SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Original
Article
Outcomes
of
non-arthroplasty
surgical
treatment
of
proximal
humeral
head
fractures
夽
Alberto
Naoki
Miyazaki,
Pedro
Doneux
Santos,
Guilherme
do
Val
Sella
∗,
Denis
Cabral
Duarte,
Giovanni
Di
Giunta,
Sergio
Luiz
Checchia
IrmandadedaSantaCasadeMisericórdiadeSãoPaulo,FaculdadedeCiênciasMédicasdaSantaCasadeSãoPaulo, DepartamentodeOrtopediaeTraumatologia,SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received3September2015 Accepted3December2015 Availableonline20August2016
Keywords:
Epiphyses/injuries Fracturefixation,internal Shoulderfractures/surgery Shoulder/surgery
Treatmentoutcome Adult
a
b
s
t
r
a
c
t
Objective:Thisstudyaimedtoassesstheoutcomesofpatientswithhumeralheadfractures treatedbyreductionandosteosynthesis.
Method:Atotalof53shoulders(52patients)withhumeralheadfractureswereoperated betweenOctober1996andDecember2009.Patientspreviouslytreatedwithprimary arthro-plastyand/orthosewhohadlessthantwoyearsfollow-upwereexcluded.Atotalof34 shouldersof34patientswerethereforereassessed.Inthesamplestudied,23patientswere maleandmeanagewas47years.CaseswereassessedbasedontheUCLAscore.
Results:Meanpost-operativefollow-upwas50months.Twelvepatientsevolvedwith excel-lentoutcome,sevengood,fiveregular,andtenwithpooroutcome(55.8%satisfactoryand 44.2%unsatisfactoryoutcomes).MeanUCLAscorewas26points.Meanpost-operativerange ofmotionmeasurementswas117◦
elevation,36◦
LRandL1MR.Attheimmediate post-operativeradiography,anatomicreductionwasevidentin17patients(50%).Necrosiswas detectedin18patients,sixGradeIIand12GradeIIIcases.Femalegenderandanatomically reducedfractureswerestatisticallybetteratUCLAscale(p=0.01andp=0.0001respectively).
Conclusions: FemalepatientshadahighermeanUCLAscorethanmalepatients(p=0.01). AnatomicallyreducedfractureshadhigherUCLAscores(p=0.0001)andlowernecrosisrate (p=0.0001).Reconstructionofhumeralheadfractureshadasatisfactoryoutcomein55.8% ofcasesandshouldbeindicatedinyoungandactivepatients.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http://
creativecommons.org/licenses/by-nc-nd/4.0/).
夽
StudyconductedattheShoulderandElbowGroup,DepartmentofOrthopedicsandTraumatology,Irmandade daSantaCasade MisericórdiadeSãoPaulo,FaculdadedeCiênciasMédicasdaSantaCasadeSãoPaulo,SãoPaulo,SP,Brazil.
∗ Correspondingauthor.
E-mail:gvsella@gmail.com(G.V.Sella).
http://dx.doi.org/10.1016/j.rboe.2016.08.011
epífise
proximal
do
úmero
Palavras-chave:
Epifises/lesões
Fixac¸ãointernadefraturas Fraturasdoombro/cirurgia Ombro/cirurgia
Resultadodotratamento Adulto
r
e
s
u
m
o
Objetivo: Avaliarosresultadosdospacientescomfraturasepifisáriastratadoscomreduc¸ão eosteossíntese.
Método:Entreoutubrode1996edezembrode2009foramoperados53ombros(52pacientes) comfraturasepifisárias.Foramexcluídosospacientestratadoscomartroplastiaprimária e/ou quetinham seguimentoinferiora doisanos. Foramreavaliados 34 ombros de 34 pacientes,23dosexomasculino,commédiade47anos.Aavaliac¸ãofoifeitacomaescala daUCLA.
Resultados: Otempodeseguimentopós-operatóriomédiofoide50meses.Dozepacientes evoluíramcomresultadosexcelentes,setebons,cincoregularesedezmaus(55,8%de result-adossatisfatóriose44,2%deinsatisfatórios).OescoreUCLAtevemédiade26pontos.As médiasdemobilidadepós-operatóriaforamde117◦deelevac¸ão,36◦deRLeL1deRM.NoRX
pós-operatórioimediato,verificamosareduc¸ãoanatômicaem17pacientes(50%).Anecrose foiconstatadaem18pacientes,seisgrauIIe12grauIII.Sexofemininoefraturasreduzidas anatomicamenteforamestatisticamentemelhoresnaescaladaUCLA(p=0,01ep=0,0001 respectivamente).
Conclusões: OsexofemininoteveumvalormédiodoUCLAsuperioraosexomasculino (p=0,01). AsfraturasreduzidasanatomicamenteobtiveramUCLAsuperior(p=0,0001)e ummenoríndicedenecrose(p=0,0001).Areconstruc¸ãodasfraturasepifisáriaslevoua resultadossatisfatóriosem55,8%,deveserindicadaparapacientesjovenseativos.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http://
creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Proximalhumeral headfractures (PHHF)are rare andtheir treatmentisalwaysachallengefortheorthopedicsurgeon, duetothecomplexityofthefracturelinesandhigh complica-tionrates.1–4
Neer3 considers them as part of the group of
fracture-dislocations,because asurfaceofthe articularfragment is compressedorfragmentedagainsttheglenoidcavityandthe restisincongruentwithit.Hesubdividedfracture-dislocations intotwotypes:impactionandthosewithanepiphysealline.3,5
Inthefirst,impaction,thearticularsurfacesinksdueto com-pressionofthehumeralheadagainsttheedgeoftheglenoidat thetimeofdislocation,regardlessofdirection:anterior (Hill-Sachslesion)orposterior(MacLaughlinlesion).3Thesecond
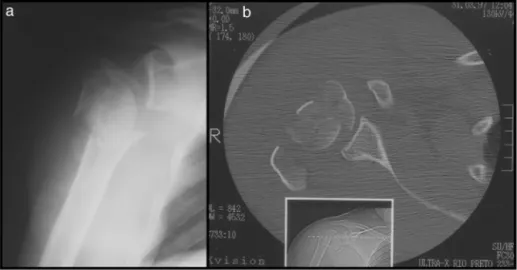
type are the head fractures of the humerus with epiphy-sealline(epiphysealfractures),causedbytheimpactofthe humeral headagainst the glenoid cavity, which fragments the articularsurface (Fig. 1).3 These are usuallyassociated
withthree-andfour-partfractures,arerelatedtohigh-energy trauma,andusuallyoccurinyoungpatients.2,3,6,7 Theyare
characterizedby great involvementof blood supply to the humeralheadanditsfragments;therefore,theyoftenevolve intonecrosis.3
Gerber et al.8 included epiphyseal fractures in the set
ofcomplex fractures, defining them as fractures inwhich thecephalicsegmentishighlyoffset,withgreatlyimpaired vascularization, presenting a higher risk of osteonecrosis and collapse of the humeral head. In addition to epi-physeal fractures, this group includes two-part fractures
of the anatomical neck and three- and four-part fracture-dislocations.7
Therearesomereportsintheliteratureofisolatedcases inwhichtheauthorscommentontherarityoftheinjury.6,9
Chesseretal.2describedeightpatientswithepiphyseal
frac-ture,threeofwhomunderwentopenreductionandinternal fixation (ORIF). Gerber et al.7 treated 32 complex fractures
usingORIF;onlytwowereclassifiedasepiphyseal,whichhad agoodoutcome.
Someauthorsindicatehemiarthroplastyasthetreatment ofchoiceforepiphysealfractures,duetotechnicaldifficulties inachievingananatomicreconstructionoftheboneandof maintainingsuchreconstructionthroughosteosynthesis. Fur-thermore,ORIFinthiskindoffractureprogresseswithhigh complicationrates,includingmalunion,pseudarthrosis,and osteonecrosis.1,3,5,10–14Hemiarthroplastyleadstosatisfactory
resultstothepatientregardingpainimprovement,butusually thereislossofliftingstrengthanddecreasedrangeofmotion, i.e.,itisobservedthatthefunctionaloutcomeofarthroplasties forthetreatmentoffracturesisgenerallyunsatisfactory.10,15
Thisstudyaimedtoevaluatetheresultsofpatientstreated withORIFofthePHHF.
Methods
Fig.1–Case4–epiphysealfractureoftheproximalthirdoftherighthumerusintofourparts:frontalradiograph(a)and computedaxialtomography(b).
fractures.Theinclusioncriteriacomprisedalladultpatients undergoing non-arthroplasty surgical treatment of proxi-malhumerus fractures classified as epiphyseal, who were followed-up for at least two years in the postoperative period.Patients withepiphyseal fracturestreated with pri-maryarthroplastyand/orthosewithlessthantwoyearsof follow-upwereexcluded.Primaryarthroplastywasindicated forpatientswhowereconsideredtobelessactiveandinthose caseswherereconstructionsurgerywasnotpossibleduring theprocedure,whichpreventeditsfixation.Thus,34 shoul-dersof34patientswerereassessed.
Ofthepatients,23weremale(67.6%)and11female(32.4%), withameanageof47years(range:24–77;Table1),and35.3% ofpatientswereyoungerthan40years.Thedominantlimb wasaffectedin15cases(44.1%).
Trauma mechanisms were: falling to the ground in 14 (41.3%),automobileaccidentinseven(20.6%),motorcycle acci-dentinsix(17.6%),fallfromheightinfour(11.7%),andbeing runoverinthree(8.8%;Table1).
Twopatients(cases8and15)had,inadditiontothe frac-ture,neurologicaldamagetotheaffectedlimb.
In all patients, “trauma series radiographs” (corrected frontal,axillary profile,and scapulaprofile) were made for fracture classification.4–16 Computed tomography was
per-formed in cases where there was doubt as to fracture classification(27patients).Allfracturesaffectedthearticular
surfaceofthe humeralhead:infour cases(11.8%)the epi-physealfracturewasassociatedwithfractureofanatomical neckintwoparts;in12cases(35.2%),inthreeparts;andin18 cases(53%),infourparts,accordingtotheNeer3classification
(Table1).
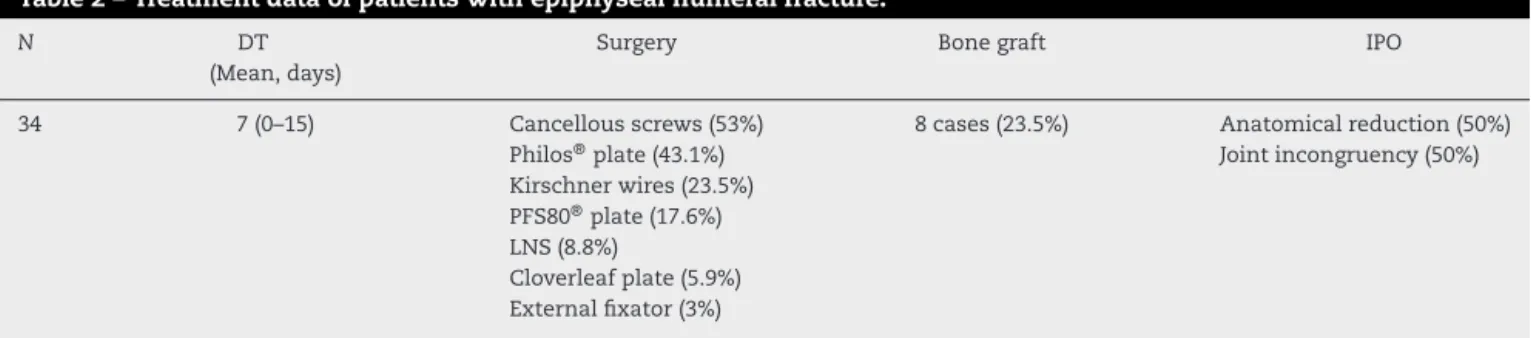
Themeanintervalbetweentraumaandsurgerywasseven days, ranging from zero to 15 days (Table 2); in 55.8% of patients,thisintervalwaslessthanoneweek.
ThechosensurgicaltreatmentmethodwasORIF,through thedeltopectoralapproach,choosingtheleasttraumatic sur-gicaltechniquepossible.Fixationmethodsvariedaccordingto thetypeoffractureandthematerialavailableatthetimeof theprocedure,asspecifiedinTable2.PFS-80®plates,5external
fixators,cloverleafplate,Kirschnerwires,Philos®plate,
liga-turewithanon-absorbablesuture(Ethibond®),andcancellous
screws.Insomeprocedures,morethanonefixationmethod wasused.ThePhilos®platewasusedin14patients(43.1%)
(Table2).
Autologouscancellousbonefromtheiliaccrestwasused asnecessary,accordingtothecomminution,ineightpatients, whichcorrespondsto23.5%ofthecases(Table2).
Shoulder mobility was measured by a goniometer. The parametersoftheAmericanAcademyofOrthopedicSurgeons (AAOS)wereused.17Resultswereassessedbythepoints
sys-temestablishedbytheUniversityofCaliforniaatLosAngeles (UCLA),proposedbyEllmanandKay.18TheFicatandEnneking
Table1–Epidemiologicaldataofpatientswithepiphysealhumeralfracture.
N Age
(Mean,years)
Sex Trauma Fracture
34 47(24–77) M(67.6%) Falltotheground(41.3%) 4Pft-dispost(11.8%) F(32.4%) Caraccident(20.6%) 4P(41.2%)
Motorcycleaccident(17.6%) 3P(35.2%) Fallfromheight(11.7%) 2P(11.8%) Beingrunover(8.8%)
Source:MedicalrecordsoftheHospital.
N DT (Mean,days)
Surgery Bonegraft IPO
34 7(0–15) Cancellousscrews(53%) 8cases(23.5%) Anatomicalreduction(50%) Philos®plate(43.1%) Jointincongruency(50%) Kirschnerwires(23.5%)
PFS80®plate(17.6%) LNS(8.8%)
Cloverleafplate(5.9%) Externalfixator(3%)
Source:MedicalrecordsoftheHospital.
N,numberofcases;DT,timeintervalbetweenthefractureandthetreatment;LNS,stitchingwithanon-absorbablesuture;IPO,immediate postoperativeperiod.
Table3–Resultsofpatientstreatedforepiphysealfractureoftheproximalhumerus.
N Meanfollow-up(months) ROM(mean) Necrosis UCLA(mean)
34 50(24–156) E117◦(50◦to160◦) Absence(16pts,47.1%) 26(9–35) LR36◦(−20◦to70◦) Grade1(0)
MRL1(T5toTroc) Grade2(6pts,17.6%) Grade3(12pts,35.3%)
Source:MedicalrecordsoftheHospital.
N,numberofcases;ROM,rangeofmotion;E◦,elevationindegrees;LR◦,lateralrotationindegrees;MR,medialrotation;Troc,trochanteric;pts, patients.
classification,modifiedbyNeer,wasalsousedforthe evalua-tionofhumeralheadosteonecrosiswhenpresent.19
TheMinitabversion16.0softwarewasusedforstatistical analysis. Thenonparametric Mann–Whitney test was used toevaluate the followingvariables: gender, age (≤40 years
or>40years),dominantside,timeintervalbetweenthedate oftraumaandsurgery(t),typeoffracture,osteosynthesis method, use of graft, immediatepostoperative radiograph, andthepresenceorabsenceofhumeralheadosteonecrosisin thefinalradiograph,comparedtotheendresultoftreatment, withp≤0.05.
Thisstudywas assessedandapprovedbythehospital’s ResearchEthicsCommittee.
Results
Minimumpostoperativefollow-uptimewas24monthsand maximumwas156months,withameanof50months.Twelve patientshadexcellentresults;seven,good;five,regular;and ten, poor. Therefore, 55.8% of the resultswere considered satisfactory (excellent and good) and 44.2%,unsatisfactory (regularandpoor).MeanUCLAscorewas26points;thelowest valuewas9andthehighestvalue,35(Table3).
Meanpostoperativemobilitymeasureswere117◦elevation
(50◦to160◦),36◦lateralrotation(
−20◦to70◦),andlumbar
ver-tebra(L1)inmedialrotation(T5totrochantericregion;Table3). Intheimmediatepostoperativeradiograph,itwasobserved whetherthe reductionofthe fracturewas anatomicalorif therewasjoint incongruity.Anatomicalreductionoccurred in17patients(50%).Inthefinalradiograph,thepresenceof necrosisofthe humeral head wasobserved in18 patients (52.9%),sixclassifiedasgradeIIand12asgradeIII(Table3).
Five cases had complications: twopatients had synthe-sismaterialintheintra-articularspace(cases5and10)and underwentsurgeryforimplantremoval;onepatient(case8) hadneurologicaldamage–iatrogenicneurotmesisofthe axil-larynerve;twopatientsdevelopedinfection(cases13and17). WhentheUCLAvariablewasassessedinrelationtoage (≤40yearsor>40years),nostatisticallysignificantdifference
was observed(p=0.94). Thisdemonstratesthatagedidnot influence the functional outcome of the shoulder inthese patients. The same was observed for the dominant limb (p=0.30), the number ofparts ofthe fracture (p=0.37), the typeoffixation(usingornotusingtheblockedPhilos®plate)
(p=0.87),andtheuseofautologousbonegraft(p=0.56). Inrelationtogender,itwasobservedthatfemaleshada highermeanUCLAthanmales,astatisticallysignificant dif-ference (p=0.01).Patients whosefracture was anatomically reduced,asobservedintheimmediatepostoperative radio-graph,obtainedahigherUCLA(p=0.0001),aswellaspatients whodidnotdevelopnecrosis(p=0.0001).
Forthevariabletimeintervalbetweentraumaandsurgery, adescriptive level(p)equalto0.11wasobserved.Itcanbe concluded that, atthe 5% significancelevel, there was no differenceintheobservedmeanUCLAscores.However,the descriptivelevelwasveryclosetothesignificancelevel, sug-gesting that calculations made with a larger sample may changethisconclusion.
TotestthesignificantlinearcorrelationbetweentheUCLA variablesandthetimebetweentraumaandsurgery(t), Pear-son’s linear correlation coefficient was calculated as 0.340 (p=0.049).Thisindicatesthatthereisadecreasinglinear rela-tionship betweenthese variables,i.e., the greater the time interval,thelowertheUCLAindex.
Table4–Publishedscientificarticles.
CollopyD,SkirvingA.Transcondral fracturedislocationoftheshoulder. JBoneJointSurgBr1995.
Reportofonecase
ChesserTJ,LangdonIJ,OgilvieC, SarangiPP,ClarkeAM.Fractures involvingsplittingofthehumeral headJBoneSurgBr.
Eightcases(onlythree underwentORIF)
GerberC,WernerCML,VienneP. Internalfixationofcomplex fracturesoftheproximalhumerus. JBoneJointSurgBr2004.
32(onlytwo epiphysealfractures)
BailieAG,McAlindenMG.Complex head-splittingfracture-dislocation oftheproximalhumerus successfullytreatedwithminimal internalfixation:acasereportand discussion.Injury2006.
Reportofonecase
asthe dependent variable,and usingas independent vari-ablesgender(1whenthepatientismaleand0whenfemale), elapsedtimeinterval(days),andthepresenceofnecrosis(1 whenitoccurredand0otherwise).
UCLA=39.5−3.72XGender−0.592Xt−11.6XNecrosis
Itisworthmentioningthatthemodelindicatesthatthere isadecrease intheUCLAindexof3.72whenthepatientis male,of0.592foreveryelapsedday,andof11.6whenthereis necrosis.
Discussion
PHHFisanuncommoninjury.1–4 However,Palvanen etal.20
suggestthattheincidenceofproximalhumerusfractureswill tripleinthenext30years.Therearefewpublishedstudiesthat comparetheresultsofORIFofthePHHF.Thepresentstudy included34 patients, the greatest samplefound instudies publishedinrecentyears(Table4).
Theprevalence ofpatients that were considered young observedinthepresentstudy,withameanageof47year-old
(35.3%under 40years), isinagreementwiththatobserved intheliterature,aswellastheprevalenceofmales (67.6%;
Table1).6,7,9WomenhadahighermeanUCLAscore;however,
therearenopublishedstudiestocomparethisfinding.These resultsareprobablyrelatedtothelower-energymechanism ofinjuryinthisgroup,since72.7%ofthewomenexperienced falltotheground,whilethetraumamechanismsinmenwere higher-energy.
Itwasobservedthattheshorterthetimebetweentrauma andsurgery,thebettertheresults.Althoughthisassociation wasnotstatisticallyproven,theanalysissuggeststhatalarger samplewouldbeabletodoso.
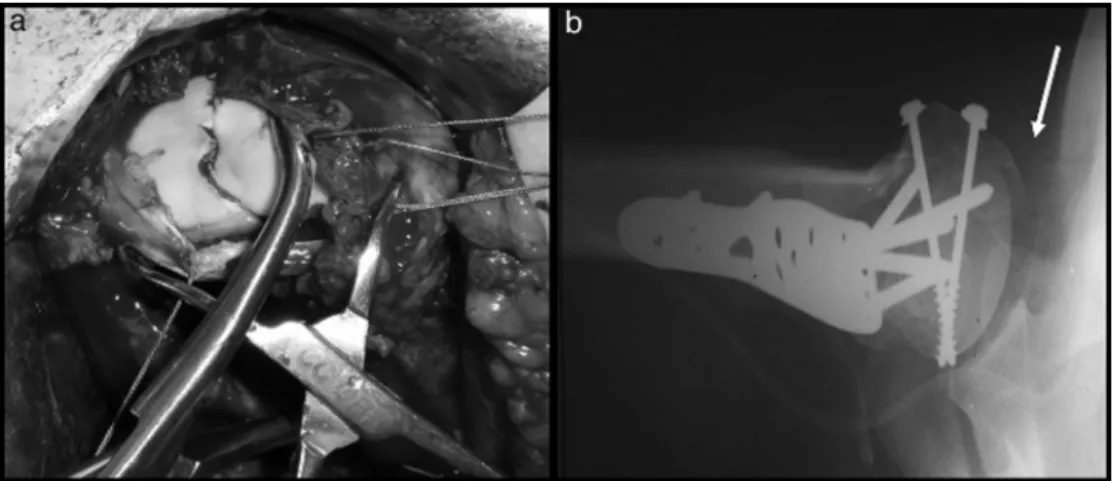
Based on the difficulty of reconstructing the anatomy (Fig.2)andthehighriskofosteonecrosis,hemiarthroplasty isatreatmentoptionforPHHF,butitmustbeborneinmind that these are extremely serious fractures affecting young patients,inwhichthepartialarthroplastywilllikelyleadto worseresults.
With a mean of 63 months offollow-up, Gerber et al.7
describedintheirstudyoncomplexfracturesacaseof epiphy-sealfracturereductionwhichwasnotconsideredanatomical and developed partial osteonecrosis, presenting regular result.
Schaietal.,14 inamulticenterstudyonsevere fractures
ofthehumeralneck,concludedthatthepatient’s ageisan importantfactor inthe choiceoftreatmentand thatthere is a higher probability of humeral head revascularization, throughintramedullaryvesselsandtheiranastomoses,when stable osteosynthesis is used. Gerber et al.8 and Chesser
etal.2advocatetreatmentwithreductionandosteosynthesis,
becauseevenincaseofunfavorabledevelopment,the replace-mentrevisionwouldbetechnicallyeasierthantheprimary hemiarthroplastyifananatomicalreconstructionhad been obtained.
Awidevarietyoffixationmethods(Table2)wereusedin thepresentstudy;choicewasmadeaccordingtothetypeof fractureandthematerialavailableatthetime;themost preva-lentmethodswere thePhilos® plate,usedin14 cases,and
cancellousscrews,usedin18patients.CollopyandSkirving9
usedtwocancellousscrewsasafixationmethod,aswellas BailieandMcAlinden.6 Warneretal.4reportedapreference
Fig.3–Case12–fractureoftheproximalthirdofthelefthumerusinfourparts,impactedinvalguswithepiphysealline: frontalradiographicimageoftheleftshoulder(a)showingtheacutefractureandafterfixation(immediatepost-operative period)withthreadedwiresandstitchingofthegreatertuberosity(b).Consolidatedfracturetwoyearsandsixmonths postoperative,butwithsignsofnecrosisandcollapseofsubchondralboneinthefrontalradiography(c)andaxial T2-weightedMRI(d).Clinicalpictureofpatientwithrangeofmotionof125◦elevation,(e)L1inmedialrotation(f)and10◦ lateralrotation(g).Goodfinalresult(UCLA=29points).
forusingscrews,whethercannulatedornot,forthistypeof fracture.
Nosignificantdifferenceswereobservedbetweenthe syn-thesismaterialusedandthefinalresult.Gerberet al.7 and
Moonot et al.21 support the thesis that a good result can
beobtainedwhen thereisananatomicalreconstructionof thefracture.Inthepresentstudy,fractureswithanatomical reductionevolvedwithgoodandexcellentresults(p=0.0001). Several authors have reported the importance of filling withbone graft the space betweenthe humeralhead and metaphyseal regionthatiscreated duringreductionofthe fracture,duetothelossoftrabecularbonedueto compres-sionofthejointsurfaceatthetimeoftrauma.Thisisdone in an attempt to promote greater bone support and help localrevascularization.22,23Inthepresentstudy,autologous
bonegraft from the iliac crest was used in eightpatients; fiveofthemdevelopedsomedegreeofosteonecrosis. Sim-ilarlytoGerberetal.,7 norelationshipwas observedinthe
presentstudybetweentheuseofbonegraft andthe devel-opment of osteonecrosis. However, there is a bias in the presentstudy,sincebonegraftwasusedformorecomminuted fractures.
Humeral headosteonecrosis is a common complication ofcomplex shoulderfractures, withan incidenceof9% to
75%.3,8,23–25Itspresenceisnotassociatedwithpoorfunctional
outcome,particularlyinpatientswithnecrosisuptogradeII. Thesepatientsmaypresentsatisfactoryclinicalresults, espe-ciallyincaseswheretheanatomyoftheproximalthirdofthe humeruswasrestoredduringsurgery(Fig.3).8,26
Ofthe34 casesinthe presentstudy,18patients(52.9%) developedhumeralheadosteonecrosis,sixclassifiedasgrade IIand12asgradeIII(Table3).Thepresenceofnecrosisalso ledtotherejectionofthehypothesisofequalitybetweenthe mean UCLAscores, which were higherinpatients without necrosis(p=0.0001).
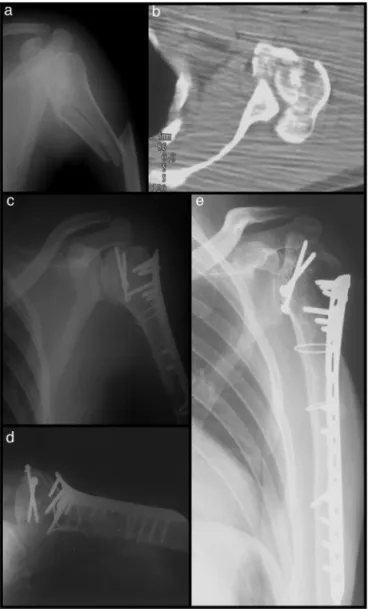
Twopatients(cases8and15)sufferedneurological dam-agethetraumatizedlimbandsomekindofsequelaepersisted during follow-up. Both evolved with unsatisfactory results and osteonecrosisgrade III; this fact may bea biasof the present study when considering the osteonecrosis results. Nerveinjurycontributed,inagreaterorlesserdegree,tothe decreasedshoulderfunction(Fig.4).
Fig.4–Case15–complexfractureoftheleftproximal humeruswithtraumaticbrachialplexusinjury:frontal radiographoftheshoulder(a)andaxialcomputed tomographyimage(b)showingtheepiphysealfracture. Immediatepostoperativeradiographicimageshowingthe double-linesignal(c),inaxillaryprofileshowingthe articularincongruity(d),and18-monthpostoperative radiographshowinggradeIInecrosis(e).Thispatient evolvedwithunsatisfactoryresults(UCLA=18).
Conclusion
ItcanbeconcludedthattheORIFofthePHHFledtogoodand excellentresultsin55.8%ofcases;itshouldbeindicatedin casesofyoungpatientsandactiveadults.
Itwas observed that female gender, shorterinterval of timebetweenthetraumaandsurgery,anatomicalreduction ofthe fractureasobservedinthe immediatepostoperative radiograph, and the absence of osteonecrosis in the post-operative follow-up were factors that influenced the best results.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.BlaineTA,BiglianeLU,LevineWN.Fracturesoftheproximal
humerus.In:RockwoodCA,MatsenFA3rd,WirthMA,Lippitt
SB,editors.Theshoulder.Philadelphia:Saunders;2004.
p.355–412.
2.ChesserTJ,LangdonIJ,OgilvieC,SarangiPP,ClarkeAM.
Fracturesinvolvingsplittingofthehumeralhead.JBoneSurg
Br.2001;83(3):423–6.
3.NeerCS.Displacedproximalhumeralfractures.I.
Classificationandevaluation.JBoneJointSurgAm.
1970;52(6):1077–89.
4.WarnerJJP,CostourosJG,GerberC.Fracturesoftheproximal
humerus.In:RockwoodCA,GreenDP,editors.Fracturesin
adults.Philadelphia:LippincottWilliams&Wilkins;2006.p.
1163–210.
5.NeerCS.Four-segmentclassificationofproximalhumeral
fractures:purposeandreliableuse.JShoulderElbowSurg.
2002;11(4):389–400.
6.BailieAG,McAlindenMG.Complexhead-splitting
fracture-dislocationoftheproximalhumerussuccessfully
treatedwithminimalinternalfixation:acasereportand
discussion.Injury.2006;37(2):82–5.
7.GerberC,WernerCM,VienneP.Internalfixationofcomplex
fracturesoftheproximalhumerus.JBoneJointSurgBr.
2004;86(6):848–55.
8.GerberC,HerscheO,BerberatC.Theclinicalrelevanceof
posttraumaticavascularnecrosisofthehumeralhead.J
ShoulderElbowSurg.1998;7(6):586–90.
9.CollopyD,SkirvingA.Transchondralfracturedislocationof
theshoulder.JBoneJointSurgBr.1995;77(6):975–6.
10.CompitoCA,SelfEB,BiglianiLU.Arthroplastyandacute
shouldertrauma.Reasonsforsuccessandfailure.ClinOrthop
RelatRes.1994;307:27–36.
11.MoeckelBH,DinesDM,WarrenRF,AltchekDW.Modular
hemiarthroplastyforfracturesoftheproximalpartofthe
humerus.JBoneJointSurgAm.1992;74(6):884–9.
12.NhoSJ,BrophyRH,BarkerJU,CornellCH,MacGillivrayJD.
Managementofproximalhumeralfracturesbasedoncurrent
literature.JBoneJointSurgAm.2007;89:44–58.
13.PrakashU,McGurtyDW,DentJA.Hemiarthroplastyforsevere
fracturesoftheproximalhumerus.JShoulderElbowSurg.
2002;11(5):428–30.
14.SchaiP,ImhoffA,PreissS.Comminutedhumeralhead
fractures:amulticenteranalysis.JShoulderElbowSurg.
1995;4(5):319–30.
15.ChecchiaSL,SantosPD,MiyazakiAN,FregonezeM,SilvaLA.
Tratamentodasfraturasdoterc¸oproximaldoúmerocoma
próteseparcialEccentra.RevBrasOrtop.2005;40(3):
130–40.
16.ChecchiaSL,SantosPD,MiyazakiAN,FregonezeM,SilvaLA.
Padronizac¸ãodoestudoradiográficodacinturaescapular.Rev
BrasOrtop.1998;33(11):883–8.
17.Jointmotion:methodofmensuringandrecording.Chicago:
AmericanAcademyofOrthopaedicsSurgeons;1965.
18.EllmanH,KaySP.Arthroscopicsubacromialdescompression
forchronicimpingement–twotofiveyearsresults.JBone
JointSurgBr.1991;73(3):395–8.
19.NeerCS.Glenohumeralarthroplasty.In:NeerR,editor.
Shoulderreconstruction.Philadelphia:Saunders;1990.
epidemiologyofproximalhumeralfractures.ClinOrthop
RelatRes.2006;(442):87–92.
21.MoonotP,AshwoodN,HamletM.Earlyresultsfortreatment
ofthree-andfour-partofthefracturesoftheproximal
humerususingthePHILOSplatesystem.JBoneJointSurgBr.
2007;89(9):1206–9.
22.ReschH,BeckE,BayleyI.Reconstructionofthe
valgus-impactedhumeralheadfracture.JShoulderElbow
Surg.1995;4(2):73–80.
23.RussoR,ViscontiV,LombardiLV,CiccarelliM,GiudiceG.The
block-bridgesystem:anewconceptandsurgicaltechniqueto
proximalhumeralfractures.JShoulderElbowSurg.
2008;17(1):29–36.
24.ReschH,ProvaczP,FrohlichR,WambacherM.Percutaneous
fixationofthree-andfour-partfracturesoftheproximal
humerus.JBoneJointSurgBr.1997;79(2):295–300.
25.SturzeneggerM,FornaroE,JakobRP.Resultofsurgical
treatmentofmultifragmentedfracturesofthehumeralhead.
ArchOrthopTraumaSurg.1982;100(4):249–59.
26.LeeCK,HansenHR.Post-traumaticavascularnecrosisofthe
humeralheadindisplacedproximalhumeralfracture.J