Knowledge, attitudes and
practices on tuberculosis in
prisons and public health
services
Conhecimento, atitudes e práticas
sobre tuberculose em prisões e no
serviço público de saúde
Sérgio Ferreira Júnior
IHelenice Bosco de Oliveira
IILetícia Marin-Léon
III City of Hortolândia Department of Health, São Paulo, Brazil
II Department of Preventive and Social Medicine, State University of Campinas, São Paulo, Brazil
Corresponding author: Helenice Bosco de Oliveira. Rua Waldyr Aparecido da Silva, 60, Resi-dencial II – Condomínio Barão do Café, Barão Geraldo, Campinas, SP, Brazil, 13085-065. e-mail: helenice@unicamp.br
Abstract
There are few studies about tuberculosis (TB) knowledge among prisoners, peni-tentiary system workers and public health network (PRN). Those carried with other populations, point out that the lack of kno-wledge about the illness is one of the main barriers to the perception of the symptoms, early diagnosis, treatment adherence and cure. Objective: To analyze the knowled-ge, attitudes and practices about TB in a prison and in public health services (PHS). Methods: A cross sectional study was car-ried out and KAP (knowledge, attitudes and practices) questionnaire was applied to 141 prisoners, 115 prison’s employees and 158 PHS workers. Epi-Info version 6.04 was used for comparison of proportions with statistic significance at p < 0.05. Results: Mistaken concepts on TB were observed among the three searched groups. PHS also showed basic errors on TB knowledge thus pointing out imperfections on training. Conclusion: KAP revealed efficient for data collection of general knowledge items but was limited on practices and attitudes and so its use as the only tool for data collection about knowledge, attitudes and practices on TB is not advisable. It is suggested its regular use to aid educational activities and con-sidering the high prevalence of TB among prisoners, it is noted the need to involve the Departments of Health in the supervision of educational activities in the prison system.
Resumo
São poucos os estudos sobre o conhecimen-to da tuberculose (TB) entre os detenconhecimen-tos, trabalhadores do sistema penitenciário e da rede pública de saúde (RPS), e aqueles realizados com outras populações apontam a falta do conhecimento sobre a doença como uma das principais barreiras para a percepção dos sintomas, diagnóstico
preco-ce, adesão ao tratamento e cura. Objetivo:
Analisar o conhecimento, atitudes e práticas sobre a TB em uma unidade prisional e na
rede pública de saúde (RPS). Metodologia:
Foi realizado estudo transversal com
apli-cação do questionário KAP (knowledge,
atittudes and practices) na coleta de dados. Participaram 141 detentos, 115 funcioná-rios do presídio e 158 da RPS. O programa Epi-Info versão 6.04 foi utilizado para com-paração de proporções com significância
estatística para p < 0,05. Resultados: Foram
observados conceitos equivocados sobre a doença entre os três grupos pesquisados. Na RPS foram detectados erros básicos sobre o conhecimento da TB, concluindo-se que há falhas nos treinamentos. O KAP mostrou-se eficaz na coleta de dados gerais sobre co-nhecimento, porém foi limitado e frágil nas informações sobre práticas e atitudes, não sendo aconselhável a sua utilização como instrumento único na coleta de dados sobre conhecimento, práticas e atitudes em TB. É sugerida sua utilização periódica como auxiliar nas atividades educativas e, consi-derando a elevada prevalência de TB entre detentos, aponta-se para a necessidade do envolvimento das Secretarias de Saúde na supervisão destas atividades educativas no sistema prisional
Palavras-chave: Tuberculose. Prisões. KAP. Conhecimento. Atitudes. Práticas. Serviço Público de Saúde.
Introduction
Confined populations, especially those comprised of incarcerated individuals, re-present a serious problem in the control of infectious and contagious diseases, such
as tuberculosis (TB) and AIDS.1 Even when
surrounded by prison walls, these individu-als are never entirely isolated from society. Bonds with the outside world continue through contact with both visitors and prison workers. Inmates also inter-relate with the community in general through releases to work, granted leaves, escapes and return to society when sentences have been served. In addition, prison workers maintain contact with their own families and the community
in general,2 and this represents a double risk
of contamination. In other words, an uncon-trolled epidemic of TB in a prison facility may represent a serious risk to individuals and to society at large. In the opposite direction, TB brought in from the outside community
can trigger off an epidemic among inmates.3
Moreover, rules related to prison envi-ronments influence the relationship of TB patients with this disease. In this regard, TB
can affect the social4 interaction between
individuals with TB and other inmates, thus reducing awareness of the seriousness of its symptoms.
Among both the general population and incarcerated groups, TB is a topic that is not easily discussed nowadays. It is associated with poverty, isolation, social exclusion, irre-gular and immoral behavior, as well as with social depravation. These values are strongly
present in the stigmatization of TB patients.5-8
Currently, treatment is usually conducted in outpatient clinics, where health workers are exposed to infection. For this reason, and due to these individuals’ vulnerability, it is essential that they have considerable
knowledge about the disease.9
early diagnosis, adhesion to treatment, and cure.10,11
The KAP (Knowledge, Attitudes and
Practices) Questionnaire12 has been used
for gathering data on knowledge, attitudes and practices about many different health
problems and diseases13 in terms of what
is known, believed and done about specific topics. This instrument was constructed in the 1950s and it was originally designed to estimate resistance against the idea of family
planning among different populations.13
KAP-TB surveys can be especially desig-ned to gather information on topics related to TB. This may include questions about general health practices and beliefs regarding the disease. The purpose is often to identify knowledge, patterns of gaps, and cultural or behavioral beliefs that facilitate understan-ding and action. They can also detect proble-ms, barriers and obstacles that arise with the
efforts to control TB.14 Data can be analyzed
quantitatively or qualitatively, depending on
the study objectives.12
The use of this instrument has fostered a certain amount of social mobilization as well as investigations of the knowledge, practices and attitudes about TB in the population. Some of these studies have been conducted in the context of control programs in different countries with high rates of occurrence of this disease, aiming to strengthen interventions
for behavioral changes.12 One increasingly
important use of the KAP Questionnaire has been to provide essential data on the impact of activities related to advocacy, communica-tion and social mobilizacommunica-tion (ACSM).
The present study was based on the as-sumption that, due to their access to training programs, public health workers and prison workers would have adequate knowledge about TB. The study was thus specifically designed to compare knowledge, attitudes and practices about TB among three distinct groups, namely, inmates, prison workers, and public health workers.
Methodology
A cross-sectional study was carried out on
a sample consisting of inmates and workers of P-III Penitentiary which is a closed prison, and public health workers, in the city of Hortolândia, State of São Paulo, Brazil. This penitentiary was selected because it had had no participants in any projects involving educational intervention for TB.
It was not possible to obtain a statistically valid sample of inmates due to the peniten-tiary conditions and security requirements. The inmates were chosen at random, ac-cording to the routine and the institution’s criteria for transferring them to a meeting room. Participants from among the pri-son employees and public health workers were selected on the basis of their own interest.
An adapted semi-structured version of
the KAP Questionnaire12 was designed and
applied. It consisted of closed questions organized into four sections dealing with the socio-demographic situation of respon-dents and the following aspects related to TB: history of the patient’s disease, knowledge, behavior toward the possibility of contracting TB, and attitudes toward patients with TB. The adapted questionnaire was pre-tested in the PI Penitentiary, located in the same complex.
The instrument was applied indivi-dually by an interviewer to both inmates and prison workers. The questionnaire for health workers was distributed to all pro-fessionals working at the selected public health units and each participant filled it out individually.
Ethical Issues
Prior to application, the present rese-arch project was authorized by the State of São Paulo Department of Penitentiary Administration and by the City of Hortolândia Department of Health and approved by the Research Ethics Committee of the State University at Campinas, under official expert opinion 942/2009 of the National Board of Health Research Ethics Committee, pursuant to Resolution 196/96. All participants signed an informed consent form and confidentiality of information was guaranteed.
Authors declared there were no conflicts of interest.
Results
At the time of the application of the questionnaire, 233 prison workers were as-signed to the PIII Penitentiary. Of these, 88 were on leaves of absence for medical rea-sons, temporary transferences, vacations or bonus leaves. A total of 115 were interviewed (79.3% of those 145 actively working). According to prison authorities, 1,153 male inmates were under detention at the time, 141 (12.2%) of whom were interviewed. For security reasons, the data collected from inmates had to be discontinued.
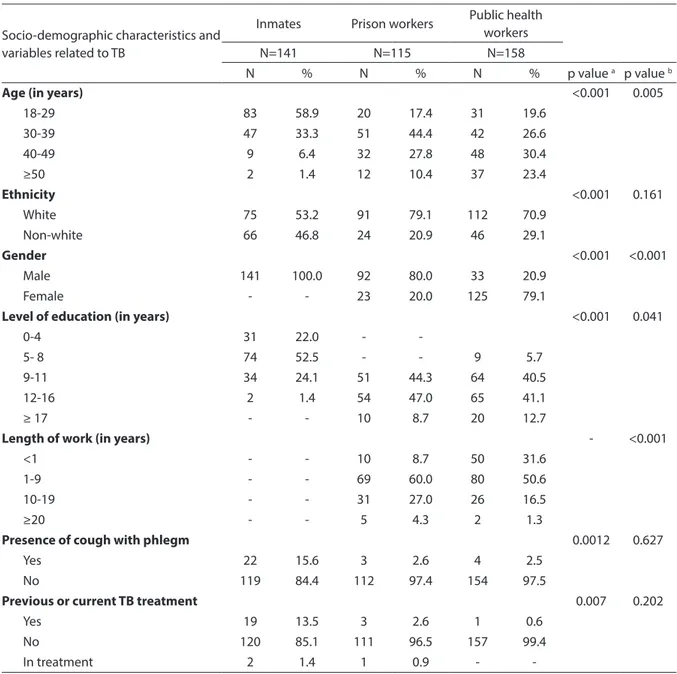
According to the Department of Human Resources, there were 1,216 active workers in the Department of Health at the time of the survey. Of these, 208 were on leaves of absence and 158 of the 508 (31.1%) working in the participating units were interviewed. Emergency units, the municipal hospital, and the adult and child mental health outpa-tient clinics were not included in this study. The respondents in one group of 35 inmates (24.8%) stated that their last arrest had been less than one year before, while 11 (7.8%) reported that it was more than six years before (data not shown). Table 1 shows that inmates and prison workers were different in terms of age, ethnicity, gender and level of education (p<0.001). Among prison workers and public health workers, differences were related to age,
gender, length of work (p<0.001) and level of education (p = 0.041).
In the investigation of respiratory symp-toms, the inmates had cough with phlegm in a higher proportion than prison workers (15.6% vs. 2.6%, p = 0.0012). A greater per-centage of inmates reported having been treated for TB previously (13.5% vs. 2.6% p = 0.007).
Knowledge about Tuberculosis
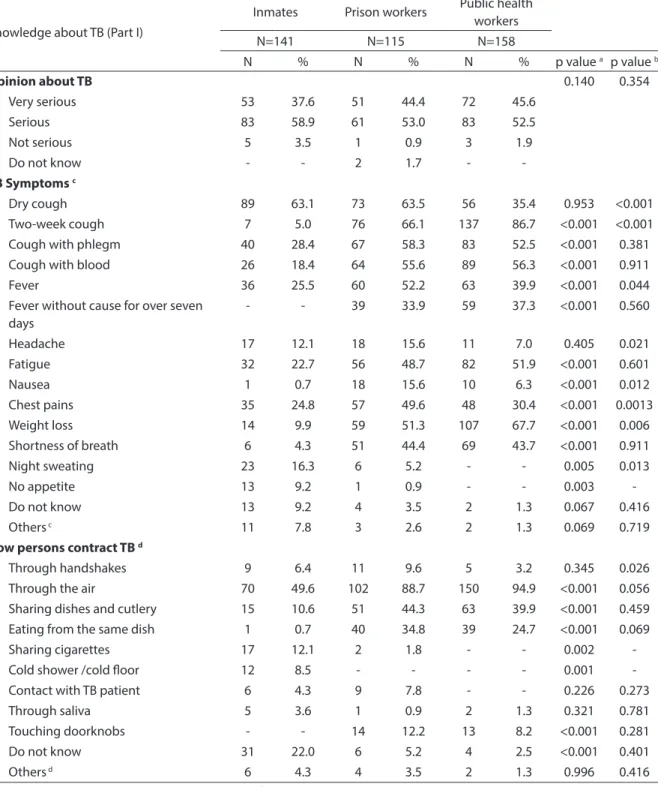
A higher proportion of prison workers than public health workers (63.5% vs. 29.8%, p<0.001) reported they had received information about TB (data not shown). According to Table 2, there were significant differences in knowledge about symptoms between inmates and prison workers, and between prison workers and public health workers. According to the inmates, TB can be transmitted by air (49.6%), by sharing cigarettes (12.1%) and by sharing cutlery (10.6%). Additionally, 22.0% were not awa-re of forms of infection. Prison workers (44.3%) and public health workers (39.9%) mentioned transmission by sharing dishes and cutlery.
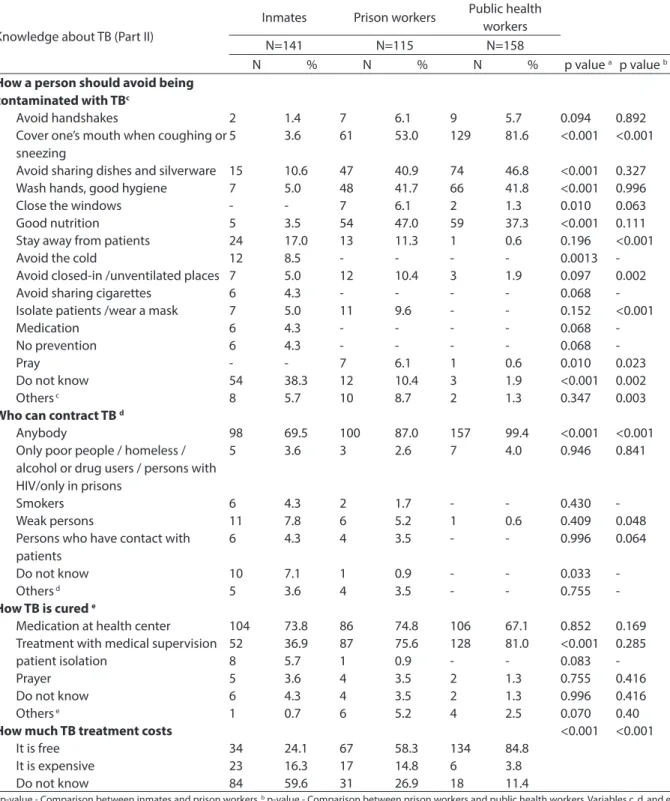
When asked “How can a person avoid
TB?” 38.3% of the inmates did not know the answer. A total of 40.9% of prison workers and 46.8% of public health workers mentio-ned “Do not share dishes or cutlery” as one of their responses (Table 3).
TB was considered a curable disease by all three categories studied. The difference
was found in the item “How to cure TB”,
when the alternative “Treatment with
me-dical supervision” was checked by 36.9% of inmates and 75.6% of prison workers (p<0.001). Only 24.1% of inmates said that the treatment for TB is provided free of char-ge. This same response was given by 58.3% of prison workers and 84.8% (p<0.001) of public health workers (Table 3).
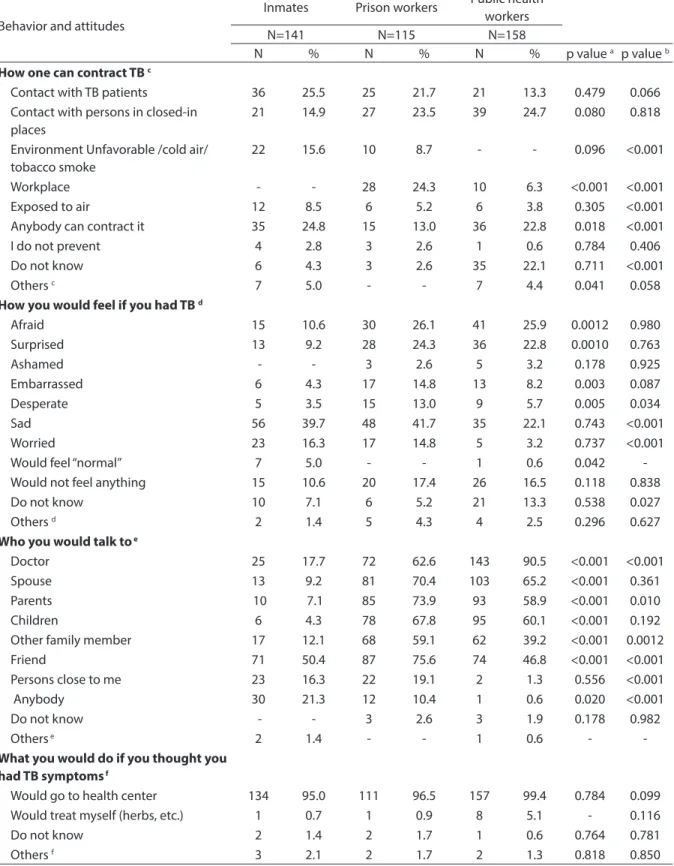
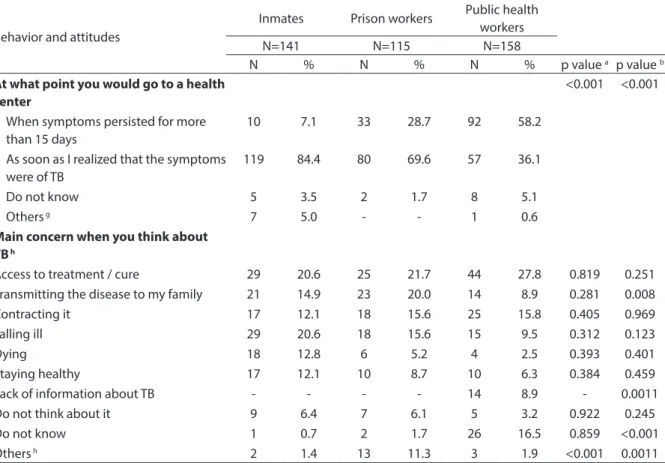
Behavior and attitudes toward the possibility of contracting tuberculosis
to be a factor that increases contamination. In this group, 22.1% could not respond “Because you can catch TB.”
One question in the KAP Questionnaire was “How would you feel if you had TB?” The objective of this question was to investigate feelings aroused by the disease. Many inma-tes answered “sad” (39.7%) and “worried”
(16.3%); while prison workers mentioned “sad” (41.7%) and “afraid” (26%); and health workers, “afraid” (25.9%) and “surprised” (22.8%).
All (100%) inmates and prison workers answered affirmatively when asked if they would talk about the disease, whereas 135 (85.4%) (p<0.001) public health workers
Table 1 - Sociodemographic characteristics and variables related to tuberculosis between prisoners, prisional unit employees and public health workers. Hortolândia, 2010.
Tabela 1 - Características sociodemográicas e variáveis relacionadas à tuberculose entre detentos, funcionários de unidade prisional e rede pública de saúde. Hortolândia, 2010.
Socio-demographic characteristics and variables related to TB
Inmates Prison workers Public health
workers
N=141 N=115 N=158
N % N % N % p value a p value b
Age (in years) <0.001 0.005
18-29 83 58.9 20 17.4 31 19.6
30-39 47 33.3 51 44.4 42 26.6
40-49 9 6.4 32 27.8 48 30.4
≥50 2 1.4 12 10.4 37 23.4
Ethnicity <0.001 0.161
White 75 53.2 91 79.1 112 70.9
Non-white 66 46.8 24 20.9 46 29.1
Gender <0.001 <0.001
Male 141 100.0 92 80.0 33 20.9
Female - - 23 20.0 125 79.1
Level of education (in years) <0.001 0.041
0-4 31 22.0 -
-5- 8 74 52.5 - - 9 5.7
9-11 34 24.1 51 44.3 64 40.5
12-16 2 1.4 54 47.0 65 41.1
≥ 17 - - 10 8.7 20 12.7
Length of work (in years) - <0.001
<1 - - 10 8.7 50 31.6
1-9 - - 69 60.0 80 50.6
10-19 - - 31 27.0 26 16.5
≥20 - - 5 4.3 2 1.3
Presence of cough with phlegm 0.0012 0.627
Yes 22 15.6 3 2.6 4 2.5
No 119 84.4 112 97.4 154 97.5
Previous or current TB treatment 0.007 0.202
Yes 19 13.5 3 2.6 1 0.6
No 120 85.1 111 96.5 157 99.4
In treatment 2 1.4 1 0.9 -
-ap-value - Comparison between inmates and prison workers. bp-value - Comparison between prison workers and public health workers
Table 2 - Knowlwdge about tuberculosis (Part I) between prisoners, prisional unit employees and public health workers. Hortolândia, 2010.
Tabela 2 - Conhecimento sobre a tuberculose (Parte I) entre detentos, funcionários de unidade prisional e rede pública de saúde. Hortolândia, 2010.
Knowledge about TB (Part I)
Inmates Prison workers Public health
workers
N=141 N=115 N=158
N % N % N % p value a p value b
Opinion about TB 0.140 0.354
Very serious 53 37.6 51 44.4 72 45.6
Serious 83 58.9 61 53.0 83 52.5
Not serious 5 3.5 1 0.9 3 1.9
Do not know - - 2 1.7 -
-TB Symptoms c
Dry cough 89 63.1 73 63.5 56 35.4 0.953 <0.001
Two-week cough 7 5.0 76 66.1 137 86.7 <0.001 <0.001
Cough with phlegm 40 28.4 67 58.3 83 52.5 <0.001 0.381
Cough with blood 26 18.4 64 55.6 89 56.3 <0.001 0.911
Fever 36 25.5 60 52.2 63 39.9 <0.001 0.044
Fever without cause for over seven days
- - 39 33.9 59 37.3 <0.001 0.560
Headache 17 12.1 18 15.6 11 7.0 0.405 0.021
Fatigue 32 22.7 56 48.7 82 51.9 <0.001 0.601
Nausea 1 0.7 18 15.6 10 6.3 <0.001 0.012
Chest pains 35 24.8 57 49.6 48 30.4 <0.001 0.0013
Weight loss 14 9.9 59 51.3 107 67.7 <0.001 0.006
Shortness of breath 6 4.3 51 44.4 69 43.7 <0.001 0.911
Night sweating 23 16.3 6 5.2 - - 0.005 0.013
No appetite 13 9.2 1 0.9 - - 0.003
-Do not know 13 9.2 4 3.5 2 1.3 0.067 0.416
Others c 11 7.8 3 2.6 2 1.3 0.069 0.719
How persons contract TB d
Through handshakes 9 6.4 11 9.6 5 3.2 0.345 0.026
Through the air 70 49.6 102 88.7 150 94.9 <0.001 0.056
Sharing dishes and cutlery 15 10.6 51 44.3 63 39.9 <0.001 0.459
Eating from the same dish 1 0.7 40 34.8 39 24.7 <0.001 0.069
Sharing cigarettes 17 12.1 2 1.8 - - 0.002
-Cold shower /cold loor 12 8.5 - - - - 0.001
-Contact with TB patient 6 4.3 9 7.8 - - 0.226 0.273
Through saliva 5 3.6 1 0.9 2 1.3 0.321 0.781
Touching doorknobs - - 14 12.2 13 8.2 <0.001 0.281
Do not know 31 22.0 6 5.2 4 2.5 <0.001 0.401
Others d 6 4.3 4 3.5 2 1.3 0.996 0.416
a p-value - Comparison between inmates and prison workers. b p-value - Comparison between prison workers and public health workers. Variables c and
d allowed for more than one response. Others (c) Diarrhea, abdominal pains, vomiting, flu, dizziness, ganglia, impotence, depression. Others (d) Drug use, kissing, contaminated food
a valor de p - Comparação entre detentos e funcionários do presídio. b valor de p - Comparação entre funcionários do presídio e rede pública de saúde. As variáveis
Table 3 - Knowledge about tuberculosis (Part II) between prisoners, prisional unit employees and public health workers. Hortolândia, 2010.
Tabela 3 - Conhecimento sobre a tuberculose (Parte II) entre detentos, funcionários de unidade prisional e rede pública de saúde. Hortolândia, 2010.
Knowledge about TB (Part II)
Inmates Prison workers Public health
workers
N=141 N=115 N=158
N % N % N % p value a p value b
How a person should avoid being contaminated with TBc
Avoid handshakes 2 1.4 7 6.1 9 5.7 0.094 0.892
Cover one’s mouth when coughing or sneezing
5 3.6 61 53.0 129 81.6 <0.001 <0.001
Avoid sharing dishes and silverware 15 10.6 47 40.9 74 46.8 <0.001 0.327
Wash hands, good hygiene 7 5.0 48 41.7 66 41.8 <0.001 0.996
Close the windows - - 7 6.1 2 1.3 0.010 0.063
Good nutrition 5 3.5 54 47.0 59 37.3 <0.001 0.111
Stay away from patients 24 17.0 13 11.3 1 0.6 0.196 <0.001
Avoid the cold 12 8.5 - - - - 0.0013
-Avoid closed-in /unventilated places 7 5.0 12 10.4 3 1.9 0.097 0.002
Avoid sharing cigarettes 6 4.3 - - - - 0.068
-Isolate patients /wear a mask 7 5.0 11 9.6 - - 0.152 <0.001
Medication 6 4.3 - - - - 0.068
-No prevention 6 4.3 - - - - 0.068
-Pray - - 7 6.1 1 0.6 0.010 0.023
Do not know 54 38.3 12 10.4 3 1.9 <0.001 0.002
Others c 8 5.7 10 8.7 2 1.3 0.347 0.003
Who can contract TB d
Anybody 98 69.5 100 87.0 157 99.4 <0.001 <0.001
Only poor people / homeless / alcohol or drug users / persons with HIV/only in prisons
5 3.6 3 2.6 7 4.0 0.946 0.841
Smokers 6 4.3 2 1.7 - - 0.430
-Weak persons 11 7.8 6 5.2 1 0.6 0.409 0.048
Persons who have contact with patients
6 4.3 4 3.5 - - 0.996 0.064
Do not know 10 7.1 1 0.9 - - 0.033
-Others d 5 3.6 4 3.5 - - 0.755
-How TB is cured e
Medication at health center 104 73.8 86 74.8 106 67.1 0.852 0.169
Treatment with medical supervision 52 36.9 87 75.6 128 81.0 <0.001 0.285
patient isolation 8 5.7 1 0.9 - - 0.083
-Prayer 5 3.6 4 3.5 2 1.3 0.755 0.416
Do not know 6 4.3 4 3.5 2 1.3 0.996 0.416
Others e 1 0.7 6 5.2 4 2.5 0.070 0.40
How much TB treatment costs <0.001 <0.001
It is free 34 24.1 67 58.3 134 84.8
It is expensive 23 16.3 17 14.8 6 3.8
Do not know 84 59.6 31 26.9 18 11.4
a p-value - Comparison between inmates and prison workers. b p-value - Comparison between prison workers and public health workers. Variables c, d, and e
allowed more than one response. Others (c) Avoid alcoholic drinks and cigarettes, avoid dust, be vaccinated, have routine exams /physical activity. Others (d) Who do not need to prevent, seniors, children. Others (e) There is no cure, medicinal herbs, rest, ventilation
a valor de p - Comparação entre detentos e funcionários do presídio. b valor de p - Comparação entre funcionários do presídio e rede pública de saúde. As variáveis c,
Table 4 - Behavior and attitudes between prisoners, prisional unit employees and public health workers in front of the possibility to catch tuberculosis. Hortolândia, 2010.
Tabela 4 - Comportamento e atitudes, diante da possibilidade de contrair a tuberculose, entre detentos e funcionários de unidade prisional e rede pública de saúde. Hortolândia, 2010.
Behavior and attitudes
Inmates Prison workers Public health
workers
N=141 N=115 N=158
N % N % N % p value a p value b
How one can contract TB c
Contact with TB patients 36 25.5 25 21.7 21 13.3 0.479 0.066
Contact with persons in closed-in places
21 14.9 27 23.5 39 24.7 0.080 0.818
Environment Unfavorable /cold air/ tobacco smoke
22 15.6 10 8.7 - - 0.096 <0.001
Workplace - - 28 24.3 10 6.3 <0.001 <0.001
Exposed to air 12 8.5 6 5.2 6 3.8 0.305 <0.001
Anybody can contract it 35 24.8 15 13.0 36 22.8 0.018 <0.001
I do not prevent 4 2.8 3 2.6 1 0.6 0.784 0.406
Do not know 6 4.3 3 2.6 35 22.1 0.711 <0.001
Others c 7 5.0 - - 7 4.4 0.041 0.058
How you would feel if you had TB d
Afraid 15 10.6 30 26.1 41 25.9 0.0012 0.980
Surprised 13 9.2 28 24.3 36 22.8 0.0010 0.763
Ashamed - - 3 2.6 5 3.2 0.178 0.925
Embarrassed 6 4.3 17 14.8 13 8.2 0.003 0.087
Desperate 5 3.5 15 13.0 9 5.7 0.005 0.034
Sad 56 39.7 48 41.7 35 22.1 0.743 <0.001
Worried 23 16.3 17 14.8 5 3.2 0.737 <0.001
Would feel “normal” 7 5.0 - - 1 0.6 0.042
-Would not feel anything 15 10.6 20 17.4 26 16.5 0.118 0.838
Do not know 10 7.1 6 5.2 21 13.3 0.538 0.027
Others d 2 1.4 5 4.3 4 2.5 0.296 0.627
Who you would talk to e
Doctor 25 17.7 72 62.6 143 90.5 <0.001 <0.001
Spouse 13 9.2 81 70.4 103 65.2 <0.001 0.361
Parents 10 7.1 85 73.9 93 58.9 <0.001 0.010
Children 6 4.3 78 67.8 95 60.1 <0.001 0.192
Other family member 17 12.1 68 59.1 62 39.2 <0.001 0.0012
Friend 71 50.4 87 75.6 74 46.8 <0.001 <0.001
Persons close to me 23 16.3 22 19.1 2 1.3 0.556 <0.001
Anybody 30 21.3 12 10.4 1 0.6 0.020 <0.001
Do not know - - 3 2.6 3 1.9 0.178 0.982
Others e 2 1.4 - - 1 0.6 -
-What you would do if you thought you had TB symptoms f
Would go to health center 134 95.0 111 96.5 157 99.4 0.784 0.099
Would treat myself (herbs, etc.) 1 0.7 1 0.9 8 5.1 - 0.116
Do not know 2 1.4 2 1.7 1 0.6 0.764 0.781
gave the same answer (data not shown). The greatest concern about TB among inmates is contracting it and how to obtain treatment and be cured. Death was mentio-ned by 12.8% of respondents in this group.
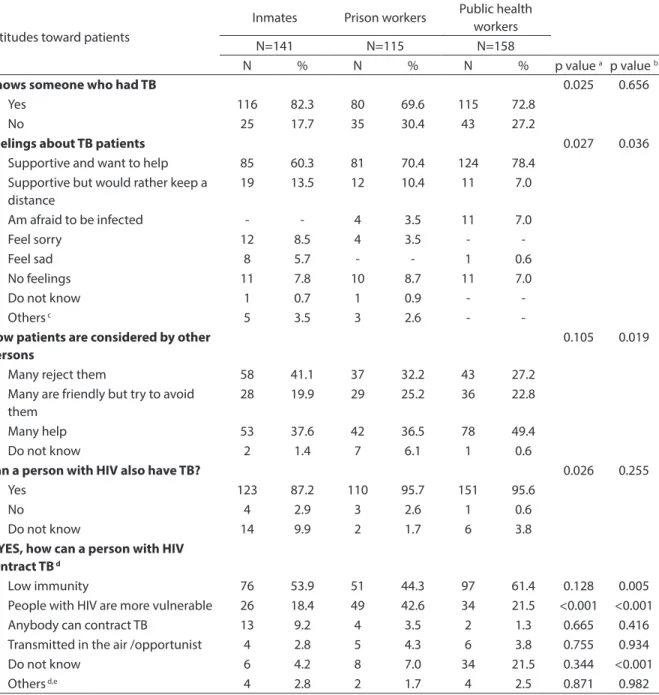
Attitudes regarding tuberculosis patients Regarding the question “How is a TB pa-tient regarded by other persons?” (see Table 5), 41.1% of inmates said that “Many people reject them.” The answer “Many people are friendly but they try to avoid patients,” was given by 25.2% of prison workers and 22.8% of public health workers.
When asked why a person who has HIV may also have tuberculosis, 44.3% of prison workers mentioned low immunity, but this same answer was given by a much greater number of public health workers (61.4%) (p = 0.005). It should be noted that 21.5% of pu-blic health workers said they “Do not know.”
Discussion
Increased drug use is one of the factors that has contributed to the increase in violence in Brazil and, consequently, to the
greater number of incarcerated persons.15
Behavior and attitudes
Inmates Prison workers Public health
workers
N=141 N=115 N=158
N % N % N % p value a p value b
At what point you would go to a health center
<0.001 <0.001
When symptoms persisted for more than 15 days
10 7.1 33 28.7 92 58.2
As soon as I realized that the symptoms were of TB
119 84.4 80 69.6 57 36.1
Do not know 5 3.5 2 1.7 8 5.1
Others g 7 5.0 - - 1 0.6
Main concern when you think about TB h
Access to treatment / cure 29 20.6 25 21.7 44 27.8 0.819 0.251
Transmitting the disease to my family 21 14.9 23 20.0 14 8.9 0.281 0.008
Contracting it 17 12.1 18 15.6 25 15.8 0.405 0.969
Falling ill 29 20.6 18 15.6 15 9.5 0.312 0.123
Dying 18 12.8 6 5.2 4 2.5 0.393 0.401
Staying healthy 17 12.1 10 8.7 10 6.3 0.384 0.459
Lack of information about TB - - - - 14 8.9 - 0.0011
Do not think about it 9 6.4 7 6.1 5 3.2 0.922 0.245
Do not know 1 0.7 2 1.7 26 16.5 0.859 <0.001
Others h 2 1.4 13 11.3 3 1.9 <0.001 0.0011
a p-value - Comparison between inmates and prison workers. b p-value - Comparison between prison workers and public health workers. Variables c, d, f and
h allowed for more than one response. Other (c) I already had TB, took drugs, God might want this. Other (d) I am predestined, I would face it, find treatment. Other (e) I would talk to God, talk with somebody I trust, would not talk to anybody. Other (f ) Would stop smoking, obtain more information, go to a drugsto-re, go to God. Other (g) When self-treatment did not work, when you are weak, would not go to a health center. Other (h) TB-MDR, to be sick and not to know it, isolation, epidemic
a valor de p - Comparação entre detentos e funcionários do presídio. b valor de p - Comparação entre funcionários do presídio e rede pública de saúde. As variáveis c, d, f, h
permitiram mais de uma resposta. Outro (c) Já tive TB, usei drogas, Deus pode querer. Outro (d) Estou predestinado, enfrentaria, procuraria tratamento. Outro (e) Falaria com Deus, falaria com quem confio, não falaria para ninguém. Outro (f) Pararia de fumar, procuraria mais informações, procuraria farmácia, procuraria Deus. Outro (g) Quando tratamento por conta não funcionasse, quando estivesse fraco, não iria ao posto. Outro (h) TB-MDR, estar doente e não saber, isolamento, epidemia.
Table 4 - Behavior and attitudes between prisoners, prisional unit employees and public health workers in front of the possibility to catch tuberculosis. Hortolândia, 2010. (continuation)
Table 5 - Attitudes from prisoners, prisional unit employees and public health workers related to sick people with TB. Hortolândia, 2010.
Tabela 5 - Atitudes em relação a doentes com TB, de detentos e funcionários de unidade prisional e da rede pública de saúde. Hortolândia, 2010.
Attitudes toward patients
Inmates Prison workers Public health
workers
N=141 N=115 N=158
N % N % N % p value a p value b
Knows someone who had TB 0.025 0.656
Yes 116 82.3 80 69.6 115 72.8
No 25 17.7 35 30.4 43 27.2
Feelings about TB patients 0.027 0.036
Supportive and want to help 85 60.3 81 70.4 124 78.4
Supportive but would rather keep a distance
19 13.5 12 10.4 11 7.0
Am afraid to be infected - - 4 3.5 11 7.0
Feel sorry 12 8.5 4 3.5 -
-Feel sad 8 5.7 - - 1 0.6
No feelings 11 7.8 10 8.7 11 7.0
Do not know 1 0.7 1 0.9 -
-Others c 5 3.5 3 2.6 -
-How patients are considered by other persons
0.105 0.019
Many reject them 58 41.1 37 32.2 43 27.2
Many are friendly but try to avoid them
28 19.9 29 25.2 36 22.8
Many help 53 37.6 42 36.5 78 49.4
Do not know 2 1.4 7 6.1 1 0.6
Can a person with HIV also have TB? 0.026 0.255
Yes 123 87.2 110 95.7 151 95.6
No 4 2.9 3 2.6 1 0.6
Do not know 14 9.9 2 1.7 6 3.8
If YES, how can a person with HIV contract TB d
Low immunity 76 53.9 51 44.3 97 61.4 0.128 0.005
People with HIV are more vulnerable 26 18.4 49 42.6 34 21.5 <0.001 <0.001
Anybody can contract TB 13 9.2 4 3.5 2 1.3 0.665 0.416
Transmitted in the air /opportunist 4 2.8 5 4.3 6 3.8 0.755 0.934
Do not know 6 4.2 8 7.0 34 21.5 0.344 <0.001
Others d,e 4 2.8 2 1.7 4 2.5 0.871 0.982
a p-value - Comparison between inmates and prison workers. b p-value - Comparison between prison workers and public health workers. Variable d allowed
for more than one response. Other (c) It is their problem, loss, discrimination, anger. Other (d) I already take the medicine, do nothing to prevent, risk of HIV
a valor de p - Comparação entre detentos e funcionários do presídio. b valor de p - Comparação entre funcionários do presídio e rede pública de saúde. A variá vel d
permitiu mais de uma resposta. Outro (c) É problema deles, perda, discriminação, raiva. Outro (d) Já toma medicamentos, não se previne, risco para HIV.
Inmates come from social classes characte-rized by poverty and difficulties in accessing health services, education and information. Consequently, this population usually has a low level of education, a characteristic also
In this study, 53.2% of the population of inmates was white, similar to the ethnic
proportion found in the city of São Paulo,16
22% having fewer than five years of educa-tion. According to the National Health Plan
for the Penitentiary System,17 the Brazilian
prison population is usually comprised of single white men under the age of 30 years. Few are literate and many had no definite profession before their arrest by the police. This means that the majority were in a si-tuation of social exclusion prior to prison. Therefore, one might consider that the pri-son population studied in Hortolândia has a higher level of formal education than the national Brazilian average, since 78% had at least five years of education.
It is a well-known fact that knowledge can influence people’s practices regarding
prevention.18 Many inmates and prison
workers had not received information about TB and several responses regarding its prevention given in the questionnaire were incorrect, as observed in studies by other
authors.19 This suggests that the forms of
communication and the strategies used to transfer knowledge in prisons fail to attain their objectives. Additionally, it indicates the absence of health education programs in general, particularly those aimed at TB
control, in prison institutions.20
In one study21 on the knowledge of the
Brazilian population about TB, 34% of the respondents reported that they were ac-quainted with someone who had the dise-ase or had previously had it. In the present study, 82.3% of inmates and 69.6% of prison workers also responded affirmatively to this same question. This result suggests that many persons in all three groups are familiar with the disease, at least to some degree. Even so, their knowledge is permeated with un-founded beliefs and mistaken information. Even many public health workers, despite their greater knowledge about TB, made basic conceptual mistakes when asked about vulnerability when sharing objects. Similar results appeared in studies on workers in
the area of nursing9 involved in family health
teams,22 although this information can easily
be found in manuals and guidelines on the Internet and in departments of
epidemio-logic surveillance.23 This fact is indicative of
deficiencies in instructions about TB provi-ded to public health workers. It also shows the serious need to disseminate informa-tion about TB among other professionals, using an interdisciplinary and intersectoral
approach.9,10 Training programs are
impor-tant strategies to increase knowledge and
practices of employees in TB tracking24 and
supervised treatment.25
Many studies that use the KAP Questionnaire fail to present the results obtained about attitudes, due to the risk of falsely generalizing the opinions and feelin-gs of a given population sector. The attempt to measure attitudes and feelings through studies has been criticized for a number of different reasons. One reason is that res-pondents tend to give answers they believe to be correct, acceptable or otherwise con-sidered relevant. More delicate questions are especially vulnerable to this tendency, and the context of an interview can strongly
influence the results.26 This situation was
present during the application of the ques-tionnaire in this study. A vague discomfort could be felt in some participants when asked certain sensitive questions, and they tended to simply respond something they thought to be correct, accepted or apprecia-ted. This behavior, for example, was noted among the inmates and prison workers for the two following questions: “How do you feel about people with TB?” and “How is a person with TB considered by others?” For the first question, the high number of inter-viewees who answered “I feel supportive and want to help,” led researchers to suspect that this was an assertion that the participants believed to be meaningful for the context of the interview, although it might not be reflecting their true attitude. To the second question, inmates answered that “Many are rejected,” while prison workers stated
that “Many people help others.” But some
the questions strange, answered them with what they felt was an appropriate answer at the moment of the interview, even if it did not reflect the truth.
With regard to how they would feel if they were infected with TB, inmates repor-ted they would feel “sad,” but this feeling could be simply associated with their condition of imprisonment and with safety- and survival-related problems, factors that would negatively affect their relationships
with other inmates.4 Prison workers and
public health workers mentioned sadness, surprise and fear. Once again, responses might not have reflected reality, but rather shown the fragility of the instrument for gathering information about attitudes. The feeling of fear is the most common cause of stigma in regard to TB.27 For Ascuntar et al.,28
this feeling is closely related to a complex set of attitudes that could interfere with the interpersonal relationships and increase risky behavior. This, in turn, might suggest the generation of stigma and discrimina-tion, thus limiting access to treatment and reducing adhesion.
Most of the inmates and prison workers expressed confidence in questionable preventive practices regarding TB, such as having good habits of cleanliness, good nutrition, washing one’s hands, avoiding the cold and not sharing dishes and cutlery. Better results from public health workers were expected in terms of their knowledge of forms of prevention, but some mentioned danger of infection from sharing dishes and cutlery. These findings are not clear in terms of what logic should be present in deciding ways to prevent infection, but they do indi-cate deficiencies in the knowledge of these individuals about the clinical and epidemio-logical management of this disease among
the studied groups.13
In regard to attitudes, the act of talking about TB and who they could talk to if they had TB, inmates mentioned the need to notify their cell mates or any other indivi-duals who might listen to them about the possibility of falling ill. This behavior can be explained in view of the fragility that TB
represents in the context of prisons.4 Patients
can put their cell mates at risk, and talking about the disease could lead these cell mates to pressure to have the patients transferred in order to lower the chances of infecting others and speed up access to the prison health service. Prison workers reported that they would talk about the disease to a friend or family member, while public health workers would talk to a doctor and relatives. This difference in findings reflects a relationship between knowledge about TB and access to
health services.18
Another source of uncertainty is that the data obtained from KAP studies are often used to plan activities focused on behavio-ral changes related to certain health issues, based on the false premise that there is a direct relationship between knowledge and behavior. A number of studies have shown that knowledge is only one of the factors that influence practice. Therefore, for there to be changes in behavior, health programs must join socioeconomic, environmental and structural factors with practices when
planning prevention programs.18
Conclusion
In the present study, the use of the KAP questionnaire presented a number of pro-blems, difficulties and drawbacks. It proved to be weak to interpret the data gathered on attitudes, thus hindering the understanding of the information obtained. Therefore, if the objective is to study behavior, practice and attitudes in regard to a given context, combinations of qualitative and quantitative methods would be more indicated.
References
1. Dara M, Grzemska M, Kimerling ME, Reyes H, Zagorskiy A. Guidelines for control of tuberculosis in prisons. Tuberculosis Coalition for Technical Assistance and International Committee of the Red Cross. 2009. Disponível em: http://pdf.usaid.gov/pdf_docs/
PNADP462.pdf. [Accessed in August 18th 2011]
2. Bick JA. Infection control in jail and prisons. Clin Infect
Dis 2007; 45(8): 1047-55.
3. Hanau-Berçot B, Grémy I, Raskine L, Bizet J, Gutierrez MC, Boyer-Mariotte S et al. A one-year prospective study (1994-1995) for a first evaluation of tuberculosis
transmission in French prisons. Int J Tuberc Lung Dis
2000; 4(9): 853-9.
4. Diuana V, Lhullier D, Sánchez AR, Amado G, Araújo L, Duarte AM, et al. Saúde em prisões: representações e práticas dos agentes de segurança penitenciária no Rio
de Janeiro, Brasil. Cad Saúde Pública 2008; 24: 1887-96.
5. Jittimanee XS, Nateniyon S, Kittikraisak W, Burapat C, Akksilp S, Chumpathat N et al. Social stigma and knowledge of tuberculosis and HIV among patients
with both diseases in Thailand. PLoS One 2009; 23: 4(7):
e6360.
6. Baral SC, Karki DK, Newell JN. Causes of stigma and discrimination associated with tuberculosis in Nepal: a
qualitative study. BMC Public Health 2007; 7: 211.
7. Pôrto A. Representações sociais da tuberculose: estigma
e preconceito. Rev Saúde Pública 2007; 41(1): 43-9.
8. Goffman E. Estigma. Notas sobre a manipulação da
identidade deteriorada. 2ªed. Rio de Janeiro: Zahar
Editores; 1978.
9. Souza NJ, Bertolozzi MR. A vulnerabilidade à tuberculose em trabalhadores de enfermagem em um
hospital universitário. Rev Latino-am Enfermagem 2007;
15(2): 259-66.
10. Alvarez-Gordilho GC, Alvarez-Gordilho FJ, Dorantes-Jiménez JE, Halperin-Frish D. Percepciones y prácticas relacionadas com la tuberculosis y la aderência al
tratamiento em Chiapas, México. Salud Pública Méx
2000; 42(6): 520-8.
11. Savicevic AJ, Popovic-Grle S, Milovac S, Ivcevic I, Vukasovic M, Viali V et al. Tuberculosis knowledge among patients in out-patient settings in Split, Croatia.
Int J Tuberc Lung Dis 2008; 12(7): 780-5.
12. World Health Organization. Advocacy, communication
and social mobilization for TB Control. A guide to developing knowledge, attitude and practice surveys. WHO/HTM/STB/2008.46.
13. Launiala A. How much can a KAP survey tell us about people’s knowledge, attitudes and practices? Some observations from medical anthropology research on
malaria in pregnancy in Malawi. Anthropology Matters
2009; 11(1): 1-13.
14. Roy A, Abubakar I, Yates S, Chapman A, Lipman M, Monk P et al. Evaluating knowledge gain from TB leaflets for prison and homeless sector staff: the National
Knowledge Service TB pilot. Eur J Public Health 2008:
18(6): 600-3
15. Brasil. Ministério da Justiça – Execução Penal. Sistema Prisional. Infopen - Estatística. Available in: http://portal.mj.gov.br/data/Pages/ MJD574E9CEITEMIDC37B2AE94C6840068B1624
D28407509CPTBRIE.htm. [Accessed in August 20th 2011].
16. Abrahão RMCM. Diagnóstico da tuberculose na
população carcerária dos Distritos Policiais da zona oeste
da cidade de São Paulo [tese de doutorado]. São Paulo:
Faculdade de Saúde Pública da USP; 2003.
17. Brasil. Ministério da Saúde. Plano Nacional de Saúde no Sistema Penitenciário. Available in: http://bvsms. saude.gov.br/bvs/publicacoes/plano_nacional_saude_
sistema_penitenciario_2ed.pdf. [Accessed in August 20th
2011]
18. Launiala A, Honkasalo ML. Ethnographic study of factors influencing compliance to intermittent preventive treatment of malaria during pregnancy
among Yao women in rural Malawi. Trans R Soc Trop
Med Hyg 2007; 101(10): 980-9.
19. Abebe DS, Biffa D, Bjune G, Ameni G, Abebe F. Assessment of knowledge and practice about
tuberculosis among eastern Ethiopian prisoners. Int J
Tuberc Lung Dis 2011; 15(2): 228-33.
20. Waisbord S. Participatory communication for
tuberculosis control in prisons in Bolivia, Ecuador, and
Paraguay. Rev Panam Salud Publica 2010; 27(3): 168-74.
21. Boaretto MC, Guimarães MTC, Natal S, Castelo Branco AC, Mondarto P, Fernandes MJ et al. The knowledge of
the Brazilian population on tuberculosis. Int J Tuberc
Lung Dis 2010; 14(11): S196.
22. Maciel ELN, Vieira RCA, Milani EC, Brasil M, Fregona G, Dietze R. O agente comunitário de saúde no controle da
tuberculose: conhecimentos e percepções. Cad Saude
Publica 2008; 24(6): 1377-86.
23. Brasil. Ministério da Saúde. Tuberculose - Guia de vigilância epidemiológica, 2005. Available in: http:// www.prosaude.org/publicacoes/guia/Guia_Vig_Epid_
novo2.pdf. [Accessed in April 24th 2011].
Acknowledgements: Project ICOHRTA AIDS/TB-Brazil, for the course held at Johns
24. Naugthon MP, Posey DL, Willacy EA, Comans TW. Tuberculosis training on physicians who perform
immigration medical examination. Int J Tuberc Lung Dis
2010; 14(11): S154.
25. Rao N, Arain I. Knowledge regarding tuberculosis among
TN course participants in Karachi. Int J Tuberc Lung Dis
2010; 14(11): S160.
26. Hausmann-Muela S, Ribera JM, Nyamongo I. Health seeking behavior and the health system response. DCPP Working Paper 2003. Available in: http://www.dcp2.org/
main/Home.html. [Accessed in April 24th 2010].
27. Courtwright A, Turner AN. Tuberculosis and
stigmatization: pathways and interventions. Public
Health Rep 2010; 125(4): 34-42.
28. Ascuntar JM, Gaviria MB, Uribe L, Ochoa J. Fear, infection and compassion: social representations of
tuberculosis in Medellin, Colombia, 2007. Int J Tuberc
Lung Dis 2010; 14(10): 1323-29.