Authors
Douglas Squizatto Leite1,2 Natasha Lure Bueno de Camargo1,2
Flamarion de Barros Cordeiro2
Adriana de Fátima Menegat Schuinski1,2
Gilberto Baroni1,2
1 Ponta Grossa State University (UEPG).
2 Santa Casa de Misericórdia de Ponta Grossa.
Submitted on: 07/29/2013. Approved on: 10/11/2013.
Correspondence to: Gilberto Baroni.
Ponta Grossa State University (UEPG). Santa Casa de Misericórdia de Ponta Grossa.
Av. Vicente Machado, nº 909, apto 71, Centro. Ponta Grossa, PR, Brasil. CEP: 84010-000 E-mail: gbaroni@superig.com.br
I
NTRODUCTIONChronic kidney disease (CKD) is a major public health concern in Brazil. The prevalence of CKD has increased with the aging of the population and the growing number of people with high blood pressure and diabetes. According to the 2011 Census of the Brazilian Society of Nephrology (SBN), 91,314 patients were on dialysis in the country that year, a number well above the 42,695 on dialysis in 2000.1,2 Ninety
percent of these patients were on hemodialysis.
According to the guidelines of the National Kidney Foundation Dialysis Outcomes Quality Initiative (NKF-DOQI), the recommended approach for CKD patients on hemodialysis is to offer them arteriovenous fistulas (AV), as they can be used for longer periods of time, require fewer maintenance interventions, and provide for lower infection rates. Nevertheless, a significant number of patients has been equipped with double-lumen catheters (DLCs) instead, mainly because hemodialysis can be initiated immediately after they are put in place.3,4 DLCs may
be used in short-term applications, such as in emergency situations, or in long-term scenarios. The latter is indicated for patients without other viable access options.
Implications of the use of vascular CDL in hemodialysis patients:
analysis of echographic insertion sites
Introduction: Chronic renal failure is a disease which prevalence has been increasing in Brazil. Hemodialysis is their primary therapeutic modality and arterio-venous fistula their preferential access. Nevertheless, many patients require the use of double-lumen catheters, either as permanent or temporary access. Vascular complications related to this procedure may occur, and their best method of non-invasive analysis is ultrasound analysis. Objective: To analyze the complications by the use of double-lumen catheter in patients with chronic kidney disease on hemodialysis, at "Santa Casa de Misericordia de Ponta Grossa" hospital, through eco-Doppler exam. Methods: Observational research, analytical, case-control type, to obtain data we used TASY®, interview, physical exam and imaging (eco-Doppler).
Results: None of the variables was significant isolated as a predictor of vascular impact in eco-Doppler, which detected changes in 31.25% of the cases. Physical exam showed poor accuracy compared to Doppler capacity to detect complications (K = -0.123).
Conclusion: We conclude that the
vascular effects of the use of CDL are frequent (31.25%). Manifesting itself in the form of occlusions with/without recanalization and stenoses. This leads us to required a prior analysis of the insertion site with Doppler, in order to avoid unnecessary procedures and possible complications.
A
BSTRACTKeywords: catheters; hemodialysis units, hospital; kidney failure, chronic.
DLCs are inserted into central veins, preferably the internal jugular and alternatively the subclavian vein, the latter being reserved for patients without a viable vein in the upper limbs.5
The literature indicates that DLCs may remain viable for a mean of 18 months.6
However, complications such as thrombosis and infection are frequent,7 and have been
described to affect 40% and 54% of the patients respectively. Vascular alterations may be analyzed with the Echo Doppler test, the best noninvasive method to assess cases of upper limb venous thrombosis.8 The sensitivity
of the Echo Doppler test for detecting stenosis of these vessels is 80%.9
This study aims to use the Echo Doppler test to evaluate vascular complications of patients on renal replacement therapy (RRT) at the Santa Casa de Misericórdia Hospital in Ponta Grossa (SCMPG), Brazil, undergoing hemodialysis with double lumen catheters.
M
ETHODSThis is a case-control analytical cohort study. Patients were enrolled as they were equipped with DLCs for purposes of RRT at the SCMPG. All catheters were placed by nephrologists assigned to the hemodialysis service of the hospital. Complications were analyzed based on clinical examination and Echo Doppler tests performed at least 30 days after the removal of the catheter. The study was carried out from November of 2012 to February of 2013.
The study protocol was approved by the institution’s Research Ethics Committee (nº 7128/2012). Patients who (1) agreed to join the study by giving informed consent and (2) were equipped with a DLC were included.
Data were collected from the TASY®
software system (the database used by the hospital to store patient personal and medical data) and a questionnaire answered by the enrolled subjects. Analyzed variables included age, gender, comorbidities, history of smoking and alcohol consumption, time using a DLC,
site of insertion, and catheter infection. Patients with signs of local infection (pain, purulent secretion) and consequent need for antibiotic therapy were deemed to have catheter infection. Patients also underwent clinical examination, which consisted of checking the site where the catheter had been placed for edema or visible collateral circulation. The subjects were then referred to the hospital’s imaging service for Echo Doppler tests. A Toshiba Xario SSA 660A®device made in Japan was used to assess
complications such as stenosis and obstruction, with and without reperfusion.
The collected data sets were stored on a database created on Microsoft Excel 2010®for
further descriptive and comparative statistical analysis.
Statistical analysis was performed using software GraphPad® to calculate Kappa, the
two-tailed Fisher’s exact test, and odds ratios.
R
ESULTSThirty-two individuals were included in the study. Most of the patients were males (66.7%) with ages under 60 years (62%) living in Ponta Grossa or neighboring municipalities served by the SCMPG. The most prevalent comorbidities were systemic hypertension (90.4%), heart disease (52.3%), and diabetes mellitus (35.7%).
The jugular vein was the preferred site of catheter insertion (73.8%), followed by the subclavian (26.1%) and femoral (4.7%) veins. In most cases (71.5%) DLCs were used for less than 30 days.
Table 1 shows the most relevant data for the enrolled patients.
(angiologists, nurses, nephrologists) must be aware of the short and long term complications and risks inherent to the use of these devices.
The most common site for catheter placement was the internal jugular vein, as recommended in the KDOQI.3 The literature, however, cites
left subclavian stenosis as the most frequent alteration,10,11 as a result of the interactions
between the subclavian vein and local bone structures.12
The incidence of infection in hemodialysis catheters has been more strongly associated with catheter dwelling time and number of hemodialysis sessions.13 Therefore, the short
time for which catheters were left in place on the subjects in our study possibly led to infection not being considered as a risk factor for the development of vascular alterations.
The absence of significant isolated predictors in the analyzed data suggests that obstruction is a multifactorial process, which means that the summation of a number of different processes may be responsible for the observed hemodynamic repercussions. Further studies using multivariate analysis on a larger number of patients are thus required to confirm this hypothesis.
Clinical findings of vascular alteration on the site of catheter placement were negatively correlated with ultrasound findings, suggesting physical examination was very inaccurate in detecting such anomalies. Echo Doppler tests are thus required, regardless of whether alterations were detected in clinical examination. This has been supported by other authors who reported presence of clinical signs and symptoms in 3.7% of the individuals with deep venous thrombosis.12,14
One possible strategy to reduce the incidence of complications is resorting to ultrasound-guided DLC placement to identify unsuitable veins (vessels with thrombi, excessively thin veins) and anatomical variations in vein positioning in relation to arteries, thereby increasing the safety of the procedure. Studies have shown that ultrasound-guided internal jugular vein DLC placement resulted in lower incidence of immediate complications.15
TABLE 1 BASELINECHARACTERISTICSOFTHEENROLLED PATIENTS
n (%)
Gender
Male 66.7
Female 33.3
Age
Above 60 years 38.0
Under 60 years 62.0
Comorbidities
Diabetes 35.7
Hypertension 90.4
Dyslipidemia 2.3
Heart disease 52.3
Habits
Smoking 35.7
Drinking 16.6
Site of insertion
Jugular 73.8
Subclavian 26.1
Femoral 4.7
Catheter dwelling time
Over 30 days 28.5
Less than 30 days 71.5
Infection 9.5
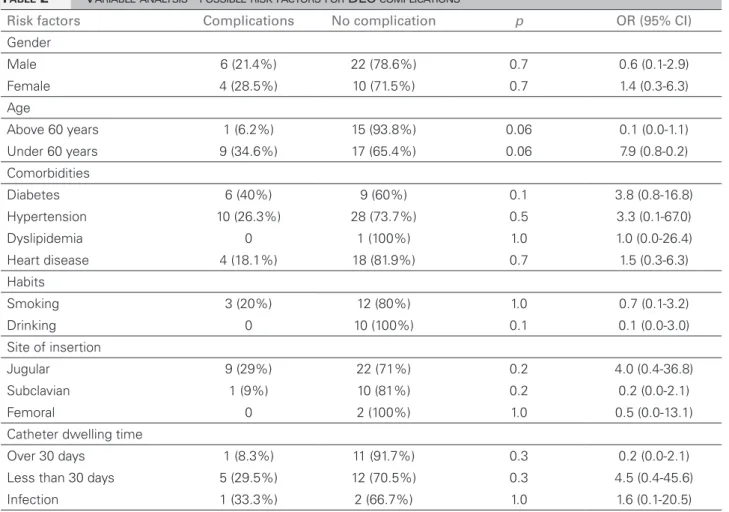
major comorbidities (systemic hypertension, heart disease, diabetes mellitus, dyslipidemia, smoking), site of insertion, and catheter dwelling time. Results are shown in Table 2.
Vascular alterations were seen on the Echo Doppler tests of 31.25% of patients. Stenosis at the site of insertion was observed in 21.9% of the cases (Figure 1), whereas obstruction with recanalization was seen in 6.25% (Figure 2) and obstruction without recanalization in 3.13% of the patients.
No correlation was observed between physical examination and ultrasound findings (k = -0.123; 95% CI: -0.238 to -0.009).
D
ISCUSSIONTABLE 2 VARIABLEANALYSIS - POSSIBLERISKFACTORSFOR DLC COMPLICATIONS
Risk factors Complications No complication p OR (95% CI)
Gender
Male 6 (21.4%) 22 (78.6%) 0.7 0.6 (0.1-2.9)
Female 4 (28.5%) 10 (71.5%) 0.7 1.4 (0.3-6.3)
Age
Above 60 years 1 (6.2%) 15 (93.8%) 0.06 0.1 (0.0-1.1)
Under 60 years 9 (34.6%) 17 (65.4%) 0.06 7.9 (0.8-0.2)
Comorbidities
Diabetes 6 (40%) 9 (60%) 0.1 3.8 (0.8-16.8)
Hypertension 10 (26.3%) 28 (73.7%) 0.5 3.3 (0.1-67.0)
Dyslipidemia 0 1 (100%) 1.0 1.0 (0.0-26.4)
Heart disease 4 (18.1%) 18 (81.9%) 0.7 1.5 (0.3-6.3)
Habits
Smoking 3 (20%) 12 (80%) 1.0 0.7 (0.1-3.2)
Drinking 0 10 (100%) 0.1 0.1 (0.0-3.0)
Site of insertion
Jugular 9 (29%) 22 (71%) 0.2 4.0 (0.4-36.8)
Subclavian 1 (9%) 10 (81%) 0.2 0.2 (0.0-2.1)
Femoral 0 2 (100%) 1.0 0.5 (0.0-13.1)
Catheter dwelling time
Over 30 days 1 (8.3%) 11 (91.7%) 0.3 0.2 (0.0-2.1)
Less than 30 days 5 (29.5%) 12 (70.5%) 0.3 4.5 (0.4-45.6)
Infection 1 (33.3%) 2 (66.7%) 1.0 1.6 (0.1-20.5)
Figure 1. Parietal thickening, diffuse stenosis, right jugular vein. Figure 2. Occlusion with proximal recanalization, left jugular vein.
In view of these findings, we must stress the importance of a having multidisciplinary care team with radiologists, nephrologists and angiologists to prevent the complications and morbidity associated with DLCs.
C
ONCLUSIONVascular alterations derived from the use of
R
EFERENCES1. Sesso RCC, Lopes AA, Thomé FS, Lugon JR, Watanabe Y, Santos DR, et al. Diálise crônica no Brasil - Relatório do Censo Brasileiro de Diálise, 2011. J Bras Nefrol 2012;34:272-7. DOI: http://dx.doi.org/10.5935/0101-2800.20120009
2. Romão Júnior JE. Doença renal crônica: definição, epidemiologia e classificação. J Bras Nefrol 2004;26:1-3. 3. National Kidney Foundation. KDOQUI Clinical Practice
Guidelines and Practice Recommendations for 2006 Updates: Hemodialysis Adequacy, Peritoneal Dialysis Adequacy and Vascular Access. Am J Kidney Dis 2006;48:S1-S322.
4. Rocha PN, Braga PS, Ritt GF, Gusmão LF, Pontes LCS, Santos MLM. Complicações imediatas relacionadas à inserção de cateteres duplo-lúmen para hemodiálise. J Bras Nefrol 2008;30:54-8. 5. Andrade G, Brito N, Marques R, Bomfim A, Abath C.
Manejo dos cateteres de hemodiálise: papel dos procedimentos intervencionistas. J Bras Nefrol 2005;27:150-6.
6. Hind D, Calvert N, McWilliams R, Davidson A, Paisley S, Beverley C, et al. Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ 2003;327:361. PMID: 12919984 DOI: http://dx.doi.org/10.1136/bmj.327.7411.361 7. Canaud B, Leray-Moragues H, Kerkeni N, Bosc JY, Martin K.
Effec-tive flow performances and dialysis doses delivered with permanent catheters: a 24-month comparative study of permanent catheters versus arterio-venous vascular accesses. Nephrol Dial Transplant 2002;17:1286-92. DOI: http://dx.doi.org/10.1093/ndt/17.7.1286 8. ACR, Apropriate criteria overview: Suspected upper
Extre-mity Deep Vein Thrombosis. 2011 [Acesso 10 Nov 2013]. Disponível em: http://www.acr.org/~/media/ACR/Documents/ AppCriteria/Diagnostic/SuspectedUpperExtremityDeepVein-Thrombosis.pdf
9. Oguzkurt L, Tercan F, Torun D, Yildirim T, Zümrütdal A, Kizilkilic O. Impact of short-term hemodialysis catheters on the central veins: a catheter venographic study. Eur J Radiol 2004;52:293-9. PMID: 15544909 DOI: http://dx.doi. org/10.1016/j.ejrad.2003.12.004
10. Schillinger F, Schillinger D, Montagnac R, Milcent T. Post catheterisation vein stenosis in haemodialysis: comparative angiographic study of 50 subclavian and 50 internal jugular accesses. Nephrol Dial Transplant 1991;6:722-4. DOI: http:// dx.doi.org/10.1093/ndt/6.10.722
11. Naroienejad M, Saedi D, Rezvani A. Prevalence of central vein stenosis following catheterization in patients with end-stage renal disease. Saudi J Kidney Dis Transpl 2010;21:975-8.
12. Vianna FJM, Castro AA, Costa AFP, Pitta GBB, Miranda Jr F. Incidência de trombose venosa profunda secundária ao implante de cateter para hemodiálise: avaliação pela ultra-sonografia com Doppler. J Vasc Br 2005;4:176-82.
13. Grothe C, Belasco AGS, Bittencourt ARC, Vianna LAC, Sesso RCC, Barbosa DA. Incidence of bloodstream infections among patients on hemodialysis by central venous catheter. Rev Latino-Am Enferm 2010;18:73-80. DOI: http://dx.doi. org/10.1590/S0104-11692010000100012
14. Vanherweghem JL, Yassine T, Goldman M, Vandenbosch G, Delcour C, Struyven J, et al. Subclavian vein thrombosis: a frequent complication of subclavian vein cannulation for hemodialysis. Clin Nephrol 1986;26:235-8. PMID: 3802586