www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
Hyperinsulinemia
and
hyperglycemia:
risk
factors
for
recurrence
of
benign
paroxysmal
positional
vertigo
夽
,
夽夽
Guilherme
Webster
a,∗,
Patrícia
Maria
Sens
a,
Márcio
Cavalcante
Salmito
b,
José
Diogo
Rijo
Cavalcante
a,
Paula
Regina
Bonifácio
dos
Santos
a,
Ana
Lívia
Muniz
da
Silva
a,
Érica
Carla
Figueiredo
de
Souza
aaHospitaldoServidorPúblicoMunicipaldeSãoPaulo(HSPM),SãoPaulo,SP,Brazil
bEscolaPaulistadeMedicina,UniversidadeFederaldeSãoPaulo(EPM/UNIFESP),SãoPaulo,SP,Brazil
Received13August2014;accepted14September2014 Availableonline9June2015
KEYWORDS
Vertigo;
Glucosemetabolism disorders;
Carbohydrate metabolism; Dizziness
Abstract
Introduction:Changesincarbohydratemetabolismmayleadtorecurrenceofbenign paroxys-malpositionalvertigo.
Objective: Toevaluatethe influenceofthe disturbanceofcarbohydratemetabolisminthe recurrenceofidiopathicBPPV.
Methods:Alongitudinalprospectivestudyofacohort,with41monthsfollow-up.Weanalyzed theresultsof72glucose---insulincurvesinpatientswithrecurrenceofBPPV.Thecurveswere classifiedintointolerance,hyperinsulinemia,hyperglycemiaandnormal.
Results:The RRfor hyperinsulinismwas 4.66andp=0.0015.Existinghyperglycemiashowed anRR=2.47,withp=0.0123.GlucoseintolerancehadaRRof0.63,withp=0.096.Whenthe examinationwaswithinnormallimits,theresultwasRR=0.2225andp=0.030.
Discussion: Metabolicchangescancausedizzinessandvertigoandareverycommoninpeople whohavecochleovestibulardisorders.However,fewstudiesdiscusstherelationshipbetween idiopathicBPPVandalterationsincarbohydratemetabolism.Inthepresentstudy,wefoundthat bothhyperglycemiaandhyperinsulinemiaareriskfactorsfortherecurrenceofBPPV,whereasa normaltestwasconsideredaprotectivefactor;allthesewerestatisticallysignificant.Glucose intolerancethatwasalreadypresentwasnotstatisticallysignificantinthegroupevaluated.
夽 Pleasecitethisarticleas:WebsterG,SensPM,SalmitoMC,CavalcanteJD,dosSantosPR,daSilvaAL,etal.Hyperinsulinemiaand
hyperglycemia:riskfactorsforrecurrenceofbenignparoxysmalpositionalvertigo.BrazJOtorhinolaryngol.2015;81:347---51.
夽夽Institution:HospitaldoServidorPúblicoMunicipaldeSãoPaulo,SãoPaulo,SP,Brazil.
∗Correspondingauthor.
E-mail:guilhermewebster@uol.com(G.Webster).
http://dx.doi.org/10.1016/j.bjorl.2014.09.008
Conclusion:Hyperinsulinemia andhyperglycemiaareriskfactorsfor therecurrenceof idio-pathicBPPVandanormalexamisconsideredaprotectivefactor.
© 2015Associac¸ãoBrasileira de Otorrinolaringologiae CirurgiaCérvico-Facial. Publishedby ElsevierEditoraLtda.Allrightsreserved.
PALAVRAS-CHAVE
Vertigem; Transtornosdo metabolismode glucose; Metabolismodos carboidratos; Tontura
Hiperinsulinismoehiperglicemia:fatoresderiscopararecorrênciadevertigem
posturalparoxísticabenigna
Resumo
Introduc¸ão:Asalterac¸õesdometabolismodocarboidratopodemlevararecorrênciade ver-tigemposicionalparoxísticabenigna.
Objetivo:AvaliarainfluênciadosdistúrbiosdocarboidratonarecorrênciadaVPPBidiopática. Método: Estudolongitudinal,dotipocoorte,prospectivo,com41mesesdeacompanhamento. Analisaram-se72resultadosdecurvasglicoinsulinêmicasempacientesportadoresde recorrên-ciadeVPPB.Ascurvasforamclassificadasemintolerância,hiperinsulinemia,hiperglicemiae normal.
Resultados: Ohiperinsulinismo teve RR=4,66 e p=0,0015.A hiperglicemia apresentou um RR=2,47ep=0,0123.NaintolerânciaaglicoseoRR=0,63ep=0,096.Noexame normal,o RR=0,2225ep=0,030.
Discussão: Asalterac¸õesmetabólicaspodemcausartonturaevertigemesãomuitofrequentes napopulac¸ãoqueapresenta distúrbios cocleovestibulares.Contudo,poucostrabalhos falam sobrearelac¸ãoentreaVPPBidiopáticaeasalterac¸õesnoscarboidratos.Nopresenteestudo, verificou-se quetanto a hiperglicemia,quanto o hiperinsulinismosão fatoresde risco para recorrênciadeVPPB,aopassoqueoexamenormalfoiconsideradofatorprotetor,todosestes estatisticamentesignificantes.Jáaintolerânciaàglicosenãotevesignificânciaestatísticano grupoavaliado.
Conclusão:Ohiperinsulinismoeahiperglicemiasecomportamcomofatoresderiscoparaa recorrênciadeVPPBidiopática,assimcomooexamenormalcomoumfatorprotetor. ©2015Associac¸ãoBrasileira deOtorrinolaringologiaeCirurgiaCérvico-Facial.Publicadopor ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
Benignpostural(orpositional)paroxysmalvertigo(BPPV)is themostcommoncauseofdizzinessintheadultpopulation, andisclassifiedasaperipheralvestibularsyndrome.1---3BPPV predominates in females and in those aged greater than 50---60years.Inaddition,approximately30%oftheelderly agedover70yearswillexperienceat leastoneepisodeof BPPVintheirlives.4,5
Inmostcases,thepatientsuffersfromidiopathicBPPV. InsecondaryBPPV, somecauseshavebeenfound,suchas: traumatic brain injury, post-operative ear surgery, verte-brobasilarinsufficiency,vestibularneuronitisandMénière’s disease.6 However, few studies have related metabolic changes with BPPV, or even identified such changes as a causeofsecondaryBPPV.7
Numerous metabolic disorders can affect the cochleovestibular apparatus.8---12 Changes in carbohy-drate metabolism, more precisely in glucosemetabolism, have been associated with frequent causes of inner ear disorders.8---12
In carbohydrate disorders, especially those affecting glucose,someauthorsproposethat,inpatientswith chroni-callyhyperglycemicdiabetesmellitus,thehistopathological
changesofmicroangiopathyandperipheralneuropathyare present.11,13Consideringthattheinnerearreceives vascu-larization through terminal branches, such changesmight compromisevestibularfunction,due toadecreasedblood supplytothisorgan.
Thepost-mortemstudyoftemporalbonesperformedby Yodaetal.10foundthatpatientswithtype1diabetes mel-litus exhibit a muchhigher prevalence of otocone debris comingfromtheutricle,comparedtohealthypatients.In addition,theseauthorsfoundthattheprevalenceof migra-tionofsuchdebrisalsowasincreased,inproportiontothe years of illness. Thus, thereis a greater chance of BPPV in patients with type 1 diabetes mellitus. Cohen et al.14 observeda20%prevalenceofdiabetesmellitusinpatients withBPPVagedbetween65and74years,anda43% preva-lenceinpeopleover75years.
Intheliterature,recurrenceofBPPVvariesbetween20% and30%.1,15Severalfactorshavebeenlinkedtothe devel-opmentofrecurrence,includingage,gender, andetiology ofBPPV.1,15 However,itstillremains uncertainwhetheror notthereisacorrelationwithmetabolicdisorders.
Methods
This study wasapproved by the Ethics Committeeof the hospitalwhereitwasconducted,accordingtoCAEEprotocol number06181512.2.0000.5442.
Thisisalongitudinalcohortstudy,whichevaluated medi-calrecordsofpatientswithanobjectivediagnosisofbenign paroxysmalpositionalvertigoestablishedbythe otoneurol-ogyoutpatientclinicoftheOtolaryngologyDepartmentofa tertiaryhospitalduringtheperiodfromDecember2009to May 2013.This diagnosis wasreviewed morethan oncein thosecaseswhererecurrenceofthediseaseoccurred.
Patients with objective idiopathic benign paroxysmal positionalvertigomonitoredintheotoneurologyoutpatient clinic until their discharge (which occurred only after an asymptomaticperiodof6months),andwhosubmittedtoa requested3-hglucosetolerancetestwereincluded.
Patients with subjective benign paroxysmal positional vertigoorwithothercausesofdizzinessnotassociatedwith BPPV, as well as patients who discontinued or were lost to follow-up before discharge, those failing to make the required tests, or patients with a previous diagnosis and treatmentforBPPVwereexcluded.Patientsdiagnosedwith secondaryBPPVofundeterminedetiology,suchastraumatic braininjury,Ménière’sdisease,vestibularneuronitis, post-operative of earsurgery, andvertebrobasilarinsufficiency werealsoexcluded.
AllclinicalrecordsofpatientswithadiagnosisofBPPV registered at the otoneurology outpatient clinic, Depart-mentofOtolaryngology,weresurveyed.Inthesecharts,we collectedtherelevantdataatdiagnosis.
Asurveyof therecordsofallpatientswhohada diag-nosis of BPPV registered at the otoneurology outpatient clinic,OtolaryngologyDepartment,wasconducted.Inthese clinical records, all data were obtained at the date of diagnosis.
Recurrence of thedisease wasevaluatedboth qualita-tivelyandquantitatively;‘‘recurrence’’wasdefinedasthat clinicalpictureinwhichdisappearanceofvertigoand posi-tional nystagmus occurred after repositioning maneuvers (RM), with assessment by Dix-Hallpike maneuver and roll test,butwithreturnofthesesignsandsymptomsverified byan ENTphysicianwithinsix monthsoffollow-up. After RM repetition, these patients were again asymptomatic. Finally,patientswhosenystagmusandvertigodidnot disap-pearwhenRMwerecarriedoutunderthesupervisionofan otolaryngologistwereclassified ashaving persistentBPPV. Itmustbeemphasizedthattherecurrencesofepisodesof BPPVwere evaluatedthrough anamnesis andalso by Dix-Hallpikemaneuverandrolltest.
The results of the glycemic curve test were analyzed and classified according toAmericanDiabetes Association (ADA)criteriapublishedin2013,andtheinterpretationof theinsulinemiccurvewasbasedonthosecriteriaproposed byKraft(1975).14,15Therefore,ourpatientswereclassified intofourgroups, accordingtotheresultsoftheir glucose-insulin curves:patients with a normal test, patients with impaired glucose tolerance (who, according to ADA, are calledpre-diabeticpatients),patientswithhyperinsulinism, andpatients withhyperglycemia (who, accordingto ADA, arecalleddiabetics);inthesepatients,therelationshipwith therecurrenceofBPPVwasevaluated.
Normal test Normal test
Normal test
Abnormal test Abnormal test
Abnormal test
Recurrent
Recurrent No recurrence
No recurrence Normal glucose-insulin curve
0.00% 10.00% 20.00% 30.00% 40.00% 50.00%
23.61% 4.17%
31.94% 40.28%
Figure 1 Distribution of patients with BPPV recurrence, regardingglucose---insulintestswithinnormallimits.
The Chi-squared test was used to assess quantita-tively the relationship between changes in carbohydrate metabolismandrateof recurrence.The statistical signifi-cancelevelwassetatp=0.05.
Results
Inthisstudy,103 medicalrecordsof patientswithbenign paroxysmalpositionalvertigoduringtheperiodfrom Decem-ber 2009 to May 31, 2013 were evaluated. Of these, 31 patientswereexcludedfromthestudy(11patientsfor hav-ingsubjectiveBPPV;5patientswhosemedicalrecordswere notfoundinthehospitalmedicalfile;7patientsfornot hav-ingperformedtherequiredtestsand/orfordiscontinuation ofclinicalfollow-up;and8patientsfornotbeingconsidered asidiopathiccases).Thus,thefinalnumberofcaseswas72 patients,whosesamplewasdividedasfollows:
• Witha normalresultin glucose---insulintests (Fig.1),a relativerisk(RR)of0.2225wasfound,withp=0.03054. • With a result of impaired glucose tolerance in
glucose---insulintests(Fig.2),RR=0.6315,p=0.096. • Witharesultofhyperinsulinemiainglucose---insulintests
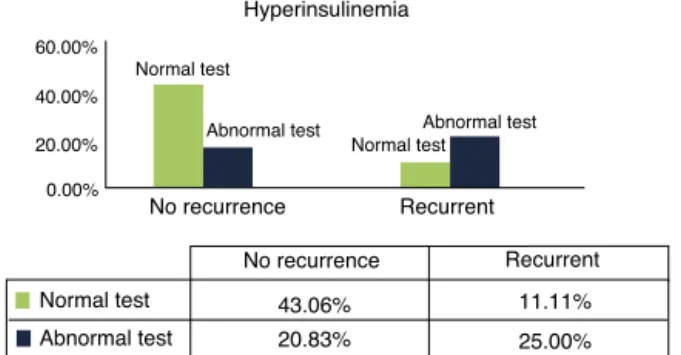
(Fig.3),RR=4.6647,p=0.0015.
• With a result of hyperglycemia in glucose---insulin tests (Fig.4),RR=2.4761,p=0.0123.
Glucose intolerance
No recurrence 0.00%
43.06%
20.83% 8.33%
27.78% 20.00%
40.00% 60.00%
No recurrence
Recurrent
Recurrent
Normal test Normal test
Normal test
Abnormal test Abnormal test
Abnormal test
Hyperinsulinemia
No recurrence
0.00%
43.06%
20.83%
11.11%
25.00%
20.00% 40.00% 60.00%
No recurrence
Recurrent
Recurrent
Abnormal test Abnormal test
Abnormal test
Normal test Normal test
Normal test
Figure 3 Distribution of patients with BPPV recurrence, regardingtestswithhyperinsulinemia.
Hyperglicemia
No recurrence
No recurrence Recurrent
Recurrent
Normal test
Normal test
Normal test
Abnormal test Abnormal test
Abnormal test
54.17%
9.72% 0.00%
20.00% 40.00% 60.00%
25.00%
11.11%
Figure 4 Distribution of patients with BPPV recurrence, regardingtestswithhyperglycemia.
Discussion
Dizzinessisamajorlimitingfactorinthedailylifeofthe gen-eralpopulation,withexacerbationintheelderlybecauseit affectsmovementsof thosewhoexperienceit,anditcan interfere with domestic and even social activities.16 The elderly lose their autonomy and become dependent indi-viduals,which further decreases their quality of life.17---20 Animportantconsequenceofdizzinessistheoccurrenceof falls,especiallyforthoseover60yearsofage,becausethe effectsareevenmoresevere.4InBrazil,6802elderly peo-plediedfromfallsintheyear201021---analarmingfactin termsofpublichealth.ThiscanbepartlyexplainedbyBPPV intheelderly.4
Althoughbenignparoxysmalpositionalvertigohasbeen arecognizedentityfor decades, itsetiologyremains pre-dominantlyidiopathic.6,22,23However,fewstudieshavebeen conductedwiththeaimtoclarifytherelationshipbetween BPPVand other comorbidities, and how they could influ-encethediseaseseverityandtheprognosisoftheseclinical pictures.
Thereisgoodevidencethatmetabolicdisorderscanbe associatedwithBPPV7---12butitisdifficulttoconfirmacausal relationship,sinceitisimpossibletoobservethe histopatho-logicalchangesin vivo.Thesemetabolicdisorderscanact asa principal etiological factor in vestibular dysfunction, aswellasanaggravatingfactorofapre-existingvestibular disorder.9
We did not find statistical significance for patients with glucose intolerance in relation to the number of recurrences, compared to normal subjects. This finding may suggest that this degree of change in carbohydrate
metabolismisnotsignificanttothepointofanassociation with the evolution of BPPV. However, no theories can be proposed untila larger numberof patients withimpaired glucosetoleranceandalsowithBPPVhavebeenevaluated. On the other hand, the presence of hyperinsulinism cannegatively impactinner earhemostasis,asaresultof theionic andmetaboliccharacteristics ofthe stria vascu-laris,whichisresponsibleformaintainingtheendocochlear potential throughpotassium secretion intoendolymphatic space.8,9 Furthermore, the labyrinth is very sensitive to small changes in plasma insulin levels, due to the large number ofinsulin receptors present inthe endolymphatic sac.11
Based on these suggestive signs (i.e., that glucose metabolismmaybeassociatedtoclinicalpicturesofbenign paroxysmalpositionalvertigo),thisstudyfoundsome rela-tions, such as: the hyperinsulinemic patient hasa RR 4.6 timeshigherforBPPVrecurrence,comparedwiththe gen-eralpopulation---astatisticallysignificantfinding.Likewise, the hyperglycemicpatient hasa RR2.47 times higherfor BPPVrecurrence,alsostatisticallysignificant.Ontheother hand,patientswithanormalglucose---insulincurvetesthave aRRofonly0.22,alsostatisticallysignificant.Thismeans thathavinganormalvalue maybeaprotective factorfor recurrenceofBPPV.
Tanimotoetal.24foundthattheonlyriskfactorfor recur-renceofBPPVwasthepresenceofendolymphatichydrops. Consideringthattheliteratureisprettyconsistentregarding theassociationbetweenhyperinsulinismandendolymphatic hydrops,wecancallintoquestionwhether,infact, hyperin-sulinismwouldnotbeanunderlyingeventtoendolymphatic hydrops---thislatterbeingtheactualriskfactor forthose recurrencevaluesfoundbytheauthorinhisseries.
Furthermore,Tanimotoetal.24 reportedthatthe recur-renceofbenignparoxysmalpositionalvertigowasassociated withsecondarycauses,morethantoidiopathicBPPV.This statement,combinedwiththe resultsofourstudy,makes it possible to propose the hypothesis of a form of BPPV secondarytoglucosemetabolismdisorders.
Conclusion
Glucose metabolism disorders are related toBPPV recur-renceinthegroupevaluated. Inthisstudy,wefound that bothhyperinsulinismandhyperglycemiabehavedasrisk fac-torsforrecurrenceofidiopathicBPPV,andalsothatanormal glucosetolerancetestactedasaprotectivefactor.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.PerezP,FrancoV,CuestaP,AldamaP,AlvarezMJ,MendezJC. Recurrenceofbenignparoxysmalpositionalvertigo.Otol Neu-rotol.2012;33:437---43.
3.ZhangY,ChenX,WangX,CaoL,DongZ,ZhenJ,etal.Aclinical epidemiologicalstudyin187patientswithvertigo.CellBiochem Biophys.2011;59:109---12.
4.Gananc¸aFF,GazzolaJM,Gananc¸aCF,CaovillaHH,Gananc¸aMM, CruzOLM.Quedasemidososcomvertigemposicional paroxís-ticabenigna.BrazJOtorhinolaryngol.2010;76:113---20.
5.ChoEI,WhiteJA.Positionalvertigo:asoccursacrossall age groups.OtolaryngolClinNAm.2011;44:347---60,viii.
6.CaldasMA,Gananc¸aCF,Gananc¸aFF,Gananc¸aMM,CaovillaHH. Clinicalfeaturesofbenignparoxysmalpositionalvertigo.Braz JOtorhinolaryngol.2009;75:502---6.
7.Kerber KA, Helmchen C. Benign paroxysmal positional ver-tigo: new opportunities but still old challenges. Neurology. 2012;78:154---6.
8.AngeliRD,LavinskyL,DolganovA.Alterationsincochlear func-tionduringinducedacutehyperinsulinemiainananimalmodel. BrazJOtorhinolaryngol.2009;75:760---4.
9.SerraAP,LopesKdeC,DoriguetoRS,Gananc¸aFF.Bloodglucose andinsulinlevelsinpatientswithperipheralvestibulardisease. BrazJOtorhinolaryngol.2009;75:701---5.
10.YodaS,CureogluS,Yildirim-BaylanM,MoritaN,FukushimaH, HaradaT,etal.Associationbetweentype1diabetesmellitus anddepositsinthesemicircularcanals.OtolaryngolHeadNeck Surg.2011;145:458---62.
11.BittarRSM,BottinoMA,SimoceliL,VenosaAR.Labirintopatia secundáriaaosdistúrbiosdometabolismodoac¸úcar:realidade oufantasia?BrazJOtorhinolaryngol.2004;70:800---5.
12.BittarRSM,Bottino MA,Zerati FE, Moraes CLdO, CunhaAU, BentoRF.Prevalênciadasalterac¸õesmetabólicasempacientes portadoresde queixas vestibulares.Braz J Otorhinolaryngol. 2003;69:64---8.
13.CohenHS.Newepidemiologicalfindingsonbenignparoxysmal positionalvertigo.JNeurolNeurosurgPsychiatry.2007;78:663.
14.CohenHS,KimballKT,StewartMG.Benignparoxysmalpositional vertigoandcomorbidconditions.ORL.2004;66:11---5.
15.DoriguetoRS, MazzettiKR,Gabilan YPL,Gananc¸a FF.Benign paroxysmalpositionalvertigorecurrenceandpersistence.Braz JOtorhinolaryngol.2009;75:565---72.
16.Standardsofmedicalcareindiabetes---2013.DiabetesCare. 2013;36Suppl.1:S11---66.
17.Kraft LR. Detection of diabetes mellitus in situ(occult dia-betes).LabMed.1975;6:10---22.
18.TakanoNA,CavalliSS,Gananc¸aMM,CaovillaHH,SantosMAdO, PelusoÉdTP,etal.Qualidadedevidadeidososcomtontura. BrazJOtorhinolaryngol.2010;76:769---75.
19.RibeiroAP,SouzaERd,AtieS,SouzaACd,SchilithzAO.A influên-ciadasquedas naqualidadede vida deidosos.CiêncSaúde Colet.2008;13:1265---73.
20.VazDP,GazzolaJM,LancaSM,DoriguetoRS,KasseCA.Clinical andfunctionalaspectsofbodybalanceinelderlysubjectswith benignparoxysmalpositionalvertigo.BrazJOtorhinolaryngol. 2013;79:150---7.
21.Brasil.Ministério daSaúde.Available at:www.datasus.gov.br
[accessed29.07.13].
22.Soto-Varela A, Rossi-Izquierdo M, Santos-Perez S. Benign paroxysmal positional vertigo simultaneously affecting sev-eral canals: a 46-patient series. Eur Arch Otorhinolaryngol. 2013;270:817---22.
23.vonBrevernM,RadtkeA,LeziusF,FeldmannM,ZieseT,Lempert T, et al. Epidemiology of benign paroxysmal positional ver-tigo:apopulationbasedstudy.JNeurolNeurosurgPsychiatry. 2007;78:710---5.