www.jped.com.br
ORIGINAL
ARTICLE
Hospitalizations
of
children
with
sickle
cell
disease
in
the
Brazilian
Unified
Health
System
in
the
state
of
Minas
Gerais
夽
,
夽夽
Ana
Paula
P.C.
Fernandes
a,
Fernanda
A.
Avendanha
a,
Marcos
B.
Viana
a,b,∗aUniversidadeFederalMinasGerais(UFMG),FaculdadedeMedicina,NúcleodeAc¸õesePesquisaemApoioDiagnóstico(Nupad),
BeloHorizonte,MG,Brazil
bUniversidadeFederalMinasGerais(UFMG),DepartamentodePediatria,BeloHorizonte,MG,Brazil
Received4April2016;accepted27July2016 Availableonline5December2016
KEYWORDS Sicklecelldisease; HospitalAdmitting Department; Epidemiology; Healthsystem; Newbornscreening; Brazil
Abstract
Objective: ToidentifyandcharacterizehospitaladmissionsandreadmissionsintheBrazilian
UnifiedPublicHealthSystem(SistemaÚnicodeSaúde[SUS])inchildrenwithsicklecelldisease diagnosedbytheMinasGeraisNewbornScreeningProgrambetween1999and2012.
Methods: Hospital Admission Authorizations with the D57 (International Classification of
Diseases-10)codeinthefieldsofprimaryorsecondarydiagnosiswereretrievedfromtheSUS Databank(1999---2012).Therewere2991hospitalizationsfor969children.
Results: 73.2%ofchildrenhadhemoglobinSS/S0-thalassemiaand48%weregirls.Themeanage
was4.3±3.2years,themeannumberofhospitalizations,3.1±3.3,andthehospitallengthof stay,5±3.9days.Hospitalreadmissionsoccurredfor16.7%ofchildren;10%ofadmissionswere associatedwithreadmissionwithin30daysafterdischarge;33%ofreadmissionsoccurredwithin sevendays post-discharge.Therewere41deaths, 95%ofwhichwerein-hospital.Secondary diagnoseswerenotrecordedin96%ofadmissions,makingitimpossibletoknowthereasonfor admission. In62%ofcases,hospitalizationsoccurredinthechild’scountyofresidence.The total numberofhospitalizationsofchildren under14withsicklecelldisease relativetothe totalofpediatrichospitalizationsincreasedfrom0.12%in1999to0.37%in2012.
夽
Pleasecitethisarticleas:FernandesAP,AvendanhaFA,VianaMB.HospitalizationsofchildrenwithsicklecelldiseaseintheBrazilian UnifiedHealthSysteminthestateofMinasGerais.JPediatr(RioJ).2017;93:287---93.
夽夽StudycarriedoutatUniversidadeFederaldeMinasGerais(UFMG),BeloHorizonte,MG,Brazil. ∗Correspondingauthor.
E-mail:vianamb@gmail.com(M.B.Viana).
http://dx.doi.org/10.1016/j.jped.2016.07.005
Conclusions: Ahighdemandforhospitalcareinchildrenwithsicklecelldiseasewasevident. Thenumberofhospitalizationsincreasedfrom1999to2012,suggestingthatthediseasehas becomemore‘‘visible.’’Knowledgeofthecharacteristicsoftheseadmissionscanhelpinthe planningofcareforthesechildrenintheSUS.
©2016SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/ 4.0/).
PALAVRAS-CHAVE Doenc¸afalciforme; Servic¸oHospitalarde Admissãode
Pacientes; Epidemiologia; SistemaÚnicode Saúde;
Triagemneonatal; Brasil
Internac¸õesdecrianc¸ascomdoenc¸afalciformenoSistemaÚnicodeSaúdenoEstado deMinasGerais
Resumo
Objetivo: Identificar e caracterizar as internac¸ões e reinternac¸ões hospitalares no Sistema
Únicode Saúde(SUS)decrianc¸ascomdoenc¸a falciforme,diagnosticadaspeloPrograma de TriagemNeonataldeMinasGeraisentre1999e2012.
Métodos: Extraíram-sedobancodedadosdoSUSasAutorizac¸õesdeInternac¸ãoHospitalarcom
ocódigoD57(Classificac¸ãoInternacionaldeDoenc¸as10)noscamposdediagnósticoprimárioou secundário(1999-2012).Identificaram-se969crianc¸as,totalizando2.991internac¸ões.
Resultados: 73,2%dascrianc¸astinhamhemoglobinaSS/S0-talassemiae48%erammeninas.A
médiadeidadefoide4,3±3,2anos,adonúmerodeinternac¸ões,3,1±3,3eadotempode permanência,5±3,9dias.Asreadmissõeshospitalaresocorreramem16,7%dascrianc¸as;10% dasinternac¸õesseassociaramàreadmissãoematé30diaspós-alta;33%dasreadmissões ocor-reramematé7diaspós-alta.Ocorreram41óbitos,95%emambientehospitalar.Odiagnóstico secundárionãofoiregistradoem96%dasinternac¸ões,impossibilitandoconheceromotivoda internac¸ão.Em62%doscasos,asinternac¸õesocorreramnomunicípioderesidênciadacrianc¸a. Ototaldeinternac¸õesdecrianc¸asaté14anoscomdoenc¸afalciformeemrelac¸ãoaototaldas internac¸õespediátricaspassoude0,12%em1999para0,37%em2012.
Conclusões: Constatou-seelevadademandaporcuidadoshospitalares,cujoaumentorelativo
entre1999e2012sugereincrementoda‘‘visibilidade’’dadoenc¸afalciforme.Oconhecimento dascaracterísticas dessasinternac¸ões podecontribuir noplanejamentodocuidado narede assistencialdoSUS.
©2016SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Este ´eumartigo OpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4. 0/).
Introduction
AccordingtotheWorldHealthOrganization(WHO) publica-tions,itisbelievedthat270millionpeopleworldwide(7%of theworld’spopulation)carrygenesthatdeterminethe pres-enceofabnormal hemoglobins(Hb).1---3 Sickle celldisease (SCD)is ageneticdisorderofgreatclinical and epidemio-logicalimportance,whosebasicetiologyistheinheritance ofthebeta S-globingene,eitherin thehomozygousstate orcombinedwithanothermutantallelethatpathologically interactswithhemoglobinS. InBrazil,thenumberof peo-plewithSCDisestimatedat25,000---30,000andthenumber ofnewbornsisestimatedat3500ayear.4Accordingtothe Neonatal Screening Program of the state of Minas Gerais (PTN-MG),the incidence ofthe sickle celltraitis 3.3% in atotalofapproximately250,000newbornsayear;theSCD rateisapproximately1:1400.5
The onsetof the disease’s clinical manifestations usu-allyoccursaftertheageof3monthsandlaststhroughout life, with a marked variation in severity between the affected individuals. They can be grouped according to twobasic pathophysiologicalevents: vasoconstrictionand chronichemolysis.6---8Clinicaleventssuchaspainfulcrises,9
bacterial infections, acute chest syndrome, and chronic complicationsleadtoseveralhospitaladmissions andhigh morbidity.Althoughmostofthehealthproblemsof individ-ualswithSCDcanbecaredforinprimarycareservices,some acuteevents,includingseverevaso-occlusivecrises,require repeatedhospitaladmissions.10
Therearefewnationalbibliographicalreferencesonthe epidemiologicalaspectsofhospitaladmissionsbySCD.The aimofthisstudywastodescribethehospitaladmissionsof childrenwithSCDthatwerescreenedbytheStateNeonatal ScreeningProgram,inhospitalunitsoftheBrazilianUnified HealthSystem(SUS),inMinasGerais,basedoninformation contained in the database of the SUS Hospital Informa-tionSystem(SIH).Associationsbetweenhospitaladmissions andclinicalandepidemiologicalvariableswerealso inves-tigated.
Methods
screenedforSCDbythePTN-MG,bornbetween01/01/1999 and12/31/2012,weresurveyedintheSIH-SUS.
The PMN-MG database contains data on all the 853 municipalitiesofMinasGeraisenrolledintheprogram.The coverageisapproximately92%ofnewbornsinthestate;the restarescreenedbyprivatelaboratories.Between1999and 2012, thePTN-MG screened 3,590,315 children.Of these, 2560werepositiveforSCDandreferredforfollow-upatthe BloodCentersoftheHemominasFoundation.
The SIH-SUSis managed by the Ministry of Health and processedbyDATASUS--- theDepartmentofInformaticsof SUS. SUS hospital units throughout Brazil send the infor-mationonhospitalizations throughtheHospital Admission Authorization (AIH). These data (approximately 50 varia-bles) are processed by DATASUS, generating the financial creditsrelatedtotheprovidedservices.
Datafromhospitalizationsrelatedtothemorbiditygroup codeD57 (Sickle cellDisorders) of the International Code of Diseases, version 10 (ICD-10) recorded in the primary and/or secondary diagnostic fields of theAIH form in the studyperiod,wereobtainedafterformalizedrequesttothe BrazilianMinistryofHealth,guaranteeingthe confidential-ityandanonymityofthepatients.Toidentifythechildren screenedintheSIH,datasuchasname,dateofbirth,city ofresidence,andmother’snamewerealsoincludedinthe PTN-MGdatabase.
AllchildrenwithcodesD57.0(sicklecellanemiawith cri-sis),D57.1(sicklecelldiseasewithoutcrisis),D57.2(double heterozygousdisorders)orD57.8(othersicklecelldisorders) intheprimaryor secondarydiagnosis fieldwereincluded. Patients witha birth date outside the study period were excludedfromtheSIHdatabase,aswellasthosethatwere notincludedinthePTN-MGdatabasewithadiagnosisofSCD atthescreeningandthosewiththecodeD57.3(sicklecell trait).Datarelatedtogenotypeanddeathswereextracted fromthePTN-MGdatabase.
Theanalyzedvariablesweregender,age,hospitallength ofstay,genotype,numberofhospitalizations,readmissions, placeofresidence,placeofhospitalization,monthof hospi-talization,andhospitalcosts.Associationbetweennominal variableswastestedwiththechi-squaredorFisher’sexact test. The comparison between continuous variables with normaldistributionwasperformedthroughanalysisof vari-anceandtheposthocBonferronitest,whenmorethantwo groupswereinvolved.Variableswithnon-Gaussian distribu-tionwere comparedusing theKruskal---Wallistest. For all thetests,analphaerrorprobability≤0.05wasconsidered. ThestudywasapprovedbytheEthicsCommitteeof Uni-versidadeFederal deMinasGeraisandby theDepartment ofPediatricsofUFMG,withouttheneedtosignaninformed consent.TheMinistryofHealthauthorized,afterdue justi-fication,theprovisionofdatabySIH-DATASUS.
Results
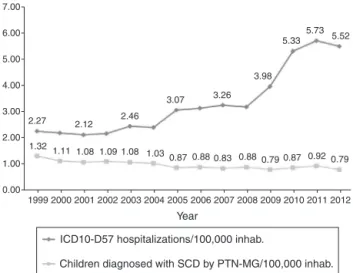
During the study period, 9020 hospitalizations of adults and children with ICD10-D57 (Sickle cell Disorders) were processedbyDATASUSastheprimary(n=8779)orsecondary (n=241)diagnosis.In2012,thehospitalizationsaccounted for0.4%ofalladmissionsthroughSUS,2.4timesthe percent-ageverifiedin1999(0.17%),excludingobstetricadmissions.
7.00
6.00
5.00
4.00
3.00
2.27 2.12 2.46
3.07 3.26 3.98
5.33 5.73
5.52
1.32
199920002001200220032004 Year
20052006200720082009201020112012 1.11 1.08 1.08 1.03
0.87 0.88 0.83 0.88 0.79 0.87 0.92 0.79 1.09
2.00
1.00
0.00
ICD10-D57 hospitalizations/100,000 inhab.
Children diagnosed with SCD by PTN-MG/100,000 inhab.
Figure1 Rateofscreenedchildrenwith sicklecelldisease andrateofICD10-D57hospitalizations(sicklecelldisorders)as primaryorsecondarydiagnosisper100,000residentsayearin MinasGerais,from1999to2012.
Fig.1showstherateofchildrenscreenedwithSCDandthe hospitalizationrateof patients withICD10-D57 registryin AIHsper100,000residentsinMinasGerais. Thesame 2.4-foldincreaseinthehospitalizationrateisobserved.
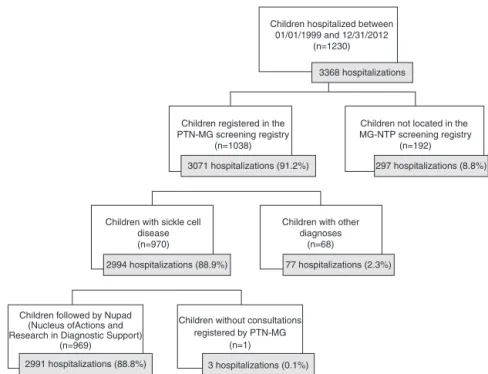
Oftheaforementioned numberof9020hospital admis-sions,3368wereselected,relatedtochildrenbornbetween 01/01/1999and12/31/2012.Fig.2illustrateshowthe num-berof2991hospitalizationswasobtained,correspondingto 969childrenwhocomprisedthestudysample.
Table1showstheclinicalanddemographic characteris-ticsof969childrenand2991hospitalizations.Mostchildren hadHbSSand anevenhigher percentagecorresponded to hospitalizationsof children with HbSS. Medianage at the hospitaladmissionswas4years.Themediannumberof hos-pitalizationsperpatientwastwo(interquartilerange:1---4). Themedianlengthofhospitalstaywasfourdays.CodeD57.0 (sicklecellanemiawithcrisis)wastheonemostfrequently recordedintheAIHs.
Thepercentageofhospitalizationsamongchildrenwith SCD aged 0---14 years in relation to the total number of pediatrichospitalizationsintheSUSinthesameagegroup (SIH-SUS data) increased approximately three-fold in the studyperiod,from0.12%in1999to0.37%in2012.
WhencomparinghospitaladmissionsforSCDwith hospi-taladmissions for otherchronic diseases inthe agegroup 0---14 years (data from the SIH-SUS), it is observed that thefrequencyofhospitalizationsforSCDduringtheperiod increased three-fold, being similar to the frequency of admissionsforcerebralpalsyanddiabetesmellitusin2012. The frequency of hospitalizations per patient is shown in Table 2. Note that 26.9% of the patients with four or morehospitalizationswereresponsiblefor62.6%ofhospital admissions.The2---4and5---9yeargroupsshowednotonlya highernumbersofhospitalizations,butalsoahighermean ofhospitalizationsperpatient.
Children hospitalized between 01/01/1999 and 12/31/2012
(n=1230)
Children registered in the PTN-MG screening registry
(n=1038)
3368 hospitalizations
3071 hospitalizations (91.2%)
2994 hospitalizations (88.9%)
2991 hospitalizations (88.8%) Children followed by Nupad
(Nucleus ofActions and Research in Diagnostic Support)
(n=969)
Children without consultations registered by PTN-MG
(n=1)
77 hospitalizations (2.3%)
3 hospitalizations (0.1%) Children with sickle cell
disease (n=970)
Children with other diagnoses
(n=68)
297 hospitalizations (8.8%) Children not located in the MG-NTP screening registry
(n=192)
Figure2 Flowchartofthestudiedsampleselectionbasedonthe3368SUShospitaladmissionswithICD10-D57asthemainor secondarydiagnosis,from1999to2012,regardingchildrenbornfromJanuary1999toDecember2012.
Table1 CharacteristicsofSUShospitalizationswithcodeD57,fromJanuary1999toDecember2012,ofthescreenedchildren withsicklecelldisease,bornbetweenJanuary1999andDecember2012.
Hospitalizations (n=2991)
n% Patients
(n=969)
n%
Gender
Female 1412 47.2% 465 48.0%
Male 1579 52.8% 504 52.0%
Genotype
HbSSorHbSß0tal 2438 81.5% 709 73.2%
HbSC 484 16.2% 234 24.1%
HbSß+tala 66 2.2% 25 2.6%
HbSDPunjaba 3 0.1% 1 0.1%
DiagnosisofICD-10D57b
D57.0 2296 76.8% ---
---D57.1 572 19.1%
D57.2 4 0.1% ---
---D57.3c 4 0.1% ---
---D57.8 115 3.8% ---
---HbSS,homozygousinheritanceforHbS;HbSDPunjab,associationbetweenHbSandthehemoglobinvariantsD-Punjab;HbSC,association
betweenHbSandC.
aThenumberofchildrenwithHbSß+talandHbSDPunjabmaybeoverestimated,asmolecularbiologymethodsfordiagnostic
confir-mationwereintroducedinthePTN-MGonlyin2010.
b D57.0,sicklecellanemiawithcrisis;D57.1,sicklecellanemiawithoutcrisis;D57.2,doubleheterozygoussicklecelldisorders;D57.3,
sicklecelltrait;D57.8,othersicklecelldisorders.
c CodeD57.3(sicklecelltrait)waserroneouslyreportedintheSIH-SUS,asitreferstochildrenwithadefinitediagnosisofsicklecell
anemiaatthescreeningtestoftheNeonatalScreeningProgramofMinasGerais.
13.3±9.4 days, with one-third of readmissions occurring withinsevendaysafterhospitaldischarge.Theyweremore frequentinchildrenwithSS/S0tal(p<0.05).
The mean length of hospital stay was 5.0±3.92 days, ranging from 0 to 63 days. This mean length of hospital stay for pediatric hospitalizations through SUS for other
Table2 Distributionofthefrequencyofhospitalizationperpatient,fromJanuary1999toDecember2012.
Frequency Patients % Hospitalizations %
1 408 42.1 408 13.6
2 188 19.4 376 12.6
3 112 11.6 336 11.2
4---9 211 21.8 1170 39.1
10---16 41 4.2 519 17.4
>16 9 0.9 182 6.1
Total 969 100.0 2991 100.0
withpatientsaged≥10yearsshowing ahigherproportion of hospitalizations lastingmorethan fivedays (p=0.035). Thedistributionofhospitalizationsthroughouttheyearwas relativelyuniform,withnoseasonalityobserved.
The amounts spent onhospital care, recorded by SIH-SUSin US dollars, wererecorded in 2444AIHs (81.7%);in the remaining 561, the data was missing.The mean cost perhospitalization, consideringthe sevenyears forwhich thedata wereavailable, was174dollars. Considering the periodsof2005---2007and2010---2012,themeanannualcost ofhospitalizationwasslightlyhigherinthesecondstudied period.
According to the PTN-MG, 41 deaths occurred among the 969 children selected for the study (4.2%), most of them (n=34)with theHb SS/Sß0tal profile. In 95% of the cases(n=39),the deathoccurred inthe hospital environ-ment,accordingtoacopyofthedeathcertificateobtained throughthePTN-MG.Infection,acutechestsyndrome,and splenicsequestrationwerethemaincausesofdeath,as dis-closedbythedeathcertificates.However,onlysevendeaths wererecordedintheAIHswiththeICD10-D57 codein the primary andsecondary diagnostic fields.In one case, the dateofhospitaldischargecoincidedwiththedateofdeath recorded bythe PTN-MG, despite thefact thatthe death wasnotrecordedintheAIH.Theother31deathsrecorded ashospitaldeathsbythePTN-MGmayhaveoccurredduring hospitalizations without the registrationof the ICD10-D57 code,orinemergencycareunitsnotrecognizedassuchby PTN-MGrecords.
In96%oftheAIHstherewasnorecordofanother diag-nosisassociatedtotheD57code,whichmadeitimpossible tostudythecomorbiditiespresent inthe hospitalizations. Infections were recorded in 90 of the 118 AIHsthat con-tained any other diagnosis rather than the D57 group registry.
Hospitalizationsoccurredin149municipalitiesofMinas Gerais.Thehospitalizedchildrenlivedin278municipalities, threeof whichwere locatedin other states ---Verdejante (PE),TrêsRios (RJ),andNovoHorizonte(BA). The munic-ipality where the care was provided coincided with the municipality of residence in 62.1% of the cases. The city withthehighestnumberofhospitalizations(43.5%)wasthe state capital, Belo Horizonte,but 54%of the hospitalized patientsdidnotliveinthecapitalandofthe20%whodid, allreceivedcareinthatcity.Themajority(97%)ofpatients living in Contagem, Ribeirão das Neves, and Santa Luzia, municipalities located in the metropolitan region, were treatedinBeloHorizonte.TabulardatarelatedtoSCD com-prising theprevalence, the rateof resident children, and
thehospitalizationratein each ofthe 28RegionalHealth UnitsofMinasGeraiscanberequestedfromtheauthors.
Comparison
of
hospitalizations
up
to
4
years
of
life
of
287
children
born
between
1999
and
2001
(
n
=
129)
with
those
born
between
2006
and
2008
(
n
=
158)
Atotal of 696 hospitalizations found in the SIH-SUSwere selectedforthispartofthestudy:247hospitalizationsupto 4yearsoflifewererecordedforthechildrenborninthefirst period,and449,amongthoseborninthesecondperiod.The 129childrenbornintheearlierperioddidnotdiffer signifi-cantlyregardinggenderortypeofhemoglobinopathyfrom the158 children born in themore recent period(p=0.35 andp=0.24,respectively).
The proportion between the number of children who had at least one hospitalization and the number of chil-dren with SCD screened by the PMN-MTN in each of the periods(623inthe firstand509inthe second)was0.207 and0.310,respectively, resultingin adifferenceof 0.103 (95% CI: 0.032---0.174, p<0.0001). The difference is even greaterwhentheproportionsbetweenthenumberof hospi-talizationsandthenumberofchildrenscreenedineachof theperiodsarecalculated:0.396and0.882,resultingina differenceof0.486(95%CI:0.438---0.533;p<1×10−9).
The meannumberof hospitaladmissions perchild was higherinthesecondperiodwhencomparedtothefirst(2.84 and1.91,respectively,p=0.001).Thehospitalization dura-tion,however,wassimilarinbothgroups(4.57vs.4.64days, respectively,p=0.85).
Accordingtotherecordsof696AIHs,therewerethree deaths,oneofachildbornintheperiodfrom1999to2001 andtwoamongthosebornfrom2006to2008.However,in 88.2%ofAIHsprocessedintheearlierperiod,therewasno positiveor negativedeathrecord(the correspondingfield wasblank),whileallthemorerecentlyprocessedAIHs con-tainedthisinformation.
Discussion
thesame,reaching5.5hospitalizationsper100,000 inhabi-tantsinMG.Consideringtheagegroupfrom0to14years, the frequency of hospital admissions for SCD was similar tothatfordiabetesmellitusandcerebralpalsy,especially amongthechronicconditionsthatmostfrequentlyresultin hospitalizationsatthepediatricagerange.11
Thisincreasebecamemoreevidentwhentheinitialand finalperiodsofthepresentstudywerecompared.The num-berofchildrenwithatleastonehospitaladmissionand,still moreevidently,thetotalnumberofadmissionsweremuch higherin the mostrecent periodin relation tothe initial one.Additionally,thefrequencyofadmissionsperchildwas alsohigherinrecentyears.
This absolute and relative increase could be simply explainedbytheincreaseinthefrequencyofhospital admis-sions for SCD to the detriment of other causes, resulting fromchangesinSCDhospitalcareguidelinesbetween1999 and2012,whichareunknowntotheauthors.Thatdoesnot seemthemostplausiblereason,though.Itisbelievedthat thebroaderknowledge ofthedisease,both bythe family members and by the health professionals, resulting from theinitiationofthestatescreeningprograminMarch1998, accounted for the more frequent registration of the D57 group codes in the AIHs. Asimilar phenomenon has been recentlyreportedinthestateofMaranhão.12
The discrepancy caused by the‘‘invisibility’’ of SCDis also evident in a study that found the rate of hospital-ization for SCD is much higher in São Paulo and Rio de Janeirothan inBahia,wherethe incidenceofthedisease isapproximatelyfiveandtwo-foldhigherthanintheother twostates,respectively.3Anotherindicationofthedisease’s ‘‘invisibility’’is thefindingthathalf ofthe193 children’s deathcertificatesrecordedbythePTN-MGdidnotinclude theterm‘‘sicklecell.’’13
TheprevalenceoftheSSgenotypeinhospitaladmissions, asinotherstudies,isexplainedbythemoresevereclinical courseofthedisease.14,15Themostfrequentcauseof hospi-talization,asobservedinotherstudies,3,16---19wasthepainful crisis,ascodeD57.0(sicklecellanemiawithcrisis),which intheabsenceofadditionaldataintheAIHswasinterpreted bytheauthorsasapainfulcrisisthatrequired hospitaliza-tion.The mean length ofstay offive dayscoincides with thatofotherstudies,whichobservedarangeof4---11days forhospitalizationsduetovaso-occlusivecrises.19---21
The regional distribution of hospitalizations followed whatwasexpectedofthe hospitalnetworkconcentration in MG at regional poles. In more than half of the hospi-talizations in Belo Horizonte, the children lived in other municipalities,mainlyinthemetropolitanregion.Similarly, buttoalesserextent,thesameoccurredinJuizdeFora, Uberaba,andUberlândia.
Themeancostofhospitalizationin2012disclosedbythe presentstudywasUS$186.00,wellbelowthemeancostof US$344.6dollars11forpediatrichospitalizationsingeneral, consistentwiththeshorterhospitallengthofstay, charac-teristicofthemostfrequentcauseofhospitaladmission,the painfulcrisis.InastudycarriedoutinNigeria,themeancost ofhospitalizationwasUS$133dollars22and,asexpected,it waslowerthanthatoftheUnitedStates.23
Thelimitationsfoundinthepresentstudyareassociated tothe qualityof the datain the AIH recordsor, possibly, tothetransferofdatarecordedbythehealthprofessionals
to the system database. Record failures, characterized primarilybytypingerrors,misinformation,ormissingdata, representthemostsignificant difficultiesforsearches car-riedoutinlargepublicdatabases.Anextensive‘‘database scanning’’ was required, compiling and cross-referencing informationtoreduceerrorsandapproximatethecollected data totheactual data. Nonetheless,thebroad epidemi-ological studies onSCD basedon governmentaldatabases should be considered valid as sources of information, as after the management of these systems by diverse professionals,withdifferentinterests,itwillbepossibleto identifyfailuresandimplementimprovements.
Simpleinterventionsandbasic healthcare providedby morefrequentfollow-upatthebasichealthunit,inaddition tothatperformedinbloodcentersandothersecondarycare units,promptrecognitionofthewarningsignsforpotentially severesituations,andimmediatesearchformedical assis-tancemaydetermine,overtime,alowerneedforhospital admissions.
Inthissense, theeducationofthe patientandhis/her family, as well as of the health professionals, focusing on empowering of the knowledge about the disease and co-responsibilityregardingthecareandtreatmentare chal-lengestobeovercome.Inrelationtothecare network,it isnecessarytotrainthemultiprofessionalteamandinclude theinformationaboutthediseaseinthefilesoftheprimary careinformationsystem,toexpandandimprovetheinitial careprovidedbytheemergencyservicestoindividualswith SCD,toincludethediseaseintheparametersofrisk regu-lationandclassification,aswellastoinstituteintegralcare ofindividualswithSCDwithinthescopeofSUS.
It is expected that epidemiological research, not only in SCD, but also regarding other prevalent conditions or with a more severe evolution in the black popula-tion, be encouraged and facilitated in the institutional databases,respectingtheethicalrequirements of secrecy andanonymity.
Theauthorsexpectthatthecontributionstothe knowl-edge on hospital admissions of children with sickle cell disease in Minas Gerais can support the planning and implementationof actions thatwill leadtothe reduction of morbimortality determined by the disease and to the improvementofthequalityoflifeofindividualswithSCD.
Funding
Conselho Nacional de Desenvolvimento Científico e Tec-nológico (CNPq), Núcleo de Ac¸ões e Pesquisa em Apoio Diagnóstico(Nupad,FaculdadedeMedicinadaUFMG).
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
References
1.SimõesBP,PieroniF,BarrosG,MachadoCL,Canc¸adoRD,Salvino MA,etal.Consensobrasileiroemtransplantedecélulas-tronco hematopoéticas:comitêdehemoglobinopatias.RevBras Hema-tolHemoter.2010;32:S46---53.
2.GomesL,CaldeiraA.Avaliac¸ão daqualidadedaassistênciaà crianc¸acom doenc¸afalciformenaatenc¸ãoprimárianonorte deMinasGerais,Brasil.MontesClaros:UniversidadeEstadual deMontesClaros;2010.
3.Loureiro MM, Rozenfeld S. Epidemiology of sickle cell dis-ease hospital admissions in Brazil. Rev Saude Publica. 2005;39:943---9.
4.Canc¸adoRD,JesusJA.Adoenc¸afalciformenoBrasil.RevBras HematolHemoter.2007;29:204---6.
5.FernandesAP,JanuárioJN,CangussuCB,MacedoDL,VianaMB. Mortalityofchildrenwithsicklecelldisease:apopulationstudy. JPediatr(RioJ).2010;86:279---84.
6.ReedW,VichinskyEP.Newconsiderationsinthetreatmentof sicklecelldisease.AnnuRevMed.1998;49:461---74.
7.InatiA,ChabtiniL,MounayarM,TaherA.Current understand-ing in the management of sickle cell disease. Hemoglobin. 2009;33:S107---15.
8.FigueiredoMS.Fatoresmoduladoresdagravidadedaevoluc¸ão clínica da anemia falciforme. Rev Bras Hematol Hemoter. 2007;29:215---7.
9.BallasSK,LusardiM.Hospitalreadmissionforadultacutesickle cellpainfulepisodes:frequency,etiology,andprognostic signif-icance.AmJHematol.2005;79:17---25.
10.AisikuIP, Smith WR,McClishDK,Levenson JL, PenberthyLT, RoseffSD, et al. Comparisonsof high versus lowemergency department utilizes in sickle cell disease. Ann Emerg Med. 2009;53:587---93.
11.DATASUS. Informac¸ões de saúde. Available from: http:// tabnet.datasus.gov.br/cgi/deftohtm.exe?sih/cnv/sxmg.def [cited23.10.15].
12.LimaAR,RibeiroVS,NicolauDI.Trendsinmortalityand hospi-taladmissionsofsicklecelldiseasepatientsbeforeandafter thenewbornscreeningprograminMaranhão,Brazil.RevBras HematolHemoter.2015;37:12---6.
13.Sabarense AP, Lima GO, Silva LM, Viana MB. Characteriza-tionofmortalityinchildrenwithsicklecelldiseasediagnosed through the Newborn Screening Program. J Pediatr (Rio J). 2015;91:242---7.
14.DayTG,TheinSL,DrasarE,DickMC,HeightSE,O’DriscollS, etal.Changingpatternofhospitaladmissionsofchildrenwith sickle celldisease over thelast50years.JPediatr Hematol Oncol.2011;33:491---5.
15.Akar NA, Adekile A. Ten-year review of hospital admissions amongchildrenwithsickle celldisease inKuwait.MedPrinc Pract.2008;17:404---8.
16.Guimarães TM, Miranda WL, Tavares MM. O cotidiano das famíliasdecrianc¸aseadolescentesportadoresdeanemia fal-ciforme.RevBrasHematolHemoter.2009;31:9---14.
17.Felix AA, Souza HM, Ribeiro SB. Aspectos epidemiológicos e sociais da doenc¸a falciforme. Rev Bras Hematol Hemoter. 2010;32:203---8.
18.BallasS,LieffS,BenjaminL,DampierC,HeeneyM,HoppeC, etal.Definitionsofthephenotypicmanifestationsofsicklecell disease.AmJHematol.2010;85:6---13.
19.Brozovi´cM,DaviesSC,BrownellAI.Acuteadmissionsofpatients withsicklecelldiseasewholiveinBritain.BrMedJ(ClinRes Ed).1987;294:1206---8.
20.Yang Y-M, Shah AK, Watson M, Mankad VN. Comparison of costs to the health sector of comprehensive and episodic healthcareforsicklecelldiseasepatients.PublicHealthRep. 1995;110:80---6.
21.PanepintoJA,BrousseauDC,HilleryCA,ScottJP.Variationin hospitalizations and hospital lengthof stay in children with vaso-occlusivecrisesinsicklecelldisease.PediatrBloodCancer. 2005;44:182---6.
22.Adegoke SA, Abioye-Kuteyi EA, Orji EO. The rate and cost of hospitalisation in children with sickle cell anaemia and its implications in a developing economy. Afr Health Sci. 2014;14:475---80.