Revista
Portuguesa
de
Cardiologia
Portuguese
Journal
of
Cardiology
www.revportcardiol.orgORIGINAL
ARTICLE
Left-sided
infective
endocarditis:
Analysis
of
in-hospital
and
medium-term
outcome
and
predictors
of
mortality
João
Pedro
Ferreira
a,b,∗,
Filipa
Gomes
a,b,
Patrícia
Rodrigues
a,b,
Miguel
Araújo
Abreu
a,b,
José
Miguel
Maia
a,b,
Paulo
Bettencourt
a,b,
André
Luz
a,b,
Severo
Torres
a,b,
João
Araújo
Correia
a,baInternalMedicineandCardiologyDepartments,CentroHospitalardoPorto,Porto,Portugal bInternalMedicineDepartment,CentroHospitalardeSãoJoão,Porto,Portugal
Received19September2012;accepted1November2012 Availableonline25October2013
KEYWORDS Infective endocarditis; Outcome; Analysis; Mortality Abstract
Introduction:Despitediagnosticandtherapeuticadvances,infectiveendocarditis(IE)remains a challenging andpotentially lethal disease. The prognosisof IE remains poor; in the last 30years,itsincidenceandmortalityhaveonlybeenmarginallyreduced.Earlyidentificationof high-riskpatientscanchangethecourseofthediseaseandimproveoutcomes.
Objectivesandmethods: To describeand investigate predictorsofmortalityduringhospital stayandinthesixmonthsafterdischargeinacohortofleft-sidedIEpatientsintwotertiary centers.AllpatientsdiagnosedwithIE(ICD9code133)wereregisteredinauniformdatabase. Results:Onehundredandforty-sevenconsecutivecasepatientswithleft-sidedIEwereincluded inthisstudy.Thirty-fivepatients(23.8%)diedduringhospitalstay.Thevariablessignificantly associatedwithincreasedmortalityinunivariateanalysiswereCharlsonindex≥5,useof immu-nosuppressants,sepsis(severesepsisand/orsepticshock),cardiogenicshockandinappropriate useofantibiotictherapy.Conversely,surgicaltherapyandhospitallengthofstay≥30dayswere significantlyassociatedwithlowermortality.Inmultivariateanalysisthemostimportant pre-dictorsofin-hospitalmortalityweresepsis(severeand/orshock),useofimmunosuppressants andinappropriateuseofantibiotictherapy.Therewasasignificantrelationbetweentheuse ofimmunosuppressantsandtheoccurrenceofsepsis.Thepresenceofsignificantvalvedisease afterIEsignificantlyincreasedtheriskofheartfailure.
Conclusions: OurresultsmayhelptoidentifyIEpatientsatincreasedriskforin-hospital mor-talityandmedium-termdisability.Thesefindingscanhelptoidentifycandidatesforearlierand moreaggressivemanagement.
© 2012 Sociedade Portuguesa de Cardiologia Published by Elsevier España, S.L. All rights reserved.
∗Correspondingauthor.
E-mailaddress:jp7ferreira@hotmail.com(J.P.Ferreira).
0870-2551/$–seefrontmatter©2012SociedadePortuguesadeCardiologiaPublishedbyElsevierEspaña,S.L.Allrightsreserved. http://dx.doi.org/10.1016/j.repc.2012.11.015
PALAVRAS-CHAVE Endocardite infecciosa; Prognóstico; Análise; Mortalidade
Endocarditeinfecciosaesquerda:análisedeprognósticoepreditoresdemortalidade Resumo
Introduc¸ão:Apesardosavanc¸osnodiagnósticoeterapêuticadaendocarditeinfecciosa,esta patologiamantém-sedesafianteepotencialmentefatal.Oprognósticodestadoenc¸amantevese praticamenteinalteradonosúltimos30anos.Aidentificac¸ãoprecocedosdoentesdealtorisco podealterarocursodadoenc¸aemelhoraroprognóstico.
Objetivosemétodos: Descrevereinvestigarospreditoresdemortalidadeduranteo interna-mento enosseismesesapósaalta dosdoentescomdiagnóstico deendocardite infecciosa esquerda(códigoICD9:133).
Resultados: Foramincluídos147doentescomendocarditeinfecciosaesquerda.Trintaecinco doentes(23,8%)morreramduranteointernamento.Registou-se umaumentosignificativoda mortalidadenaanáliseunivariadacom:Charlsonindex≥5,usodeimunossupressores,sépsis (sépsisgravee/ouchoquesético),choquecardiogénicoeusoinapropriadodeantibioterapia. Contudo,arealizac¸ãodecirurgiacardíacaetempodeinternamento≥30diasassociaramse significativamente com taxas de mortalidade mais baixas. Os preditores mais relevantes de mortalidadeintra-hospitalar naanálisemultivariada foram: sépsis(grave e/ou choque), usodeimunossupressoreseusoinapropriadodeantibioterapia.Verificou-seumainterac¸ão sig-nificativaentreousodeimunossupressoreseaocorrênciadesépsis.Apresenc¸adepatologia valvularapósresoluc¸ãodoquadroinfecciosoaumentouoriscodeinsuficiênciacardíaca. Conclusões:Osnossosresultadospodemajudaraidentificarquaisosdoentescommaiorrisco demortalidadeintra-hospitalaredecomplicac¸õesamédioprazo,assimcomoajudaratriaros candidatosquedevemsersujeitosaumamonitorizac¸ãomaisapertada.
© 2012 SociedadePortuguesa de Cardiologia. Publicado por Elsevier España, S.L.Todos os direitosreservados.
Introduction
Despite diagnostic and therapeutic advances, infective endocarditis (IE) remains a challenging and potentially lethal disease1 with a dismal prognosis. In the last
30yearstheincidenceandmortalityofIEhaveonly been marginally reduced.2 Most series report in-hospital
mor-tality between 9.6 and 26%3---7 and long-term (more than
six months) mortality between 20 and 37.1%.7---9 Only a
limited number of studies have focused on medium-term outcomes.10
Heterogeneityin clinicalpresentation, thepresence of structural heart disease, the different types of microor-ganism involved, the development of complications, and patientcharacteristics,allrequireamultidisciplinaryteam to be involved in the treatment of IE.1,11 Many
stud-ies suggest that early identification of high-risk patients can change the course of the disease and improve outcomes.12
Prognosisisinfluencedbyfourtypesoffactors:patient characteristics, associated complications, microbial eti-ology, and echocardiographic findings.3,13 Patients with
heart failure (HF), perivalvular complications, and/or methicillin-resistant Staphylococcus aureus (MRSA) infec-tionsusuallyhavehighermortalityandoftenneedsurgery in the active disease phase.13,14 Several studies have
identified different independent prognostic factors asso-ciated with higher mortality, such as higher number of comorbidities, advanced age, renal insufficiency, sep-tic shock, insulin-dependent diabetes, heart failure with reducedejectionfraction,prostheticvalveIE,andcerebral embolism.3,5,7,15,16
Objectives
Todeterminethecharacteristicsofourpopulationwith left-sided IEand toinvestigate factors associated withhigher mortalityduring hospitalstay and inthe sixmonths after discharge inatwo-centercohort ofleft-sidedIE patients. Thisanalysisisintendedtoidentifyclinicalproceduresthat could be improved to minimize mortalityassociated with left-sidedIE.
Methods
Studypopulation
All patients diagnosed with IE (ICD9 code 133) in two tertiaryhospitalsinPorto,Portugal,wereregisteredina uni-formdatabasebasedoninformationfrommedicalrecords between January2000andJune 2011.The studyincluded casesfrombothcommunityandreferralhospitals.
Criteriaanddefinitions
Left-sided IE wasdefined according tothe modified Duke criteria17fordefiniteorpossibleIE.
Foreachcase,datawerecollectedregardingage, gen-der,valvularinvolvement,comorbidities,echocardiographic findings, microbiologic agents, associated complications, treatment(includingsurgery),andoutcome(in-hospitaland in the six months after discharge). The European System for Cardiac Operative Risk Evaluation (EuroSCORE) surgi-calriskscore18 wasdeterminedin allpatients.Inpatients
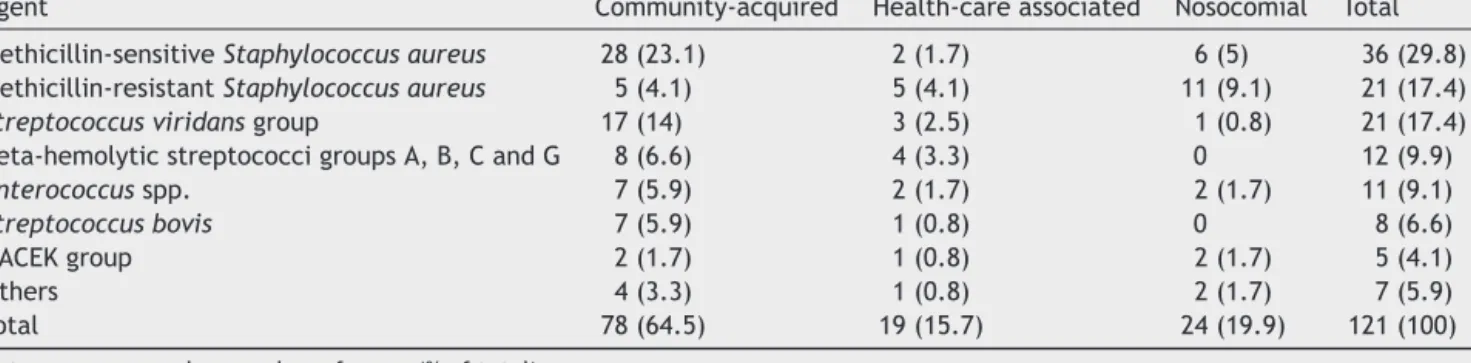
Table1 Microbiologicetiologybymodeofacquisition.
Agent Community-acquired Health-careassociated Nosocomial Total Methicillin-sensitiveStaphylococcusaureus 28(23.1) 2(1.7) 6(5) 36(29.8) Methicillin-resistantStaphylococcusaureus 5(4.1) 5(4.1) 11(9.1) 21(17.4)
Streptococcusviridansgroup 17(14) 3(2.5) 1(0.8) 21(17.4)
Beta-hemolyticstreptococcigroupsA,B,CandG 8(6.6) 4(3.3) 0 12(9.9)
Enterococcusspp. 7(5.9) 2(1.7) 2(1.7) 11(9.1)
Streptococcusbovis 7(5.9) 1(0.8) 0 8(6.6)
HACEKgroup 2(1.7) 1(0.8) 2(1.7) 5(4.1)
Others 4(3.3) 1(0.8) 2(1.7) 7(5.9)
Total 78(64.5) 19(15.7) 24(19.9) 121(100)
Dataareexpressedasnumberofcases(%oftotal).
undergoingsurgery,theSocietyofThoracicSurgeons(STS) surgicalriskscore19wasalsoused.
Patients with nosigns of infection and negativeblood cultures after a complete course of antibiotic therapy were considered cured. Relapse was defined asa new IE episodecausedbythesameagentwithinsixmonths. Rein-fectionwasdefinedasanewIEepisodecausedbyadifferent agent.
Immunosuppressionwasconsidered tobepresent when patients had been taking immunosuppressants or ≥15 mg ofprednisolone orequivalentfor morethanthreemonths and/or had CD4 counts of <350 cells/mm3 when infected
withhumanimmunodeficiencyvirus.
Appropriacyofantibiotictherapywasdefinedaccording tothelatestguidelines.12
The primary outcome was overall all-cause in-hospital mortalityanddeathfromcardiaccausewithinsix months ofdischarge.
Thestudywasapprovedbythelocalethicscommittee.
Statisticalanalysis
Comparisonbetweengroupswasperformedwithparametric ornon-parametric tests,asappropriate.Continuous varia-bles are expressedas mean ± standard deviation (SD)or median(inter-quartilerange,IQR).Categoricalvariablesare expressedinabsolutenumbersandproportions.
Theassociationbetweenvariablesandtheprimary out-come wasfirst tested by univariateanalysis. Asignificant associationwasdefinedbyapvalue≤0.05.Variableswith significantassociationweretestedbystepwisemultivariate analysis.Predictorsofoutcome wereidentifiedby logistic regressionanalysis.The statisticalanalysiswasperformed usingSPSSsoftwareversion19,Chicago,IL,USA.
Results
Onehundredandforty-sevenconsecutivecasepatientswith left-sidedIEwere included.The medianage was63years (IQR45-74).Onehundredandfive(71.4%)weremale.
Onehundredandtwenty-nine(87.8%)caseswere consid-eredasdefiniteand18(12.2%)aspossibleIE,accordingto themodifiedDukecriteria.
Most patients (128, 87.1%) hadIE onnative valves. Of the19(12.9%)patientswithprostheticvalves,3(16%)were
consideredearlyand16(84%)lateIE.Theaorticvalvewas affectedin74(50.3%)cases,themitralvalvein60(40.8%), andbothvalvesin13(8.8%)patients.
Ninety-threepatients(63.3%)underwentboth transtho-racic (TTE) and transesophageal (TEE) echocardiography, 48(32.7%)hadTTEalone,andsix(4.1%)TEEalone.Overall, 81(55.1%)hadavalvulopathyand/orinterventionpossibly predisposing for IE: 31 (21.1%) had degenerative valvular disease;20(13.6%)hadprostheticvalves;12(8.2%)had con-genitalheartdisease;12(8.2%)hadrecentlyundergonean invasivegastrointestinalintervention;five(3.4%)had previ-ousIE;andone(0.7%)hadrheumaticvalvulardisease.
ThemedianCharlsonindexwas5(IQR3-7).Onehundred andsixteen (78.9%)patientshadsignificantcomorbidities. Of these, 37 (25.2%) had diabetes (of whom 15 [10.2%] weretakinginsulinand22 [15%]weretaking oral antidia-beticagents), 27 (18.4%) were taking immunosuppressive agents, 17 (11.6%) had renal failure undergoing dialysis, 15(10.2%)hadactivecancer,15(10.2%)wereintravenous drugabusers,12(8.2%)hadlivercirrhosis,and11(7.5%)had chronicobstructivepulmonarydisease(COPD).
Feverand/orgeneralsymptomswerepresent forabout amonthbeforeadmission(median27.5days,IQR15-30).
Etiology was established by isolating the causative agentfromblood culture in 121 (82.3%)patients. Ninety-eight(66.7%)of the infections werecommunity-acquired, 21(14.3%)werehealth-careassociated,and28(19%)were nosocomial. Methicillin-sensitive Staphylococcus aureus
(MSSA) was the most frequent microorganism isolated, followed by methicillin-resistant Staphylococcus aureus
(MRSA), Streptococcus viridans group, beta-hemolytic streptococci groups A, B, C and G and Enterococcus spp. (Table1).Antibiotictherapywasconsideredappropriatein 123 (83.7%) patients. In the 24 (16.3%) patients in whom antibiotictherapy wasconsidered inappropriate, this was duetoshortdurationoftreatmentinnine(6.1%)patients, inappropriatespectrum in nine(6.1%) patients, and inap-propriatedurationandspectruminfour(2.7%).Five(3.4%) patientshadinfectionrelapseandanotherfivehad reinfec-tion.
Seventy-nine (53.7%) patients had a single vege-tation smaller than 20 mm, 16 (10.9%) had a single vegetationlargerthan20mm,and52(35.4%)hadmultiple vegetations.
Complications were frequent: 54 (36.7%) had severe valvularregurgitation (28[19%] involving theaortic valve
and26[17.7%]involving themitralvalve), 39(26.5%)had perivalvular complications (of whom 27 [18.4%] had an abscess,five[3.4%]hadafistula,five[3.4%]hadperforation, two[1.4%]hadaneurysm, 50(34%) hadperipheral and/or splenic embolicphenomena, 31 (21.1%) presented neuro-logiccomplications(ofwhom21[14.3%]hadsepticemboli, six[4.1%]hadhemorrhage,three[2%]hadabscess,andone [0.7%]hadmeningitis),22(15%)hadsepticshock,16(10.9%) hadcardiogenicshock,andthree(2%)hadmyocardial infarc-tion.
Valvular surgery wasperformed in 57 (38.8%) patients (urgent/emergentin 47[31.9%]patients andscheduled in 10[6.8%]cases).Ofthepatientsundergoingsurgery,the aor-ticvalvewasreplacedin28(19%)patients,themitralvalve in18(12.2%),andbothvalvesin10(6.8%).Allthe57patients undergoingsurgeryhadheartfailureandvalvedysfunction. Of these, 40 (70%) had severe valvular regurgitation and 24(42%)hadperivalvularcomplicationwithextensionofthe infectiousprocess.Inthepatientswhounderwentsurgery, themedianSTSscorewas4.5(IQR1.4-8.3),andthemedian EuroSCOREwas4.4(IQR1.6-6.9).Therewerenodifferences inEuroSCOREvaluesbetweenpatientswhodidandwhodid notundergosurgery(OR0.99;95%confidenceinterval[CI] 0.97-1;p=0.9).Ofthese57 patientspost-surgery informa-tionwasavailablefor54:14(25.9%)hadcomplications(four [29%]pneumonia,two[14%]arrhythmia,two[14%]stroke, two[14%] death, two [14%]cardiac tamponade, one[7%] ischemicheartdisease,andone[7%]valvulardysfunction); theother40(74.1%)hadnoevents.
Thirty-five patients (23.8%) died during hospital stay. Themain causesof deathweresepticshock in13(37.1%) patients, cardiogenic shock in 8 (22.9%), and neurologic complicationsinasimilarpercentage.
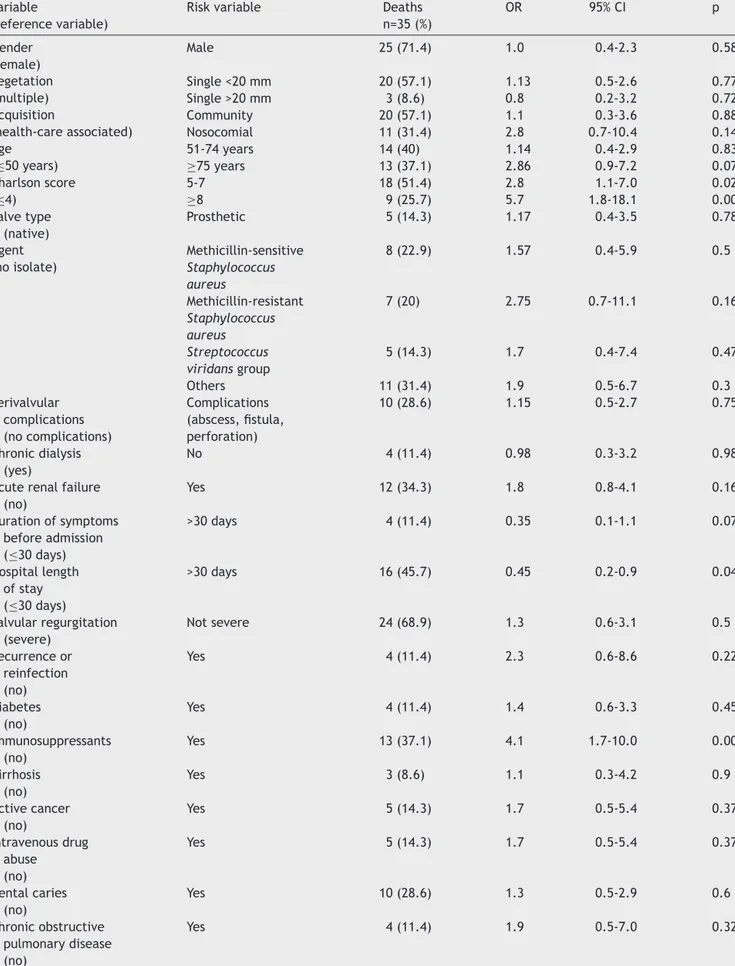
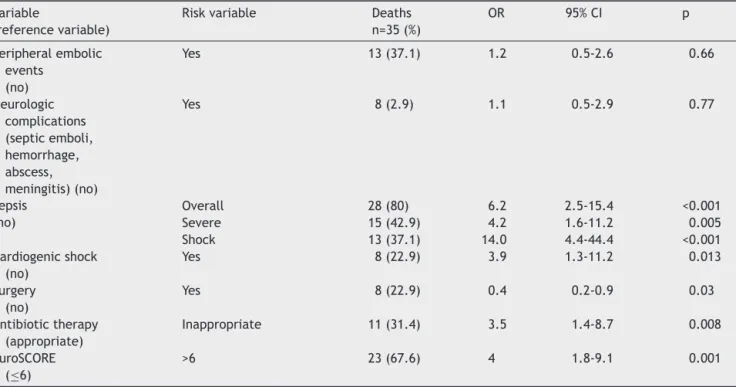
The variables significantly associated with increased in-hospital mortality in univariate analysis were Charlson index≥5,EuroSCORE>6,useofimmunosuppressants,sepsis (severeand/orshock),cardiogenicshockandinappropriate useofantibiotic therapy.Conversely,patients who under-went surgery and those with hospital stay ≥30 days had significantlylowermortality(Table2).Inmultivariate anal-ysisthemostimportantpredictorsofmortalityweresepsis (severe and/or shock) (odds ratio [OR] 10.6; 95% CI 3.5-31.7; p<0.001), use of immunosuppressants (OR 8.6; 95% CI2.6-28.8; p<0.001),EuroSCORE>6 (OR3.5; 95% CI 1.2-9.7;p=0.019),andinappropriateuseof antibiotictherapy (OR6.8;95%CI2.0-23.6;p=0.002).Therewasasignificant relationbetweentheuseofimmunosuppressantsandsepsis (p=0.003).
PatientswithEuroSCORE>6hadincreasedmortality,but thiswasnotstatisticallysignificant(OR3;95%CI0.6-14.3; p=0.15). In our study the EuroSCORE cut-off that maxi-mizedsensitivityandspecificityforpredictingmortalitywas 7(area under thecurve 0.75; 95% CI 0.65-0.86; p<0.001) (Figure1).
Themedianlengthofhospitalstaywas40days(IQR 22.5-56).
During the six months after hospitalization, another 11(9.8%)patientsdied,nine(81.8%)duetoIEcomplications (heartfailureduetovalvulardysfunction),andtwo(18.2%) duetoothercauses(infectiouscomplications).Thirty-eight patients developed heart failure (32 [84.2%] in New York HeartAssociation [NYHA] classII and six[15.8%] in NYHA
1,0 0,8 0,6 0,6 1- specificity Sensitivity 0,8 1,0 0,4 0,4 0,2 0,2 0,0 0,0
Figure1 ReceiveroperatorcurveforEuroSCORE.
class III). Fifteen patients had valvular dysfunction (five [33.3%] moderate aortic regurgitation, one [6.7%] severe aortic regurgitation,seven[46.7%]moderatemitral regur-gitation,andtwo[13.3%]severemitralregurgitation).Ten patientshadneurologicsequelae(six[60%]motorandfour [40%] other complications such asepilepsy, diplopia, and aphasia).
Thepresence ofvalvular sequelaeafter IEsignificantly increased the risk of heart failure and mortality due to cardiac causes duringfollow-up (OR 7.4;95% CI 2.3-23.5; p=0.001andOR1.6;95%CI1.2-6.3;p<0.001,respectively). Meansurvivalwasfourmonths(95%CI3.3-4.6)(Figure2).
Discussion
In ourstudy,we observed similarcharacteristics and out-comesforIEpatientstothosedescribedpreviously.2,10,12
We see in the infrequent use of inappropriate antibi-otictherapy(durationand/orspectrum)anopportunityto improveoutcomeofIEpatients.20---22
Delayindiagnosis,complications,lengthofhospitalstay, andmortalityremainhighinIE.1Althoughmortalitylower
than20%hasbeenreported,23,24 itusuallyrangesbetween
1,0 Sur viv al function Survival function 0,8 0,6 0,4 0,2 0,0 0 1 2 Time (months) 3 4
Death After Hospitalization
5
Figure 2 Kaplan-Meier curve for survival (months) after discharge.
Table2 Univariateanalysisofin-hospitalmortality. Variable
(referencevariable)
Riskvariable Deaths
n=35(%) OR 95%CI p Gender (female) Male 25(71.4) 1.0 0.4-2.3 0.58 Vegetation (multiple) Single<20mm 20(57.1) 1.13 0.5-2.6 0.77 Single>20mm 3(8.6) 0.8 0.2-3.2 0.72 Acquisition (health-careassociated) Community 20(57.1) 1.1 0.3-3.6 0.88 Nosocomial 11(31.4) 2.8 0.7-10.4 0.14 Age (≤50years) 51-74years 14(40) 1.14 0.4-2.9 0.83 ≥75years 13(37.1) 2.86 0.9-7.2 0.07 Charlsonscore (≤4) 5-7 18(51.4) 2.8 1.1-7.0 0.028 ≥8 9(25.7) 5.7 1.8-18.1 0.003 Valvetype (native) Prosthetic 5(14.3) 1.17 0.4-3.5 0.78 Agent (noisolate) Methicillin-sensitive Staphylococcus aureus 8(22.9) 1.57 0.4-5.9 0.5 Methicillin-resistant Staphylococcus aureus 7(20) 2.75 0.7-11.1 0.16 Streptococcus viridansgroup 5(14.3) 1.7 0.4-7.4 0.47 Others 11(31.4) 1.9 0.5-6.7 0.3 Perivalvular complications (nocomplications) Complications (abscess,fistula, perforation) 10(28.6) 1.15 0.5-2.7 0.75 Chronicdialysis (yes) No 4(11.4) 0.98 0.3-3.2 0.98
Acuterenalfailure (no) Yes 12(34.3) 1.8 0.8-4.1 0.16 Durationofsymptoms beforeadmission (≤30days) >30days 4(11.4) 0.35 0.1-1.1 0.07 Hospitallength ofstay (≤30days) >30days 16(45.7) 0.45 0.2-0.9 0.04 Valvularregurgitation (severe) Notsevere 24(68.9) 1.3 0.6-3.1 0.5 Recurrenceor reinfection (no) Yes 4(11.4) 2.3 0.6-8.6 0.22 Diabetes (no) Yes 4(11.4) 1.4 0.6-3.3 0.45 Immunosuppressants (no) Yes 13(37.1) 4.1 1.7-10.0 0.001 Cirrhosis (no) Yes 3(8.6) 1.1 0.3-4.2 0.9 Activecancer (no) Yes 5(14.3) 1.7 0.5-5.4 0.37 Intravenousdrug abuse (no) Yes 5(14.3) 1.7 0.5-5.4 0.37 Dentalcaries (no) Yes 10(28.6) 1.3 0.5-2.9 0.6 Chronicobstructive pulmonarydisease (no) Yes 4(11.4) 1.9 0.5-7.0 0.32
Table2(Continued) Variable
(referencevariable)
Riskvariable Deaths
n=35(%) OR 95%CI p Peripheralembolic events (no) Yes 13(37.1) 1.2 0.5-2.6 0.66 Neurologic complications (septicemboli, hemorrhage, abscess, meningitis)(no) Yes 8(2.9) 1.1 0.5-2.9 0.77 Sepsis (no) Overall 28(80) 6.2 2.5-15.4 <0.001 Severe 15(42.9) 4.2 1.6-11.2 0.005 Shock 13(37.1) 14.0 4.4-44.4 <0.001 Cardiogenicshock (no) Yes 8(22.9) 3.9 1.3-11.2 0.013 Surgery (no) Yes 8(22.9) 0.4 0.2-0.9 0.03 Antibiotictherapy (appropriate) Inappropriate 11(31.4) 3.5 1.4-8.7 0.008 EuroSCORE (≤6) >6 23(67.6) 4 1.8-9.1 0.001
CI:confidenceinterval;OR:oddsratio.
20%and 30%.4 Inour study,in-hospitalmortalityof 23.8%
wasobserved,suggestingthatourpopulationreflectssimilar samplesfromregistries.
A Charlson index of more than 2 has been reported tobean independentriskfactor for mortalityin previous studies.15,25Weusedtheage-adjustedindex,assumingage
toberelatedtopoorprognosis.26Inourstudy,age≥75years
hada trend towards higher mortality.Significantly higher mortalitywasfoundinpatientstakingimmunosuppressants, similartothatreportedinaFrenchstudy.7
The EuroSCORE tool is used for predicting in-hospital mortalityforcardiacsurgery.27AEuroSCORE>6isconsidered
highrisk.28Ourresultsareconsistentwiththisclassification;
wealsofoundituseful forpredicting overallmortality(in allpatients).Basedonthesefindingswerecommend calcu-latingtheEuroSCOREforanypatientadmittedforinfective endocarditis.
Shorter (≤30 days) hospital stay was associated with increasedmortality(mostpatientsdiedinthefirst30days ofhospitalstay).
Sepsiswithdysfunctionoftwoormoreorganswas inde-pendently associated with increased mortality. Previous studieshavefoundanassociationbetweensepticshockand increased mortality.5,26 This variable, particularly severe
sepsis,helpstoidentifyhigh-riskpatientswhocanbenefit fromearly,protocol-basedaggressivemanagement.
Unlike other studies3 we did not find heart failure at
admission(NYHAclassIIIorIV)tobeassociatedwithworse prognosis. This observation corroborates previous results pointing in the same direction.26 However, mortality was
higher when patients developed cardiogenic shock during hospitalization.Onepossibleexplanationforthesefindings is thatdevelopment of cardiogenic shock during hospital-izationis, in most cases,due tosevere valve dysfunction
needingemergentsurgicalrepair.Bycontrast,heartfailure at admission (due to fluid overload, arrhythmia, anemia, etc.)canberesolvedwithmedicaltreatment.
The role of surgery in the treatment of infective endocarditis is expanding, and current guidelines advo-cate surgical managementfor complicatedleft-sided IE.12
Early surgery is also strongly indicated for patients with IE and congestiveheart failure.14 Recently, another study
found that early surgery in patients with IE and large vegetations significantly reduced death from any cause and specifically embolic events by effectively decreasing the risk of systemic embolism.29 Surgery was also found
to be a protective factor in our study. This interest-ing finding has been described in previous observational studies.3,15,26Thisisprobablyrelatedtothehighnumberof
complicatedcaseswithseverevalvulardysfunctionand car-diogenicshock.However,theseresultsshouldbeinterpreted with caution since this was a retrospective observational study.
Asexpected,inappropriateuseofantibiotictherapywas strongly associated with increased mortality, reinforcing theneed forcorrectmanagementofblood cultures,early initiation of antibiotic therapy, and adjustments accord-ingtopharmacokinetics,pharmacodynamics,microbiologic findings,andcurrentrecommendationsregardinglengthof treatmentandpotentialantimicrobialassociations.12
Diabetes,30prostheticvalveIE,31 Staphylococcusaureus
etiology,32 neurologiccomplications,24 largevegetations,25
and perivalvular extension of infection13,24 have all been
identifiedasrisk factorsfor highermortality.Such associ-ationswerenotfoundinourstudy,possiblyduetothesmall samplesizeineachsetting.
In our study, six-month mortality was 9.8%, similar to medium-termoutcomesdescribedbyotherauthors.10,33
Notsurprisingly,thepresenceofvalvulopathyafterIE sig-nificantlyincreasedtherisk ofheart failureat sixmonths afterdischarge.Nosignificantassociationswerefoundwith mortalityatsixmonths,possiblyduetothesmallnumberof deathsrecorded.
Ourstudyhascertainlimitations:(1)itwasa retrospec-tiveobservationalstudy:informationwaslimitedtomedical records, important data may have been incomplete, and someresultsmaybebiased(suchasthe protectiveeffect ofsurgery,sincehighsurgicalriskpatientsmayhavebeen refused surgery); (2) changes in the clinical management ofIEhaveoccurredduringthestudyperiod;(3)somecases werefromreferralcenters,andsothepercentageof compli-catedcasesmaybeoverestimated;(4)somepatientswere losttofollow-uportransferredtootherhospitals.
Conclusions
Thedevelopmentofseveresepsisisastrongpredictorofa dismaloutcomeandantibiotictreatmentshouldbestarted promptly.Patientsonimmunosuppressantsalsohaveaworse prognosis. As expected, obtaining an early diagnosis and following the antibiotic guidelineshave a positive impact onoutcome.Theneedforsurgeryismainlydeterminedby heartfailure,whichshouldbecarefullyevaluated.
OurresultsmayhelptoidentifyIEpatientsatincreased risk for in-hospital mortality and medium-term disability. These findings can help toidentify candidates for earlier andmoreaggressivemanagement.
Ethical
disclosures
Protection of human and animal subjects.The authors declarethatnoexperimentswereperformedonhumansor animalsforthisstudy.
Confidentialityofdata.Theauthorsdeclarethattheyhave followedtheprotocolsoftheirworkcenteronthe publica-tionofpatientdataandthatallthepatientsincludedinthe studyreceivedsufficientinformationandgavetheirwritten informedconsenttoparticipateinthestudy.
Righttoprivacyandinformedconsent.The authorshave obtained the written informedconsent ofthe patients or subjectsmentionedinthearticle.Thecorrespondingauthor isinpossessionofthisdocument.
Conflicts
of
interest
Theauthorshavenoconflictsofinteresttodeclare.
References
1.ThunyF,GrisoliD,CollartF,HabibG,RaoultD.Management ofinfectiveendocarditis:challengesandperspectives.Lancet. 2012;379:965---75[Epub2012February7].
2.Moreillon P, Que YA. Infective endocarditis. Lancet. 2004;363:139---49.
3.Chu VH, Cabell CH, Benjamin Jr DK, et al. Early predic-torsofin-hospitaldeathininfectiveendocarditis.Circulation. 2004;109:1745---9[Epub2004March22].
4.TornosP,IungB,Permanyer-MiraldaG,etal. Infective endo-carditisinEurope:lessonsfromtheEuroheartsurvey.Heart. 2005;91:571---5.
5.WallaceSM, WaltonBI, KharbandaRK, et al. Mortality from infectiveendocarditis: clinicalpredictors ofoutcome.Heart. 2002;88:53---60.
6.CabellCH,JollisJG,PetersonGE,etal.Changingpatient char-acteristics and theeffect onmortalityin endocarditis. Arch InternMed.2002;162:90---4.
7.DelahayeF,Alla F,BeguinotI,et al.In-hospitalmortalityof infectiveendocarditis:prognosticfactorsandevolutionoveran 8-yearperiod.ScandJInfectDis.2007;39:849---57.
8.CastilloJC,AnguitaMP,RamirezA,etal.Longtermoutcomeof infectiveendocarditisinpatientswhowerenotdrugaddicts:a 10yearstudy.Heart.2000;83:525---30.
9.Netzer RO, Altwegg SC, Zollinger E, et al. Infective endo-carditis:determinantsoflongtermoutcome.Heart.2002;88: 61---6.
10.Nomura A, Omata F, Furukawa K. Risk factors of mid-term mortality ofpatients with infective endocarditis. Eur J Clin MicrobiolInfectDis.2010;29:1355---60[Epub2010July17]. 11.Habib G. Management of infective endocarditis. Heart.
2006;92:124---30.
12.HabibG, Hoen B,Tornos P,et al.Guidelines onthe preven-tion,diagnosis,andtreatmentofinfectiveendocarditis(new version2009):theTaskForceonthePrevention,Diagnosis,and TreatmentofInfectiveEndocarditisoftheEuropeanSocietyof Cardiology(ESC).EndorsedbytheEuropeanSocietyofClinical MicrobiologyandInfectiousDiseases(ESCMID)andthe Interna-tionalSocietyofChemotherapy(ISC)forInfectionandCancer. EurHeartJ.2009;30:2369---413[Epub009August27].
13.SanRomanJA,LopezJ,VilacostaI.,etal.Prognostic stratifi-cationofpatientswithleft-sidedendocarditisdeterminedat admission.AmJMed.2007;120:369e1---7.
14.Prendergast BD, Tornos P.Surgery for infective endocarditis: whoandwhen?Circulation.2010;121:1141---52.
15.HasbunR,VikramHR,BarakatLA,etal.Complicatedleft-sided nativevalveendocarditisinadults:riskclassificationfor mor-tality.JAMA.2003;289:1933---40.
16.JassalDS,NeilanTG,PradhanAD,etal.Surgicalmanagementof infectiveendocarditis:earlypredictorsofshort-termmorbidity andmortality.AnnThoracSurg.2006;82:524---9.
17.Durack DT, Lukes AS, Bright DK. New criteria for diagnosis ofinfectiveendocarditis:utilizationofspecific echocardiogra-phicfindings. DukeEndocarditisService.AmJMed.1994;96: 200---9.
18.RoquesF,NashefSA,MichelP,etal.Riskfactorsandoutcome inEuropeancardiacsurgery:analysisoftheEuroSCORE multi-nationaldatabaseof19030patients.EurJCardiothoracSurg. 1999;15:816---22,discussion22---3.
19.JinR,FurnaryAP,FineSC,etal.UsingSocietyofThoracic Sur-geonsriskmodelsforrisk-adjustingcardiacsurgeryresults.Ann ThoracSurg.2010;89:677---82.
20.HoenB,AllaF,Selton-SutyC,etal.Changingprofileof infec-tiveendocarditis:resultsofa1-yearsurveyinFrance.JAMA. 2002;288:75---81.
21.MoulyS,RuimyR,LaunayO,etal.Thechangingclinicalaspects ofinfectiveendocarditis:descriptivereviewof90episodesin aFrenchteachinghospitalandriskfactorsfordeath.JInfect. 2002;45:246---56.
22.StromBL,AbrutynE,BerlinJA,etal.Riskfactorsforinfective endocarditis: oralhygiene and nondentalexposures. Circula-tion.2000;102:2842---8.
23.Ben-AmiR,GiladiM,CarmeliY,etal.Hospital-acquired infec-tive endocarditis: should the definition be broadened? Clin InfectDis.2004;38:843---50[Epub2004March1].
24.Murdoch DR, Corey GR, Hoen B, et al. Clinical presenta-tion, etiology,and outcome of infective endocarditis in the
21stcentury:theInternationalCollaborationon Endocarditis-ProspectiveCohortStudy.ArchInternMed.2009;169:463---73. 25.ThunyF,DiSalvoG,BelliardO,etal.Riskofembolismanddeath
ininfectiveendocarditis:prognosticvalueofechocardiography: a prospectivemulticenterstudy.Circulation.2005;112:69---75 [Epub2005June27].
26.Galvez-AcebalJ,Rodriguez-BanoJ,Martinez-MarcosFJ,etal. Prognostic factors in left-sided endocarditis: results from the Andalusianmulticentercohort. BMC Infect Dis. 2010;10: 17.
27.Xu J, Zhang FR, Zhu JH, et al. Study on the efficiency of the European System for Cardiac Operative Risk Evaluation (EuroSCORE)inpredictingin-hospitalmortalityofthepatients withpercutaneous coronary intervention. Zhonghua Liu Xing BingXueZaZhi.2010;31:1170---3.
28.DiDeddaU,PelisseroG,AgnelliB,etal.Accuracy,calibration andclinicalperformanceofthenewEuroSCOREIIrisk stratifi-cationsystem.EurJCardiothoracSurg.2012;20:20.
29.Kang DH, Kim YJ, Kim SH, et al. Early surgery versus con-ventionaltreatmentforinfectiveendocarditis.NEnglJMed. 2012;366:2466---73.
30.Kourany WM, Miro JM, Moreno A, et al. Influence of dia-betesmellitusontheclinicalmanifestationsandprognosisof infectiveendocarditis:areportfromtheInternational Collab-orationonEndocarditis-MergedDatabase. ScandJInfect Dis. 2006;38:613---9.
31.LalaniT,KanafaniZA,ChuVH,etal.Prostheticvalve endocardi-tisduetocoagulase-negativestaphylococci:findingsfromthe InternationalCollaborationonEndocarditisMergedDatabase. EurJClinMicrobiolInfectDis.2006;25:365---8.
32.Fowler Jr VG, Miro JM, Hoen B, et al. Staphylococcus aureusendocarditis:aconsequenceofmedicalprogress.JAMA. 2005;293:3012---21.
33.Martinez-SellesM,MunozP,EstevezA,etal.Long-termoutcome ofinfective endocarditisinnon-intravenousdrugusers.Mayo ClinProc.2008;83:1213---7.