
Presidente da Banca
Profª. Drª. Eulália Maria de Chaves Maia (CCHLA-UFRN/CCS)
Membros da Banca
Profª. Drª. Simone Tomaz da Nobrega Moreira (UFRN) Profª. Drª. Luciana Carla Barbosa de Oliveira (UFRN) Prof. Drª. Maria de Fátima Lobato da Cunha (UFPA) Profª. Drª. Divanise Suruagy Correia (FFAL)
Natal 2014
DEDICATÓRIA
A Deus e Nossa Senhora por ter me acompanhado nesse caminho;
Ao meu querido e eterno amor André que sempre caminhou comigo, dando apoio e atenção nesta jornada;
Aos meus pais, pela dedicação e permanente incentivo no caminho percorrido;
A professora Eulália e Maria José por me conduzirem nesse percurso.
AGRADECIMENTOS
A minha orientadora, Professora Eulália Maria Chaves Maia por estar comigo durante toda minha vida acadêmica, acreditando e incentivando os trabalhos realizados e pela qual tenho enorme gratidão e amizade.
A minha co-orientadora, Professora Maria José Pereira Vilar pela dedicação, amizade e orientação para o desenvolvimento deste estudo.
Aos pacientes que participaram da pesquisa, pois sem eles este trabalho não seria possível.
A estatística Janiere Lira que realizou a análise estatística da presente pesquisa. Ao
Programa de Pós-Graduação em ciências da saúde da UFRN, aos meus pais, que mesmo
sem saber me motivaram à continuar esta jornada; aos professores que incentivaram este
trabalho; aos amigos que me apoiaram; e especialmente ao meu grande amor André Coelho
que me ajudou não só na efetuação deste trabalho, mas que sempre esteve comigo me
apoiando e compartilhando todos os momentos felizes e difíceis desta construção.
RESUMO
Objetivo: Avaliar a resiliência e os comportamentos de adesão ao tratamento auto-relatados, em pacientes com LES, investigando quais destes fatores encontram-se associados à resiliência. Método: Estudo de caráter transversal, multidisciplinar, realizado com a ajuda da equipe de médicos reumatologistas do Hospital Universitário Onofre Lopes, a equipe de psicologia da base de pesquisa de estudos de psicologia e a estística. O estudo foi realizado com 40 mulheres com Lúpus Eritematoso Sistêmico (LES). Utilizou-se um questionário de informações sócio-demográficas e a Escala de Resiliência de Wagnild & Young. Resultados: 62,5% realizam o tratamento medicamentoso adequadamente, porém, 55% sente dificuldade em segui-lo. 27,5% dos pacientes apresentaram resiliência baixa, 57,5% moderada e 15% alta. No teste Qui-quadrado a resilência associou-se (p-valor < 0,05) com as variáveis trabalho; compreensão do LES; procurou saber sobre o LES; faz o tratamento corretamente; dificuldade de seguir o tratamento; com o fato de deixar de fazer alguma atividade devido a doença. Na análise de correlação a resiliência associou-se com: idade (-0,3960), carga horária de trabalho (0,5533), tempo de doença após o diagnóstico (-0,8014) e duração de tratamento especializado (-0,8103). Conclusão: Pacientes com resiliência alta tendem a seguir o tratamento corretamente, buscando compreender a doença e se aderir ao tratamento, de forma a evitar riscos e promover fatores de proteção. Neste processo, se faz importante que o Estado possa tomar as medidas necessárias para facilitar o acesso ao tratamento, a assistência médica e a programas de educação. Promover o conhecimento da doença e o acompanhamento psicológico pode contribuir para que estes pacientes potencializem as capacidades individuais de aprender a lidar com a doença, tendo o apoio psicológico da família e dos médicos um papel significativo.
Palavras-chave: Resiliência, Adesão ao Tratamento, Lúpus Eritematoso Sistêmico
LISTA DE ABREVIATURAS E SIGLAS
LES Lúpus Eritematoso Sistêmico
ACR American College of Rheumatology
OMS Organização Mundial da Saúde
SUS Sistema Único de Saúde
UFRN Universidade Federal do Rio Grande do Norte
HIV Vírus da Imunodeficiência Humana
HUOL Hospital Onofre Lopes
SUMÁRIO
1. INTRODUÇÃO ... 09
2. JUSTIFICATIVA ... 13
3. OBJETIVOS ... 15
4. MÉTODO ... 16
5. ARTIGO PRODUZIDO ... 19
6. COMENTÁRIOS, CRÍTICAS E SUGESTÕES ... 46
7. REFERÊNCIAS BIBLIOGRÁFICAS ... 51
8. ANEXOS ... 55
1. INTRODUÇÃO
O Lúpus Eritematoso Sistêmico (LES) é uma doença reumática inflamatória, crônica, multissistêmica, autoimune, de etiologia ainda confusa, embora já se tenham dados de que
fatores genéticos, hormonais e ambientais estejam envolvidos neste quadro1-3. Afeta
praticamente todos os órgãos e sistemas, mas especialmente a pele, articulações, rins e
vasos sanguíneos de forma concomitante ou sucessivamente4-6.
A maioria dos dados epidemiológicos sobre o LES é vinda de países como EUA e
Inglaterra, tendo o Brasil pouca literatura acerca da epidemiologia da doença7. A incidência
da doença em Natal-RN mostrou que esta cidade parece ter a maior incidência de LES já
descrita na literatura: 8,7 casos novos/100 mil habitantes/ano8. Quanto à faixa etária mais
comum de se iniciar o LES, a literatura aponta uma maior ocorrência entre 20-40 anos, acometendo principalmente mulheres jovens. No entanto, o sexo masculino também pode ser acometido numa proporção de 9:1. Quanto à presença da doença segundo a etnia, esta pode
ocorrer em todas as etnias e em todas as partes do mundo3.
Devido à multiplicidade de danos orgânicos, o LES requer um cuidado constante e sistemático. O diagnóstico precoce e a manutenção de um acompanhamento periódico contínuo, incluindo medidas preventivas, como a baixa exposição à radiação ultravioleta, pode prevenir reativações da doença, especialmente detectando precocemente o acometimento renal9-12.
O diagnóstico é norteado utilizando-se os critérios de classificação propostos em 1982
pelo American College of Rheumatology (ACR), revisados em 199713. Utilizando os critérios
propostos pelo American College of Rheumatology o diagnóstico se fundamenta na presença de pelo menos quatro critérios dos 11 citados a seguir: Eritema malar, Lesão discóide, Fotossensibilidade, Úlceras orais/nasais, Serotite, Artrite não erosiva, Comprometimento renal, Alterações neurológicas, Alterações hematológicas, Alterações imunológicas,
Anticorpos antinucleares14.
Um estudo realizado na cidade de Natal, com o objetivo de determinar a frequência das manifestações clínicas e laboratoriais de pacientes com LES e identificar os danos precoces em pacientes com diagnóstico recente, verificou que os danos orgânicos mais presentes em
provavelmente, é correlacionado a uma maior quantidade de luz solar (radiação ultravioleta) na região5,15.
Quanto ao tratamento medicamentoso, varia de agentes antimaláricos,
corticosteroides e agentes imunosupressores9. Entre as medidas gerais utilizadas no
tratamento16, destacam-se: Educação (informar ao paciente e a seus familiares sobre a
doença e sua evolução, possíveis riscos e os recursos disponíveis para diagnóstico e tratamento. Ressalta-se a necessidade de cumprimento das medidas estabelecidas pelo médico); Apoio psicológico; Atividade física (com repouso nos períodos de atividade sistêmica da doença, deve ser recomendada); Dieta (embora não haja evidência científica de que os alimentos possam influenciar o desencadeamento ou a evolução da doença: recomenda-se a adoção de dieta balanceada, evitando-se excessos de sal, carboidratos e lipídios); Proteção contra luz solar e outras formas de irradiação ultravioleta; Evitar tabagismo; e Controle rigoroso dos fatores de risco cardiovascular (glicemia, hipertensão arterial, dislipidemia e obesidade).
Estudos que investigam os impactos do LES na qualidade de vida do sujeito apontam a fadiga e dor crônica como manifestações comuns na doença e extremamente
comprometedoras ao paciente17-22. São também relatadas na literatura manifestações
psicológicas como angústia19 e desordens psiquiátricas podendo ser associadas a prejuízo
cognitivo e a pobre qualidade de vida, número de hospitalizações, ansiedade, depressão associada à dor. Estes três últimos aspectos são apontados como determinantes principais na
saúde relacionada à qualidade de vida23. A incapacidade para o trabalho associada a
qualidade de vida limitada também tem sido amplamente citada na literatura24,25. A
intervenção psicológica também tem sido alvo de investigações no sentido de avaliar a
redução de fatores psicológicos como angústia psicológica, depressão, entre outros22,26,
colaborando para melhorias na qualidade de vida do paciente.
Historicamente, o termo resiliência surge associado aos estudos da Física e da Engenharia, referindo-se à capacidade que um material tem de absorver energia sem sofrer deformações permanentes. A resiliência psicológica consiste na capacidade de superar as
adversidades, o que não significa que o indivíduo saia da crise ileso30. A compreensão da
resiliência, embora seja bastante subjetiva, pertence à estrutura do desenvolvimento psicológico, podendo ser entendida como a capacidade pessoal de enfrentar a adversidade,
não no sentido de resistir, mas de ultrapassá-la e superá-la com êxito31.
Os primeiros trabalhos sobre resiliência dizem respeito, sobretudo, às crianças e aos adolescentes; todavia, atualmente evidenciam-se estudos das diferentes fases de vida: desde
a infância até à velhice32. Embora ainda escassos, mais recentemente já existem estudos
envolvendo resiliência e doenças crônicas como HIV27, Diabetes33 e LES34.
A resiliência associada à enfermidade pode ser compreendida como a capacidade individual de lidar com a doença, aceitando suas limitações, colaborando com aderência ao
tratamento, readaptando-se e sobrevivendo de forma positiva35. A resiliência também
compreende os fatores de risco e proteção. Fatores de risco são todos os eventos que se configuram como obstáculo ao nível individual ou ambiental e que potencializam a vulnerabilidade do indivíduo a resultados desenvolvimentais negativos. Os fatores de proteção são os fatores com potencial capacidade para minimizar os eventuais efeitos negativos ou
disfuncionais na presença do risco29. Para este estudo considerou-se que a adesão ao
tratamento pode ser compreendida como um importante comportamento de proteção, já que,
seguindo o tratamento, o paciente poderá evitar o agravamento da doença36. A não adesão
ao tratamento foi compreendida neste trabalho como um comportamento que pode ser
considerado de risco (fator de risco), já que poderá agravar os sintomas da doença37. A falta
de adesão ao tratamento coopera para o aumento da sintomatologia e de hospitalizações38.
A terminologia envolvendo a adesão ao tratamento varia muito na literatura, mas no geral, a literatura médica aponta que a adesão ao tratamento está relacionada com o fato do paciente seguir as recomendações médicas e tomar a medicação conforme prescrito pelo seu
médico37, seguir uma dieta ou executar mudanças no estilo de vida e o plano terapêutico
orientado pelo agente promotor de saúde38. A “concordância” do paciente, atualmente tem
sido também colocada como importante fator no processo de adesão, indicando um acordo
entre o paciente e o médico sobre o tratamento a ser tomado37,38. No LES esta adesão ao
comorbidades, a adesão ao tratamento poderá diminuir os impactos da doença e melhorar a
qualidade de vida do paciente37.
Um ponto importante a ser considerado quando se trata da adesão ao tratamento em pacientes com LES é que, embora recentemente tenha havido uma diminuição drástica da mortalidade por LES, que pode ser parcialmente atribuída aos avanços do tratamento que retardam a progressão da doença e minimizam os danos, para muitos pacientes com LES, no entanto, estes regimes de tratamento são complexos, causando problemas na adesão ao
tratamento39. Assim, várias causas da não adesão ao tratamento são citadas na literatura,
desde aquelas situações em que o paciente ‘opta’ por não seguir um tratamento e
recomendação, causadas por inúmeras razões como, por exemplo, a comunicação médico-paciente, as crenças do médico-paciente, efeitos colaterais, entre outros, até problemas de adesão
“não intencionais” quando um paciente não consegue seguir as recomendações de
tratamento devido a circunstâncias que estão fora de seu controle, como por exemplo, a falta
de compreensão, a barreira da língua, esquecimentos, etc39. Neste caminho, a aliança de
trabalho entre médico e paciente, caracterizada por uma boa comunicação das metas e tarefas de tratamento, juntamente com a confiança e simpatia na relação, poderão contribuir
para a adesão do paciente40.
Considerando as medidas gerais recomendadas na abordagem terapêutica em
pacientes com LES16, bem como artigos que abordam a questão da adesão ao tratamento
nestes pacientes37,39, consideramos, para o presente estudo, como comportamentos que
podem ser compreendidos como de risco para o paciente (fatores de risco) a não adesão ao
tratamento. Consideramos como não adesão: não realizar o tratamento medicamentoso e os
tratamentos sugeridos, não conhecer a doença, não aceitar suas limitações, não seguir as recomendações médicas (de comparecimento sistemático ao médico, de não fumar, se proteger contra a luz solar e realizar controle de risco cardiovascular) e não possuir rede de
apoio. Como comportamentos de proteção (fatores de proteção) consideramos a adesão ao
tratamento e possuir rede de apoio.
2. JUSTIFICATIVA
Tendo em vista os impactos do LES na vida do paciente, que incluem danos físicos
com presença de dor, o que pode levar a uma limitação de atividades de vida diária26, com
presença de sintomas psicológicos como angústia e depressão41,42, baixa qualidade de
vida26,43, e o fato de Natal-RN ter uma alta incidência da doença8, sendo crescente a evolução
tecnológica na assistência à saúde, que permite uma maior sobrevivência de pacientes com
diversas doenças crônicas, como o LES39,44, é importante compreender a resiliência nestes
pacientes. Pois se resiliência associada à enfermidade pode ser compreendida como a capacidade individual de lidar com a doença, aceitando suas limitações, colaborando com
aderência ao tratamento, readaptando-se e sobrevivendo de forma positiva35, pode-se supor
que a resiliência poderá ser um fator importante na adesão ao tratamento e para melhoria da qualidade de vida destes pacientes. Uma vez que a resiliência poderá proporcionar ao paciente uma melhor adaptação à situação de conviver com a doença crônica, já que o sujeito com resiliência alta tende a ter uma postura ativa frente à adversidade, de forma a enfrentá-la
e se adaptar a esta nova realidade33,34. Compreendendo como se encontra a resiliência
destes pacientes podemos conhecer como pacientes com resiliência alta, média e baixa se portam frente ao tratamento, de forma a aderir ou não a ele.
Com este estudo poderemos traçar um perfil das pacientes atendidas, bem como a visão delas das dificuldades ou não de seguir o tratamento, e se estes aspectos se encontram associados à resiliência, ou seja, se pacientes com valores altos de resiliência conseguem ter uma maior adesão ao tratamento. Buscamos também conhecer a visão do paciente frente à acessibilidade dos serviços de saúde, compreensão importante quando se trata de adesão ao tratamento, pois se o acesso ao serviço e a medicação forem dificultosos para o paciente, podemos supor que isto poderá ser um fator apto a dificultar a adesão ao tratamento.
colocassem a doença num ponto central em sua escala pessoal de valores45. Conhecendo esta realidade podem-se construir terapêuticas que visem à melhoria da resiliência nestes pacientes, já que a resiliência tem sido apontada como um importante fator para a adaptação
do paciente à doença e para a adesão ao tratamento33. Além disso, há uma carência de
estudos que avaliam a resiliência em pacientes com LES. Identificamos apenas um que avalia
diretamente a resiliência nestes pacientes34.
3. OBJETIVOS
3.1 Geral
Avaliar a resiliência e os comportamentos de adesão ao tratamento autorrelatados, em
pacientes com LES, investigando possíveis associações entre resiliência e adesão ao
tratamento.
3.2 Específicos
Delinear o perfil sociodemográfico das pacientes com LES atendidas no serviço de
Reumatologia do Hospital Universitário Onofre Lopes – UFRN;
Identificar as redes de apoio citadas pelos pacientes;
Identificar os principais motivos autorrelatados quando não há adesão ao tratamento;
Caracterizar os aspectos relativos à assistência a estes pacientes, no que diz respeito
ao acesso a consulta, a exames e a medicação.
4. MÉTODO
Trata-se de um estudo de caráter transversal, com finalidade descritiva e exploratória.
População e Amostra
A população desta pesquisa foi composta de 40 pacientes com diagnóstico de LES em atendimento no Ambulatório de Reumatologia do HUOL-UFRN, do sexo feminino, com idade acima de 18 anos e que concordaram em participar da pesquisa. O cálculo para obtenção da amostra total foi feito através da Amostra Aleatória Simples, com o intervalo de confiança de 95%.
Os critérios de inclusão foram: pacientes em atendimento no Ambulatório de Reumatologia do HUOL-UFRN com diagnóstico de LES confirmado segundo os critérios do
ACR13 e idade acima de 18 anos, sem comprometimento neuropsiquiátrico grave que
impossibilite a compreensão e a realização da pesquisa.
Procedimentos e protocolos
Como instrumento se utilizou a Escala de Resiliência desenvolvida por Wagnild &
Young46 e um questionário de informações sociodemográficas e dados referentes à doença.
Para avaliar as características de resiliência, foi utilizada a Escala de Resiliência
desenvolvida por Wagnild & Young46 (ANEXO II). Trata-se de instrumento utilizado para medir
níveis de adaptação psicossocial positiva em face de eventos de vida importantes. Possui 25 itens descritos de forma positiva com resposta tipo likert variando de 1 (discordo totalmente) a 7 (concordo totalmente). Os escores da escala oscilam de 25 a 175 pontos, com valores altos indicando elevada resiliência. A literatura aponta que este instrumento possui boa
confiabilidade e validade, já sendo adaptado para o português47.
análise, já que se trata de um recorte de um estudo maior que envolve resiliência e adesão ao tratamento: a qualidade de vida que foi avaliada através do SF-36, as crenças destas mulheres sobre a doença, estratégias de enfrentamento e sentimentos frente à doença.
Inicialmente, o pesquisador apresentou o projeto ao Comitê de Ética e Pesquisa da
UFRN para aprovação, que foi realizada em 12/08/2009 com parecer no 066/2009. Após
aprovação do Comitê e consentimento da pesquisa in loco, iniciamos um estudo piloto, com a parceria dos reumatologistas que atendem os pacientes com LES no HUOL, tendo em vista os critérios de inclusão. Este estudo piloto objetivou corrigir possíveis falhas, e delinear corretamente o estudo em sua amplitude e procedimentos.
Após estudo piloto e reajuste nos instrumentos, deu-se início à coleta de dados, que foi realizada de Março de 2010 a Janeiro de 2011. Para isso realizamos um levantamento e triagem, em conjunto com os reumatologistas do hospital, dos pacientes solicitados conforme as exigências dos critérios de inclusão da pesquisa. Todos os instrumentos foram aplicados oralmente e individualmente nos pacientes selecionados.
Antecedendo a aplicação, o pesquisador informou ao paciente sobre os objetivos da pesquisa, aplicação do instrumento, privacidade, e destino dos dados obtidos. Após explicação foi solicitada a assinatura do termo de Consentimento Livre e Esclarecido.
Primeiramente foram coletados dados do questionário e posteriormente a escala de resiliência desenvolvida por Wagnild & Young. O tempo para realizar todo o procedimento foi em média 40 minutos.
Análise e tratamento dos dados
Para análise dos dados foi utilizado o programa Statistic, versão 6.0. A estatística
facilitado a medicamento). A análise de correlação foi aplicada para verificar se existia associação entre a resiliência e as variáveis quantitativas envolvidas no estudo (Idade, carga horária de trabalho, quando o médico foi consultado após aparecer os primeiros sintomas, tempo de descoberta do diagnóstico após procurar o médico, duração de tratamento especializado e tempo de doença após diagnóstico). O nível de significância adotado nos testes foi de 5% (p-valor < 0,05). Na Escala de Resiliência se utilizou a correção do manual. A
categorização utilizada foi: 25-75 = resiliência baixa, 76-125 = moderada e 126 – 175 – alta28.
Aspectos éticos
O estudo foi aprovado pelo Comitê de Ética em Pesquisa da Universidade Federal do
Rio Grande do Norte no. 066/2009, Brasil, tendo cumprido todas as exigências estabelecidas
5. ARTIGO PRODUZIDO
Artigo: Resilience and Treatment Adhesion in Patients with Systemic Lupus Erythematosus
Periódico: The Open Rheumatology Journal
Status da publicação: The Open Rheumatology Journal, 2014, vol8, 1-8. Iss 1874-3129/ DOI
10.2174/1874312920140127001
Send Orders for Reprints to reprints@benthamscience.net
The Open Rheumatology Journal, 2014, 8, 1-8 1
1874-3129/14 2014 Bentham Open
Open Access
Resilience and Treatment Adhesion in Patients with Systemic Lupus
Erythematosus
Daniella Antunes Pousa Faria*,1, Luciana Silva Revoredo1, Maria José Vilar1 and Eulália Maria Chaves Maia1,2
1Programa de Pós-Graduação em Ciências da Saúde, Universidade Federal do Rio Grande do Norte (UFRN), Natal,
Brazil
2
Programa de Pós-Graduação em Psicologia, Universidade Federal do Rio Grande do Norte, Natal, Brazil
Abstract: Background: Systemic Lupus Erythematosus (SLE) is a chronic autoimmune, rheumatic inflammatory disease that can cause significant morbidity with evident psychological impacts and obvious harm to quality-of-life that require the patient to adapt treatment.
Objective: Assessment of resilience and the self-reported treatment adhesion behaviors of patients with SLE, investigating which of these factors are associated to resilience.
Method: Cross-sectional study of 40 women with SLE. A questionnaire with social demographic data, health history and the Wagnild Young Resilience Scale were used.
Results: 62.5% followed the medical treatment properly but 55% found it difficult. 27.5% of the patients presented low resilience, 57.5% medium and 15% high resilience. Resilience was associated in the chi-square test (p-value < 0.05) with the variables work, understanding SLE, trying to find out about SLE, following the treatment correctly, difficulty in following the treatment and stopping some activity because of the disease. In the correlation analysis, resilience was associated with age (-0.3960), number of working hours (0.5533), specialized treatment duration (-0.8103) and disease duration from diagnosis (-0.8014).
Conclusion: Patients with high resilience tended to follow treatment correctly, tried to understand the disease and adhered more to the treatment to avoid risks and promote protection factors. Therefore knowledge of resilience in patients with SLE is necessary. It is important that the state takes necessary actions to facilitate access to treatment, to educational programs and to medical support. Awareness and counselling sessions must be initiated to develop and promote individual capacities to learn how to tackle with the disease for which psychological support of family and doctors can play a significant role.
Keywords: Resilience, treatment adhesion, systemic lupus erythematosus.
INTRODUCTION
Systemic Lupus Erythematosus (SLE) is a chronic autoimmune, rheumatic inflammatory disease that can affect several organs and systems in the body, causing significant morbidity [1-3] with evident psychological impacts [3,4] such as anxiety and depression [5,6] and obvious harm to life satisfaction [3] and quality-of-life [7,8] that require the patient to adapt treatment and the situation of living with a chronic disease. It is more common in young persons, especially women [3]. The incidence of SLE in Natal RN/Brazil is apparently higher than those reported in other regions of the world, 8.7/100 000/year [9].
*Address correspondence to this author at the UFRN Programa de Pó s-graduação em Ciências da Saúde, Tereza Campos, 2070, apto, 601, Lagoa Nova, CEP 59062-530. Natal, Rio Grande do Norte. Brazil;
Tel: (+55)8433429776; Fax: (+55)8433429776; E-mail: daniellapousa@gmail.com
In this context, it is important to introduce the concept of resilience: it is an unfixed, universal capacity, that can be triggered and disappear at certain times of life [10-13], and allows the subject to prevent, minimize or overcome noxious effects of adversities, and that even if not unscathed, he/she can come out strengthened or transformed from these situations [10-12]. Resilience further involves risk factors that refer to every event that is an obstacle at the individual or environmental level and that enhance the individual´s vulnerability to negative developmental results while protection includes factors with potential capacity to minimize the possible negative or dysfunctional effects in the presence of the risk [13].
2 The Open Rheumatology Journal, 2014, Volume 8 Faria et al. understood as an important protection behavior for
disease-related resilience and non-adherence as a risk factor, because not following the treatment could worsen the disease [15].
Therefore in SLE, risk is considered, in this study, non-adhesion to the treatment that includes: not following the medication and suggested treatments, not knowing about the disease, not accepting its limitations, and not following medical recommendations (regular visits to the physician, no smoking, avoiding sunlight and controlling heart disease risk). Adhesion to the treatment and having a support network are considered as protection factors. Thus when dealing with resilience in the situation of living with a chronic disease such as SLE, adhesion to the treatment is a central issue.
Thus the objective of the present study was to assess resilience and treatment adhesion behaviors reported by patients with SLE, investigating which of these factors were associated with resilience.
MATERIALS AND METHODOLOGY
Cross-sectional study, descriptive and exploratory purpose, with patients diagnosed for SLE.
Population Studied
Forty female patients over 18 took part, diagnosed for SLE, from the Rheumatology Outpatients Department of the Onofre Lopes Hospital (HUOL), Natal/RN – Brazil, who agreed to participate in the research. The data were collected from March 2010 to January 2011, after approval from the Ethics Committee; research number 066/09, at the Federal University of Rio Grande do Norte, Brazil. This research followed the norms established by theHelsinki Declaration of 1975, as revised in 2008.
The total sample was obtained using The Single Random Sample, with 95% confidence interval. The inclusion criteria were: the patients were in treatment at the HOUL Rheumatology Outpatients Department, diagnosed for SLE and over 18, without clinical conditions that in the opinion of the physician, could damage participation in the investigation, and no record of neuropsychiatric disorders.
Instruments Used
A questionnaire was administered with social and demographic data, health aspects and history (disease data, diagnosis and support network data, treatment data, treatment adhesion behaviors, disease impact data, risk and protection factors and data on the patient´s daily life) elaborated based on information contained in the Systemic Lupus Erythematosus Consensus [16]. The Resilience Scale developed by Wagnild & Young [17] was used that measures the levels of positive psychological adaptation to important life events where 25 items are described positively with a likert type response ranging from 1 (disagree completely) to 7 (agree completely). The scale scores range from 25 to 175 points and high values indicate high resilience. This is a valid and reliable instrument that has been translated into Portuguese [18].
Methodological Procedures
Rheumatologists were contacted to identify patients diagnosed with SLE that met the inclusion criteria and the research objectives were explained to these patients. On their approval to participate, the patients were made to sign a free consent term. The questionnaire was then administered, followed by the Wagnild & Young Resilience Scale [17]. The procedure took approximately 40 minutes.
Data Analysis
The Statistic program, version 6.0, was used to analyze the data. Descriptive statistics were used to describe the profile of the patients analyzed and characterize the disease and disease-induced behavior. The chi-squared test was applied to verify whether there was association between the resilience variable and the categorical variables involved in the study (work, SLE understanding, attempt to find out about SLE, followed the treatment correctly, difficulty in following the treatment, stopped activity because of SLE, education, family income, understanding of SLE care, understanding the treatment, medical attention frequency, smoking, heart disease risk control which includes hypertension, obesity, dyslipidemia and glucose control [16], extra medication treatment, received support, government assistance, facilitated access to consultation, facilitated access to tests and facilitated access to medication). Correlation analysis was applied to verify whether there was association between resilience and the quantitative variables listed below involved in the study (age, number of working hours, when the physician was consulted after first symptoms appear, time taken for diagnosis after seeking the physician, specialized treatment duration and disease duration from diagnosis).
The level of significance adopted in the cases was 5% (p-value < 0.05). The Resilience Scale was corrected by the manual. For this study, resilience was considered as: 25-75 = low resilience, 76-125 = medium and 126 – 175 –high resilience [12].
RESULTS
Table 1 shows the profile of the patients analyzed.
According to the above table, 32.5% of the patients were in the 42 to 48-year-old age group, 52.5% were married, 50% had only primary education, 65% had 1-3 minimum wage family income and only 17.5% worked outside the home.
The patients had SLE for an average of 6.88 ± 5.39 years duration, mean 5.0 years. The patients reported that after getting medical help they took on average 7.58 ± 9.66 months to discover the diagnosis, mean 3.0 months. The average treatment duration of these patients was 6.47 ± 4.93 years, mean 5.0 years.
Resilience and Treatment Adhesion in Patients with Systemic Lupus Erythematosus The Open Rheumatology Journal, 2014, Volume 8 3
Table 1. Social and Demographic Profile of the Study Sample
Characteristics N %
Age Group in Years
21 to 27 8 20.0
28 to 34 9 22.5
35 to 41 3 7.5
42 to 48 13 32.5
49 to 55 4 10.0
56 to 62 3 7.5
Civil State
Single 14 35.0
Married 21 52.5
Divorced 4 10.0
Other 1 2.5
Education
Primary 20 50
High School 15 37.5
University 1 2.5
University unfinished 4 10.0
Work Outside Home
No 33 82.5
Yes 7 17.5
Working Hours
Does not work 33 82.5
20 hours 5 12.5
40 hours 2 5.0
Family Income (in Minimum Wage)
Less than 1 m.w. 10 25.0
From 1 to 3 m.w. 26 65.0
From 4 to 6 m.w. 3 7.5
From 7 to 9 m.w. 1 2.5
symptoms of depression (8.6%) and disease activity (8.6%). The pain reported by 65.5% of the patients was the symptom that distressed them most.
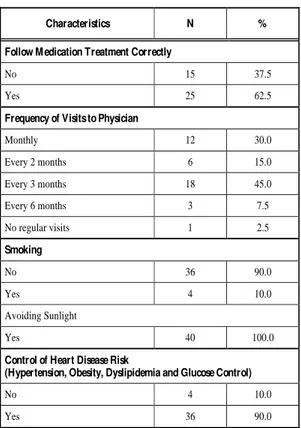
Resilience involves risk and protection factors; in the case of SLE risk is considered non-adhesion to the treatment and protection is adhesion to the treatment. The patients were asked some questions to understand their reports of the characteristics of adhesion to the treatment, using as reference the general means highlighted as important in the therapeutic approach of the Systemic Lupus Erythematosus Consensus [16] and the results are shown in Table 2.
The medication treatment was carried out properly by 62.5% of the patients and only 2.5% did not visit the physician regularly. Most followed the recommendations not
to smoke, (90%), avoid sunlight (100%) and control heart disease (90%). However, 55% reported difficulty in following the medication treatment because the medication was not available from the SUS – Single Health System (Sistema Único de Saúde) (54.5%) and forgetfulness (36.4%). The SUS is the public health care system that ensures access to whole, universal and free health care for the Brazilian population; 9.1% did not know how to answer the reason for difficulty.
Table 2. Risk and Protection Factors Assessed of 40 Patients with SLE
Characteristics N %
Follow Medication Treatment Correctly
No 15 37.5
Yes 25 62.5
Frequency of Visits to Physician
Monthly 12 30.0
Every 2 months 6 15.0
Every 3 months 18 45.0
Every 6 months 3 7.5
No regular visits 1 2.5
Smoking
No 36 90.0
Yes 4 10.0
Avoiding Sunlight
Yes 40 100.0
Control of Heart Disease Risk
(Hypertension, Obesity, Dyslipidemia and Glucose Control)
No 4 10.0
Yes 36 90.0
Of the patients assessed, 32.5% stated that they did not understand SLE, 42.5% partly understood it and 25% stated they understood the disease regarding self-care, 60% stated they understood the self-care they should take because of the disease, 37.55% partly understood and 2.5% did not know what care they should take. Regarding understanding the treatments, 60.5% declared that they understood the treatments and 37.5% partly understood. In addition, 42.5% stated that they did not look for information on SLE other than that given by the physician, 57.5% looked for information on SLE in addition to what was said by the physician.
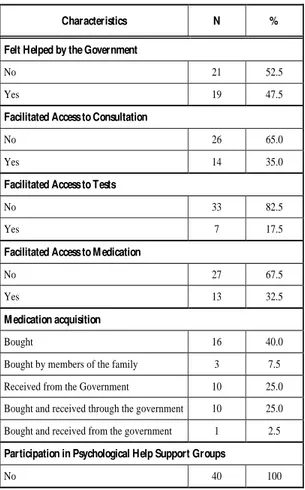
Regarding the support network perceived by the patients, 82.5% of the patients stated they received support and 72.5% felt supported by their family. Table 3 shows the results regarding the government support network.
4 The Open Rheumatology Journal, 2014, Volume 8 Faria et al.
Table 3. Description of the Government Support Network
Characteristics N %
Felt Helped by the Government
No 21 52.5
Yes 19 47.5
Facilitated Access to Consultation
No 26 65.0
Yes 14 35.0
Facilitated Access to Tests
No 33 82.5
Yes 7 17.5
Facilitated Access to Medication
No 27 67.5
Yes 13 32.5
Medication acquisition
Bought 16 40.0
Bought by members of the family 3 7.5
Received from the Government 10 25.0
Bought and received through the government 10 25.0
Bought and received from the government 1 2.5
Participation in Psychological Help Support Groups
No 40 100
and tests are free of charge through the Single Health System, called SUS. This health system is financed by the state. But not always patients seeking SUS services can receive medical care due to the large number of patients and lack of professionals to serve them. Furthermore, no patient participated in a support group or had psychological help.
27.5% of the patients presented low resilience, 57.5% medium resilience and around 15% presented high resilience. Table 4 shows that patients presented a mean resilience of 99.83
± 27.70 points, average of 106.50. These results were categorized as medium resilience [12].
The chi square and Pearson tests were applied in order to identify which of the variables analyzed had to be associated with resilience. Only six of the 19 variables analyzed were associated with resilience (p-valor < 0.05). Therefore resilience was associated with the variables work, giving up some activity because of SLE, following the treatment properly, the difficulty in following the treatment, trying to know more about lupus and understanding lupus, at the level of 5% significance (Table 5).
The results indicated that the patients that worked tended to present high resilience, while those that did not work presented low resilience. None of the patients with low resilience worked outside the home. 91% of the patients with medium resilience did not work, and those that had high resilience corresponded to 83% of the patients that worked.
Patients who stopped some activity because of SLE tended to present low resilience while those that did not, tended to present high resilience. The patients with low resilience had stopped some activity because of SLE. Among those with high resilience, 83% were the patients who did not stop any activity due to SLE.
The patients who carried out the medication treatment correctly tended to present high resilience, while those that did not tended to present low resilience. 91% of patients with low resilience were patients that did not follow the medication treatment correctly. Among those that had medium resilience 78% followed the treatment correctly, while all those with high resilience followed the medication treatment properly. Furthermore the patients who found it difficult to follow the treatment tended to present low resilience, while those that did not tended to present high resilience levels. All the patients that found it difficult to follow the treatment had low resilience. Among those with medium resilience 52% did not find it difficult to follow the treatment and those with high resilience were all the patients that did not find it difficult to follow the treatment.
The patients that understood SLE tended to present high resilience, while those who did not tended to present low resilience. 64% of the patients with low resilience were the patients who did not understand SLE. Among those with medium resilience, 52% understood in part, and those with high resilience corresponded to 83% of the patients who understood SLE.
Patients who tried to find out about SLE, who looked for information on the disease in addition to that given by the physicians, tended to high resilience, while patients who did not tended to present low resilience. 73% of the patients with low resilience were the patients that did not try to find out about SLE. 39% of the patients with medium resilience did not try to find out about SLE and those with high resilience corresponded to 83% of patients that tried to find out about SLE.
The correlation test showed that resilience was associated with 04 of the variables analyzed, at 5% level of significance (p-value <0.05), shown in Table 6.
There was low and negative correlation between resilience and age, -0.3960 (39.6%): as age increased resilience decreased. There was a positive and moderate correlation between resilience and working hours, 0.5533 (55.33%): as the number of hours worked increased
Table 4. Resilience Values Achieved by Patients Evaluated
Variables Value Absolute Mean ± DP Average Confidence Interval (95%)
Minimum Maximum Minimum Maximum
Resilience and Treatment Adhesion in Patients with Systemic Lupus Erythematosus The Open Rheumatology Journal, 2014, Volume 8 5
Table 5. Pearson Test Chi-Square for the Resilience Classification Variable
Pearson Chi-Square Analysis of Association p-Value
Resilience x Work p=0.00002
Resilience x giving up activity because of SLE p=0.00000
Resilience x following treatment correctly p=0.00006
Resilience x Difficulty in following the treatment p=0.00022
Resilience x Found out about SLE p=0.00641
Resilience x Understanding SLE p=0.00119
Resilience x Education p=0.15114
Resilience x Family income p=0.38561
Resilience x Understanding care of SLE p=0.43320
Resilience x Understanding treatment p=0.26602
Resilience x Frequency of visiting the physician p=0.80272
Resilience x Smoking p=0.46573
Resilience x Control of heart disease risk p=0.63335
Resilience x Extra-medication treatment p=0.30162
Resilience x Receiving support p=0.99670
Resilience x Government assistance p=0.98291
Resilience x Facilitated access to consultations p=0.58628
Resilience x Facilitated access to tests p=0.36778
Resilience x Facilitated access to medication p=0.94107
Table 6. Analysis of Resilience Correlation
Correlation Resilience
Age -0.3960
Number of working hours 0.5533
When the physician was consulted after first symptoms appear 0.2084
Time taken for diagnosis after seeking the physician 0.0666
Specialized treatment duration -0.8103
Disease duration from diagnosis -0.8014
resilience also increased. There was a negative and high correlation between resilience and disease duration from diagnosis, -0.8014 (80.14%): as disease duration increased, resilience decreased. There was strong and negative correlation between resilience and specialized treatment duration, -0.8103 (81.03%): as treatment duration increased resilience decreased.
DISCUSSION
The patients assessed were in an age group where people are normally in full working activity, but in the population investigated most had stopped working due to SLE. Furthermore, the patients had stopped doing housework and leisure activities because of fatigue, depression symptoms,
disease activity and pain and the latter was the most distressing. These symptoms are also described in the literature as being associated to incapacity for work [2,19-21].
Many of the SLE symptoms interfered in several areas of the patient´s life [22] and consequently in their quality of life [7,8] and consequences can include giving up regular work [2,19,21] and daily activities, as the results above show. Nevertheless, resilience can be a contributing factor so that these patients can change their lifestyle but maintain their activities as far as possible because resilience is successful adaptation in spite of adversity or stress and implies efficacious performance of daily activities [12,13, 23].
The association found between resilience and work and the association found between resilience and stopping some activity because of the disease, corroborated with the statement that high resilience helps the subject overcome difficulties that he/she may find in life [11] tending to maintain their activities as far as possible even in adversity, in the case of SLE. The correlation analysis corroborated these statements showing a moderate and positive correlation between resilience and working hours, because resilience also tended to increase as the number of working hours increased. This result strengthens the discussion that patients with high resilience tend to be adapted to the adverse situation [11-13] and continue work and activities, even with the limitations of the disease.
Most of the patients in the present study had medium resilience, this result was similar to a study that aimed to assess the resilience in forty-five patients with SLE, in which the majority (71%) had scores in the average levels of resilience [23], that means that they were managing to adapt to the disease to avoid risks and to promote protection factors that contributed to treatment adhesion. Thus, resilience could be understood as a contributor to protective effect [23], and high scores are associated with better physical health, fewer symptoms and a better quality of life while low scores are inversely related to depression and other psychiatric disorders [24].
6 The Open Rheumatology Journal, 2014, Volume 8 Faria et al.
with low resilience. The patients that did not find it difficult tended to present high resilience.
Forgetfulness was reported as one of the difficulties, but the main cause indicated was that the medication was not available from the SUS. The population investigated in the present study depended on government assistance to carry out treatment and was predominantly from the lower economic class. The government provided the medication free, but in practice it was frequently not available at the points of delivery. Thus most patients did not feel helped by the government because they did not have facilitated access to consultation, tests and medication, the factors that prevented these patients from adhering to the treatment.
Furthermore, no patient had access to support groups or psychological treatment. The support the patients stated to have was usually from the family, because they could not have access to psychological treatment and support groups
via the SUS, which is a matter of concern because psychological manifestations such as depression [4,5,28], mood disturbance and anxiety [28,29] are common in patients with SLE and require specialized psychological support.
The measures for protection factors were mostly followed by the patients, because most carried out the medication treatment and recommendations correctly such as not smoking, avoiding sunlight, systematic heart disease control, and visiting the physician regularly. Following the medical recommendations and the treatment properly are significant factors for treatment adhesion [26,27] and for understanding disease-linked resilience, because these adhesion behaviors indicate that the patient is managing to be resilient adapting to the adversity of having a chronic disease, accepting limitations, managing to overcome these limitations positively, not necessarily unscathed, but managing to adhere to the treatment.
Trying to understand the disease was also an important factor for treatment adhesion. Most of the patients assessed stated they understood at least in part the disease and most also stated that they understand the self-care. But few looked information on SLE, besides what was said by the physician that can be justified by their low education level, most patients had only primary education. However, there was association between resilience and understanding SLE and resilience and trying to find out about SLE, in addition to the information given by the physician; that is, the patients who understood SLE tended to present high resilience, and those that did not understand tended to present low resilience; patients that tried to find out about SLE also tended to present high resilience and those that did not, tended to present low resilience.
Awareness of the disease is an important factor for treatment adhesion [30] because even the most active patients, when they were not properly informed and did not establish a link with the health service, were more likely not to accept the treatment suggested [30]. Those that accepted the treatment, making it part of their daily routine, no longer perceived as an obligation [30]. Another study investigated the relationship between representations of the disease and depression in lupus patients and reported a perception of the disease as having negative, unpredictable life consequences
and patients with little understanding of lupus presented high depression levels [5]. Therefore understanding the disease is an important factor even for the psychological health of the patient.
Age had low and negative correlation with resilience; as age increased, resilience tended to decrease. But as the correlation was low, this result should be further investigated because there are few reports on resilience and age in the literature. However, research on resilience and its relationship with age and sex in 1.719 Swedish participants aged 19-103 showed that resilience was related to age [31] and the older individuals presented high resilience indices, contrary to the results of the present study.
Negative correlation between resilience and disease duration from diagnosis meant that as the disease duration increased resilience decreased and a strong and negative correlation between resilience and specialized treatment duration, meant that as treatment duration increased, resilience decreased, highlighting the issue that SLE is an unpredictable disease with fluctuating disease activity [21] and requires long-term treatment, and patients have to live with medication side-effects and the damage caused by the disease itself, that often results in reduced quality-of-life for the patient [22]. These aspects can discourage the patient, reducing the adaptation capacity and can further lead to dissatisfaction with life that interferes in resilience.
In this context, it is important to think about ways to promote resilience in patients with SLE because resilience has been described as one of important factors to achieve better treatment and health outcomes in patients with SLE [15]. To promote resilience, interventions are necessary in the environmental or external aspects, psychosocial and internal aspects of the subject [32], involving the articulation of the risk and protection factors [11,32,33].
An important factor that can contribute to promoting resilience in the population studied is a reorganization of certain external, psychological and social factors. Actions are required from the state to improve issues related to the situation of risks to the health of patients with SLE, for example, greater effectiveness in medication delivery and facilitated access to consultations and examinations to facilitate the adhesion to the treatment, especially for the population studied, that has little education and depends directly on the public health service. Furthermore, to promote resilience education also should be considered [15]. Assistance institutions should act to promote school education and educative actions for these patients because, as can be observed in the results, few patients really understand SLE, which is a determining factor for adhering to the treatment [15,30] and promoting resilience [15]. Understanding the disease the patients probably will be able to have a greater self-care, avoiding risk factors linked to the disease, such as exposure to the sun and smoking but taking protective measure such as, taking the medication correctly and frequent medical visits to control the disease.
Resilience and Treatment Adhesion in Patients with Systemic Lupus Erythematosus The Open Rheumatology Journal, 2014, Volume 8 7
they received from the family and their friends [15,32] have also been shown as factors that allow patients to feel more motivated to persevere and deal better with the disease [15].
As medical support is shown as important to overcoming the processes linked to the disease [15], there is a need for professionals and assistance institutions to implant a more friendly assistance service, offering information for patients about the disease, ways of caring and treatment, taking into account their educational level and culture, because this could contribute to the process of promoting resilience in these patients. For this to occur, specialization courses are necessary so that these professionals can understand the process of resilience and develop techniques to promote it in patients with SLE.
Regarding the internal protective factors associated to promoting resilience, generally, studies in several populations have shown that a person triggers a resilience process when he presents a sense of self efficacy, sense of humour and has intellectual capacities such as the potential for insight [11], self esteem [34] and autonomy [12] along with the addition of self-care, the development of positive challenging and self defence strategies [15]. Living with SLE implies just adjusting to the complex dynamic among the changes in lifestyle and habits that can contribute to preventing the risk factors, adaption of routines and adhesion to medication, the implementation of care and treatments.
Thus it is important to promote resilience so that the patient accepts the limitations of the disease, develops positive mental attitudes [15] and protection factors [12], that even include the treatment [15]. For this, it is necessary to adopt a healthy lifestyle, including modification in diet, regular physical exercise, stress control and excess work control, avoiding events that may trigger or aggravate symptoms [15]. Psychological support can be a factor that can help to develop or enhance these characteristics. The implantation of support groups and psychological assistance groups would be important for patients with SLE, because one could attempt to develop in these patients individual potentialities that could help to promote resilience as is the case of self-esteem [12,15], self-care [15] and autonomy [12]. The literature also reports that some patients with SLE have found strength to face the disease in spiritual inspiration [15] that is therefore an important factor to be considered in the process of promoting resilience.
CONCLUSION
It was concluded that resilience provides a healthy way of living for the patient with SLE and allows him/her to adapt to the life style and incorporate therapeutic practices that involve alterations in daily behavior patterns. Patients with high resilience tended to carry out the treatment correctly, tried to understand the disease and had greater treatment adhesion to promote the protection factors, and managed to maintain their daily activities, even with the limitations of the disease. Therefore, it is necessary to develop mechanisms that help promote resilience in patients with SLE. For the population studied, it must be taken into account that their low educational level probably meant that they had difficulty in understanding the disease and their low purchasing power means that these patients depend solely on
state aid, which is precarious in Brazil. State actions are needed to facilitate access to treatment, in addition to educational policies to improve understanding of the disease and the necessary treatments. Medical and family support are also described as fundamental to promote resilience. The internal aspects of the subject, such as the potential for insight, self-esteem, autonomy, self-care, development of positive reactive strategies and self-defense should also be considered for resilience promotion. Psychological support could help to develop these internal characteristics, contributing to promoting resilience and consequentially adhesion to treatment.
Limitation was cross-sectional presenting a cut of the sample studied. It is further emphasized that the sample number was small because of the requirements of the research inclusion criteria and that possible associations were not assessed between resilience and disease activity. Regarding the use of indices of disease activity such as SLEDAI, SLAM and the index of damage SLICC ACR-DI, unfortunately we could not apply them during the study due to operational issues of high demand of patients for outpatient care. That could be important data for the study of resilience linked to SLE, the subject of an intended future study. It is hoped that this study has gathered together information to increase knowledge of resilience in SLE patients, because there are very few studies on resilience and rheumatic diseases that limits comparison, mainly with results of studies from local populations, where there are specific studies yet on resilience and chronic patients of patients with SLE.
CONFLICT OF INTEREST
We declare that there is no conflict of interest.
ACKNOWLEDGEMENTS
The authors thank the UFRN Health Sciences Graduate Program in Health Sciences and the statistician Janiere Lira.
REFERENCES
[1] Daleboudt GM, Broadbent E, Berger SP, Kaptein AA. Illness perceptions in patients with systemic lupus erythematosus and proliferative lupus. Lupus 2011; 20(3): 290-8.
[2] Baker K, Pope J, Fortin P, Silverman E, Peschken C. Work disability in systemic lupus erythematosus is prevalent and associated with socio-demographic and disease related factors. Lupus 2009; 18(14): 1281-8.
[3] Kulczycka L, Sysa-Jedrzejowska A, Robak E. Life satisfaction together with positive and negative aspects in Polish patients with systemic lupus erythematosus. J Eur Acad Dermatol Venereol 2009; 23(3): 251-5.
[4] Carr FN, Nicassio PM, Ishimori ML, et al. Depression predicts self-reported disease activity in systemic lupus erythematosus. Lupus 2011; 20(1): 80-4.
[5] Philip EJ, Lindner MA, Lederman HL. Relationship of illness perceptions with depression among individuals diagnosed with lupus. J Depress Anxiety 2009; 26(6): 575-82.
[6] Lederman LF, Lindner H, Greenwood KM, et al. Depression and pain in night time and daytime functioning of individuals with lupus. Psychol Health 2008; 23(5): 537-50.
8 The Open Rheumatology Journal, 2014, Volume 8 Faria et al.
[8] Reis MG, Costa IP. Qualidade de vida relacionada à saúde em paci-entes com lúpus eritematoso sistêmico no Centro-Oeste do Brasil. Rev Bras Reumatol [serial on the Internet]. 2010 August; [cited 2013 September 30]; 50(4): 408-22. Available from www.scielo.br/ scielo.php?script=sci_arttext&pid=S0482-50042010000400006&ln g=en. http://dx.doi.org/10.1590/S0482-50042010000400006 [9] Vilar MJP, Rodrigues JM, Sato EI. Incidência de lúpus eritematoso
sistêmico em Natal, RN - Brasil. Rev Bras Reumatol [serial on the Internet]. 2003 December; [cited 2014 January 02]; 43(6): 343-346. Available from http://www.scielo.br/scielo.php?script=sci_arttext& pid=S0482-50042003000600005&lng=en
[10] Oliveira MA, Reis VL, Zanelato LS, Neme CMB. Resiliência: Análise das Publicações no Período de 2000 a 2006. Psicol Cienc Prof [serial on the Internet]. 2008 December; [cited 2013 September 30]; 28(4): 754-67. Available from http://pepsic.bvsal ud.org/scielo.php?script=sci_arttext&pid=S1414-98932008000400008 [11] Carvalho FT, Morais NA, Koller SH, Piccinini CA. Fatores de
proteção relacionados à promoção de resiliência em pessoas que vivem com HIV/AIDS. Cad Saúde Pública [serial on the Internet]. 2007 September; [cited 2013 September 30]; 23(9): 2023-33. Available from http://www.scielo.br/scielo.php?script=sci_arttext& pid=S0102-311X2007000900011&lng=en&nrm=iso&tlng=pt [12] Ferreira CL, Santos LMO, Maia EMC. Resiliência em idosos
atendidos na rede de atenção básica de saúde em município do nordeste brasileiro. Rev Esc Enferm USP [serial on the Internet]. 2012 April; [cited 2013 September 30]; 46(2): 328-34. Available from http://www.scielo.br/scielo.php?script=sci_arttext&pid=S008 0-62342012000200009
[13] Poletto M, Koller SH. Contextos ecológicos: promotores de resiliência, fatores de risco e de proteção. Estud psicol (Campinas) [serial on the Internet]. 2008 September; [cited 2013 September 30]; 25(3): 405-16. Available from http://www.scielo.br/scielo.ph p?script=sci_arttext&pid=S0103-166X2008000300009&lng=en&n rm=iso&tlng=pt
[14] Bianchini DCS, Dell’Aglio DD. Processos de resiliência no contexto de hospitalização: um estudo de caso. Paidéia [serial on the Internet]. 2006 February; [cited 2014 January 02]; 16(35): 427-436. Available from http://www.scielo.br/pdf/paideia/v16n35/v16n 35a13.pdf
[15] Sutanto B, Singh-Grewal D, McNeil HP. et al. Experiences and perspectives of adults living with systemic lupus erythematosus: thematic synthesis of qualitative studies. Arthritis Care Res 2013; 65(11): 1752-65.
[16] Borba EF, Latorre LC, Brenol JCT, et al. Consenso de Lúpus
Eritematoso Sistêmico. Rev Bras Reumatol [serial on the Internet]. 2008 August; [cited 2013 September 30]; 48(4): 196-207. Available from http://www.scielo.br/scielo.php?script=sci_arttext& pid=S0482-50042008000400002&lang=pt
[17] Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. Research Support, Non-U.S. Gov’t. Journal of Nursing Measurement 1993; 1:165-178. [18] Pesce RP, Assis SG, Avanci JQ, et al. Adaptação transcultural,
confiabilidade e validade da escala de resiliência. Cad Saúde Pública [serial on the Internet]. 2005 April; [cited 2013 September 30]; 21(2): 436-48. Available from http://www.scielo.br/scielo.ph p?pid=S0102-311X2005000200010&script=sci_arttext
[19] Baker K, Pope J. Employment and work disability in systemic lupus erythematosus: a systematic review. Rheumatology (Oxford) [serial on the Internet]. 2009 January; [cited 2013 September 30]; 48(3): 281-4. Available from http://rheumatology.oxfordjournals. org/content/48/3/281.full.pdf+html
[20] Robinson DJ, Aguilar D, Schoenwetter M. et al. Impact of systemic lupus erythematosus on health, family, and work: The patient perspective. Arthritis Care Res (Hoboken) [serial on the Internet]. 2010 February; [cited 2013 September 30]; 62(2): 266-73. Available from http://onlinelibrary.wiley.com/doi/10.1002/acr. 20077/pdf
[21] Araújo AD, Traverso-Yépez MA. Expressões e sentidos do lúpus eritematoso sistêmico. Estud de Psicol [serial on the Internet]. 2007 August; [cited 2013 September 30]; 12(2): 119-27. Available from
http://www.scielo.br/scielo.php?pid=S1413-294X2007000200003&script=sci_arttext
[22] Aberer E. Epidemiologic, socioeconomic and psychosocial aspects in lupus erythematosus. Lupus 2010; 19(9): 1118-24.
[23] Cal SF, Santiago MB. Resilience in systemic lupus erythematosus. Psychol Health Med 2013; 18(5): 558-63.
[24] Wagnild GM, Collins JA. Assessing resilience. J Psychosoc Nurs Ment Health Serv 2009; 47(12): 28-33.
[25] Julian LJ, Yelin E, Yazdany J, et al. Depression, medication adherence, and service utilization in systemic lupus erythematosus. Arthritis Rheuma [serial on the Internet]. 2009 February; [cited 2013 September 30]; 61(2): 240-6. Available from http://www. ncbi.nlm.nih.gov/pmc/articles/PMC2875189/pdf/nihms138455.pdf [26] Oliveira-Santos M, Verani JFS, Klumb EM, Albuquerque EM.
Evaluation of adherence to drug treatment in patients with systemic lupus erythematosus in Brazil. Lupus 2011; 20(3): 320-9. [27] Garcia-Gonzalez A, Richardson M, Popa-Lisseanu MG, et al.
Treatment adherence in patients with rheumatoid arthritis and systemic lupus erythematosus. Clin Rheumatol 2008; 27(7): 883-9. [28] Jarpa E, Babul M, Calderon J, et al. Common mental disorders and
psychological distress in systemic lupus erythematosus are not associated with disease activity. Lupus 2011; 20(1): 58-66. [29] Bachen EA, Chesney MA, Criswell LA. Prevalence of mood and
anxiety disorders in women with systemic lupus erythematosus. Arthritis Rheum [serial on the Internet]. 2009 June; [cited 2013 September 30]; 61(6): 822-9. Available from http://www.ncbi.nlm. nih.gov/pmc/articles/PMC2763591/
[30] White-Koning M, Bertozzi-Salamon AI, Vignes M, Arnold C. Compliance to treatment of adolescents with cancer. Bull Cancer [serial on the Internet]. 2007 April; [cited 2013 September 30]; 94(4): 349-56. Available from http://www.jle.com/e-docs/00/04/2 E/8D/vers_alt/VersionPDF.pdf
[31] Lundman B, Strandberg C, Eisemann M, Gustafson Y, Brulin C. Psychometric properties of the swedish version of the resilience scale. Scand J Caring Sci 2007; 21(2): 229-37.
[32] Rodrigues FS, Polidori MM. Enfrentamento e Resiliência de Pacientes em Tratamento Quimioterápico e seus Familiares. Rev Bras Cancerologia [serial on the Internet]. 2012 August; [cited 2013 December 15]; 58(4): 619-627. Available from http://www.inca.gov.br/rbc/n_58/v04/pdf/07-artigo-enfrentamento-resiliencia-pacientes-tratamento-quimioterapico-familiares.pdf [33] Yunes MAM. Psicologia positiva e resiliência: o foco no indivíduo
e na família. Psicol Estud [serial on the Internet]. 2003 June; [cited 2013 December 15]; 8: 75-84. Available from http://www.scielo.br/ scielo.php?script=sci_arttext&pid=S1413-73722003000300010&ln g=en&tlng=pt. 10.1590/S1413-73722003000300010
[34] Tavares BC, Barreto FA, Lodetti M L, Silva DMGV, Lessmann JC. Resiliência de pessoas com Diabetes Mellitus. Texto contexto enferm. [serial on the Internet]. 2011 December; [cited 2013 December 12]; 20(4): 751-757. Available from http://www.scielo.b
r/scielo.php?script=sci_arttext&pid=S0104-07072011000400014&lng=en. http://dx.doi.org/10.1590/S0104-07072011000400014
Received: October 28, 2013 Revised: January 20, 2014 Accepted: January 20, 2014
© Faria et al.; Licensee Bentham Open.