O
BJECTIVE
To i nvest i gat e whet her hyperhom ocyst ei nem i a i s an i ndependent ri sk f act or f or at her oscl er ot i c di sease i n elderly individuals.
M
ETHODS
A case-control study with 172 elderly individuals, 88 belonging to control group and 84 to case group, who showed coronary angiography requested for clinical indications. Quantitative coronary angi ography was per f ormed i n 9 1 % of t he pat i ent s. Homocysteinemia was assessed in a continuous and categorized way, through univariate and multivariate analysis.
R
ESULTS
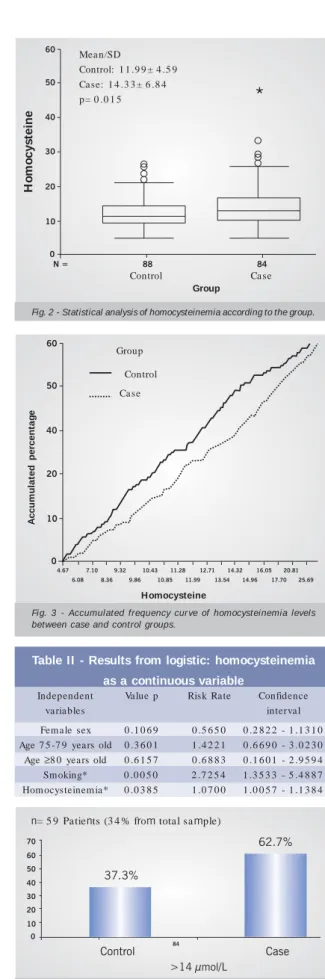
W hen analyzed continuously, in univariate analysis, it was veri f i ed t hat case gr oup el derl y i ndi vi dual s showed an average homocysteinemia levels significantly higher than the cont rol gr oup i ndi vi dual s’ (1 4 .3 3 ± 4 .5 9 µmol /l agai nst 1 1 .9 9 ± 4 .5 9 µmol /l , p= 0 .0 1 5 ). In mul t i vari at e anal ysi s, continuous homocysteinemia was associated to the risk rate for cor onar y ar t er y di sease of 1 . 0 7 f or each 1 µ m ol /l i ncrease of homocyst ei ne l evel . Na i ncrease of 5 µmol /l corresponded to the risk rate of 1 .4 0 . W hen analyzed in categorized way, the values found over percentile 75 of control group (14 µmol/l) were defined as hyperhomocysteinemia. Hyperhomocysteinemia was found in 34% of elderly individuals, being 37.3% in control group and 62.7% in case group (p= 0.009). In multivariate analysis, hyperhomocysteinemia constitu-ted an independent risk factor for coronary atherosclerotic disease for elderly individuals, with a risk rate for coronary artery disease of 2.03, confidence interval 95%, 1.02-4.03.
Mailing address:Claudia Felícia Gravina Taddei • Rua Padre João Manoel, 188/41 - 01411-000 - São Paulo, SP - Brazil E-mail: clau-gravina@hotmail.com, cgtaddei@lee.dante.br Received on 07/10/2003 • Accepted on 03/04/2005
This research was funded by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP).
Hyperhomocysteinemia as a Risk Factor for
Coronary Atherosclerotic Diseases in the Elderly
Claudia Felícia Gravina-Taddei, Michel Batlouni, Camila Sarteschi, Valéria T. Baltar,
Nívea A. C. Salvarini, Marcelo C. Bertolami, José Eduardo M. R. Sousa
Instituto Dante Pazzanese de Cardiologia - São Paulo, SP - Brazil
C
ONCLUSION
Hyperhomocysteinemia was an independent risk factor for coronary artery disease in elderly individuals.
K
EY
WORDS
The main cause of mortality and morbidity among e ld e rly in d ivid u a ls is ca rd iova s cu la r d is e a s e1 a n d ,
particularly, coronary atherosclerotic disease, responsible for half of deaths and deficiencies in the group of elderly individuals over 8 0 years old2. Although only 2 0 to 3 0 %
among elderly individuals show clinical manifestations of coronary disease, approximately 7 0 % of people over 7 0 years old show coronary atherosclerosis at necropsy3.
There are many factors that can contribute to coronary a rtery disea se, such a s h ypertension, Dyslipidem ia , s m oking, obes ity, s edenta ry lifes tyle, a nd dia betes . However, new risk factors have been detected. Among those we find hyperhomocysteinemia.
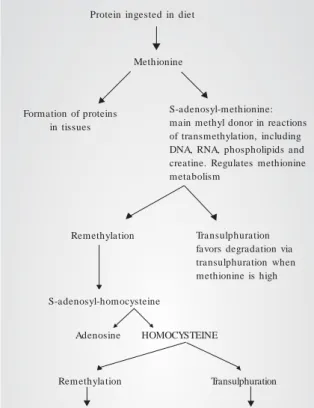
Homocysteine is an amino acid that contains sulfur, formed during methionine. It follows two end paths: part of it returns to methionine formation and the other part is
excreted in urine4 (fig. 1 ). So, homocysteine, which is
part of methionine cycle. Contribute simultaneously to its m a intena nce (m eth ionine a nd h om ocys teine a re precursory to each other). A disorder at any stage of such metabolism induces to the increase of homocysteine5.
In 1 9 6 9 , Mc Cully et al. identified the direct clinical importance of hyperhomocysteinemia, by suggesting for the first time the connection between genetic metabolic d is tu rb a n ce , ca u s e d b y h om ozygotic d e ficie n cy of cys ta tion in e B-s yn th a s e , a n d a p p e a ra n ce of e a rly a th eros cleros is in necrop s y-s ubm itted infa nts6. Th e
homozygotic deficiency of cystationine B-synthase was associated to high levels (> 1 0 0 µmol/l) of plasma and urine homocysteine, followed by diffuse atherosclerosis, which led to the appearance of coronary atherosclerotic disease, peripheral vascular disease and cerebrovascular accident in infants. It was also observed that individuals with m odera te increa se of h om ocysteine levels a lso sh owed a n increa sed risk of ca rdiova scula r disea se. Such m odera te increa se resulted from h eterozygotic d e fic ie n c y o f c ys t a t io n in e B -s yn t h a s e (CBS ) o r of m e th yle n e te tra h yd rofola te re d u c ta s e (MTHFR), an enzyme involved in the homocysteine remethylation in methionine.
In a ddition to congenita l fa ctors (h om ozygotic or heterozygotic deficiency of CBS, and heterozygotic of MTH FR), o t h e r fa c t o rs m a y c a u s e in c re a s e o f h om ocys te in e m ia in a s m a lle r p rop ortion, s u ch a s nutritional factors (deficit of vitamins B6 , B1 2 and folate), ph ysiologica l fa ctors (a ge, sex)7, lifestyle (sm oking8,
e xc e s s ive in ge s tion of c offe e9, a lc oh olic b e ve ra ge
consumption1 0, sedentary lifestyle1 0), the action of some
m e d ic in e s (n it ric oxid e , is on ia zid e , t h e op h yllin e , c a rb a m a ze p in e , m e t h o t re xa t e , n ia c in , c h o le s t y-ra m ine)1 1 ,1 2, s om e dis ea s es (ch ronic rena l fa ilure1 3,
psoria sis). It is a lso considered tha t a n a ging-rela ted decrease in the activity of enzymes responsible for the metabolism of homocysteine1 4 may occur. It was also
s u gge s t e d t h a t va s c u la r c h a n ge s a re in d u c e d b y homocysteine itself1 5.
Action m ech a nism s by wh ich h yperh om ocysteine would cause injurious effects are not clear yet. It is believed th a t e n d oth e lia l d ys fu n ction, s m ooth va s cu la r ce ll proliferation and coagulation disturbances1 6 -1 9, constitute
important factors in that process.
Th e a s s oc ia tion b e twe e n p la s m a h om oc ys te in e concentration and atherosclerosis has been investigated in some clinical studies2 0 -2 7, with controversial results.
Such disagreement existent in medical literature attracted the attention to the research of hyperhomocysteinemia as an independent risk factor for coronary disease in elderly individuals.
Another point of disagreement among the authors is the limits of normal variation of homocysteine plasma concentra tion a m ong the genera l popula tion a nd the d e fin ition of h yp e rh om ocys te in e m ia . Som e a u th ors
Recycling of 5 0 % intra cellula r h o m o c ys t e in e in m e t h io n in e through 2 reactions:
1 ) 5 m e t h ylt e t ra h yd ro fo la t e -hom ocysteine m ethyltransferase enzyme (methionine synthase). Methylcobalamin (vitamin B1 2 ) and methyltetrahydrofolate serve as co-factor and co-substrate for that enzyme.
5 -m eth yltetra h ydrofola te repre-sents the main circulating form of folate, and is catalyzed by methy-le n e te tra h yd rofola te re d u cta s e (MTHFR),
2 ) b e ta in e h om ocys te in e m e -thyltransferase enzyme.
5 0 % of intra cellula r hom ocys-t e in e c o m b in e s w iocys-t h s e rin e through B6 -dependent enzyme, Cys t a t h ion in e -b e t a -Syn t h a s e (CBS) to form cystathionine. Cystathionine is metabolized in cysteine and alpha-cetobutyrate b y B6 ga m m a cys ta th ion a s e -dependent enzyme.
Cys t e in e /ot h e r a m in o a c id s : excreted in urine.
Protein ingested in diet
Methionine
S-adenosyl-methionine: main methyl donor in reactions of transmethylation, including DNA, RNA, phospholipids and creatine. Regulates methionine metabolism
Formation of proteins in tissues
Transulphuration favors degradation via transulphuration when methionine is high Remethylation
S-adenosyl-homocysteine
Adenosine HOMOCYSTEINE
Transulphuration
Fig. 1 - Schematized metabolic cycle of homocysteine.
suggested that such values may vary in several countries, being recommendable that each country determines its own normality values. In Japan, for example, average values of homocysteine, in health individuals, are 6 µmol/ l, and in South Africa, they are 1 3 µmol/l2 8.
The definition of hyperhomocysteinemia in a population is perform ed by using a n a rbitra ry cut-off point, for example, above percentile 9 5 , a method similar to the in it ia l a s s e s s m e n t m e t h o d s fo r c h o le s t e ro l a n d hypertension levels2 9 ,3 0. According to some authors, the
“normal” blood homocysteine limits oscillate between 5 and 1 5 µmol/l3 1 ,3 2. According to others, the average value
for plasma homocysteine lies between 9 to 1 0 µmol/l3 3 ,3 4.
Values that are equal to or greater than 1 6 µmol/l are, arbitrarily called hyperhomocysteinemia, which can be m odera te (1 6 -3 0 µm ol/l), interm edia te (3 1 -1 0 0 ), or severe (> 1 0 0 µmol/l ). Among elderly individuals, the limits of normal variation have not been established yet.
M
E
T
H
O
D
S
A case-control-type study was performed, with data collection in 1 7 2 patients with age equal to or higher than 6 5 years old and recent coronary angiography. Data we re colle cte d b y m e a n s of coron a ry a n giogra p h y, anamnesis, questionnaire, physical exam, anthropometric measurements and blood tests. “Off-line” quantitative coronary angiography, by using Quantitative Coronary Angiography-Cardiovascular Measure System (QCA-CMS) program of Medical Imaging System, version 5 .1 and 3 .0 , was performed in 9 1 % of elderly individuals.
Th e inclusion criteria were a s follows: a ) Ca ses: represented by elderly individuals who showed coronary angiography-proven CAD, with lesion from 7 0 % to 1 0 0 % in one or more main arteries (left coronary trunk, anterior descending artery, right coronary artery, circumflex artery). The lesion magnitude was confirmed by a duly qualified observer by means of an “off-line” quantitative analysis. b) Controls: represented by elderly individuals who did not show obstructive lesions at coronary angiography or wh o sh owed, in seconda ry bra nch , discreet pa rieta l irregularities or single inferior lesion at 3 0 %, measured by off-line quantitative angiography.
The quantitative angiography analysis was performed in initial, middle and distal portions of left coronary trunk, anterior descending artery, septal artery, diagonal arteries, circum flex a rtery, m a rgina l a rteries, circum flex a rtery atrioventricular branch, right coronary artery, posterior ventricular artery, posterior descending artery and left ventricular fraction of ejection.
The elderly individuals were submitted to coronary angiography for several reasons, such as investigation of precordialgia, valvopathies or arrhythmias.
The exclusion criteria were as follows: regular use of vitamins; neoplasias lack of compression of the protocol;
history of myocardial revascularization or angioplasty; acute coronary insufficiency in the last 3 0 days; serum creatinine higher than 2 mg/dl; cerebrovascular accident.
Homocysteine, glucose, triglycerides, total cholesterol, HDL cholesterol (calculation of LDL cholesterol through Friedewald formula), creatinine, blood count, albumin, TSH, T4 free were dosed in the blood.
Hom ocysteinem ia was dosed through fluorescence p ola riza tion im m unoa s s a y (FP IA), b y us ing AXSYM equipment from Abbott, duly validated through correlation with Imx® Homocysteine assay, by using linear regression
analysis3 5. For its turn, Imx® Homocysteine assay was
d u ly va lid a te d with th e tra d ition a l m e th od of h igh performance liquid chromatography (HPLC)3 6.
The material collected for homocysteinemia dosage was placed in a dry tube, without anticoagulant, and centrifuged in a period shorter than 3 0 minutes3 7, at the
collection site, in order to separate red blood cells from serum. The resulting serum was placed in 2 ml cryotubes. It was then transported to the central laboratory and stored in a refrigerator for a further analysis, at a temperature of -8 0 °C. After defrosting, the sam ples were com pletely h om oge n ize d th rou gh a gita tion, in low s p e e d , a n d ce n trifu ge d a ga in, to re le a s e th e s a m p le from a n y in terferen ce a n d a s s u re th e con s is ten cy of res u lts . Hom ocys teine dos a ge wa s repea ted in a ll a na lyzed samples, with an excellent reproducibility, confirming the results found in accordance to the variation coefficient described for the method3 8.
Variables of the study: anam nesis, physical exam , analysis of risk factors and serum dosages allowed for esta blishing dia gnoses of dyslipidem ia , hypertension, diabetes mellitus, hypertriglyceridemia, obesity, smoking a nd sedenta ry lifestyle, which a re necessa ry for the assessment of hyperhomocysteinemia as an independent risk fa ctor. The elderly individua ls who m a de use of antihypertensive medication and those who showed high blood pressure on the da y of the a ppointm ent were considered as hypertensive, according to consensus of Diretrizes em Cardiogeriatria da Sociedade Brasileira de Cardiologia3 9 (systolic blood pressure ≥1 4 0 mmHg and/
measurement4 1 and waist-hip ratio measurement4 2. For
the elderly individual not being regarded as sedentary, the practice of at least 1 5 minutes of programmed physical a ctivity, 3 tim es a week4 3, wa s necessa ry. Dia betes
mellitus was diagnosed through feast glycemia > 1 2 6 mg/dl, through the use of hypoglycemic medication or previous diabetes diagnosis.
For the comparison of the groups, the chi-square test, for qualitative variables, and the t-test of Student, for quantitative variables, were used in univariate analysis. In ca s e s in wh ich th e re wa s n o n orm a lity in d a ta distribution, the non-parametric test of Mann-Whitney was used. For the comparison of more than two means (as with “age”) the non-parametric test of Kruskall-Wallis was used. In m ultiva ria te a na lysis th e logistic regression method was used. The inclusion criteria of independent va ria bles in regression m odel were th e results from u n iva ria t e a n a lys is a n d c lin ic a l re le va n c e . Th e independent variables included in the model were sex, age classes (6 5 -7 4 years old, 7 5 -7 9 years old, and ≥8 0 years old), sedentary lifestyle, smoking (smokers versus non-smokers), high LDL cholesterol, low HDL cholesterol, high total cholesterol, hypertension, diabetes, obesity (according to BMI), homocysteinemia, serum creatinine > 1 .4 mg/dl (yes versus no).
The observa tion of hom ocysteine levels, displa yed continuously on the accumulated frequency curve in the 2 groups, allowed for the identification of the point at which the homocysteinemia of the patients of case and control groups were most different, percentile 7 5 . So, we selected the value of homocysteinemia found in percentile 7 5 of the sample under study, 1 4 µmol/l, as cut-off point for categorization in hyperhomocysteinemia. That value coincides with the value of percentile 8 0 of Robinson’s sample4 4, arbitrarily chosen as cut-off point to calculate
the prevalence of hyperhomocysteinemia in the population he studied. Then, a second univariate analysis with chi-square test, and a second m ultivariate analysis, with logistic regression m odel, were ca rried out, in which hyperhomocysteinemia was assessed as a categorical variable (≤1 4 and > 1 4 µmol/l). The inclusion criteria of independent variables were the results from the univariate analysis and clinical relevance. The independent variables included in the previous analysis were repeated.
The results whose descriptive levels (p values) were lower than 0 .0 5 were regarded as statistically significant.
R
E
SULTS
One hundred and seventy-two (1 7 2 ) patients with age ranging between 6 5 and 8 0 years old, with 8 4 belonging to case group and 8 8 to control group. The distribution of age, sex and risk factors is exhibited in table I.
Patients from case group, in addition to show severe lesion in main arteries, showed other different intensity lesions in secondary branches. Control group patients showed corona ries free of a therosclerotic process a t coronary angiography in 8 3 % of the cases; only 1 5 patients showed discreet parietal irregularities or single lesion of discreet level (< 3 0 %) in secondary arterial branch.
Quantitative coronary angiography was performed in 9 1 % of the patients, confirming coronary angiographic data. The main diagnoses found were HAS (8 3 .1 %), coronary insufficiency (5 0 %, from which 2 5 .6 % have already had m yoca rdia l infa rction), dyslipidem ia (4 1 %), dia betes mellitus (2 7 .9 %), arrhythmia (1 3 .4 %), segmental or diffuse left ventricular dysfunction (5 7 .1 %), congestive heart failure (4 . 1 %), a tria l fibrilla tion (5 .2 %), m itra l insufficiency (3 .5 %), aortic insufficiency (2 .9 %), aortic stenosis (5 .2 %), mitral stenosis (1 .2 %), syncope (2 .3 %).
Th e m a in m edicines under use were a ntipla telet (6 6 .3 %), conversion enzyme inhibitors (5 8 .1 %), diuretics (5 3 . 5 % ), b e t a -b loc ke rs (4 7 . 1 % ), n it ra t e s (4 3 % ), hypolipemiants (2 4 .4 %), hypoglycemic (2 3 .8 %), calcium channel antagonists (1 8 %), digital (1 0 .5 %), aldosterone II receptor antagonists (5 .2 %), anticoagulants (3 .5 %)
The mean and standard deviation of homocysteinemia levels found in elderly individuals were 1 1 .9 9 µmol/l ± 4 .5 9 in control group, and 1 4 .3 3 µmol/l ± 6 .8 4 in case group, p= 0 .0 1 5 (fig. 2 ). The accumulated frequency
Control Group Case Group Total p
n (%) n (%)
Age (years old) 6 5 -8 8 6 5 -8 6 6 5 -8 8 0 .4 0 5
Mean± SD 7 2 .2 ± 0 .4 6 9 7 2 .7 7 ± 0 .4 9 5 7 2 .4 8 ± 0 .3 4
Sex
Male 2 7 (3 0 .7 ) 4 5 (5 3 .6 ) 7 2 (4 1 .9 ) 0 .0 0 2 *
Female 6 1 (6 9 .3 ) 3 9 (4 6 .4 ) 1 0 0 (5 8 .1 )
Hypertension 7 7 (8 7 .5 ) 6 6 (7 8 .6 ) 1 4 3 (8 3 .1 ) 0 .1 1 8
Dyslipidemia 2 7 (3 0 .7 ) 4 4 (5 2 .4 ) 7 1 (4 1 .3 ) 0 .0 0 4 *
Diabetes 1 9 (2 1 .6 ) 2 9 (3 4 .5 ) 4 8 (2 7 .9 ) 0 .0 5 9
Smoking
Non-smoker (never smoked) 5 9 (6 7 ) 3 2 (3 8 .1 ) 9 1 (5 2 .9 ) < 0 .0 0 1 *
Smoker (ex-smoker/smoker) 2 9 (3 3 ) 5 2 (6 1 .9 ) 8 1 (4 7 .1 )
Physical activity
Yes 6 9 (7 8 .4 ) 5 5 (6 5 .5 ) 1 2 4 (7 2 .1 ) 0 .0 3 1 *
No 1 9 (2 1 .6 ) 2 9 (3 4 .5 ) 4 8 (2 7 .9 )
Obesity
BMI ≥3 0 kg/m2 2 9 (3 3 ) 2 4 (2 8 .6 ) 5 3 (3 0 .8 ) 0 .5 3 4
Waist-hip ratio 2 5 (2 8 .4 ) 2 6 (3 1 ) 5 1 (2 9 .7 ) 0 .7 1 5
Man > 0 .9 8 cm Woman > 0 .9 0 cm
Abdominal circumference 5 3 (6 0 .2 ) 5 1 (6 0 .7 ) 1 0 4 (6 0 .5 ) 0 .9 4 8
Man > 1 0 2 cm Woman > 8 8 cm
Table I - Distribution of age, sex and risk factors
curve of homocysteine levels demonstrated that, along the whole sample, more control group patients showed lower values than the patients from case group (fig. 3 ).
In multivariate analysis, by using the logistic regression model, the stepwise forward method for the final selection of independent variables for obstructive atherosclerotic disease was employed. Variables that remained in the final equation, after the use of stepwise forward method, were smoking, and homocysteinemia. Sex and age had their entry forced in the final model, in spite of not showing statistical significance after the use of stepwise forward method. Those variables were included in a special way, for being frequent questionings when a relation between a va ria b le a n d a clin ica l con d ition is tr yin g to b e esta blished. Continuously a na lyzed hom ocysteinem ia showed a risk rate of 1 .0 7 , with confidence interval from 1 .0 0 5 7 to 1 .1 3 8 4 , p= 0 .0 3 8 5 . This means that for every increase of a unit (1 µmol/l) of homocysteine, the elderly individual showed 7 % more chance of being case, which means, of showing coronary disease. An increase of 5 µmol/l of homocysteine was associated to the risk rate of 1 .4 0 3 (which means, 4 0 % more chance of being case).
Smoking showed a risk rate of 2 .7 2 5 4 , confidence interval from 1 .3 5 3 3 to 5 .4 8 8 7 , p= 0 .0 0 5 0 (tab. II).
Ca t e go rize d h o m o c ys t e in e m ia a n a lys is (hyperhomocysteinemia): from 1 7 2 elderly individuals, 5 9 (3 4 %) showed hyperhomocysteinemia (homocysteine levels > 1 4 µmol/l). From those, 3 7 .3 % were in control group and 6 2 .7 % in case group; p= 0 .0 0 9 (fig. 4 ). In m ultiva ria te h yp erh om ocys teinem ia a na lys is , a ga in, hom ocysteine and sm oking rem ained as independent variables. Sex and age, although non-significant, were included in the final equation. Smoking showed a risk rate of 2 .7 6 4 4 , with a confidence interval from 1 .3 7 0 9 to 5 .5 7 4 4 , p= 0 .0 0 4 5 . Hyperhomocysteinemia showed a risk rate of 2 .0 2 9 7 , with a confidence interval from 1 .0 2 0 7 to 4 .0 3 6 1 , p= 0 .0 4 3 5 . This means that elderly individuals with homocysteinemia higher than 1 4 µmol/ l showed 2 .0 3 times more chance to be CAD than elderly individuals with plasma levels of homocysteine lower than 1 4 µmol/l (tab. III).
D
IS
C
USSION
Th e re s u lt s from t h is c lin ic a l-e p id e m iologic a l
A
c
c
u
m
u
la
te
d
p
e
rc
e
n
ta
g
e
Homocysteine
Control Group
Fig. 3 - Accumulated frequency curve of homocysteinemia levels between case and control groups.
Table II - Results from logistic: homocysteinemia
as a continuous variable
Independent Value p Risk Rate Confidence
va ria bles interva l
Fem ale sex 0 .1 0 6 9 0 .5 6 5 0 0 .2 8 2 2 - 1 .1 3 1 0 Age 7 5 -7 9 years old 0 .3 6 0 1 1 .4 2 2 1 0 .6 6 9 0 - 3 .0 2 3 0 Age ≥8 0 years old 0 .6 1 5 7 0 .6 8 8 3 0 .1 6 0 1 - 2 .9 5 9 4 Sm oking* 0 .0 0 5 0 2 .7 2 5 4 1 .3 5 3 3 - 5 .4 8 8 7 Hom ocysteinem ia * 0 .0 3 8 5 1 .0 7 0 0 1 .0 0 5 7 - 1 .1 3 8 4
n= 5 9 Patients (3 4 % from total sample)
Fi g. 4 - Preval ence of hyperhomocyst ei nemi a (> 1 4 µmol /l ) second group.
Table I I I - Results from logistic regression: hyperhomocysteinemia as categorized variable
(> 1 4 mmol/l)
Independent Value P Risk Rate Confidence
va ria bles interva l
Fem ale sex 0 .1 3 8 7 0 .5 9 1 1 0 .2 9 4 7 - 1 .1 8 5 5 Age 7 5 -7 9 years old 0 .3 2 8 8 1 .4 5 6 3 0 .6 8 4 8 - 3 .0 9 6 8 Age ≥8 0 years old 0 .7 7 7 5 0 .8 1 6 4 0 .1 9 9 9 - 3 .3 3 4 7 Sm oking* 0 .0 0 4 5 2 .7 6 4 4 1 .3 7 0 9 - 5 .5 7 4 4 Hyperhomocysteinemia* 0 .0 4 3 5 2 .0 2 9 7 1 .0 2 0 7 - 4 .0 3 6 1 Mea n/SD
Control: 1 1 .9 9 ± 4 .5 9 Case: 1 4 .3 3 ± 6 .8 4 p= 0 .0 1 5
H
o
m
o
c
y
s
te
in
e
Control Ca se Group
Fig. 2 - Statistical analysis of homocysteinemia according to the group.
s t u d y, w it h c a s e -c on t rol p la n , d e m on s t ra t e d t h a t hyperhomocysteinemia is an independent risk factor for obstructive atherosclerotic disease in elderly individuals (ris k ra te of 1 . 0 7 for ea ch increa s e of 1 µ m ol/l of h o m o c ys t e in e m ia ). An in c re a s e o f 5 µ m o l/l o f homocysteinemia corresponded to an estimate risk (risk rate) of 1 .4 0 . Elderly individuals with hyperhomocys-teinemia showed a risk rate of 2 .0 3 .
Stampfer et al. performed blood collection and a 5 -year follow-up of 1 4 ,9 1 6 apparently healthy physicians. The main outcome analyzed was myocardial infarction (AMI) or death due to coronary artery disease. Blood samples from 2 7 1 physicians who developed AMI were analyzed for homocysteinemia dosage, with matching and a djusted controls for a ge a nd sm oking. Th e a uth ors concluded that moderately high levels of homocysteine were associated with subsequent AMI risk, regardless of other factors4 5. Meta-analysis carried out by Boushey
showed that an increase of 5 µmol/l of homocysteine was associated to an increase in risks of coronary artery disease of 6 0 % in men and 8 0 % in women4 6. Glueck et
al. dosed homocysteine in 4 8 2 consecutive patients, sent for d ia gn os is a n d t re a t m e n t of d ys lip id e m ia , a n d concluded tha t it is a n independent risk predictor of coronary disease4 7. A revision made by Van der Griend4 8
p res en ted a growin g ep id em iologica l evid en ce th a t hyperhomocysteinemia is an “independent cardiovascular risk factor, although the cause and effect relationship is not proven yet.”
Howe ve r, oth e r s tu d ie s d id n ot s h ow th e s a m e conclusion. Folsom et al., in a prospective case-cohort-type study, with a duration of 3 .3 years, asserted that their findings give rise to doubts to conclusions tha t hyperhomocysteinemia be an independent risk factor for coronary artery disease. Those authors suggested that a therosclerosis could a lone rise hom ocysteine levels, w h ic h w o u ld re s u lt in a n a s s o c ia t io n b e t w e e n h yp erh om ocys teinem ia a nd corona ry a rtery dis ea s e (CAD), t h ro u gh a re ve rs e c a s u a lt y m e c h a n is m (hyperhomocysteinemia could be the consequence and not the cause of CAD). It was also suggested that, in CAD patients, hyperhomocysteinemia could forecast a bad prognosis, reflecting severity of CAD and the possibility of a risk of thrombosis4 9.
St a m p le r, in a p re viou s ly m e n t ion e d a rt ic le4 6,
a nticipa tes tha t question a nd a sserts tha t the doubt whether high homocysteine could be the consequence a nd not the ca use of a cute m yoca rdia l infa rction, is rejected by the prospective planning of his study.
Similarly, that reverse casualty hypothesis was not accepted by Bostom and Selhub5 0, who asserted, in an
editorial published in 1 9 9 9 , it was not the same supported b y e p id e m iologic a l e vid e n c e of m a n y w orks a n d by the findings in studies in humans and animals, such a s t h e p re s e n c e o f a t h e ro t h ro m b o t ic e ve n t s a t 3 0 yea rs of a ge, in 5 0 % of infa nts with non-trea ted
hyperhom ocysteinem ia , a nd in young a dults, without traditional risk factors and with homocystinuria due to deficiency of cysta tionine syntha se. The reduction of h om ocysteinem ia levels in th ose pa tients sh owed a decrease of the incidence of cardiovascular events5 1 ,5 2.
Randomized and controlled studies revealed that diet-induced hyperhom ocysteinem ia resulted in a bnorm a l vascular reactivity in primates5 3. Among young individuals,
without atherosclerosis or risk factors for coronary disease and with normal flow reactivity of brachial artery5 4, a
stressed reduction of flow reactivity of brachial artery after acute hyperhomocysteinemia, caused by an oral dose of L-methionine, was observed.
Studies in th e litera ture used a ppa rently h ea lth y individuals, with absence of clinical symptoms of coronary in s u fficie n cy or e le ctroca rd iogra p h ic ch a n ge s5 5, a s
inclusion criteria in control group. However, due to the sca rce a nginous sym ptom a tology, wh ich m a y occur among elderly individuals, the option in this work was for not choosing control group among apparently healthy elderly individuals. So, despite the difficulty to detect elderly individuals, with age equal to or higher than 6 5 yea rs old, with corona ry a ngiogra ph y dem onstra ting absence of lesions or ischemia, such criterion was used for considering it stricter and to allow for a greater reliability in the comparison between groups.
The findings of the present study agree on the fact that hyperhomocysteinemia constitutes a risk factor for coronary disease in elderly individuals. It suggests, for example, that the average value of homocysteine among Brazilians may be similar to that among Americans: the Hordaland Homocysteine Study9 (carried out in 3 ,3 1 8
elderly individuals from 6 5 to 6 7 years old) detected average levels of homocysteine of 1 2 .3 µmol/l in men and 1 1 µmol/l, in women; the Framingham study5 6 (with
1 1 6 0 elderly individuals from 6 7 to 9 6 years old) showed an average homocysteine concentration of 1 1 .9 µmol/l, which coincides exactly with the one in this study, 1 1 .9 9 µmol/l. Studies with a greater number of Brazilian elderly individuals are necessary to confirm such suggestion.
It was also observed that differences between the m ea ns of h om ocysteine levels a m ong elderly indivi-d u a ls w it h a n indivi-d w it h ou t t h e indivi-d is e a s e w e re s m a ll, 2 .3 4 µmol/l or 1 6 %. That finding is in accordance to the one found by other a uthors. Verhoef5 7 (who evinced
hyperhomocysteinemia being an independent risk factor for myocardial infarction, with risk rate of 1 .3 5 for each increase of 3 µmol/l of homocysteine), found an 1 1 % difference. In the Physicians Health Study4 6, the cases
had an average homocysteine level only 5 .7 % higher than the one in controls. The authors considered that, although the differences had been modest, they were similar to the differences of means for many established risk factors, such as cholesterolemia and blood pressure.
as the values found in this study, over 1 4 µmol/l, were associated to an estimate risk of 2 .0 3 for coronary disease.
It was not observed significant difference in traditional risk factors in both groups, except smoking. Such fact is justified for the own structure of the study model used here, in which, although control group patients were free from coronary disease, they showed many risk factors. Besides, risk factors were being controlled. The same happened to Robinson’s study4 5, regarding dyslipidemia,
a nd to Trom so’s study5 8, rega rding hypertension a nd
h yp e rtriglyce rid e m ia . Th e a u th ors con s id e re d s u ch findings as resulting from the treatment of risk factors and change in lifestyle.
In conclusion, data obtained in this study allow for
concluding th a t elderly individua ls with obs tructive corona ry a therosclerotic disea se showed significa ntly higher homocysteinemia levels than elderly individuals without obstructive coronary atherosclerotic disease, and tha t hyperhom ocysteinem ia wa s a n independent risk fa ctor for corona ry a th erosclerotic disea se in elderly individuals.
A
C
KNOWL
ED
G
E
M
E
NTS
To the radiology technician Wagner Vieira Pinto and the em ployees from the Clinical Laboratory, of Dante Pa zza nes e Ins titute of Ca rdiology for th e im p orta nt collaboration in this work.
1 . La Ros a J . Pre ve n t ion of c a rd iova s c u la r d is e a s e in t h e e ld e rly population. In: Wenger N. Inclusion of Elderly Individuals in Clinical Trials: Cardiovascular Disease and Cardiovascular Therapy as a Model.
Kansas City: Marion Merrell Dow, 1 9 9 3 : 2 2 9 -4 2 .
2 . We n ge r N. Th e la n d s c a p e of c a rd iova s c u la r illn e s s in th e n e xt millennium: challenges an opportunities for the care of the oldest old. In : We n ge r N. Ca rd iova s cu la r Dis e a s e in th e Octoge n a ria n a n d Beyond. Ma rtin Dunitz, 1 9 9 9 : 1 -8 .
3 . Tresch D, Aronow W. Recognition a nd dia gnosis of corona ry a rtery d is e a s e in th e e ld e rly. In : Tre s ch D, Aron ow W. Ca rd iova s cu la r Disease in the Elderly Patient. New York: Marcel Dekker, 1 9 9 9 : 1 9 7 -2 1 -2 .
4 . Ma ye r E, J a cob s e n D, Rob in s on K. Hom ocys te in e a n d coron a ry atherosclerosis. J Am Coll Cardiol 1 9 9 6 ; 2 7 : 5 1 7 -2 7 .
5 . Sta m pfer M, Ma linow R. Ca n lowering hom ocysteine levels reduce cardiovascular risk? N Engl J Med 1 9 9 5 ; 3 3 2 : 3 2 8 -9 .
6 . Mckully KS. Vascular pathology of homocysteinemia: Implications for the pathogenesis of arteriosclerosis. Am J Pathol 1 9 6 9 ; 5 6 : 1 1 1 -2 8 .
7 . Nygard O, Vollset SE, Refsum H et al. Total plasma homocysteine and ca rd iova s cu la r ris k p rofile : th e Hord a la n d Hom ocys te in e Stu d y. JAMA 1 9 9 5 ; 2 7 4 : 1 5 2 6 -3 3 .
8 . Stampfer MJ, Malinow MR, Willet W et al. A prospective study of plas-mahomocysteine and risk of myocardila infarction in US physicians. JAMA 1 9 9 2 ; 2 6 8 : 8 7 7 -8 1 .
9 . Nygard O, Refsum H, Ueland P et al. Major lifestyle determ inants of p la s m a t o t a l h o m o c ys t e in e d is t rib u t io n : t h e H o rd a la n d Hom ocysteine study. Am J Clin Nutr 1 9 9 8 ; 6 7 : 2 6 3 -7 0 .
1 0 . Volssset S, Nyga rd O, Kva le G et a l. The Horda la nd Hom ocysteine Study: lifestyle a nd tota l pla sm a hom ocysteine in Western Norwa y. In : Gra h a m I, Re fs u m H, Ros e n b e rg I, Ue la n d P. Hom ocys te in e Me t a b o lis m : fro m Ba s ic S c ie n c e t o Clin ic a l Me d ic in e . Ma ssa chusetts: Kluwer Aca dem ic, 1 9 9 7 : 1 7 7 -8 2 .
1 1 . Welch G, Loscalzo J. Hom ocysteine and atherothrom bosis. N Engl J Med 1 9 9 8 ; 3 3 8 : 1 0 4 2 -5 9 .
1 2 . Warren CJ. Emergent cardiovascular risk factor: homocysteine. Prog Cardiovasc Nurs 2 0 0 2 ; 1 7 : 3 5 -4 1 .
1 3 . Bostom AG, Shem in D, La pa ne KL et a l. Hyperhom ocysteinem ia and traditional cardiovascular disease risk factors in end-stage re n a l d is e a s e in p a t ie n t s o n d ya lis is : a c a s e -c o n t ro l s t u d y. Atherosclerosis 1 9 9 5 ; 1 1 4 : 2 7 4 3 -8 .
REFERENCES
1 4 . Nord s trom M, Kje lls trom T. Age d e p e n d e n cy of cys ta tion e b e ta -s yn t a -s e a c t ivit y in h u m a n fib rob la -s t -s in h om oc i-s t e in e m ia a n d atherosclerotic vascular disease. Atherosclerosis 1 9 9 2 ; 9 4 : 2 1 3 -2 1 .
1 5 . Mc Cully KS. Hom ocysteine theory of a rteriosclerosis developm ent a nd current sta tus. Atherosclerosis 1 9 8 3 ; 1 1 : 1 5 7 -2 4 6 .
1 6 . Ka n a n i P, Sin ke y C, Brow in g R e t a l. Role of oxid a n t s t re s s in e n d o t h e lia l d ys fu n c t io n p ro d u c e d b y e xp e rim e n t a l hyperhom ocysteinem ia in hum a ns. Circula tion 1 9 9 9 ; 1 0 0 : 1 1 6 1 -8 .
1 7 . Ch a m b e rs J , Mcgre gor A, J e a n -Ma rie J e t a l. De m on s tra tion of r a p id o n s e t va s c u la r e n d o t h e la l d ys fu n c t io n a f t e r h yp e rh om oc ys t e in e m ia . An e ffe c t re ve rs ib le w it h vit a m in a C th era p y. Circula tion 1 9 9 9 ; 9 9 : 1 1 5 6 -6 0 .
1 8 . Jacobsen D. Hom ocysteine and vitam ins in cardiovascular disease. Clinic Chem ist 1 9 9 8 ; 4 4 : 1 8 3 3 -4 3 .
1 9 . Woo KS, Ch ook P, Lolin Y e t a l. Hip e rh om ocys te in e m ia is a ris k fa ctor for a rteria l endoth elia l dys function in h um a ns . Circula tion 1 9 9 7 ; 9 6 : 2 5 4 2 -4 .
2 0 . Selhub J, Jacques P, Bostom AG et al. Association between plasma ho-mocysteine concentrations and extracranial carotid-artey stenosis. N Engl J Med 1 9 9 5 ; 3 3 2 : 2 8 6 -9 1 .
2 1 . Nyga rd O, Nord re h a u g J , Re fs u m H, Ue la n d P e t a l. P la s m a hom ocysteine levels a nd m orta lity in pa tients with corona ry a rtery disease. N Engl J Med 1 9 9 7 ; 3 3 7 : 2 3 0 -6 .
2 2 . Malinow MR, Ducimetiere P, Luc G et al. Plasma homocysteine levels a nd gra de risk for m yoca rdia l infa rction: findings in two popultions at contrasting risk for coronary artey disease. Atherosclerosis 1 9 9 6 ; 1 2 6 : 2 7 -3 4 .
2 3 . Verh oef P, Hennekens C, Ma linow M et a l. A pros pective s tudy of plasm a hom ocysteine and risk of ischem ic stroke. Stroke 1 9 9 4 ; 2 5 : 1 9 2 4 -3 0 .
2 4 . Donner M, Klein G, Mathes P et al. A plasm a hom ocysteine levels in p a t ie n t s w it h e a rly- o n s e t c o ro n a r y h e a r t d is e a s e a n d a lo w ca rdiova scula r risk profile. Meta bolism 1 9 9 8 ; 4 7 : 2 7 3 -9 .
2 5 . Wa ld N, Wa tt H, La w M et a l. Hom ocys teine a nd is ch em ic h ea rt disea se. Results of a prospective study rega rding prevention. Arch Intern Med 1 9 9 8 ; 1 5 8 : 8 6 2 -7 .
2 7 . Aronow W, Ahn C. Association between plasm a hom ocysteine and older person. Am J Cardiol 1 9 9 7 ; 8 0 : 1 2 1 6 -8 .
2 8 . Alfthan G, Aro A, Gey K. Plasm a hom ocysteine and cardiovascular disease m ortality. Lancet 1 9 9 7 ; 3 4 9 : 3 9 7 .
2 9 . Ha nkey G, Eikelb oom J W. Hom ocys teine a nd va s cula r d is ea s e. Lancet 1 9 9 9 ; 3 5 4 : 4 0 7 -1 3 .
3 0 . Ca m m e re r MA, Ma n froi WC, Ma s ca re n h a s MA. Hom ocis te ín a , doenças cardiovasculares e fatores nutricionais. Rev Soc Cardiol Estado de São Paulo 2 0 0 1 ; 1 1 : 1 0 -7 .
3 1 . Ma linow MR, Bos tom AG, Kra us s RM. Hom ocys teine, diet, a nd ca rdiova scula r disea ses: A sta tem ent for hea lthca re professiona ls from t h e Nu t rit ion Com m it t e e , Am e ric a n He a rt As s oc ia t ion . Circula tion 1 9 9 9 ; 9 9 : 1 7 8 -8 2 .
3 2 . Christen W, Ajani U, Glynn R et al. Blood levels of homocysteine and increa sed risks of ca rdiova scula r disea se. Ca usa l or ca sua l ? Arch Intern Med 2 0 0 0 ; 1 6 9 : 4 2 2 -3 4 .
3 3 . Du e ll P B, Ma lin o w MR. H o m o c ys t e in e m ia a n d ris k o f atherosclerosis: a clinical approach to evaluation and management. Endocrinologist 1 9 9 8 ; 8 : 1 7 0 -7 .
3 4 . Ma lin ow M. Hyp e rh om oc ys t e in e m ia . A c om m on a n d e a s ily resersible risk factor for occlusive atherosclerosis. Circulation 1 9 9 0 ; 8 1 : 2 0 0 4 -6 .
3 5 . Pa ssing H, Ba blok W. A new biom etrica l procedure for testing the equa lity of m ea surem ents from two different a na lytica l m ethods. J Clin Chem Clin Biochem 1 9 8 3 ; 2 1 : 7 0 9 -2 0 .
3 6 . Yu H H, J o u b ra n R, As m i M e t a l. Ag re e m e n t a m o n g fo u r h o m o c ys t e in e a s s a ys a n d re s u lt s in p a t ie n t s w it h c o ro n a r y atherosclerosis and controls. Clinic Chem istry 2 0 0 0 ; 4 6 : 2 5 8 -6 4 .
3 7 . Rasmussen K, Moller J. Total homocysteine in clinical practice. Ann Clin Biochem 2 0 0 0 ; 3 7 : 6 2 7 -4 8 .
3 8 . Na tiona l Com m ittee for Clinica l La bora tory Sta nda rds. Eva lua tion of p recis ion p erform a n ce of clin ica l ch em is try d evices . Secon d Edition; Tentative Guideline. NCCLS Docum ent EP5 -T2 . Villanova, PA: NCCLS, 1 9 9 2 .
3 9 . I Dire t rize s e m Ca rd io ge ria t ria d a S o c ie d a d e Bra s ile ira d e Cardiologia. Arq Bras Cardiol 2 0 0 2 ; 7 9 : 1 -4 5 .
4 0 . J a n s s e n I, Ka t zm a r zyk P, Ro s s R. Bo d y m a s s in d e x, w a is t circu n feren ce, a n d h ea lth ris k: evid en ces in s u p p ort of Cu rren t National Institutes of Health Guidelines. Arch Intern Med 2 0 0 2 ; 1 6 2 : 2 0 7 4 -9 .
4 1 . III Dire t rize s s ob re Dis lip id e m ia e Dire t riz d e P re ve n ç ã o d e Ateros cleros e d o Dep a rta m ento d e Ateros cleros e d a Socied a d e Brasileira de Cardiologia. Arq Bras Cardiol 2 0 0 1 ; 7 7 : 1 -2 3 .
4 2 . Da gena is GR, Kouz S. On beh a lf of th e Hope Study Investiga tors. Progn os tic im p a c t of tota l b od y m a s s a n d wis t-to -h ip ra tio in w om e n a n d m e n a t h igh t -ris k of c a rd iova s c u la r e ve n t s . Arc h Intern Med 2 0 0 2 in p res s , a p ud Avezum A. Fa tores de ris co a s s o c ia d o s c o m in fa r t o a gu d o d o m io c á rd io n a re giã o m e t ro p olit a n a d e Sã o Pa u lo. Sã o Pa u lo, 2 0 0 2 . Te s e (Dou t ora d o) -Fa culda de de Medicina , Univers ida de de Sã o Pa ulo.
4 3 . Gravina Taddei CF, Ramos LR, Moraes JC et al. Estudo multicêntrico de idosos a tendidos em a m bula tórios de Ca rdiologia e Geria tria de Instituições Brasileiras. Arq Bras Cardiol 1 9 9 7 ; 6 9 : 3 2 7 -3 3 .
4 4 . Robinson K, Mayer E, Miller D et al. Hyperhom ocysteinem ia and low pyridoxal phosphate: common and reversible risk factors for coronary a rtery disea se. Circula tion 1 9 9 5 ; 9 2 : 2 8 2 5 -3 0 .
4 5 . Sta m pfer MJ, Ma linow MR, Willet W et a l. A prospective study of p la s m a h om oc ys t e in e a n d ris k of m yoc a rd ia l in fa rc t ion in US physicians. JAMA 1 9 9 2 ; 2 6 8 : 8 7 7 -8 1 .
4 6 . Boushey CJ, Beresford SA, Im enn GS, Motulsky AG. A qua ntita tive a s s es s m ent of p la s m a h om ocys teine a s a ris k fa ctor for va s cula r d is ea s e: p os s ib le b enefits of increa s ing folic a cid inta kes . J AMA 1 9 9 5 ; 2 7 4 : 1 0 4 9 -1 0 7 .
4 7 . Glueck C, Sha w P, La ngJ, Tra cyT, Sieve-Sm ith L, Wang Y. Evidence tha t hom ocysteine is a n independent risk fa ctor for a therosclerosis in hyperlipidem ic pacients. Am J Cardiol 1 9 9 5 ; 7 5 : 1 3 2 -6 .
4 8 . Van Der Griend R, BiesmaD, Banga JD. Hyperhomocysteinaemia as a cardiovascular risk factor: an update. Netherlands J Med 2 0 0 0 ; 5 6 : 1 1 9 -3 0 .
4 9 . Folsom A, Ja vier Neto F, Mc Govern PG et a l. Prospective study of c o ro n a r y h e a r t d is e a s e in c id e n c e in re la t io n t o fa s t in g t o t a l hom ocysteine, rela ted genetic polim orphism s a nd B vita m ins. The atherosclerosis risk in Communities (ARIC) study”. Circulation 1 9 9 8 ; 9 8 : 2 0 4 -1 0 .
5 0 . Bostom A, Selhub J. Hom ocysteine and arteriosclerosis: subclinical a nd clinica l disea se a ssocia tions. Circula tion 1 9 9 9 ; 9 9 : 2 3 6 1 -3 .
5 1 . Mudd SH, Skovby F, Levy HL et al. Natural history of hom ocystinuria d u e to cys ta th ion in e b eta s yn th a s e d eficien cy. Am J Hu m Gen et 1 9 8 5 ; 3 7 : 1 -2 5 .
5 2 . Wilc ke n DE. Th e n a t u ra l h is t o r y o f va s c u la r d is e a s e in h om ocystinuria a nd th e effects of trea tm ent. J . Inh erit Meta b Dis 1 9 9 7 ; 2 0 : 2 9 5 -3 0 0 .
5 3 . Le n t z SR, Sob e yCG, P ie gors DJ e t a l. Va s c u la r d ys fu n c t ion in m onkeys with diet-induced h yperh om ocysteinem ia . J Clin Invest 1 9 9 6 ; 9 8 : 3 2 8 -9 .
5 4 . Chambers JC, Mc Gregor A, Jean-MarieJ, Kooner JS. Acute hyperhomocysteinemia and endothelial dysfunction. Lancet 1 9 9 8 ; 3 5 1 : 3 6 -7 .
5 5 . Graham I, Daly L, Refsum H et al. Plasma homocysteine as a risk factor for vascular
disease. The European Concerned Action Project. JAMA 1 9 9 7 ; 2 7 7 : 1 7 7 5 -8 1 .
5 6 . Selhub J, Jacques PF, Wilson PWF et al. Vitamin status and intake as prim ary determ inants of hom ocysteinem ia in an elderly population. JAMA 1 9 9 3 ; 2 7 0 : 2 6 9 3 -8 .
5 7 . Verhoef P, Stampfer M, Buring J et al. Homocysteine metabolism and risk of m yo ca rd ia l in fa rction : re la tion with vita m in s B6 , B1 2 , and folate. Am J Epidem iol 1 9 9 6 ; 1 4 3 : 8 4 5 -5 9 .