COMPARATIVE STUDY OF INTRA OSSEOUS WIRING, MINIPLATE
OSTEOSYNTHESIS AND RECONSTRUCTION PLATE WITH BONE
GRAFT IN THE METHOD OF TREATMENT FOR MANDIBULAR
FRACTURE
Asok Kumar Saha1, Siddhartha Das2, Prasanna Datta3, Arup Chakrabarty4, Anindya Priya Saha5,
Sananda Saha6
HOW TO CITE THIS ARTICLE:
Asok Kumar Saha, Siddhartha Das, Prasanna Datta, Arup Chakrabarty, Anindya Priya Saha, Sananda Saha.
”Comparative Study of Intra Osseous Wiring, Miniplate Osteosynthesis and Reconstruction Plate with Bone Graft in the Method of Treatment for Mandibular Fracture”. Journal of Evidence based Medicine and Healthcare; Volume 2, Issue 32, August 10, 2015; Page: 4677-4686, DOI: 10.18410/jebmh/2015/658
ABSTRACT: The mandible or lower jaw is one of the most commonly encountered maxillo facial fractures in our clinical practice. Un-displaced, single and closed fractures are usually managed by closed method with maxillo-mandibular fixation (MMF). Displaced open and multiple fractures are treated by open reduction and internal fixation (ORIF). Displaced, open and multiple fractures are treated by ORIF by various methods like intraosseus wiring, miniplate osteosynthesis and reconstruction plate with bone graft. Present study is done to evaluate these three methods of ORIF and their post-operative outcome. Our study material comprises 72 cases of isolated mandibular fracture of adult patient. All these patients are treated by ORIF by either of the three above methods. These patients are divided into three groups. Group A includes 18 cases treated by intra osseous wiring and post-operative maxillo mandibular immobilization for 4 weeks. Group B includes 38 cases treated with single or double miniplate and no post-operative immobilization. Group C includes 11 cases treated by reconstruction plate with bone graft along with miniplate in patients having bone loss or gap fractures. The surgical outcome based on parameters such as malocclusion, intra oral exposure of plate, wound dehiscence, delayed union, plate fracture, non- union and sensory deficit are compared at 4-6 weeks after operation among the three groups and patients are followed up every three months interval. The results are statistically analysed and it is concluded that the use of miniplate gives better result in comparison to intra osseous wiring. In cases of bone loss or gap fracture reconstruction plate and bone graft along with miniplate are effective.
KEYWORDS: Mandibular fractures, Intra osseous wiring, Miniplate osteosynthesis, Reconstruction plate, Bone graft.
Aims and Objective of Present Study:
To analyze the treatment modality by miniplate osteosynthesis over intraosseus wiring
To evaluate the usefulness of Reconstruction plate in comminuted or gap fractures.
MATERIALS AND METHODS: The study was conducted in ENT department, Medical College & Hospital.
Study Period: November 2007 – October 2014.
108 patients (Male & Female) sustained maxillofacial fracture were admitted in ENT department of Medical College & Hospital, Kolkata for ORIF.
Factors analyzed were age, sex, anatomical sites, cause of fractures and treatment modality used. Statistical analysis for the comparison of mode of treatment was done by suitable statistical tests at p <= level.
OBSERVATIONS:
Incidence of Fractures: Out of 108 patients, 72 cases were mandibular fractures, 24 cases were Zygomatic fractures and 12 cases were maxillary fractures. Ratio of mandibular, Zygomatic and maxillary fractures is 6:2:1 respectively.
Sex: Out of 72 patients sustained mandibular fractures 54 patients were male and 18 patients were female, Male: Female =3:1(male are more predominant for sustained mandibular fracture).
Causes of Fractures:
Road traffic accident (30) = 41.7%. Assault (24) = 33.3%.
History of fall (10) = 13.9%. Work accident (6) = 8.3%. Pathological fractures (2) =2.8%.
Age of Incidence: It is ranging from 15 years to 60 years of age; Peak age incidence is 25 – 34 years of age.
Age group in years Number of patients Percentage
15-24 18 25
25-34 32 44.44
35-44 14 19.44
45-54 6 8.33
>55 2 2.77
Table 1: Age of Incidence
Location of Fractures in Mandible:
Fractures (#) No. of patients %
Body of Mandible 24 33
Condyle 18 25
Angle of mandible 16 22
Symphysis 8 11
Ramus 2 3
Alveolar 2 3
Coronoid 2 3
Table 2: Location of fractures in mandible
Clinical Findings are; Mandibular Pain.
Malocclusion.
Inability to fully open mouth
Preauricular pain with biting.
Imaging Studies Include:
Panoramic radiograph of mandible - it is most informative radiological study.
Plain films include lateral/ posterio anterior and periepical views.
CT scan helps to visualize the fracture in other areas like frontal bone, NEO complex and orbit. CT is ideal for condylar fractures which are difficult to visualize in plain films.
Treatment: Both closed and open methods are useful for reduction and immobilization of the mandibular fractures. In closed methods intra dental wiring and inter maxillary fixation (IMF) are done. Most of the condylar fractures are also treated by closed methods except bilateral displaced condylar neck and high intra-capsular fractures that are managed by open method.(2) In open
method fracture site is exposed and fragments are reduced and fixed by direct intraosseus wiring or miniplate fixation. In case of bone loss or gap fractures reconstruction plate and corticocancellous bone graft along with mini plate fixation are effective. In our study all the patients underwent ORIF.
Indications for ORIF are:
Displaced or unstable angle, body or parasymphyseal fractures;
Multiple fractures, associated condylar fractures and fracture of an edentulous mandible when IMF not possible.
Surgical Approaches for Mandibular Fractures are:
Intraoral approach is used for fracture of Symphysis and parasymphysis region.(3)
Extra oral submandibular approach by Ridson’s incision is made to access the fractures of ramus, angle and posterior body of mandible.
Internal Fixation is done by:
Intraosseus wiring for fixation of parasymphyseal fracture and angle fracture with post- operative maxillomandibular immobilization for 4 weeks.
In our study this was done in 18 cases of mandibular fractures without gap or no bone loss (Group A).
Miniplate osteosynthesis technique with no postoperative immobilization was used in 38 cases to get rigid and stable fixation by single miniplate or double miniplate (Group B), in anterior mandible two plates are used while posteriorly one plate is usually sufficient.(4) In gap fracture fixation is reinforced with reconstruction plate and bone graft harvested
Dimension of Miniplate and Miniscrews available are:
Plates and monocortical screws are made of stainless steel or titanium.
The plates available in various sizes are 4 holes, 6 holes, 8-16 holes plates.
Plate thickness is 0.9mm.
Diameter of the hole is 2.1 mm with a bevel of 30 degree.
Self-tapping screw is 2mm in diameter and 10mm in length.
Drill used to prepare the hole in the bone is 1.6mm (0.4 mm smaller than the screw size).
One turn of the screw is 1mm penetration into the bone.
In our study only Titanium miniplates were used;
Fig. 3 & 4: Miniplate, Miniscrews, reconstruction plates and instrument s used for ORIF
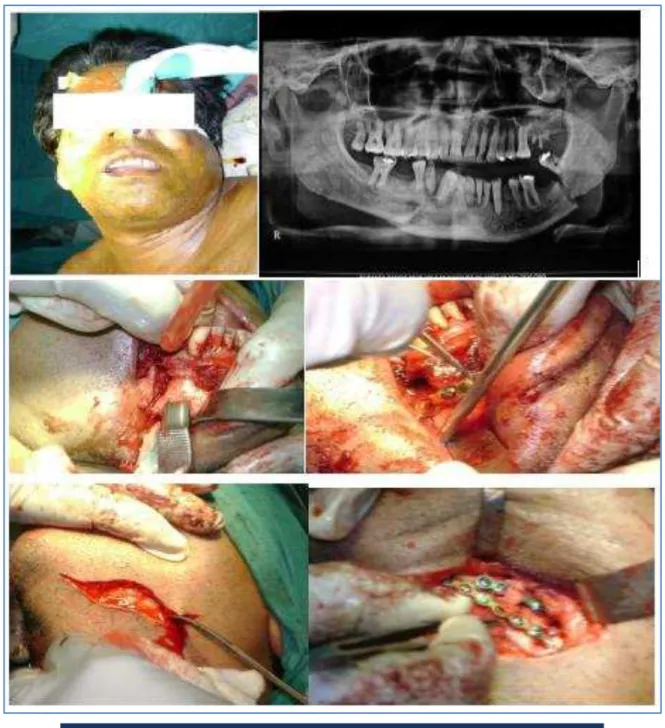
Fig. 9-11: 36years old female patient presented with parasymphyseal fracture (R) following assault. ORIF is done
by miniplate fixation with intraoral approach
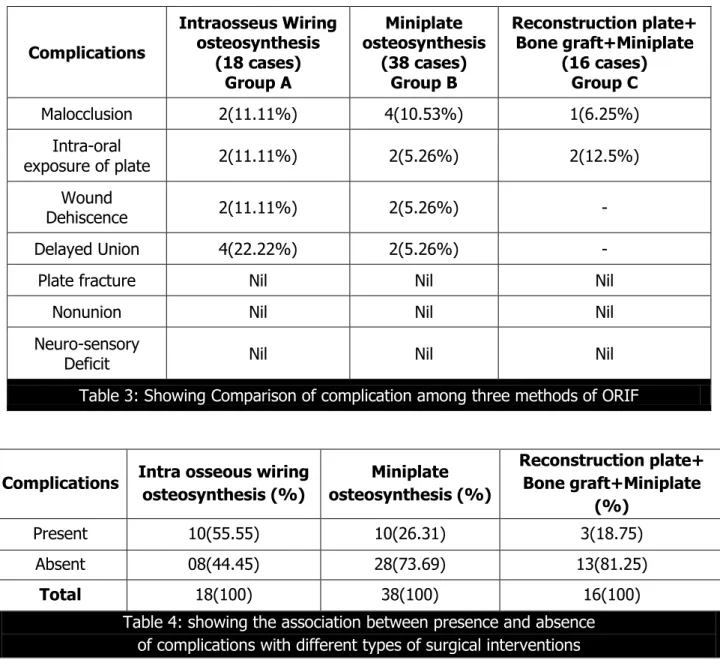
RESULTS: It is a Prospective study; Patients are reviewed at 4-6 weeks following operation and followed every 3 months interval. Clinical and radiological outcome of treatment in respect to malocclusion, intraoral exposure of plate, wound dehiscence, delayed union, plate fracture, non-union and neuro sensory deficit were analysed in table 3.
Complications Intraosseus Wiring osteosynthesis (18 cases) Group A Miniplate osteosynthesis (38 cases) Group B Reconstruction plate+ Bone graft+Miniplate (16 cases) Group C
Malocclusion 2(11.11%) 4(10.53%) 1(6.25%)
Intra-oral
exposure of plate 2(11.11%) 2(5.26%) 2(12.5%)
Wound
Dehiscence 2(11.11%) 2(5.26%) -
Delayed Union 4(22.22%) 2(5.26%) -
Plate fracture Nil Nil Nil
Nonunion Nil Nil Nil
Neuro-sensory
Deficit Nil Nil Nil
Table 3: Showing Comparison of complication among three methods of ORIF
It has been seen that rate of complication in Intra osseous wiring osteosynthesis, Miniplate osteosynthesis and Reconstruction plate + Bone graft + Miniplate are 55.55%, 26.31% and 18.75% respectively. Statistical analysis (Chi square test at the significant level of 0.05) has been done to find out the association between presence and absence of complications with different types of surgical interventions. The Chi square value is 6.4508, p value is 0.039739. The result is significant at p=<0.05. So from the analysis it can be said that the rate of complication is highest in Intra osseous wiring osteosynthesis followed by Miniplate osteosynthesis and Reconstruction plate + Bone graft + Miniplate and this association is statistically significant at p=<0.05.
Complications Intra osseous wiring osteosynthesis (%) Miniplate osteosynthesis (%) Reconstruction plate+ Bone graft+Miniplate (%)
Present 10(55.55) 10(26.31) 3(18.75)
Absent 08(44.45) 28(73.69) 13(81.25)
Total 18(100) 38(100) 16(100)
DISCUSSION: Traditionally, Maxillo Mandibular fixation (MMF) is the treatment of choice.
Nowadays plating technique is unique treatment modality for open reduction and internal fixation (ORIF).
Merits of MMF:
Low treatment cost.
Short operating time.
Daycare procedure.
Demerits of MMF(5):
Long fixation (3-6 weeks).
Increase airway compromise.
Poor nutrition.
TMJ ankylosis.
Advantages of ORIF:
Earlier mobilization.
Exact bone fragment re-apposition.
Disadvantages:
Well-equipped OT facility.
Increase treatment cost.
Temporary intraosseus wiring was done in most of the cases in our study before application of miniplate fixation. Intraosseus wiring alone did not always give rigid fixation per operatively in unstable and comminuted fractures. In our study 72 cases of mandibular fracture were divided into three groups. Group - A includes 18 cases, treated by interosseous wiring and post-operative maxillo- mandibular immobilization with arch bars and rubber bands for 4 weeks. Group B Includes 38 cases treated with miniplates and no post-operative immobilization.
Group C, 11 cases treated with reconstruction plates and bone graft along with miniplates in patients having bone loss or gap fracture.
Surgical outcome based on clinical and radiological findings were analysed. The parameters such as malocclusion, intraoral exposure of plate, wound dehiscense, delayed union, plate fracture, non-union and neurosensory deficit were compared among the three groups at 4-6 weeks following operation and patients were followed up every 3 months interval. Statistical analysis was done to find out significant result of three modes of treatment. It is found that use of miniplates for mandibular fracture gives excellent result over intraosseus wiring as it has high adaptability, minimal mass effect and relatively strong holding power of two point fixation to allow earlier mobilization.(6,7) Miniplate osteosynthesis also prevents poor nutrition and avoids TMJ
ankylosis.
CONCLUSION: ORIF is the treatment of choice for displaced, comminuted and multiple fractures of mandible.
Rigid internal fixation by monocortical miniplate osteosynthesis provides good long term results and satisfactory cosmesis without any significant sequela.
Reconstruction plates and bone graft along with miniplate is reserved for patients having bone loss or gap fracture.
REFERENCES:
1. Beirne JCB, Bradj F, Ryan D et al. Changing trends in mandibular fractures treated at the national maxillofacial unit Dublin. J. of Irish College of surg. & phys 1995; 24: 177-8.
2. Zide MF, Kent JN. Indications for open reduction of mandibular condylar fractures. Journal of Oral & Maxillofacial Surgery, 1983; 41: 89-98.
3. Champy M, Lodd e JP, Schmitt R, Jaeger JH, Muster D. Mandibular Osteosynthesis by miniature screwed plates via a buccal approach. Journal of Maxillo Facial Surgery, 1978; 6: 14-21.
4. Ellis 3rd E. Treatment Methods for fractures of mandibular angle, International Journal of
Oral & Maxillo facial Surgery, 1999; 28: 243-52.
5. William JG, Cowood JI. Effect of intermaxillary fixation on pulmonary function. J.Oral maxillofac surg. 1990: 19.76.
6. Cowood JI, Small plate osteosynthesis of mandibular fractures. Br. J. oral maxillofac surg. 1985; 23: 77-91.
7. Shivani Jain, Shipra Gupta- Titanium Miniplate versus Intraosseus Wires as methods of fixation of Mandibular Fractures: A Clinical Study, Indian J Stomatol 2011; 2(4): 238-44.
5. Post Graduate Tutor, Department of Dental, GNIDSR.
6. Post Graduate Tutor, Department of Dental, AMDC.
NAME ADDRESS EMAIL ID OF THE CORRESPONDING AUTHOR:
Dr. Asok Kumar Saha,
‘Krishnanagar Bhawan’,
323, Nabapathy, Sector IV, Saltlake, Nowbhanga, Kolkata-700105.
E-mail: dr.asoksaha@gmail.com
Date of Submission: 22/07/2015. Date of Peer Review: 23/07/2015. Date of Acceptance: 28/07/2015. Date of Publishing: 04/08/2015.
AUTHORS:
1. Asok Kumar Saha 2. Siddhartha Das 3. Prasanna Datta 4. Arup Chakrabarty 5. Anindya Priya Saha 6. Sananda Saha
PARTICULARS OF CONTRIBUTORS:
1. Associate Professor, Department of ENT, MCH.
2. RMO cum Clinical Tutor, Department of ENT, NRSMC.
3. Post Graduate Tutor, Department of ENT, MCH,