Brazilian
Journal
of
OTORHINOLARYNGOLOGY
www.bjorl.org
ORIGINAL
ARTICLE
Impact
of
early
elective
tracheotomy
in
critically
ill
patients
夽
Isabel
Araújo
Marques
Correia
∗,
Vítor
Sousa,
Luis
Marques
Pinto,
Ezequiel
Barros
HospitalSãoJosé,Lisbon,Portugal
Received27November2013;accepted9February2014 Availableonline22July2014
KEYWORDS
Intratracheal intubation;
Intensivecareunits; Otorhinolaryngologic
surgicalprocedures
Abstract
Introduction:Tracheotomyisoneofthemostfrequentsurgicalproceduresperformedin criti-callyillpatientshospitalizedatintensivecareunits.Theidealtimingforatracheotomyisstill controversial,despitedecadesofexperience.
Objective:Todeterminetheimpactofperformingearlytracheotomiesincriticallyillpatients ondurationofmechanicalventilation,intensivecareunitstay,overallhospitalstay,morbidity, andmortality.
Methods:Retrospectiveandobservationalstudyofcasessubjectedtoelectivetracheotomyat oneoftheintensivecareunitsofthishospitalduringfiveconsecutiveyears.Thepatientswere stratifiedintotwogroups:earlytracheotomygroup(tracheotomyperformedfromdayoneup toandincludingdaysevenofmechanicalventilation)andlatetracheotomygroup(tracheotomy performedafterdayseven).Theoutcomesofthegroupswerecompared.
Results:Intheearlytracheotomygroup,therewasastatisticallysignificantreductionin dura-tionofmechanicalventilation(6daysvs.19days;p<0.001),durationofintensivecareunit stay(10daysvs.28days;p=0.001),andincidenceofventilator-associatedpneumonia(1case
vs.44cases;p=0.001).
Conclusion:Earlytracheotomyhasasignificantpositiveimpactoncriticallyillpatients hospi-talizedatthisintensivecareunit.Theseresultssupportthetendencytobalancetherisk-benefit analysisinfavorofearlytracheotomy.
© 2014Associac¸ãoBrasileira de Otorrinolaringologiae CirurgiaCérvico-Facial. Publishedby ElsevierEditoraLtda.Allrightsreserved.
夽
Pleasecitethisarticleas:CorreiaIA,SousaV,PintoLM,BarrosE.Impactofearlyelectivetracheotomyincriticallyillpatients.BrazJ Otorhinolaryngol.2014;80:428---34.
∗Correspondingauthor.
E-mail:isabelmcorreia@gmail.com(I.A.M.Correia).
http://dx.doi.org/10.1016/j.bjorl.2014.07.008
1808-8694/©2014Associac¸ãoBrasileiradeOtorrinolaringologia eCirurgiaCérvico-Facial. PublishedbyElsevierEditoraLtda.All rights
PALAVRAS-CHAVE
Intubac¸ão intratraqueal;
Patologiacirúrgica;
Procedimentos cirúrgicos
otorrinolaringológicos
Impactodatraqueotomiaeletivaprecocenosdoentescríticos
Resumo
Introduc¸ão: Atraqueotomiaéum dosprocedimentoscirúrgicosmaisfrequentesem doentes críticosinternadosem unidadesdeterapiaintensiva.Oseutimingidealéainda,apesarde décadasdeexperiência,umaquestãocontroversa.
Objetivos: Determinaroimpactodarealizac¸ãodetraqueotomiasprecocesem doentes críti-cosnadurac¸ãodaventilac¸ãomecânica,dointernamentonaunidadedeterapiaintensiva,do internamentohospitalar,emortalidadeemorbidade.
Método: Estudoobservacionalretrospectivodoscasossubmetidosàtraqueotomiaeletivaem umadasunidadesdeterapiaintensivadonossohospitaldurante5anosconsecutivos.Osdoentes foramdivididosemdoisgrupos,tendosidosubmetidosatraqueotomiasprecoces(atéo7◦dia
de ventilac¸ãomecânica, inclusive)ou tardias(após o 7◦ dia de ventilac¸ãomecânica), eos
resultadosforamcomparados.
Resultados: Nosdoentes submetidosauma traqueotomiaprecoce verificou-seuma reduc¸ão estatisticamentesignificativanadurac¸ãodaventilac¸ãomecânica(6diasvs.19dias;p<0,001), nadurac¸ãodointernamentonaunidadeterapiaintensiva(10diasvs.28dias;p=0,001)ena incidênciadepneumoniaassociadaaoventilador(1casovs.44casos;p=0,001).
Conclusão:Atraqueotomiaprecocetemumimpactopositivoestatisticamentesignificativonos doentescríticos.Osresultadossuportamatendênciadeequilibrarorisco-benefícioemfavor datraqueotomiaprecoce.
©2014Associac¸ãoBrasileiradeOtorrinolaringologiaeCirurgiaCérvico-Facial.Publicado por ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
Tracheotomy is one of the most frequently performed
surgical procedures in critically ill patients admitted to
intensivecareunits(ICUs).1Theadvantagesoftracheotomy
regarding prolonged orotracheal intubation have been described,suchasthereductionoflaryngeallesions,greater ease in ventilator weaning by decreasing airway resis-tance,decreasedneedfordeepsedation,betterpulmonary hygiene, increased patient mobility, improved communi-cation and oral nutrition, and subjective improvement in patientsatisfaction.2---4 In addition tothese,some studies
haveshownanassociationbetweenearlytracheotomyand shorterdurationofmechanicalventilationandICUstay,with a decrease in ventilator-associated pneumonia (VAP).4---7
However,tracheotomycarriessome risk ofcomplications, includingbleeding, infection ofthe stoma, pneumothorax or pneumomediastinum,injury tovascular ornerve struc-tures,trachealstenosis,tracheoesophagealfistula,oreven death.5,7,8 Thus, the decision to perform a tracheotomy
and when the procedure should be conducted must be based on a balance between risks and benefits, while alsoconsideringthecostsandanefficientmanagementof resources.2Despitedecadesofexperience,theoptimal
tim-ing of tracheotomy is still a contentious issue, for both otorhinolaryngologists and intensivists, and the impactof earlytracheotomyontheresultsofpatientsadmittedtoICU isstillunclear7,9,10(andeventhedefinitionofearlyandlate
tracheotomy is a controversial subject).7,11 The practices
have been heterogeneousamong thevarious centers.7,9,10
Thisissuewasanincentivetoperformaretrospectivestudy incriticallyillpatientsadmittedtoapolyvalentICUatthe present hospital,in order to analyzethe impactof early electivetracheotomyinoutcomesof patientsadmittedto
theICU.Theaimwastotestthehypothesisthatearly tra-cheotomy,comparedwithlatetracheotomy,canreducethe durationofmechanicalventilation,lengthofstayintheICU andinthehospital,VAPincidence,andmortalityincritically illpatients.
The main objectives of the study were to compare critical patients undergoing early tracheotomy and those undergoinglatetracheotomy,inrelationtothedurationof mechanicalventilation,lengthofstayin ICUandin hospi-tal,incidence ofVAP, and mortality.Secondary objectives includedevaluatingtheincidenceof complicationsof tra-cheotomyand whether there were significant differences betweenthetwogroupsregardingage,gender,ICU admis-siondiagnosis,comorbidities,andcomplications.
Materials
and
methods
Studydesignandeligibility
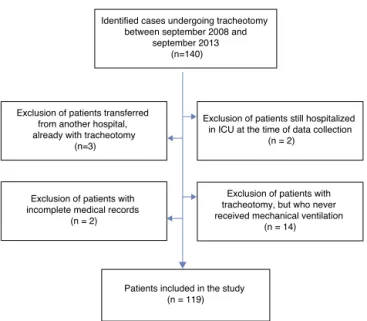
Identified cases undergoing tracheotomy between september 2008 and
september 2013 (n=140)
Exclusion of patients transferred from another hospital, already with tracheotomy
(n=3)
Exclusion of patients still hospitalized in ICU at the time of data collection
(n = 2)
Exclusion of patients with incomplete medical records
(n = 2)
Exclusion of patients with tracheotomy, but who never received mechanical ventilation
(n = 14)
Patients included in the study (n = 119)
Figure1 Diagramofpatientexclusion.
mechanical ventilation (vocal cord paralysis, laryngeal fracture, mandibular fracture, and cervical abscess);and twodue toincomplete medical records. Thus, a total of 119patientswereincludedinthisstudy.
Patientsandprocedure
The119patientsweredividedintotwogroups,dependingon thetimingoftracheotomy.Intheearlytracheotomygroup, patientswhounderwenttracheotomybetweendaysoneand seven(included)of mechanicalventilation wereincluded; in the late tracheotomy group, patients who underwent tracheotomy after the seventh day of mechanical venti-lation were included. Early and late tracheotomy were definedassuch,sincemostrecentstudieshaveadoptedthis definition,4---7andsomeauthorsindicatethatthereare
sig-nalsofendolaryngeallesionsaftersevendaysoforotracheal intubation.2
All patients were over 18 yearsold. All tracheotomies wereelectiveandperformedbyotolaryngologistsusingthe traditionalsurgicaltechnique,whetheratthebedside(ICU) orintheoperatingroom.IntheICU,thetracheotomieswere performedunderunconscioussedation,andinthe operat-ingroomundergeneralanesthesia.Thetechniqueconsisted ofahorizontalskinincision, theinfra-isthmicapproachof trachea,withopeningofthetracheain‘‘lyingdownH.’’In mostpatients,Shileycuffedcannulas(#6or#8,inwomen and men, respectively) were placed, unless the patient’s anatomynecessitatedtheuseofanothertypeofcannula.
Collectionofdata
Data were collected by the authors and organized with MicrosoftExcel®forMac2011.Dataondemographics;cause ofICU admission;comorbidities;date of admissionandof hospitalandICUdischarge;dateoforotrachealintubation; date of starting and ending of mechanical ventilation; incidenceofVAP(definedasa visiblepulmonary infiltrate onachestradiographwithfever,leukocytosis,andpurulent
tracheobronchialsecretionswithpositivecultures,starting at least 48h after intubation);12 date and place of
tra-cheotomy;andcomplicationsoftracheotomyandmortality werecollected.
Duetosomecharacteristicsinherenttotheorganization ofthePortugueseHealthService,48patients(40.3%)were transferred,afterdischargefromICU,toothernational hos-pitalsintheirareaofresidence(orinternationalhospitals, inthecaseofforeignpatients),ortocontinuedcareunits. Forthisreason,hospitaldischargedateswereonlyobtained fortheremaining71(59.7%)patients,whoweretransferred tootherinpatientservicesofthepresenthospital.
Data
analysis
ThedurationofmechanicalventilationandofICUand hos-pitalstaywasthencalculated.Mechanicalventilationwas measured(indays)fromtheconnectionoftheorotracheal tube to the ventilator until the complete disconnection, or patientdeath; durationofICU staywasmeasuredfrom admission untildischarge fromthe ICU, or patientdeath; and duration of hospital stay was measured from admis-sionuntilhospitaldischarge,or patientdeath. The timing of tracheotomywasmeasured in daysfromthe beginning ofmechanicalventilationuntilthedayoftracheotomy.The timeelapsed betweenthetracheotomyandthe discharge fromICUwasalsocalculated.
The statistical analysis was performed with SPSS 20.0 forMac.Todescribecategoricalvariables,frequenciesand proportions wereused. Forcontinuous variables,medians and interquartilerangewere usedasmeasures of central tendencyanddispersion,respectively,astheyhadskewed distribution. Inthe analysis of association between varia-bles, the following nonparametric tests were performed: Mann---WhitneyU,chi-squared,andSpearman’scorrelation. Avalueofp<0.05wasconsideredstatisticallysignificant.
Results
Characteristicsofpatients
Ofthe119patientsincludedinthestudy,18(15.1%) under-went early tracheotomy (ET), i.e. up to seven days of mechanical ventilation; the remaining 101 (84.9%) under-wentlatetracheotomy(LT),i.e.aftertheseventhday.
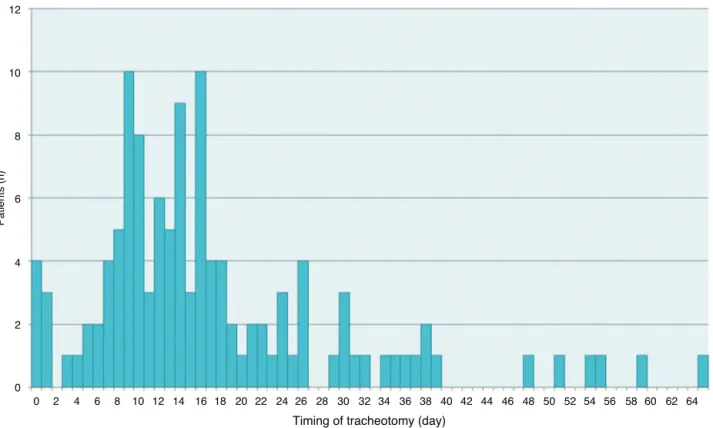
Thedistributionofpatientsbytimingofthetracheotomy isdepictedinFig.2.
ETand LT groups didnot differsignificantly bygender (p=0.17),age (p=0.56),admissiondiagnosis (p=0.56),or comorbidities(p=0.08)(Table1).
12
10
8
6
4
2
0
0 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 32 34 36 38 40 42 44 46 48 50 52 54 56 58 60 62 64
Timing of tracheotomy (day)
Patients (n
)
Figure2 Distributionofpatientsbytimingoftracheotomy.
Siteoftracheotomyandcomplications
The groups also did not differ significantly regarding the tracheotomy site (p=0.49) (Table 1). Most tracheotomies were performed at the ICU bedside (96.6% ICU vs. 3.4% operating theater). The tracheotomies performed in the operatingroomwereconductedinpatientsundergoingother surgeries,inwhomtherewasaneedfortracheotomy;both procedureswereperformedduringthesameoperation. Oth-erwise,thetracheotomywouldhavealsobeenperformedat thebedside.
Theoccurrenceofearlycomplications(uptoonemonth aftertracheotomy)wasobservedinonly14patients(11.8%), and the most common complication was tracheostoma bleeding(8.4%);othercomplicationsweretheemergenceof afalsepassage(1.7%)necessitatingatracheotomyrevision; decannulationandtracheostomainfection,whichoccurred in the same patient (0.8%), and laceration of the poste-rior wall of the trachea in another patient (0.8%). Most bleedings were of low output and self-limited, occurring 24---48h after the procedure; some had to be controlled withcompressionpackingusingahemostaticagent.There were no statistically significant differences between the twogroupsregardingcomplications(ET22.2%vs.LT22.9%; p=0.07).
Durationofmechanicalventilation,ICUstay,and
hospitalstay
Table2showsthemainresultsinaccordancewiththe tim-ing of tracheotomy. In all patients, the median duration ofmechanicalventilationwas17days(interquartilerange
10---34)and,for the ICU stay,26days(interquartilerange 15---42). However, ET was associated with a significantly shorterduration ofmechanical ventilation (6vs.19 days, p<0.001)andashorterdurationofICUstay,alsostatistically significant(10vs.28days,p=0.001).
Asexplainedinthemethodologyofthisstudy,theauthors hadaccessonlytodatesofhospitaldischargefor71patients (59.7%).Inthesepatients,themediandurationof hospital-izationwas44days(interquartilerange27---95). Ashorter durationof hospitalizationintheETgroup(39daysvs.45 days)was found, although withno statistical significance (p=0.41).
The time elapsed between tracheotomyand discharge fromICUwasshorterinETgroup(3daysvs.7days),although notstatisticallysignificant(p=0.26).
Figs.3and4showthedistributionofpatientsbytimingof tracheotomy(timeelapsedbetweentheonsetof mechani-calventilationandthetracheotomyprocedure)andduration ofmechanicalventilationorICUstay,respectively.A corre-lationbetweenthedurationofmechanicalventilationand timingoftracheotomy(Spearman’scorrelation=0.68, cor-respondingtoaR2=0.46)andbetweenthedurationofICU stay and the timing of tracheotomy (Spearman’s correla-tion=0.61;R2=0.37)wasfound.
IncidenceofVAPandmortality
VAP occurred in 45 patients (37.8%). Only one patient in ETgroupdeveloped VAP. The differencebetweenthe two groupswasstatisticallysignificant(p=0.001)(Table2).
Table1 Characteristicsofpatients,complications,andsiteofthetracheotomy.
Total(n=119) Earlytracheotomy (n=18)
Latetracheotomy (n=101)
p-value
Gender 0.17
Female 38(31.9) 3(16.7) 35(34.7)
Male 81(68.1) 15(83.3) 66(65.3)
Age,median(interquartilerange) 66(51---76) 63(46---75) 66(52---76) 0.56
Admissiondiagnosis,n(%) 0.56
Respiratoryinsuf./failure 21(17.6) 3(16.7) 18(17.8)
Cardiovascularinsuf./failure 18(15.1) 2(11.1) 16(15.8)
Neurological 36(30.3) 5(27.8) 31(30.7)
Sepsis 15(12.6) 1(5.6) 14(13.9)
Polytrauma 21(17.6) 4(22.2) 17(16.8)
Other 5(4.2) 2(11.1) 3(3.0)
2ormorediagnoses 2(1.7) 1(5.6) 1(1.0)
Unknown 1(0.8) 0(0.0) 1(1.0)
Comorbidities,n(%) 0.08
Hypertension 12(10.1) 0(0.0) 12(11.9)
Coronaryarterydisease 3(2.5) 0(0.0) 3(3.0)
TypeIIDM 2(1.7) 1(5.6) 1(1.0)
Stroke 2(1.7) 0(0.0) 2(2.0)
Neoplasticdisease 4(3.4) 0(0.0) 4(4.0)
Other 14(11.8) 3(16.7) 11(10.9)
Missing/unknown 25(21.0) 8(44.4) 17(16.8)
Twoormorecomorbidities 57(47.9) 6(33.3) 51(50.5)
Complications,n(%) 0.07
None 105(88.2) 14(77.8) 91(90.1)
Tracheostomableeding 10(8.4) 1(5.6) 9(8.9)
Falsepassage 2(1.7) 1(5.6) 1(1.0)
Decannulation+tracheostomainfection 1(0.8) 1(5.6) 0(0.0)
Tracheallaceration 1(0.8) 1(5.6) 0(0.0)
Tracheotomysite,n(%) 0.49
Bedside(ICU) 115(96.6) 17(94.4) 98(97.0)
Operatingtheater 4(3.4) 1(5.6) 3(3.0)
DM,diabetesmellitus;ICU,intensivecareunit.
Table2 Mainresults.
Total(n=119) Earlytracheotomy (n=18)
Latetracheotomy (n=101)
p-value
MVlength(days),median(interquartile range)
17(10---34) 6(2---8) 19(12---35) <0.001
ICUlength(days),median(interquartile range)
26(15---42) 10(7---26) 28(17---43) 0.001
Inpatienthospitallength(days),median (interquartilerange)
44(27---95) 39(13---80) 45(27---98) 0.41
Tracheotomylength---dischargeICU(days), median(interquartilerange)
6(3---21) 3(2---17) 7(3---21) 0.26
Mortality,n(%) 27(22.7) 2(11.1) 25(24.8) 0.36
VAP,n(%) 45(37.8) 1(5.6) 44(43.6) 0.001
200
150
100
50
0
20
0 40 60
Time between MV start and tracheotomy
MV time (days)
R2Linear = 0.462
Figure 3 Spearman’s correlation: correlation was found between the duration of mechanical ventilation (MV) and timing of tracheotomy (time between MV start and tra-cheotomy)−R2=0.46.
R2 Linear = 0.373
20
0 40 60
Time between MV start and tracheotomy 200
150
100
50
0
ICU stay (days)
Figure 4 Spearman’s correlation: correlation was found between thedurationofICU stayandtiming oftracheotomy (timebetweenMVstartandtracheotomy)−R2=0.37.
although with a tendency tolower mortality in ET group
(11.1% vs.24.8%). None of the deaths were attributedto
thetracheotomyprocedure.
Discussion
This study demonstrates that the practice of early
tra-cheotomyin criticallyillICU patients isassociated witha
statisticallysignificantreductionindurationofmechanical
ventilation,durationofICUstay,andincidenceofVAP.This
findingis inagreement withmanystudies thathave been
conductedinothercenters.4---7ThissuggeststhatET,aswell
ashavingapositiveimpactonpatientmorbidity(lower inci-denceofVAP),hasthepotentialtopositivelyinfluencethe managementof resourcesassociated withthe hospitaliza-tionofpatientsinanICU,bydecreasingtheICUstay.
In addition, a correlation between the duration of mechanicalventilationandtimingoftracheotomy(Fig.3), andbetweenthelengthofICUstayandthetimingofthe tra-cheotomy(Fig.4)wasfound,whichindicatesthatthetiming of the tracheotomy explains 46% of the days of mechan-icalventilation(R2=0.46)and37% ofthedaysofICU stay (R2=0.37).Therefore,consideringthatcontinuousvariables werecompared, it can beconcluded that the soonerthe patientissubjectedtotracheotomy,theshorterthe dura-tionofmechanicalventilationandofICUstay.
Mortality was not significantly lower in ET group, although there was a trend toward reduced mortality in thisgroupcomparedtotheLTgroup(11.1%vs.24.8%).This findingisconsistentwithmoststudiesintheliterature.4---7,13
Consideringthat71patientsremainedhospitalizedafter dischargefromtheICU,thedurationofthetotal hospitaliza-tionwasnotsignificantlyreducedinETgroup(althoughwith atendencytowardreduction),ashasbeendemonstratedin manystudies,andinaccordancewiththeshorterduration ofICUstayofthisgroup.
After tracheotomy, discharge from the ICU occurred rapidly(ET3daysvs.LT 7days)andinasimilarperiodin bothgroups(p=0.26),suggestingthatthisprocedurewasa keyfactorinfacilitatingthediscontinuationofinvasive ven-tilationsupport,decreasingthelevelofintensivecare,and infacilitatingICUdischarge,ashasbeensuggestedinother studies.4---6,11
Gender, age, admission diagnosis, and comorbidities weresimilarinbothgroups.
Electivetracheotomybytraditionalsurgicaltechniqueis asafeprocedure; inthepresentstudy,alowincidenceof earlycomplicationswasfound(11.8%),mostlyunimportant (self-limitedbleeding)andwithoutseriousconsequencesfor thepatient.Theseearlycomplicationswerealsosimilarin bothgroups.
Most procedures were performed in the ICU, and this contributedtoareductioninthecostandtimeassociated withsurgery,avoidingunnecessarycostsofroomoccupancy in the operating theater and of movement of ventilated patients,withbetterpatientcomfort.Likewise,no differ-encesbetweengroupswerefoundresultingfromthesiteof theprocedure.
Thisstudyhastheadvantageofdemonstratingbenefitsof ETonapopulationofunselectedcriticallyillpatients,while mostpreviousstudieshavefocusedonmorespecificpatient subgroups:medicalpathology,14 traumaticcondition,6and
theelderly,5amongothers.
Due to its retrospective design, this study has some limitations. Althoughthe data analysisfor age,admission diagnosis, and comorbidities of the two groups did not show statistically significant differences, a selection bias of patients who underwent ET, compared toLT, probably occurred;thisbiaswouldbeeliminatedwithaprospective randomizedstudy.Thetimingoftracheotomywaschosenby thephysicianresponsibleforthepatient;certainly,an indi-vidualselectionprocessfortherealizationofETexisted,a processthatwasnot documentedinthe medicalrecords, such as when the decision to perform tracheotomy was made,andtheexactreasonforit.
did not occur; instability of the patient for an early tra-cheotomy;anddifficultweaningfrominvasiveventilation. Variousattemptshavebeenmadetodevelopaformulafor predicting the likelihoodof a patient requiring prolonged ventilation;suchaformulawouldallowabetterselectionof patientsforperformingET.Todate,novalidatedsystemhas beenfound toforecast theneedfor prolongedventilation intheintensivecaregeneralpopulation,andthereforethe selectionofpatientsfortracheotomyremainsasubjective decision.However,thefavorableresultsofthistrialandof studiesconductedinothercenterssuggestabenefitinearly performanceoftracheotomy(uptodaysevenofmechanical ventilation).
Conclusions
This study suggeststhat ET (uptoday seven of mechani-calventilation)hasastatisticallysignificantpositiveimpact in critically ill ICU patients, by reducing the duration of mechanicalventilation,ICUstay,andincidenceofVAP,and likelyreducing mortality and length of hospital stay. The studydemonstratedthatthesoonerthepatientissubjected totracheotomy,theshorterthedurationofmechanical ven-tilationandthetimeofICUstay.Theseresultssupportthe tendencytobalancetherisk-benefitanalysisinfavorofearly tracheotomy.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgement
TheauthorswouldliketothankDr.ManuelJoséMagalhães forhishelpwiththestatisticalanalysis.
References
1.DurbinJrCG.Tracheostomy:why,when,andhow?RespirCare. 2010;55:1056---68.
2.McWhorterAJ.Tracheotomy:timingandtechniques.CurrOpin OtolaryngolHeadNeckSurg.2003;11:473---9.
3.HeffnerJE,HessD.Tracheostomymanagementinthe chroni-callyventilatedpatient.ClinChestMed.2001;22:55---69.
4.TongCC,KleinbergerAJ,PaolinoJ,AltmanKW.Tracheotomy timingandoutcomesinthecriticallyill.OtolaryngolHeadNeck Surg.2012;147:44---51.
5.SchneiderGT, ChristensenN,DoerrTD.Earlytracheotomyin elderlypatientsresultsinlessventilator-associatedpneumonia. OtolaryngolHeadNeckSurg.2009;140:250---5.
6.Arabi Y, Haddad S, Shirawi N, AI Shimemeri A. Early tra-cheostomyinintensivecaretraumapatientsimprovesresource utilization: a cohort study and literature review. Crit Care. 2004;8:347---52.
7.Griffiths J, Barber VS, Morgan L, Young JD. Systematic review and meta-analysis of studies of the timing of tra-cheostomyinadultpatientsundergoing artificialventilation. BMJ.2005;330:1243.
8.LindmanJ,MorganC,PeraltaR,ElluruR,UpdatedSep18 Tra-cheostomy.Emedicine-Medscape;2012.
9.HolevarM,DunhamJC,BrautiganR,ClancyTV,ComoJJ,Ebert JB,etal. Practicemanagementguidelinesfor timing of tra-cheostomy: the EAST Practice Management Guidelines Work Group.JTrauma.2009;67:870---4.
10.WangF,WuY, BoL, LouJ,ZhuJ,ChenF,etal. Thetiming oftracheotomyincriticallyillpatientsundergoingmechanical ventilation:asystematicreviewandmeta-analysisof random-izedcontrolledtrials.Chest.2011;140:1456---65.
11.MacIntyreNR,CookDJ,ElyJrEW,EpsteinSK,FinkJB,Heffner JE,etal.Evidence-basedguidelinesforweaningand discontin-uingventilatorysupport:acollectivetaskforcefacilitatedby theAmericanCollegeofChestPhysicians;theAmerican Associ-ationforRespiratoryCare;andtheAmericanCollegeofCritical CareMedicine.Chest.2001;120:375S---95S.
12.MeduriGU.Diagnosisand differentialdiagnosisof ventilator-associatedpneumonia.ClinChestMed.1995;16:61---93.
13.BlotF,SimilowskiT,TrouilletJL,ChardonP,KorachJM,Costa MA,et al. Early tracheotomyversus prolonged endotracheal intubationinunselectedseverelyillICUpatients.IntensiveCare Med.2008;34:1779---87.