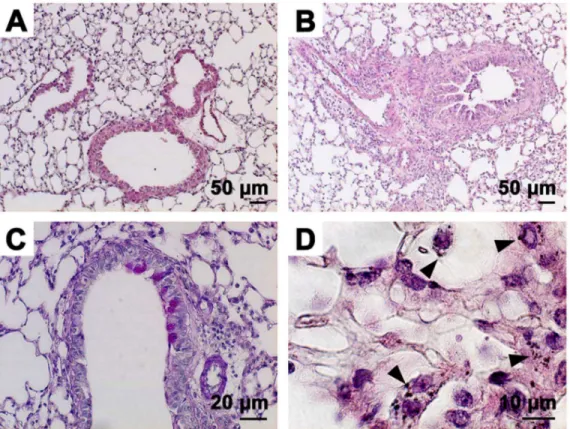
Allergic airway inflammation by nasal inoculation of particulate matter (PM2.5) in NC/Nga mice.
Texto
Imagem
Documentos relacionados
IgE-dependent cytokine generation by mast cells - Contrary to the inhibition of allergic airway inflammation observed when rmIL-10 was given by intra-nasal route, its
Inhibition of allergic airway inflammation in mice lacking nitric oxide synthase 2. Role of exhaled nitric oxide
This study has proven the efficacy of rupatadine in treating patients with persistent allergic rhinitis, reducing nasal symptoms, improving signs secondary to mucosal
In addition, we showed that Treg cells that accumulated in the airways of allergic mice also acquired activated phenotype, as revealed by increased expression of CTLA-4, GITR, and
We evaluated the effects of chronic allergic airway inflammation and of treadmill training (12 weeks) of low and moderate intensity on muscle fiber cross-sectional area and mRNA
Objective: To assess the prevalences of asthma, allergic rhinitis, and allergic rhinoconjunctivitis in adolescents in the city of Belo Horizonte, Brazil, in 2012 by administering
In the present study, source apportionment of the ambient summer and winter time particulate carbonaceous matter (PCM) in aerosol particles (PM 1 and PM 10 ) has been.. conducted
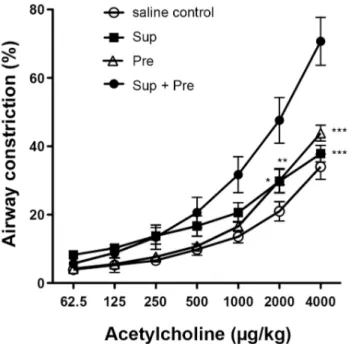
To determine whether skin-derived TSLP could cause airway hyper-responsiveness in RBP-jCKO mice, we used the OVA-induced model of allergic inflammation and challenged the lung